Greyish pigmentation of the mucosa around implants after abutment insertion and crown cementation is considered an esthetic failure. This pigmentation is due to use of metallic abutments or a thin periodontal biotype. The purpose of the present report was to improve gingival esthetic appearance of patients with thin biotype, by modifying color in the sub-mucosal region of a screwed-on, custom made, zirconium abutment, successfully improving gingival aesthetics in a right lateral incisor.
Se considera un fracaso estético la visible decoloración grisácea de la mucosa periimplantar, después de la inserción del pilar y la cementación de la corona, esto se debe al uso de pilares metálicos o a un biotipo periodontal delgado. El objetivo de este reporte de caso es mejorar la apariencia estética gingival en pacientes con biotipo delgado, modificando el color en la región submucosa de un pilar personalizado atornillado de zirconio en un incisivo lateral derecho.
An implant-supported crown for a single tooth in the anterior section of the mouth represents an alternative with excellent results. Materials most used to achieve this are metallic abutments with a ceramicmetal restoration, or zirconium abutments with a fully ceramic crown. Nevertheless, use of metallic abutments is associated to aesthetic problems.
Due to its excellent mechanical retention,1 for many years, titanium has been the material preferred by manufacturers to achieve standardized abutments for implants. Nevertheless, their grey hue becomes visible in the presence of a thin periodontal biotype, creating thus a gingival appearance different from the gingival tissue of adjoining teet;2 moreover, in case of a gingival recession occurring after the restoration, the titanium abutment results exposed, negatively affecting patient's aesthethics.3,4 Although viable from the prosthetic perspective, these restorations can become an aesthetic failure.5
Based on scientific evidence, periodontal biotype can be diagnosed through clinical inspection, observing periodontal probe transparency through the mucosa.6,7
When mucosa measures over 1 mm in thickness, it is considered thick periodontal biotype; mucosa with thickness lesser than 1 mm is defined as thin periodontal biotype, it exhibits a delicate, almost translucent appearance and is susceptible to gingival recession,7,8 generating a greyish, unaesthetic effect known as «shine through» underneath the mucosa located around the implant.9
To replicate appearance of a natural tooth is of the utmost importance, therefore, anatomy, color appearance and thickness of the mucosa surrounding the implant must be evaluated. These are decisive and determinant factors in order to achieve soft tissue aesthetics.10
There are other factors that influence restoration aesthetics such as implant position, shape, contour and color of the prosthetic abutment.11
A study that assessed restorations on single tooth implant in aesthetic zone revealed that 60% of all cases exhibited color inequality between restoration soft tissue over implant when comparing it with the natural tooth. This represents one of the main problems found when performing implant-supported restorations.5
Zirconium abutments were introduced in implantology in an effort to improve this disadvantage. When compared to titanium-made devices, these abutments possess excellent biological advantages such as low bacterial adhesion and biocompatibility with soft tissue,10–13 thus, zirconium abutments provide highly aesthetic results.
The target of the present report was to show color modification in the sub-mucosa area of a custommade screwed-on zirconium abutment, successfully improving gingival esthetics.
Clinical case reportA 24 year old female, in apparent good general health, sought consultation due to marginal inflammation at the site of the right upper lateral incisor, with 8 mm vestibular probing depth as well as a ceramic crown restoration; patient lacked history of untoward functional habits (Figure 1).
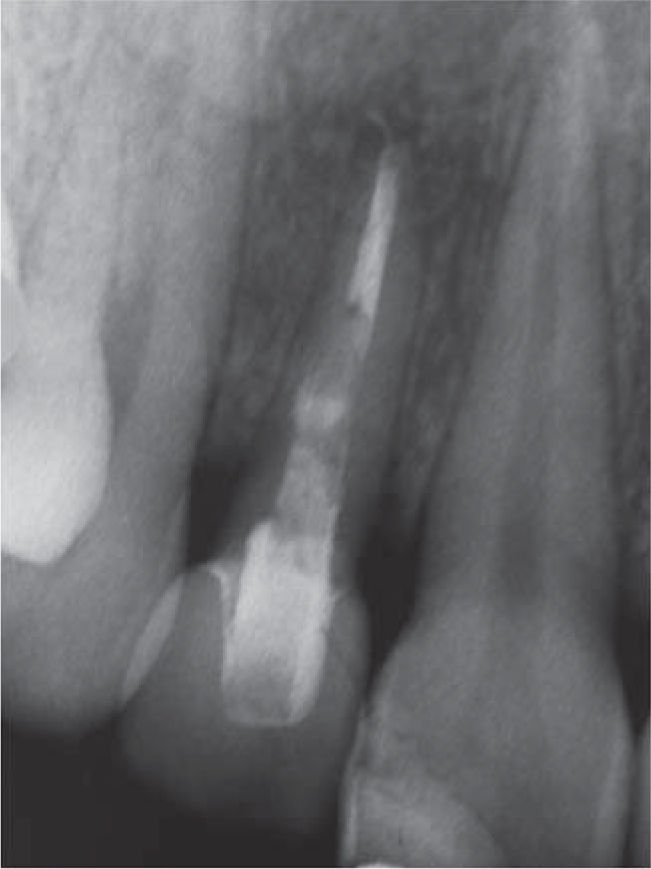
X-ray evaluation revealed one endodontically treated tooth, a lesion at the periapex and a fiber glass post (Figure 2).
Based on clinical and radiographic examination a diagnosis of longitudinal root fracture with poor prognosis was emitted.
Indications that prompted tooth extraction and immediate implant placement were the following: root fracture, advanced bone support loss, retained primary tooth, endodontic failures, non-restorable crown and dento-alveolar trauma.
After discussing different treatment options and with the patient's consent it was decided to substitute the tooth for an implant supported crown.
Requested studies such as panoramic and periapical X rays, photographs, study models and computerized axial tomography (CAT), allowed identification of anatomical structures, bone quality and availability.
The patient was medicated with etoricoxib-type analgesic (100 mgs every 24 hours), antibiotic (clindamycin 300 mg every 6 hours), extra oral ice pack applications were recommended for the first day as well as 0.2% chlorhexidine rinses for eight days.
Local, infiltrative anesthesia was applied to the area (2% lidocaine hydrochloride roxicaine) was applied to the area of the right upper lateral incisor. After this, the tooth was extracted with socket preservation (Figure 3). A 3.5 x 13 mm Replace Select (Nobel Biocare) implant was placed. Implant primary stability was confirmed by insertion of a 35 Ncm torque; in order to compensate vestibular wall alterations space between implant and buccal wall was sealed with Bi-Oss small medullar particle bone graft (Geistlich Pharma) (Figure 4). Immediate provisional treatment was achieved with prefabricated plastic abutment (Nobel Biocare) (Figure 5).
Final impression was taken six months after healing with an impression coping. Abutment pattern was manufactured with acrylic resin (Pattern Resin GC). After this it was subjected to scanning with CAD/ CAM technique (Procera Forte, Nobel Biocare USA) using zirconium (Procera oxido de zirconio, Nobel Biocare USA). Abutment setting and adaptation was verified with a periapical X-ray (Figure 6). Ceramic was applied on the polished zirconium abutment, with incisal guide parameters and aesthetics similar to the contra-lateral tooth.
A 0.5 mm thick layer of pink ceramic (Ivoclar Vivadent) was placed in the sub-mucosal section of the custom built abutment, according to manufacturer's indications, mimicking the color of gingival tissue of adjacent teeth (Figure 7), in order to compensate the greyish hue of the mucosa observed when the tooth is lacking this pinkish ceramic layer in cervical position (Figure 8).
Final restoration was screwed on with a 15 Ncm torque (Figure 9); 24 months after prosthetic load, mucosa surrounding the implant was found to be in suitable circumstances.
DiscussionBased on scientific evidence, it can be proposed that parameters bearing influence on mucosa located around the implant are tissue thickness and abutment material.14,15 This case report documents the impact exerted by color modification on the sub-mucosal section of a zirconium abutment, which yielded favorable aesthetic results.
Thickness of mucosa surrounding the implant has been assessed to possess an average of 2.0 ± 0.7 mm. Chang et al8 and Olson et al,16 in this case tissue thickness was lesser than 2 mm. According to Park et al9,17 tissue surrounding the implant tends to be delicate, with an almost translucent appearance, allowing titanium abutments to show through leaving a greyish appearance at the margin level. Discoloration caused by a titanium abutment can be decreased as opposed to titanium-made abutments; it is clinically visible at the level of the implant in the aesthetic area. Therefore, use of zirconium implants (ZrO2) are indicated for use in highly demanding aesthetic areas.4,18,19
Nevertheless, Bresan et al20 report that white zirconium abutments generate mild discoloration in thin mucosa; in order to counteract this effect, Buchi et al10 propose zirconium abutment modification by applying pinkish ceramic in the sub-mucosa area; this technique achieves excellent results. In the present case, this observation was confirmed, for that reason, the zirconium abutment in the whitish sub-mucosal area was masked with pinkish ceramic, in the crown area fluorescent ceramic was used, eliminating thus the greyish hue caused by the gingival translucency of the mucosa surrounding the implant. An additional factor is that the pink ceramic translucency is compensated, preserving tissue luminosity as well as natural-looking mucosa change of color which satisfied patient's requirements.
ConclusionType of material used for abutment and mucosa thickness bear significant influence in the change of color of mucosa surrounding the implant; this requires modification of the abutment sub-mucosa area with the application of pinkish-hued ceramic.
Additional surgery involving connective tissue graft can be avoided with the use of a modified ceramic abutment in the cervical region. Before restoring an implant in the esthetic zone, the patient must be consulted on the matter of cost-benefit of the final restoration.