To perform anthropometric assessment of patients with quadriplegic, chronic non-progressive encephalopathy, comparing two distinct references of nutritional classification and to compare the estimated height to the length measured by stadiometer.
MethodCross-sectional study including 0-3-year children with quadriplegic chronic non-progressive encephalopathy in secondary public hospital. Length, weight, arm circumference, triceps skinfold and knee height were measured. The arm muscle circumference and estimated height were calculated. The following relations were evaluated: weight-for-age, length-for-age and weight-for-length, using as reference the charts of the World Health Organization (WHO) and those proposed by Krick et al.
ResultsFourteen children with a mean age of 21 months were evaluated. Assessment of anthropometric indicators showed significant difference between the two classification methods to assess nutritional indicators length/age (p=0.014), weight/age (p=0.014) and weight/length (p=0.001). There was significant correlation between measured length and estimated height (r=0.796, p=0.001). Evaluation of arm circumference and triceps skinfold showed that most patients presented some degree of malnutrition. According to arm muscle circumference, most were eutrophic.
ConclusionsSpecific curves for children with chronic non-progressive encephalopathy appear to underestimate malnutrition when one takes into account indicators involving weight. Curves developed for healthy children can be a good option for clinical practice and weight-for-length indicator and body composition measurements should be considered as complementary tools.
Realizar a avaliação antropométrica de pacientes com encefalopatia crônica não progressiva quadriplégica, usando referências distintas de classificação do estado nutricional, e comparar a altura estimada com o comprimento mensurado por antropômetro.
MétodosEstudo transversal descritivo, incluindo crianças com encefalopatia crônica não progressiva quadriplégica de 0-3 anos em hospital público secundário. Foram aferidos comprimento, peso, circunferência do braço, prega cutânea tricipital e altura do joelho. Foram calculadas a circunferência muscular do braço e a estimativa da altura. Foram avaliadas as relações peso/idade, comprimento/idade e peso/comprimento, utilizando como referência os gráficos da Organização Mundial de Saúde e os propostos por Krick et al.
ResultadosForam avaliadas 14 crianças com idade média de 21 meses. A avaliação dos indicadores antropométricos mostrou diferença significativa entre os dois métodos de classificação nutricional ao avaliar os indicadores comprimento/idade (p=0,014), peso/idade (p=0,014) e peso/comprimento (p=0,001). Houve correlação significativa entre comprimento mensurado e estatura estimada (r=0,796; p=0,001). A avaliação da circunferência do braço e prega cutânea tricipital mostrou que a maioria dos pacientes apresentava algum grau de desnutrição, mas, de acordo com a medida da circunferência muscular do braço, a maioria estava eutrófica.
ConclusõesCurvas específicas para crianças com encefalopatia parecem subestimar a desnutrição, quando se leva em consideração indicadores que envolvem peso. Curvas elaboradas para crianças hígidas podem ser boa opção para prática clínica, devendo-se considerar indicador peso/estatura e as medidas de composição corporal como ferramentas complementares.
Anthropometrics is used to assess nutritional status, as it is a simple, noninvasive technique with no additional costs. It is, therefore, the tool of choice to assess dimorphism in children.1 It becomes difficult to employ anthropometric methods developed for the general pediatric population in patients with non-progressive chronic encephalopathy (NPCE) due to postural alterations (some children are unable to remain in the standing position, have contractures, scoliosis, and involuntary muscle spasms) and little cooperation (cognitive impairment).2 Although the problem of measurement can be attenuated with the use of alternative measures, the main problem remains the reference standard.3
Some methods have been validated to measure body composition, such as the doubly-labeled water technique (DEXA), hydrostatic weighing, and bioelectrical impedance. However, these methods may not be feasible in clinical follow-up. Clinicians often use a variety of anthropometric measurements to estimate adiposity, but the applicability of such measures in the prediction of body fat percentage in these children is unclear.4
Specific growth references for children with NPCE should facilitate a uniform assessment of growth and nutritional status and simplify the comparative interpretation of growth data.5 Moreover, as it is an extremely heterogeneous condition, the use of growth charts for NPCE as a reference standard may not be very accurate.6
Currently, the Brazilian Food and Nutrition Surveillance System (Sistema de Vigilância Alimentar e Nutricional – SISVAN)7 recommends that the classification to be used in healthy children should be performed using the growth curves of the World Health Organization (WHO).8 A classification method using the curves developed by Krick et al5 is specific for patients with quadriplegic NPCE aged 0 to 120 months according to: weight/age, height/age, and weight/height. Nutritional assessment becomes crucial, not only because it allows identifying and monitoring cases or possible cases of malnutrition, common in neurologically impaired individuals, but it also allows the adoption of measures to minimize the process through proposals of adequate and individualized dietary counseling and monitoring of the nutritional status, aiming to achieve appropriate body size.9
The aim of the study was to perform the anthropometric assessment of patients with quadriplegic NPCE using two different nutritional classification references, to assess the nutritional classification according to measures of the arm circumference (AC), arm muscle circumference (AMC), and triceps skinfold thickness (TSF), and to compare the estimated height through the formula proposed by Stevenson with the length measured in a stadiometer.
MethodsThis is a cross-sectional descriptive study carried out at the Instituto Nacional da Saúde da Mulher, da Criança e do Adolescente Fernandes Figueira in Rio de Janeiro, RJ, Brazil. All children with quadriplegic NPCE aged 0 to 3 years and 11 months, treated and followed at the Motor Physical Therapy Outpatient Clinic at the hospital during the month of September of 2012 that met the criteria were included in the study. The one-month collection period is justified by the fact that new patients are not accepted at the clinic due to a full schedule, and this time interval is enough to collect data from all patients who meet the inclusion criteria. Patients with a diagnosis confirmed by a neurologist, whose parents/guardians signed an informed consent form were included, whereas children with some type of associated genetic syndrome were excluded.
Of the total of 20 children with quadriplegic NPCE treated at the clinic, 14 met the study inclusion criteria. Anthropometric data were collected on the same day of physical therapy care and recorded in a specific protocol. The assessment of social class was adapted from that of the Brazilian Association of Research Companies (Associação Brasileira de Empresas de Pesquisa – ABEP), in which families are pertinently classified as social classes: A, B, C, D, and E.
Anthropometric assessment was performed by measuring the following parameters: length, using a horizontal anthropometer 110 cm long and with a 0.1 cm precision; weight, in a digital Filizola® scale (Filizola, São Paulo, Brazil) used to weigh babies, with a maximum capacity of 15 kg and 10 g of variation for children younger than 2 years, and a platform-type Filizola® mechanical scale (Filizola, São Paulo, Brazil) with a maximum capacity of 150 kg and variation 0.1 kg by calculating the weight difference between the child and the caregiver for children older than 2 years; AC, with an inextensible millimeter tape, graduated every 0.5 cm; TSF, using a Lange® skinfold caliper (Power Systems, Inc., Tennessee, USA) with a precision of 1 mm; and knee height (KH), measured with an inextensible millimeter tape with a variation of 0.5 cm, corresponding to the distance between the knee and the ankle.
All these measurements were performed in duplicate and the mean of two measurements was considered for the analysis. Based on these measurements, the AMC and the estimated height by the KH were calculated. The length measured by the stadiometer was compared to the estimated height by the KH, according to the formula proposed by Stevenson et al.10
The weight for age (W/A), length for age (L/A), and weight for length (W/L) ratios were assessed using the World Health Organization (WHO) charts8 and those proposed by Krick et al5 as reference. Classification of nutritional status was performed by AC, AMC, and TSF, using as reference the values proposed by Frisancho11, for children older than 1 year, and by Jelliffe12 for those younger than 1 year.
All procedures performed in this study were approved by the Research Ethics Committee of the institution, under protocol number: 03375512.2.0000.5269.
For data analysis, measures of central tendency and dispersion were calculated, using the chi-squared test to evaluate the association between categorical variables. Spearman's coefficient was used to evaluate associations between measured height and estimated height. A p-value <0.05 was considered significant. The database and statistical analyses were performed using SPSS for Windows software, release 17 (SPSS Inc., Chicago, USA).
ResultsA total of 14 children with quadriplegic NPCE were included. Age ranged from 8 to 45 months, with a mean of 21 ± 11 months, and 79% were males. Social class C was the most frequent (85%), and the same frequency was observed for classes B and D (8%). None of the patients was classified as belonging to classes A and E. Of the studied children, most had received prior nutritional counseling (64%), and 56% had been advised by nutritionists. Most patients had been hospitalized once since birth (36%). Only 29% had a history of repetitive pneumonia and 21% were fed through gastrostomy.
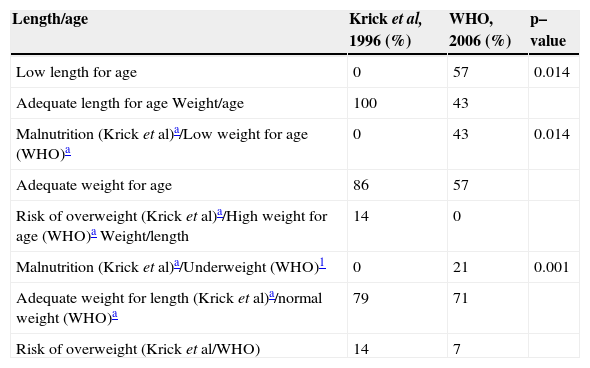
The evaluation of anthropometric indicators based on nutritional classification methods proposed by Krick et al5 and the WHO8 regarding the L/A showed that, according to the specific reference for patients with NPCE,5 all patients had adequate L/A. When assessed by WHO8 standards, it was observed that the majority (57%) had short L/A. Statistical analysis showed a significant difference (p=0.014) between the two methods used for L/A assessment (Table 1).
Classification of nutritional status according to the length/age, weight/age, and weight/length indicators (Rio de Janeiro, Brazil, 2012)
| Length/age | Krick et al, 1996 (%) | WHO, 2006 (%) | p–value |
|---|---|---|---|
| Low length for age | 0 | 57 | 0.014 |
| Adequate length for age Weight/age | 100 | 43 | |
| Malnutrition (Krick et al)a/Low weight for age (WHO)a | 0 | 43 | 0.014 |
| Adequate weight for age | 86 | 57 | |
| Risk of overweight (Krick et al)a/High weight for age (WHO)a Weight/length | 14 | 0 | |
| Malnutrition (Krick et al)a/Underweight (WHO)1 | 0 | 21 | 0.001 |
| Adequate weight for length (Krick et al)a/normal weight (WHO)a | 79 | 71 | |
| Risk of overweight (Krick et al/WHO) | 14 | 7 |
Regarding W/A, when assessing the curves by Krick et al,5 it was observed that the majority had adequate W/A (86%), 14% were classified as at risk for overweight, and no child was classified as malnourished. When using the WHO curves,8 it was also observed that the majority had adequate W/A (57%). However, 43% of patients showed low W/A and none had high W/A. A statistical difference was observed between the two methods of assessment (p=0.014; Table 1).
In assessing W/L, it was observed that, when using Krick et al's reference,5 no patient had malnutrition, 79% had normal W/L, and 14% were at risk of overweight. When using the WHO curves,12 21% of the patients were underweight, 71% had normal weight, 7% were at risk of overweight, and none showed overweight or obesity. Significant differences were observed regarding the classification of nutritional status, using the W/L index between the references by Krick et al5 and WHO8 (p=0.001; Table 1).
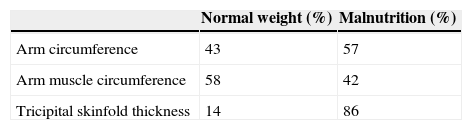
The classification of nutritional status, obtained by AC, demonstrated that most patients (57%) had some degree of malnutrition. The AMC showed that 58% of the patients had normal weight and the assessment by TSF showed that most patients (86%) were malnourished (Table 2). It was not possible to associate the circumference and skinfold assessments to the other anthropometric indicators (H/A, W/A, and W/L), due to the small sample size.
Regarding the evaluation of length, a significant correlation was demonstrated between the measured length by stadiometer and the estimated height from KH (r=0.796, p=0.001).
DiscussionThe health management of children with NPCE requires nutritional assessment as growth disorders and nutritional deficits are present in approximately one third of these pediatric patients.13 For this purpose, a variety of methods, parameters, and classifications have been suggested, leading to results and interpretations at different clinical levels, making it difficult to collect data and perform meta-analyses.14
The evaluation of L/A in this study demonstrated that, according to the reference by Krick et al, no child had length deficit, whereas according to the classification of the WHO, the majority had short L/A. There are several reasons why children with NPCE are shorter than their healthy peers of the same age. Shapiro et al15 observed that isolated nutritional factors are not responsible for the delay in linear growth observed in this population. It is suggested that non-nutritional factors and disease severity have a remarkable influence on the growth of children with NPCE.5
According to Stallings et al16 in children with severe cerebral palsy, linear growth is reduced to lower than the third percentile, considering growth curves for healthy children. This reduction in linear growth can occur due to factors related to the brain injury itself.17 Children with NPCE grow and develop, but at a slower pace. However, their development is not only delayed, but disorderly and impaired as a result of the brain injury.18 Moreover, chronic malnutrition or other nutritional deficiencies can impair proper growth and development.9,19
The W/A index evaluated in this study showed that according to the curve by Krick et al, the majority had adequate W/A and none was classified as malnourished. According to the classification by the WHO curves, 43% were underweight for age. Regarding the W/L, it was observed that no patient had malnutrition according to the curves by Krick et al, and that most had adequate W/L.
When evaluating the WHO reference, it was observed that 21% were underweight, most had normal weight, and no patient was overweight or obese. It must be considered that growth and weight gain in these children often differ from those of healthy children of the same age. However, this study demonstrated that, even when considering the curve created for healthy children, most had adequate W/A and weight for height, showing that it is possible to attain this condition despite the diagnosis of NPCE. Since a high percentage of children with a nutritional diagnosis of low W/A according to the WHO was observed, it is suggested that the curve by Krick et al may underestimate low weight.
The ideal weight for this population is estimated at the 10th percentile of weight for height in the curves developed for healthy children, allowing for adequate body fat and muscle reserves.5 Since the W/L index assesses the child's association with him/herself, regardless of age, the findings of this study suggest that the reference by Krick et al may underestimate malnutrition in these patients and overestimate the risk of overweight. Krick et al5 suggest that the specific curves are used together with the growth curves for healthy patients, and that the 50th percentile of W/L, according to the reference for NPCE, should be considered the target.
Tomoum et al6 reported a low percentage of malnutrition using the specific reference standards for children with quadriplegic NPCE. Recent data suggest that these references seem to mask patients' malnutrition and their needs; therefore they are not considered the preferred method to be used.14 In fact, another study of children with quadriplegic NPCE, using the WHO reference, demonstrated that 92% of the assessed children were malnourished.20
As it was observed, there are differences regarding the type of growth chart to be used and the cutoff points, which result in different prevalence rates according to the method chosen for assessing nutritional status. This fact was reinforced by the present study, as statistical differences were observed when comparing the two growth curves on all indicators evaluated, suggesting that the nutritional diagnosis of these patients also depends on the type of reference used.
The arm anthropometry describes body composition in relation to weight and should be used to provide additional data when analyzing growth.5 The use of AC as an index of protein stores is well recognized.21 The current study demonstrated that most patients have malnutrition, when taking into account the evaluation of the AC. This evaluation should be considered, given that, according to Sullivan et al,22 weight and measurement of AC are easy to obtain and both are good indicators of nutritional status in children with NPCE.
Studies show a reduction in fat-free mass in patients with NPCE due to impaired linear growth, muscle mass depletion and atrophy.6,23,24 The present study, when assessing the fat-free mass by AMC, found different results from those reported in the literature, as most patients had a nutritional classification of normal weight, evidencing that the lean body mass of the assessed patients was still preserved.
The TSF is used in the determination of body fat and also allows for the assessment of nutritional status. This appears to be the simplest and most practical method available to determine both subcutaneous and total body fat.6 One study demonstrated that the measurement of triceps skinfold has sensitivity and specificity to predict malnutrition.4
According to Samson-Fang and Stevenson,25 TSF can be considered the best screening tool for the diagnosis of malnutrition in children with NPCE. The present study demonstrated that most patients were malnourished when evaluated by this method. Similar results were reported by other studies.4,25 Rieken et al25 showed that children with CP have less subcutaneous fat and more intra-abdominal fat. Another case-control study demonstrated that fat mass is significantly lower in the group with NPCE than in the control group. Fat mass was positively correlated with weight and body mass index in both groups.18
As it was observed in the present study, many children had adipose compartment impairment. Since the assessment of the TSF has been reported in the literature for patients with NPCE, it appears that the results can adequately reflect the nutritional status of the analyzed patients.
The literature review retrieved four studies that investigated the validity of skinfold measurement and bioelectrical impedance analysis in children with severe NPCE in comparison with other methods, such as DXA and isotope dilution. Although most studies have reported a favorable ratio for such measures, these conclusions are hampered by small and heterogeneous samples and the lack of methodological quality. Therefore, the validity of skinfold measurements and bioelectrical impedance analysis in children with NPCE needs a more robust evaluation.26
In the present study, data from the nutritional diagnosis by body composition were closer to the results found when using the WHO curves. However, the small number of cases assessed did not allow for the analysis of the correlation between body composition data and the evaluated curves.
Regarding the measurement of height, there is a difficulty due to the presence of skeletal contractures and the incapacity of most patients to stand up.18 Stevenson et al10 developed formulas to estimate height by segmental measures; the length from knee to ankle (KH) is the most appropriate, using the following equation: estimated height= (KHx2.69)+24.2. In the current study, as the patients were not capable of standing up unaided, which was also related to the young age range included in the study, it was not possible to measure the height, but length was measured in all patients, as well as the KH, allowing for the application of the equation proposed by Stevenson et al.10
Statistical analysis evidenced a positive correlation between these two measures, suggesting that the use of both is safe for nutritional monitoring. This result is corroborated by the study by Linhares,27 which demonstrated that the anthropometric method described by Stevenson et al10 allows for a better nutritional monitoring of children with NPCE.
Regarding the comparison of the two methods of nutritional status classification of children with NPCE proposed by the current study, statistical differences between the growth curves were observed. It should be noted that the specific curve for children with encephalopathy is limited to the age of 10 years, which restricts its use. Moreover, the specific curves appear to underestimate malnutrition when indices involving weight and body composition are considered.
Therefore, it is suggested that the curves created for healthy children can be a good option for clinical practice, considering the W/H index and, when evaluating the height/age index, the stunting that occurs in most of these patients should be taken into account. The association of measures of body composition, whenever possible, is also recommended as complementary tools. Regarding the measurement of height/length, it was observed that, when it is not possible to perform the actual measurement, the estimation of stature is a safe method. At any rate, each child must be evaluated individually, and the follow-up needs to be constant, in order to preserve the nutritional status.
The small sample size constituted a limitation of the present study, as it reflects the specificity of the assessed encephalopathy (quadriplegic), the fact that only outpatients were selected (considering that hospitalization can influence the nutritional status), the short follow-up period, and the reality of the center where the study was conducted, which does not have the facilities to treat a large number of patients.
Further studies, preferably multicenter with larger sample sizes, are necessary in order to establish recommendations for this population. Furthermore, it should be emphasized that the study was conducted in a referral hospital, in which patient care is performed by a multidisciplinary team.
The fact that most of the study population had normal weight, regardless of the evaluation method, demonstrates that a multidisciplinary follow-up can optimize the growth and development of these children, despite all the limitations associated with encephalopathy. Therefore, it is recommended that multidisciplinary care of these patients is implemented as early as possible, in order to prevent deficiencies and disorders that may directly interfere with their development, as well as with family routine and social life.
Conflicts of interestThe authors declare no conflicts of interest.