The present article purports the aim of showing, in a series of cases, the application of excisional biopsy with gingivoplasty technique as treatment of pyogenic granuloma. It can be observed that accurate excision as well as elimination of contributing factors considerably decreases recurrence probabilities. Presence of pyogenic granuloma has been described in this report of a series of cases related to pregnancy, local factors such as absence of interproximal contact, presence of calculi and poor oral hygiene indexes. Moreover, it is recommended that oral hygiene instruction be the first step in treatment of pyogenic granuloma, and that after lesion excision patients receive supporting periodontal therapy.
Este artículo tiene el propósito de mostrar en una serie de casos la aplicación de la técnica de biopsia excisional con gingivoplastia como tratamiento del granuloma piógeno. También se puede observar que la correcta extirpación; así como la eliminación de los factores contribuyentes disminuye considerablemente la probabilidad de recidiva. En este reporte de serie de casos se ha descrito la presencia del granuloma piógeno relacionado al estado de gestación, a factores locales como ausencia de contacto interproximal, presencia de cálculo e índices de higiene oral malos. Además, se recomienda que la instrucción de higiene oral sea el primer paso en el tratamiento del granuloma piógeno y que posteriormente a la extirpación de la lesión los pacientes reciban terapia periodontal de soporte.
Pyogenic granuloma is a non-neoplastic tumor growth in the tissues of the mouth or skin. It is the most common type of hyperplasia in the mouth; its histology reveals proliferation of granulation tissue with inflammatory infiltrate and great angiogenic capacity; for these reasons, vascular neoformations of different diameter are normally present, these formations exhibit abrupt onset and completion within the tissue.1 From the histological point of view, this lesion can be classified into two groups: when capillary vessels are found to be organized into granulomatous tissue lobes surrounded by a thin collagen band, the formation is called «capillary lobular hemangioma», whereas when vascular formations are intertwined in the tissue without apparent order, it is called «non lobular capillary hemangioma».2
Etiology of this type of lesions is still not very clear. It is considered to be a lesion reactive to several low-degree stimuli, among which we can count repeated trauma, aggressions, hormonal factors and certain drugs. High incidence of this lesion during pregnancy is associated to high levels of estrogen and progesterone.2
Hyperplasic reactive lesions are very frequent in mouth disease. Kadeh determined that pyogenic granuloma constitutes 37% of all gingival reactive lesions in patients aged 30.4 (± 14.9) years.3
Epivatianos et al reported higher prevalence in females (1:1.5) and presence of local etiologic factors in 16% of all cases.4
From the clinical point of view, pyogenic granuloma appears as a soft, rapid-growing mass, possibly pediculated, of variable lobulated surface size and reddish hue. It can be ulcerated and exhibits high propensity to bleeding.2 Its main location is the gums (75% of all cases). It can appear less frequently on the lips, tongue, oral mucosa and palate. Lesions are more common in the upper jaw, in anterior areas and vestibular zone of the gingiva. Some lesions extend to the interproximal areas and involve lingual and vestibular aspects of the gingiva.1,2
Traditionally, treatment of choice for this type of lesions is full surgical excision with sub-periosteal curettage. In order to avoid recurrence potential irritant factors must equally be removed (plaque, overflowing restorations etc.).1 Therefore, the aim of the present article was to show a series of cases where application of accurate excision technique as well as removal of contributory factors, considerably decreased probabilities of recurrence.
Case presentationCase 1A systemically healthy, 34 year old female patient was referred to the Periodontics Masters’ Clinic of the San Martin de Porres University due to a gingival lesion located next to teeth 3.4 and 3.5. The patient informed of a bleeding gingival growth of about one year, which was at the time treated with resection. She reported gradual growth of a new lesion, which led to discomfort and bleeding when eating and brushing her teeth, as the lesion reached occlusal plane. Patient informed she was not pregnant or in any hormonal treatment.
Clinical examination revealed an inflammatory gingival lesion at the level of teeth 3.4 and 3.5. Measuring approximately 15 x 9 mm. The lesion covered the vestibular side of the clinical crown, it was firm, lobulated, of rugged texture and bleeding upon stimulus (Figures 1and2). Periodontal assessment did not reveal periodontal pockets; presence of plaque was observed, and an O’Leary oral hygiene index of 18.75 was determined. Radiographic evaluation revealed absence of interproximal contact between teeth 3.4 and 3.5 as well as restorative material in the interproximal area (Figure 3).
Presumptive diagnosis: pyogenic granuloma.
Treatment: a first session of oral hygiene instruction was conducted, followed by supra-gingival scraping.
An excisional biopsy of the lesion was taken during the second session (Figure 4). The lesion was removed during this intervention as well as a healthy tissue margin and adjacent periosteum. For histopathological examination, a sample was taken, and transported in 10% formaldehyde. After this, soft tissue was recontoured (gingivoplasty) (Figure 5), and a periodontal cement pack was placed. Use of analgesic for 48 hours was prescribed, as well as 0.12% chlorhexidine rinses. Due to allergic reactions these rinses had to be discontinued after five days due to onset of ulcerative lesions at the level of attached gingiva.
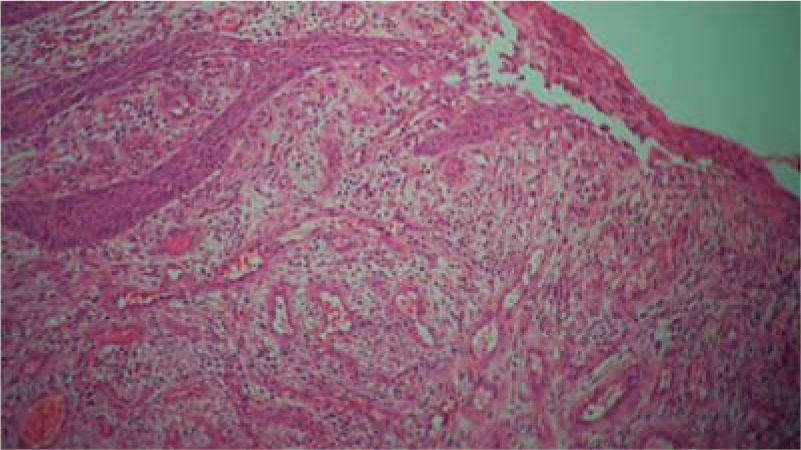
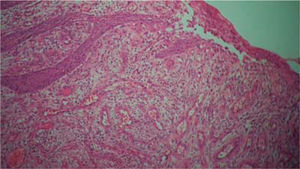
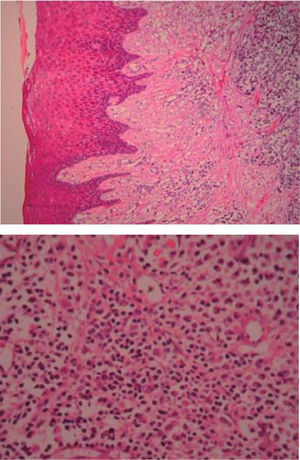
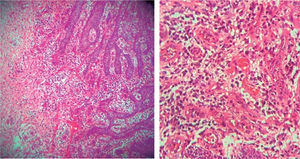
Histopathological examination: the sample was composed of acanthic epithelium, showing pseudoepitheliomatous hyperplasia, lamina propria, vascular canals coated with endothelial cells, inflammatory infiltrate composed of lymphocytes, plasma cells, histiocytes and occasional polymorphonuclear cells (Figure 6). Clinical diagnosis was confirmed with these findings.
Controls: lesion volume decreased after a week, nevertheless, the area still exhibited a reddish hue, therefore, it was kept under observation (Figure 7). Two weeks later, a slight volume increase with whitish and reddish hue was observed, thus a relapse was suspected. At the third week decrease of tissue volume was observed without any presence of inflammatory signs.
During a seven month follow-up suitable oral hygiene level was observed, no lesion relapse was observed (Figure 8).
Case 2A 37 year old female patient sought consultation at the Periodontics Masters Clinic of the San Martin de Porres University. The patient informed of a growing and bleeding gingival lesion which had its onset during the second trimester of her pregnancy and was persisting for nine months after pregnancy completion.
Clinical examination revealed an inflammatory gingival lesion at the site of teeth 1.1 and 2.1. The lesion measured 9 x 9 mm approximately and covered one third of the clinical crown; the lesion was asymptomatic, firm, lobulated, of rugged texture, bleeding upon stimulus (Figure 9). Periodontal evaluation did not reveal periodontal pockets, nevertheless, presence of plaque was observed; oral hygiene index of 50% (O’Leary) was obtained.
Radiographic examination revealed bone crest alteration between teeth 1.1 and 2.1 (Figure 10).
Presumptive diagnosis: pyogenic granuloma.
Treatment: fist session devoted to oral hygiene instruction followed by excisional biopsy of the lesion and gingivoplasty (Figures 11and12).
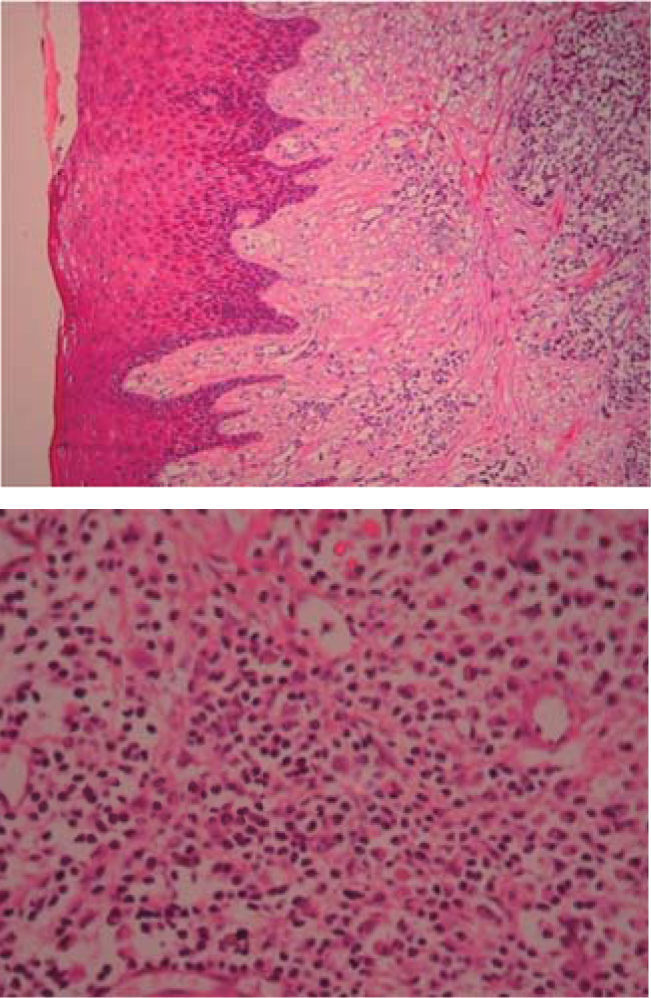
Histopathological examination: sample composed of acanthic epithelium, pseudoepitheliomatous hyperplasia, lamina propria, vascular canals coated with endothelial cells, inflammatory infiltrate composed of lymphocytes, plasma cells, histiocytes and occasional nuclear polymorphs. These findings confirmed clinical diagnosis (Figures 13 and 14).
(HE 5x) Acanthic epithelium, pseudoerpithelimatous hyperplasia, lamina propria, apparent vascular canals and inflammatory infiltrate. (HE 10x) Vascular canals coated with endothelia cells, inflammatory infiltrate composed of lymphocytes, plasma cells, histiocytes and occasional nuclear polymorphs.
Control: lesion volume decreased after one week, nevertheless, a reddish hue persisted in the area, therefore patient was maintained in observation. After six months, patient exhibited relapse of lesser intensity (7 x 7 mm) (Figure 15). Dental plaque was equally observed, obtained oral hygiene index (O‘Leary) was 52%. An additional oral hygiene instruction session was conducted, with plaque removal and a second lesion excision. During this procedure, a greater margin of apparently healthy tissue was removed, reaching removal of periosteum adjacent to the lesion.
Favorable evolution was observed in the next controls, oral hygiene levels were more satisfactory, lesion did not relapse up to a seven month follow up period (Figure 16).
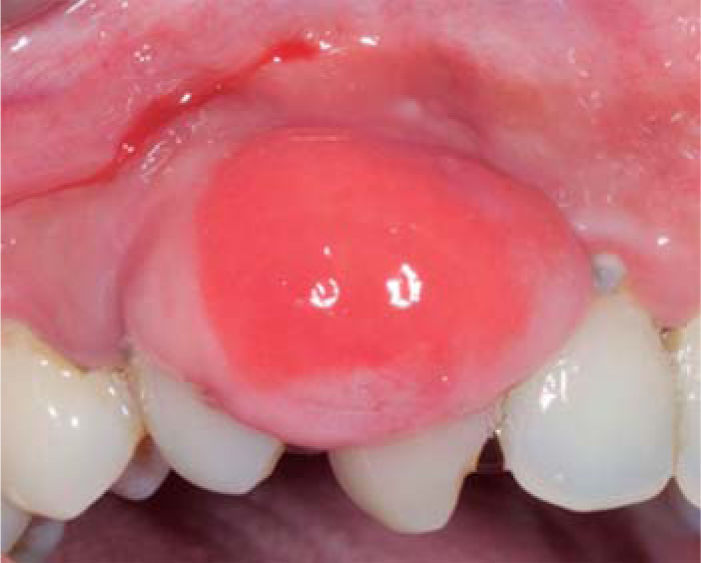
Case 3A systemically healthy, 29 year old female sought consultation due to a three year old gingival lesion located at the anterior sector of the upper jaw. Patient reported lesion onset during her pregnancy, and progressive lesion growth without presence of pain. Clinical evaluation revealed a soft, mobile, pedicled tumor, approximately measuring 20 x 16 mm located at the level of teeth 23 and 24. The tumor was of a pinkish hue and exhibited keratinization foci (Figure 17). Periodontal assessment revealed periodontal pockets and a 78% oral hygiene index (O’Leary). Radiographic examination showed interproximal calculus in the gingival lesion area (Figure 18).
Presumptive diagnosis: pyogenic granuloma.
Treatment: oral hygiene instruction was administered, followed by root scaling and planing, after which an excisional biopsy of the lesion was conducted (Figure 19) as well as a gingivoplasty procedure. Moreover, support periodontal therapy was recommended with periodontal maintenance sessions every three months during the first year.
Histopathological examination: the sample exhibited pseudoepitheliomatous hyperplasia, lamina propria, vascular canals coated with endothelial cells, inflammatory infiltrate composed of lymphocytes, plasma cells, histiocytes and occasional nuclear polimorphs. These findings confirmed clinical diagnosis.
Controls: decrease of inflammatory circumstances of the wound area was observed after one week (Figure 20). Favorable evolution was observed in the following controls, more suitable oral hygiene levels were observed as well as lack of lesion recurrence, up to a six month follow-up period.
Case 4A 46 year old female patient sought consultation due to a gingival lesion located at the level of teeth 1.3 and 1.4. The patient informed she was not under any drug or hormonal regimen.
Clinical examination revealed an inflammatory gingival lesion around teeth 1.3 and 1.5, measuring 9 x 9 mm approximately and covering a third of the clinical crown. The lesion was asymptomatic, firm, lobulated, smooth and bleeding on stimulus (Figures 21and22).
Periodontal evaluation revealed presence of plaque and calculus, as well as a 50% oral hygiene index (O’Leary). Patient exhibited a caries lesion in the distal aspect of tooth 1.3.
Presumptive diagnosis: pyogenic granuloma.
Treatment: oral hygiene instruction session and excisional biopsy with gingivoplasty (Figure 23).
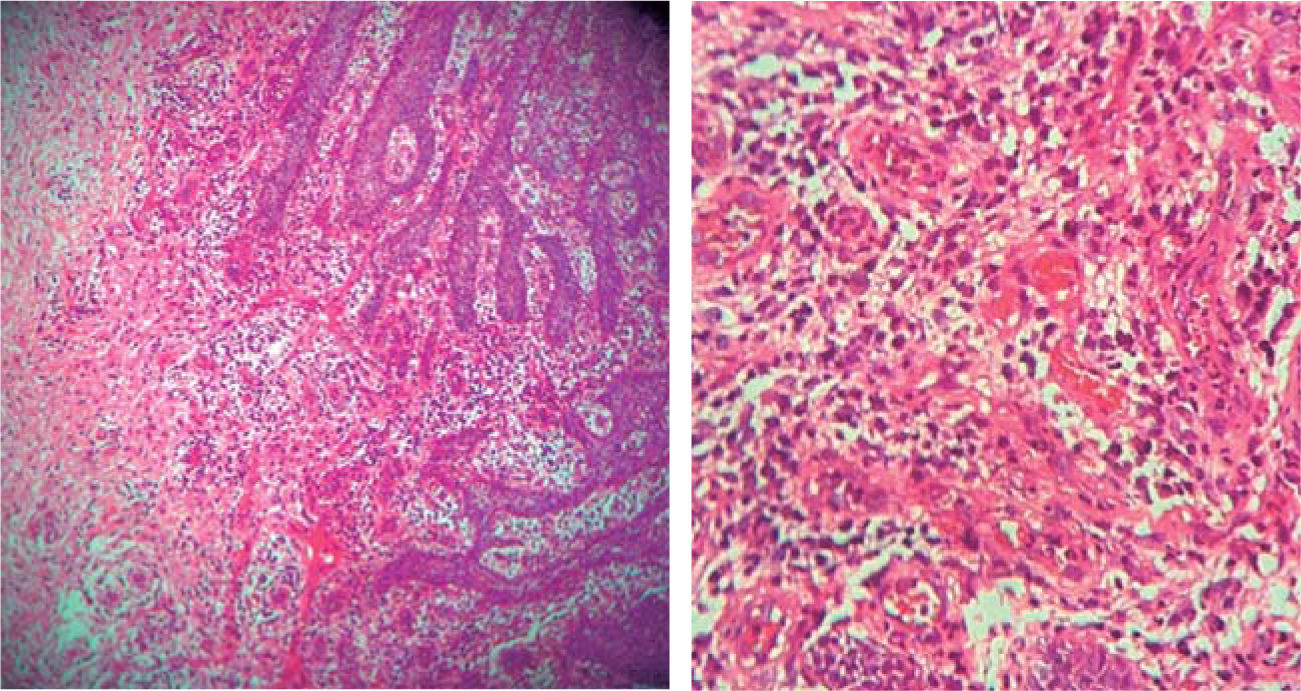
Histopathological examination: pseudoepitheliomatous hyperplasia and granulation tissue, vascular canals coated with endothelium and ingurgitation of erythrocytes, inflammatory infiltrate with neutrophil and histiocyte predominance (Figures 24 and 25).
Controls: a reddish hue in the area was observed after one week, compatible with healing process. Evolution was favorable, with better maintenance of oral hygiene levels, and with no lesion recurrence up to a six month follow-up period.
Case 5A systemically healthy 27 year old male patient sought consultation due to a gingival lesion located at the level of teeth 3.3 and 3.4. Patient informed of a non-contributory history.
Clinical examination revealed inflammatory gingival lesion approximately measuring 9 x 9 mm, partially covering the clinical crown's lingual and vestibular areas. The lesion was firm, smooth and lobulated (Figures 26and27). Periodontal evaluation revealed presence of plaque and calculi, as well as a 40% (O’Leary) oral hygiene index.
Treatment: oral hygiene instruction and excisional biopsy with gingivoplasty.
Histopathological examination: acanthic epithelium, showing pseudoepitheliomatous hyperplasia, lamina propria, vascular canal coated with endothelial cells, inflammatory infiltrate composed of lymphocytes, plasma cells, histiocytes and occasional nuclear polymorphs.
Controls: suitable evolution and healing wound were observed after one week. Five months later, no lesion recurrence was observed.
DiscussionPyogenic granuloma is an inflammatory hyperplasia formed as a result of an exaggerated reaction of connective tissue to some localized minor lesion or any underlying irritation. Irritation factors can be dental calculi, poor oral hygiene, some unspecified infection as well as over contoured restorations.1,5–11 Caused by this irritation, underlying fibro-vascular connective tissue becomes hyperplastic and there is proliferation of granulation tissue, which leads to the formation of pyogenic granuloma.1,4 In order to determine pyogenic granuloma diagnosis, some factors such as hormonal changes during puberty or pregnancy, administration of certain drugs and some kinds of trauma1,4,5 should be contemplated.
In the present case report, presence of pyogenic granuloma has been described in relation to pregnancy, local factors such as absence of interproximal contact, presence of calculi and poor oral hygiene indexes.
From a histological point of view there are two kinds of pyogenic granuloma: the first is characterized by proliferating capillaries which organize in lobes. This type of PG is called lobular capillar hemangioma (LCH). The second type (non LCH) consists of vascular proliferation resembling granulation tissue. When compared to central area of non-LCH, LCH lobular area contains great amounts of small diameter capillaries. Descsribed differences suggest that these two histological types represent different entities.1,6–12 Microscope examination of pyogenic granuloma reveals great vascular proliferation resembling granulation tissue, tissue formed by endothelial fibrotic stroma can be seen, with abundant capillaries coated with thick endothelial cells. Stratified epithelium can be hyperplastic, thinned down or ulcerated. Purulent exudate, which confers its name to this type of lesion, is not always present.11
With respect to treatment, Powell described use of Nd YAG laser to excise this lesion, since lesser bleeding risks are incurred upon when comparing it with other surgical techniques.1
Verma et al6 reported use of a flash lamp pumped pulsed dye laser in a mass of granulation tissue which had not responded to conventional treatments; they reached the conclusion that tissue responded favorably. Tay et al13 after a three year follow up of a treatment conducted with flash lamp pumped pulsed dye laser reported 0% relapse after conducting treatment in one session for 25% of patients, two sessions 40%, three sessions 30% and six sessions 5%.
Ishida and Ramos-Silva14 described cryosurgery as a very useful technique for pyogenic granuloma treatment; they reported that oral mucosa, due to its softness and dampness, is an ideal site for this technique. On the other hand, Ghodsi15 compared treatment which conducted surgical excision, performed in one session, and exhibiting 0% relapse, with cryosurgery, conducted in one session for 63% of all patients, two sessions for 32% of all patients and three sessions for 5% of all patients, exhibiting 0% relapse. Matsumoto et al16 found 0% relapse when they conducted treatment with monoethanolamine oleate used as sclerosing substance in one session.
Nevertheless, up to the present moment, most reports suggest use of surgical excision as treatment of choice. After lesion excision, it is recommended to perform curettage of underlying tissue, performing an excision with 2 mm margins in the periphery and at a depth that will include periosteum. Moreover, any foreign body, calculus or restoration that might be associated to onset of pyogenic granuloma must be removed.1,2,5,6,11
Al Khaleeb et al3 after a 12 year follow up, reported 5.8% of cases with relapse when conducting treatment of surgical excision with periosteum removal and even performing adjacent bone tissue curettage. This technique implies second intention healing, therefore use of a pack such as a surgical-cement pack is indicated.17,18
Due to all the reasons hereby provided, it can be recommended that, to reach accurate diagnosis it is important to observe clinical signs as well as ascertain detailed clinical history of the patient's systemic circumstances, as well as of local factors which might stimulate overblown tissue response and subsequent formation of pyogenic granuloma. Clinical diagnosis must always be confirmed with histological examination. According to what was observed in the present case series, one of the most important contributing factors to be considered was the oral hygiene index, therefore, physiotherapy must be considered the first step in pyogenic granuloma treatment. Moreover, in these cases it would be advisable for patients to receive supporting periodontal therapy.
It has equally been observed that different studies have evaluated different treatment techniques with high success and low relapse percentages; these techniques are, cryosurgery, flash lamp pumped pulsed dye laser, as well as conventional surgical excision. Nevertheless, it must be taken into account that surgical excision can be performed in one single session with basic surgical instruments, as opposed to other techniques which require several sessions as well as specific training and equipment. This technique can be easily applied in daily clinical practice, providing thus greater comfort to the patient.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam