To identify the association between both, body mass index and aerobic fitness, with cardiovascular disease risk factors in children.
MethodsCross-sectional study, carried out in Itaúna-MG, in 2010, with 290 school children ranging from 6 to 10 years-old of both sexes, randomly selected. Children from schools located in the countryside and those with medical restrctions for physical activity were not included. Blood sample was collected after a 12-hour fasting period. Blood pressure, stature and weight were evaluated in accordance with international standards. The following were considered as cardiovascular risk factors: high blood pressure, high total cholesterol, LDL, triglycerides and insulin levels, and low HDL. The statistical analysis included the Spearman's coefficient and the logistic regression, with cardiovascular risk factors as dependent variables.
ResultsSignificant correlations were found, in both sexes, among body mass index and aerobic fitness with most of the cardiovascular risk factors. Children of both sexes with body mass index in the fourth quartile demonstrated increased chances of having high blood insulin and clustering cardiovascular risk factors. Moreover, girls with aerobic fitness in the first quartile also demonstrated increased chances of having high blood insulin and clustering cardiovascular risk factors.
ConclusionThe significant associations and the increased chances of having cardiovascular risk factors in children with less aerobic fitness and higher levels of body mass index justify the use of these variables for health monitoring in Pediatrics.
Identificar a associação do índice de massa corporal e aptidão física aeróbica com fatores de risco de doenças cardiovasculares em crianças.
MétodosEstudo transversal realizado na cidade de Itaúna-MG no ano de 2010 com 290 escolares de 6 a 10 anos de ambos os sexos, aleatoriamente selecionados. Crianças de escolas da zona rural e aquelas com limitações médicas para prática de atividade física não foram incluídas. Coletou-se o sangue após jejum de 12 horas. A pressão arterial, a estatura e o peso foram avaliados segundo padrões internacionais. Foram considerados fatores de risco cardiovascular: hipertensão arterial, colesterol total, LDL, triacilgliceróis e insulinemia elevados e HDL baixo. A análise estatística incluiu a Correlação de Spearman e a Regressão Logística, com os fatores de risco cardiovascular como variáveis dependentes.
ResultadosCorrelações significativas foram encontradas, nos dois sexos, entre índice de massa corporal e aptidão física aeróbica com a maioria dos fatores de risco cardiovascular. Crianças dos dois sexos com índice de massa corporal acima do percentil 75 apresentaram chances aumentadas para insulinemia alterada e agrupamento de fatores de risco cardiovascular. Meninas com aptidão física aeróbica no primeiro quartil apresentaram chances aumentadas para insulinemia alterada e agrupamento de fatores de risco cardiovascular.
ConclusãoAs associações significativas e as chances aumentadas para presença de fatores de risco cardiovascular em crianças com menor aptidão física aeróbica e maior índice de massa corporal justificam o uso dessas variáveis no monitoramento da saúde em pediatria.
Diseases of the circulatory system have been the leading cause of death among the adult population over the last 30 years in Brazil.1 Cardiovascular diseases (CVD) are caused by the association between genetic and behavioral risk factors, and may originate in childhood.2–4 Among the major risk factors for CVD are hereditary factors, obesity, smoking, physical inactivity, dyslipidemia, hypertension, diabetes, insulin, and gender.5,6 The control of modifiable risk factors should begin in childhood, aiming to decrease cardiovascular morbidity and mortality in adulthood.7
For the diagnosis of overweight and obesity, the body mass index (BMI) is considered a good indicator of overall adiposity, as it is associated with subcutaneous fat.6 Both BMI and other measures of adiposity are related to aerobic fitness in children.8 Aerobic fitness is inversely associated with CVD risk factors in children and adults.9–11 Even among overweight or obese children, better aerobic fitness appears to have a protective effect on CVD risk factors.11
The associations between anthropometric variables, aerobic fitness, and CVD risk factors lack cross-sectional and longitudinal studies in Brazilian children, aiming to better understand their magnitude and mechanisms. Therefore, this study aimed to identify the association of BMI and aerobic fitness with CVD risk in children aged 6 to 10 years.
MethodsThe study population consisted of schoolchildren aged 6 to 10 years enrolled from first to fifth grade in public schools in the urban area of Itaúna, state of Minas Gerais, Brazil. A total of 4,649 students were assessed. To determine the minimum sample size, a survey (pilot study) was conducted with 25 students aged 6 to 10 years of both genders, in whom the variables systolic blood pressure (SBP), diastolic blood pressure (DBP), high-density lipoprotein (HDL) cholesterol (mg/dL), low-density lipoprotein (LDL) cholesterol (mg/dL), total cholesterol (mg/dL), triglycerides (mg/dL), and insulin (µIU/mL) were measured, and their respective means and standard deviations were obtained. A maximum tolerance error was established for estimating the population mean for each variable that did not compromise result reliability.
To calculate the minimum sample size for each variable, the respective sample's standard deviation was used as a population estimate at a significance level of 5%. Thus, it was decided to presuppose the maximum sample size as between the minimum obtained values, resulting in 228 individuals related to the variable insulinemia, which, in turn, was limiting for the sampling, as it showed the highest variability. Therefore, the sample size was set at 228 students as the minimum to meet the margin of error in population measurements for all variables of interest. However, after estimating a loss of 50%, the final sample consisted of 456 children. Stratification by gender and age was performed in each school so that the proportion of age and gender was maintained. With the data obtained in each school, students were numbered in each series in sequence. Then, using a table of random numbers generated by Excel 2003 (Microsoft Corporation, Washington- USA), the corresponding number of children was selected in the list created in each series, until the number necessary to constitute the sample for that age and gender at each school was reached.
Inclusion criteria were children aged between 6 and 10 years, enrolled in state or municipal schools from the first to the fifth grade. Exclusion criteria were clinical and/or motor limitations to undergo the physical testing and enrollment in rural schools, which represented 6% of students in the municipality.
Children were included only after their parents or guardians agreed to their participation by signing the informed consent. The project was approved by the Departmental Board of Pediatrics of Faculdade de Medicina da UFMG (Edict No. 93/2009) and by the Research Ethics Committees of UFMG (Edict No. 0040.0.203.000-10) and of Universidade de Itaúna (Edict 012/10).
Body mass was measured with children wearing light clothing, on a digital Seca electronic scale (Scales Galore, New York - USA), with maximum capacity of 150 kg and precision of 0.1 kg. The weight corresponding to clothing was not subtracted from the measured weight. Height was measured in an Alturaexata vertical stadiometer (Alturaexata, Minas Gerais - Brazil) calibrated in centimeters (cm) with precision of 0.001 m. Body weight and height were measured twice, and the mean value was considered. BMI was calculated using the ratio between total body mass in kilograms and height in meters squared.
Blood pressure was measured using an Onrom automatic blood pressure device, model HEM711 (Omron Healthcare, Illinois - USA), validated for use in children.12 Three measurements were performed on the right arm after at least 5 minutes of rest, with the child sitting with legs and arms in a relaxed position. There was a two-minute interval between each measurement, according to the recommendations of Anderssen et al.13 The mean value of the three measurements was considered for the analysis.
Aerobic fitness was assessed using the 20 m shuttle run test,14 which consists of running a distance of 20 m repeatedly, at a specified pace with progressive intensification until exhaustion. The pace was determined by a sound signal emitted by a CD player using the specific test CD. The distance was established on the gym floor or another area with paved floor available in the schools. The test starts at 8.5 km/h and increases by 0.5 km/h every minute until the child is unable to keep pace for two consecutive beeps. All children were verbally encouraged to achieve maximal test effort. For the calculation of maximum oxygen consumption (VO2 max) in mL.kg−1.min−1, the equation described by Leger and Gadoury15 was used: VO2 max = 31.025 + 3.238 (final test speed in km/h) - 3.248 (age in years) + 0.1536 (final speed × age).
After a 12-hour fast, 10 mL of blood were collected in disposable plastic syringes and divided into two tubes in equal amounts. The material was stored in a cooler at ambient temperature and taken to the laboratory within one hour, then immediately analyzed. One of the tubes containing fluoride anticoagulant was centrifuged at 5,000 rpm for 5 minutes to obtain plasma and perform fasting glucose measurement by the enzymatic method, with the LABTEST reagent (LABTEST, Minas Gerais - Brazil) in a Clinline 150 apparatus (Biomerieux – USA). Of the remaining 5 mL, after centrifugation at 5,000 rpm for 5 minutes, 500 µL of serum were taken for analysis of total cholesterol and fractionated by the enzymatic colorimetric method, as well as for the analysis of triglycerides by enzymatic-automated method, all carried out with the LABTEST reagents in a 150 Clinline device. A 1 mL volume of serum was used for insulinemia analysis by chemiluminescence immunoassay measuring μIU/mL, in an Immulite 2000 automated device (Immulite 2000 Automated Immunoassay Analyzer, Boston - USA).
The following were considered CVD risk factors in this study: altered values of the variables SBP, DBP, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, and insulin.
Due to the non-normal distribution of some variables, Spearman's correlation was used to assess the association of BMI and aerobic fitness with each of the CVD risk factors. The BMI z-score was previously calculated at each age for each gender and used to make the association with risk variables. Three or more factors present in the same child were considered for the clustering of risk factors.
The cutoffs used for the risk variables were: blood pressure and insulin levels > 80th percentile for age and gender, HDL-cholesterol < 45 mg/dL, and LDL-cholesterol, triglycerides, and blood glucose > 100 mg/dL.16 The logistic regression analysis estimated the odds ratio for arterial hypertension, low HDL, high LDL, high triglycerides, high insulin, and clustering of CVD risk factors in children above the 75th percentile and below the 75th percentile for BMI, and above and below the 25th percentile for aerobic fitness. Data were analyzed using the SPSS software for Windows, release 17.0 (SPSS Inc. Released 2008. SPSS Statistics for Windows, Chicago - USA). A probability level of p<0.05 was used to indicate statistical significance.
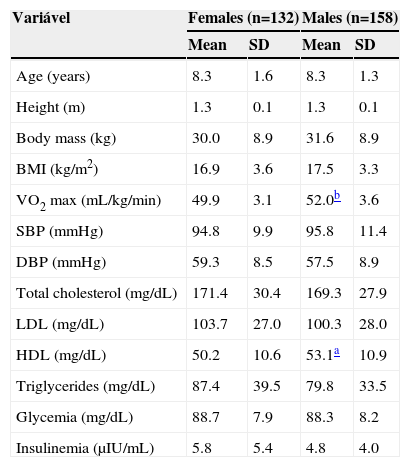
ResultsThe sample's descriptive characteristics are shown in Table 1. The intraclass correlation coefficient for the two measures of height and weight were, respectively, 0.997 and 1.0 (p<0.001). Regarding the socioeconomic status, the sample was classified as 0.7% in class B1, 9.7% in B2, 35.9% in C1, 35.2% in C2, 17.9% in D, and 0.7% in E.
Anthropometric characteristics and cardiovascular risk factors in males and females aged 6 to 10 years (n=290)
| Variável | Females (n=132) | Males (n=158) | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (years) | 8.3 | 1.6 | 8.3 | 1.3 |
| Height (m) | 1.3 | 0.1 | 1.3 | 0.1 |
| Body mass (kg) | 30.0 | 8.9 | 31.6 | 8.9 |
| BMI (kg/m2) | 16.9 | 3.6 | 17.5 | 3.3 |
| VO2 max (mL/kg/min) | 49.9 | 3.1 | 52.0b | 3.6 |
| SBP (mmHg) | 94.8 | 9.9 | 95.8 | 11.4 |
| DBP (mmHg) | 59.3 | 8.5 | 57.5 | 8.9 |
| Total cholesterol (mg/dL) | 171.4 | 30.4 | 169.3 | 27.9 |
| LDL (mg/dL) | 103.7 | 27.0 | 100.3 | 28.0 |
| HDL (mg/dL) | 50.2 | 10.6 | 53.1a | 10.9 |
| Triglycerides (mg/dL) | 87.4 | 39.5 | 79.8 | 33.5 |
| Glycemia (mg/dL) | 88.7 | 7.9 | 88.3 | 8.2 |
| Insulinemia (μIU/mL) | 5.8 | 5.4 | 4.8 | 4.0 |
SD, standard deviation; BMI, body mass index; VO2 max, maximum oxygen uptake; LDL, low-density lipoprotein cholesterol; HDL, high-density lipoprotein cholesterol;
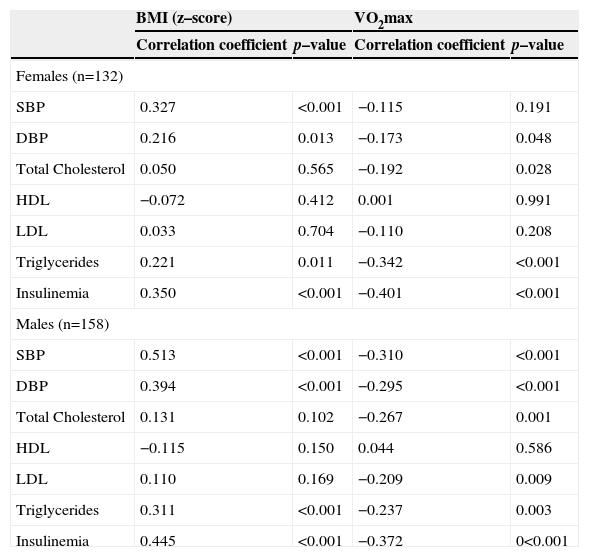
Spearman's correlation coefficients for BMI and aerobic fitness with CVD risk factors are shown in Table 2. Both genders showed a significant positive correlation between the BMI z-score and SBP, DBP, triglycerides, and insulinemia. The correlations between the BMI z-score and total cholesterol, HDL, and LDL levels were not significant in either gender. Aerobic fitness in female was negatively and significantly correlated with DBP, total cholesterol, triglycerides, and insulinemia. In boys, a strong negative and significant correlation (p<0.01) was found between aerobic fitness and SBP, DBP, total cholesterol, LDL, triglycerides, and insulinemia.
Spearman's correlation coefficients between BMI (z–score) and VO2 max with CVD risk factors in females and males aged 6 to 10 years (n = 290)
| BMI (z–score) | VO2max | |||
|---|---|---|---|---|
| Correlation coefficient | p–value | Correlation coefficient | p–value | |
| Females (n=132) | ||||
| SBP | 0.327 | <0.001 | −0.115 | 0.191 |
| DBP | 0.216 | 0.013 | −0.173 | 0.048 |
| Total Cholesterol | 0.050 | 0.565 | −0.192 | 0.028 |
| HDL | −0.072 | 0.412 | 0.001 | 0.991 |
| LDL | 0.033 | 0.704 | −0.110 | 0.208 |
| Triglycerides | 0.221 | 0.011 | −0.342 | <0.001 |
| Insulinemia | 0.350 | <0.001 | −0.401 | <0.001 |
| Males (n=158) | ||||
| SBP | 0.513 | <0.001 | −0.310 | <0.001 |
| DBP | 0.394 | <0.001 | −0.295 | <0.001 |
| Total Cholesterol | 0.131 | 0.102 | −0.267 | 0.001 |
| HDL | −0.115 | 0.150 | 0.044 | 0.586 |
| LDL | 0.110 | 0.169 | −0.209 | 0.009 |
| Triglycerides | 0.311 | <0.001 | −0.237 | 0.003 |
| Insulinemia | 0.445 | <0.001 | −0.372 | 0<0.001 |
BMI, body mass index; VO2 max, maximum oxygen uptake; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol
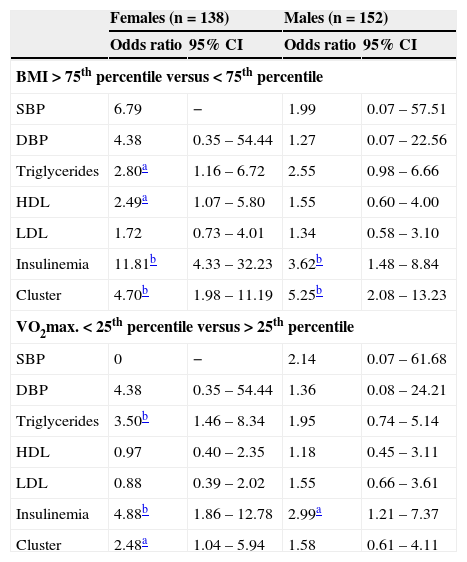
Increased odds ratios for clustering of CVD risk factors and insulinemia in relation to the variables BMI and aerobic fitness in both genders are shown in Table 3.
Odds ratio for cardiovascular disease risk factors in females and males aged 6 to 10 years (n = 290)
| Females (n = 138) | Males (n = 152) | |||
|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | |
| BMI > 75th percentile versus < 75th percentile | ||||
| SBP | 6.79 | − | 1.99 | 0.07 – 57.51 |
| DBP | 4.38 | 0.35 – 54.44 | 1.27 | 0.07 – 22.56 |
| Triglycerides | 2.80a | 1.16 – 6.72 | 2.55 | 0.98 – 6.66 |
| HDL | 2.49a | 1.07 – 5.80 | 1.55 | 0.60 – 4.00 |
| LDL | 1.72 | 0.73 – 4.01 | 1.34 | 0.58 – 3.10 |
| Insulinemia | 11.81b | 4.33 – 32.23 | 3.62b | 1.48 – 8.84 |
| Cluster | 4.70b | 1.98 – 11.19 | 5.25b | 2.08 – 13.23 |
| VO2max. < 25th percentile versus > 25th percentile | ||||
| SBP | 0 | − | 2.14 | 0.07 – 61.68 |
| DBP | 4.38 | 0.35 – 54.44 | 1.36 | 0.08 – 24.21 |
| Triglycerides | 3.50b | 1.46 – 8.34 | 1.95 | 0.74 – 5.14 |
| HDL | 0.97 | 0.40 – 2.35 | 1.18 | 0.45 – 3.11 |
| LDL | 0.88 | 0.39 – 2.02 | 1.55 | 0.66 – 3.61 |
| Insulinemia | 4.88b | 1.86 – 12.78 | 2.99a | 1.21 – 7.37 |
| Cluster | 2.48a | 1.04 – 5.94 | 1.58 | 0.61 – 4.11 |
Cluster: three or more of the following factors present in the same child: LDL, triglycerides, and glucose levels > 100 mg/dL; HDL cholesterol <45 mg/dL; Insulinemia, systolic, and diastolic blood pressure > 80th percentile for age and gender; 95% CI=95% confidence interval
In the present study, BMI was positively associated in both genders with SBP, DBP, triglycerides, and insulinemia. Children with BMI above the 75th percentile had increased odds ratio for CVD risk factors, when compared with children below the 75th percentile. Aerobic fitness was negatively associated in both genders with DBP, total cholesterol, triglycerides, and insulinemia. Increased odds ratio for altered insulinemia in both genders and for clustering of CVD risk factors in girls were found when comparing aerobic fitness below and above the 25th percentile. Mean values of the CVD risk variables found in this study for both genders, except total cholesterol (171.4 mg/dL) and LDL (103.7 mg/dL) in females, are within the range considered “desirable” according to the I Guideline for the Prevention of Atherosclerosis in Childhood and Adolescence16 and are similar those found in the Belo Horizonte Heart Study (Estudo do Coração de Belo Horizonte).17
Other studies corroborate the present investigation with significant and positive correlations between BMI and SBP, DBP,2,18 triglycerides, and insulin.2,19 However, the non-significant correlations found in this study between BMI and total cholesterol, HDL, and LDL in both genders are not in agreement with the results of the aforementioned studies. As in the present study, Sinaiko et al20 also found no significant correlation between BMI and HDL (p=0.07), nor between BMI and LDL (p=0.48) in males, whereas this correlation was significant in females. In the present study, females above the 75th BMI percentile in comparison to those below the 75th percentile had odds increased by 2.8, 2.5, and 11.8 fold for altered triglycerides, HDL, and insulinemia, respectively. In males, the odds for those with a BMI above the 75th percentile were 3.6 fold higher for elevated insulinemia.
The odds of having a clustering of CVD risk factors for females and males, respectively, were 4.7 and 5.3-fold higher for those above the 75th percentile. Falaschetti et al2 studied 5,002 children aged 7 to 12 years and found significant odds ratios among those below the 85th percentile and those above the 95th percentile of BMI in both genders, for hypertension, high triglycerides, and low HDL levels. The Belo Horizonte Heart Study found, in 1,450 children and adolescents aged 6-18 years, significant odds ratios for CVD risk variables when comparing students with BMI below and above the 85th percentile.17 In that study, the odds for altered HDL and elevated SBP and DBP were, respectively, 2.2, 3.6, and 2.7 fold higher for students with a BMI above the 85th percentile. Perhaps no increased odds for elevated SBP and DBP were observed for both genders in the present study because the cutoff point was established above the 75th percentile for BMI, rather than above the 85th percentile, as in the Belo Horizonte Heart Study.
Although BMI does not discriminate abdominal from visceral obesity, the latter is associated, through several mechanisms, to some risk factors for CVD. Visceral adipose tissue secretes larger amounts of adipocytokines compared to subcutaneous fat. The adipocytokines have inflammatory and immune functions that mediate insulin resistance, cardiovascular complications, and especially the atherogenic process via inflammatory biomarkers such as TNF-alpha, IL-6, and C-reactive protein (CRP).21,22 The adipocytokines indirectly mediate lipolysis and increase hepatic fatty acid synthesis, thus increasing serum levels of fatty acids and triglycerides.21
The high correlations between BMI, insulinemia, and triglycerides for both genders in the present study corroborate the aforementioned studies.
Aerobic fitness showed a significant and negative correlation with DBP, total cholesterol, triglycerides, and insulinemia in girls in the present study. In boys, the correlations were stronger (p<0.01) and also more significant with SBP and LDL-cholesterol. These results are similar to several other studies in the pediatric population.10,11,23,24 Kriemler et al9 found an inverse association between aerobic fitness and the sum of four skinfolds, insulin resistance, and metabolic risk; furthermore, they observed a 6% reduction in insulin resistance for each increase of one stage in an aerobic fitness test.
The importance of aerobic fitness was emphasized by Kelly et al,25 who observed improvement in VO2 max, HDL cholesterol, and endothelial function after eight weeks of aerobic training in a group of children, when compared to the control group without training. A study conducted with overweight and obese children and adolescents submitted to 12 weeks of moderate-intensity aerobic training three times per week showed reductions in total cholesterol/HDL ratio, C-reactive protein, and body fat, concomitant with an increase in aerobic fitness.26
In the present study, females with aerobic fitness below the 25th percentile were 3.5 and 4.9-fold more likely to have increased triglycerides and insulin, when compared to the other girls. Males below the 25th percentile of aerobic fitness were three-fold more likely to have altered insulinemia. The increased odds for altered insulinemia in children with BMI in the last quartile and aerobic fitness in the first quartile can perhaps be partially explained by the cutoff above the 80th percentile used for insulinemia. However, a recent review showed that the 75th and 80th percentiles are the most used cutoffs in epidemiological studies in children. 21 As hyperglycemia is rarely present in children, fasting glucose and the homeostatic model assessment – insulin resistance (HOMA-IR) index bring less information than insulinemia alone.20 For this reason, it was decided to use insulinemia in the present study.
Two-and-a-half-fold higher odds were found for a cluster of CVD risk factors in girls below the 25th percentile of aerobic fitness, compared to the other girls. The analysis of 9-year-old schoolchildren observed 13-fold higher odds of having clustering of CVD risk factors for those in the first quartile of aerobic fitness in relation to those who were in the fourth quartile.13 Another study, with 1,140 European children aged 9-10 years, showed 3.1-fold higher odds of clustering of metabolic risk factors for females and 2.4-fold higher odds for males, when comparing those below and above the 75th percentile of aerobic fitness.11
Ruiz et al23 used analysis of variance to compare the means of variables of CVD risk among the four quartiles of aerobic fitness. Significant differences were observed between the first and fourth quartiles of aerobic fitness for insulin resistance in both genders, and between the first and fourth quartiles for triglycerides and total cholesterol/HDL ratio in girls. Males and females in the first quartile of aerobic fitness also had lower metabolic risk in relation to other children.
Aerobic fitness can be assessed in a running test in which the body mass of the assessed individual directly affects test performance or in cycle ergometer tests, in which body mass may or may not be considered. As the present study used a running test to evaluate aerobic fitness, overweight and obese children probably had worse results, which may explain the poorer risk profile of children below the 25th percentile of aerobic fitness. Although the physical fitness test used is strongly correlated with laboratory measures of aerobic fitness and has been used in recent studies with children,9,27 motivational factors can affect test results, and perhaps this may explain the inconsistencies in the odds of cardiovascular risk between the genders observed here.9,27
Even in overweight children, better aerobic fitness attenuates the metabolic and CVD risk by mechanisms that possibly involve genetic factors, adipocytokines, and oxidative capacity of skeletal muscle.28 The benefits of aerobic fitness may involve improved insulin action, improved glucose transport, improved fat metabolism, increased levels of HDL-cholesterol, and decreased sympathetic tone and blood pressure.29 Therefore, the association between aerobic fitness and CVD risk factors justifies the inclusion of aerobic fitness assessment, especially in the school environment, as part of children's health monitoring.
Possible limitations of this study include its cross-sectional design, which prevents establishing a causal association between the variables and the generalization of these data to other regions of the country due to possible ethnic, cultural, and socioeconomic differences. Despite these limitations, the results reinforce the contribution of high BMI and a low level of aerobic fitness to the presence of clustering of cardiovascular disease risk factors in children.
Conflicts of interestThe authors declare no conflicts of interest.
FundingFAPEMIG – process APQ 02341-10. Universidade de Itaúna – MG: project 016/2010.