Due to its hardness, zirconia abutments may damage the titanium of the implant's connection during its clinical use. This study aimed to assess the wear of the seating platforms of externally hexed titanium implants when connected to zirconia abutments comparing to titanium abutments, after thermocycling and mechanical loading (TCML).
MethodsSix BNT® S4 external connection implants (Phibo® Dental Solutions, Barcelona, Spain) were selected and divided into two groups (n=3): TiCE, screwed to titanium abutments and ZrCE, screwed to zirconia abutments. The samples underwent thermocycling (5000 cycles; 5–55°C) and mechanical loading (1.2×106 cycles; 88.8N; 4Hz). Before and after TCML, the seating platforms of the implants were analyzed by 3D profilometry in two areas to measure their topography based on the superficial analysis parameters (Sa and Sz) parameters, and were studied by scanning electron microscopy (SEM). Data were statistically analyzed by Mann–Whitney test (p<0.05).
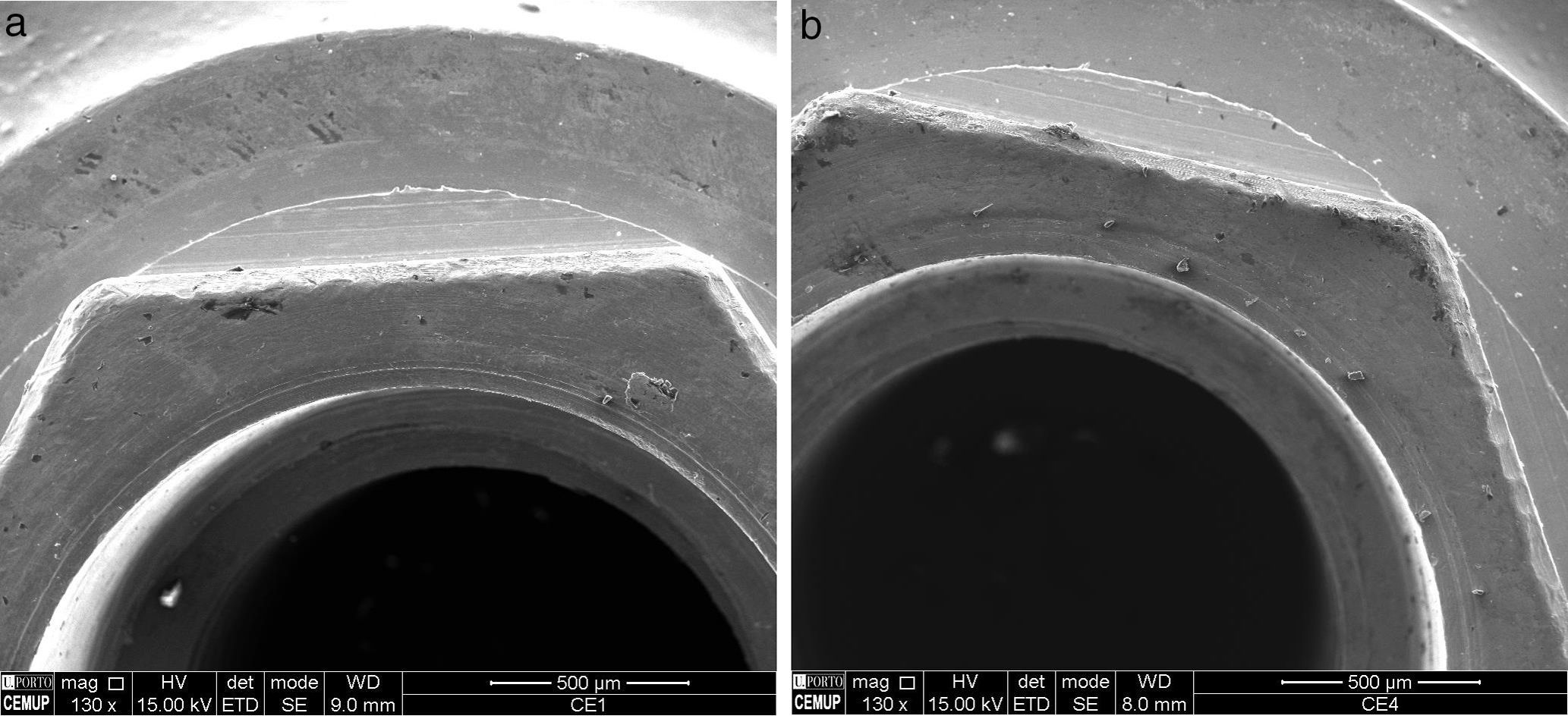
ResultsNo statistically significant differences were observed in the Sa and Sz values between the implants at initial state and after TCML (p=0.573>0.05 and p=0.059). The abutment's material (titanium/zirconia) did not statistically significantly influence the Sa and Sz values after TCML (p=0.886>0.05 and p=0.200, respectively). However, the SEM analysis reveals a mild wear in some vertices of the hex when connected to zirconia abutments.
ConclusionsAfter simulating five years of clinical use, the externally hexed implants, analyzed by 3D profilometry, showed similar wear patterns in the corresponding seating platforms when connected to zirconia or titanium abutments. The SEM images showed zirconia particles being transferred to the implant, which requires further study.
Devido á sua dureza, os pilares de zircónia podem provocar danos sobre o titânio da conexão do implante durante a utilização clínica. O presente trabalho pretendeu avaliar o desgaste das plataformas protéticas de implantes de titânio com conexão hexágono externo quando conectados com pilares de zircónia em comparação com pilares de titânio, após carga cíclica e termociclagem (TCML).
MétodosForam selecionados 6 implantes de conexão externa BNT® S4 Phibo® Dental Solutions (Barcelona, Espanha), que foram divididos em 2 grupos (n=3): TiCe aparafusados a pilares de titânio e ZrCe aparafusados a pilares de zircónio. As amostras foram submetidas a TCML (5.000 ciclos; 5–55°C) e carga cíclica (1,2×106 ciclos; 88,8N; 4Hz). Antes e após TCML, as plataformas de assentamento de conexão dos implantes foram sujeitas a análise por perfilometria 3D em 2 localizações para a medição da sua topografia com utilização dos parâmetros de análise superficial (Sa e Sz) e examinadas por microscopia eletrónica de varrimento(MEV). Análise estatística: Mann-Whitney test (p<0,05).
ResultadosNão se observaram diferenças estatisticamente significativas nos valores de Sa e de Sz entre os implantes no estado inicial e após TCML (p=0,573>0,05 e p=0,059). O material do pilar (titânio/zircónia) não exerceu influência estatisticamente significativa nos valores de Sa e Sz após TCML (teste U p=0,886>0,05 e p=0,200, respetivamente). No entanto, a análise por MEV revelou ligeiro desgaste em alguns vértices do hexágono quando conectados com pilares de zircónia.
ConclusõesApós uma simulação de 5 anos de utilização clínica, os implantes com hexágono externo, analisados por perfilometria 3D, apresentaram padrões de desgaste das plataformas de assentamento equivalentes quando conectados a pilares de zircónia ou de titânio. As imagens de MEV mostram a passagem de partículas de zircónia para o implante, aspeto que merece investigação suplementar.
Currently, dental esthetics criteria are one of the success factors in implantology, especially in the rehabilitation of anterior regions. Accordingly, metal has been replaced by ceramics not only in crowns and bridges but also in the components of implant systems, as titanium abutments might impair esthetics by causing a grayish staining in the peri-implant tissues in patients with thin biotypes.1–4 Due to their optical, mechanical, and biological properties, high-strength ceramic abutments, such as yttria-stabilized tetragonal zirconia polycrystals (3Y-TZP), have been increasingly used.5 These abutments have provided high technical and biological success rates and have shown performances similar to those of titanium abutments. This fact has been reported in clinical studies of up to 12 years.6–10
Most clinical studies have been focused on abutment/implant assemblies with externally hexed connections.6,11–13 Recent systematic review supports the use of zirconia abutments in the external connection implants due to their long term performance.9 In vitro studies show that secondary metallic components (two piece) have a positive influence on the zirconia abutments stability.14 Other studies advise against direct link abutment to the implant head.15 Clinical and in vitro studies on the performance of single abutments connected to external connection implants have reported the loosening of the screw as the main technical problem.1,11,15,16 On the other hand, the stability of the abutment/implant connection is considered the main factor for the implant system to reach clinical success. It is influenced by several factors, such as the material of the abutments, the adjustment and precision in the fabrication of its components, its contamination by saliva, the preload on the retaining screw, the microgap, the connection geometry, and aging.17–25
Despite the success reported by clinical studies, some issues are still not clear, including the fact that connecting zirconia to titanium implants subjected to loading leads to changes in the connection surfaces. In fact, mastication may involve micromovements in the contacting surfaces of the abutment/implant assemblies, thus causing wear/fretting.26–29 When the abutment/implant assemblies are made of the same material (Ti/Ti), with the same Young's modulus, the strain energy is equally distributed to both components, despite the fact that titanium, implant constituent (cp-Ti grade II), shows a hardness (177 HV) shorter than the pillar titanium alloy (grade V, Ti6Al14V) 256 HV (Vickers).30
However, when titanium is replaced by zirconia (hardness 1354 HV), in one of the components (Ti/Zr), the strain energy is directed to the component with a lower Young's modulus, which in this case is the titanium from the implant connection.28 The detachment of material from the seating platforms may result in a worse performance of the abutment/zirconia assemblies, and may even cause cytotoxicity in the human tissues.30–33
In this study, we aimed to assess the wear of the seating platforms of external connection titanium implants when connected to zirconia abutments and titanium abutments, after thermocycling and mechanical loading (TCML) in a wet environment. The null hypothesis tested was: there are no differences in wear of the seating plattforms between sets T/Ti and Ti/Zr afterTCML.
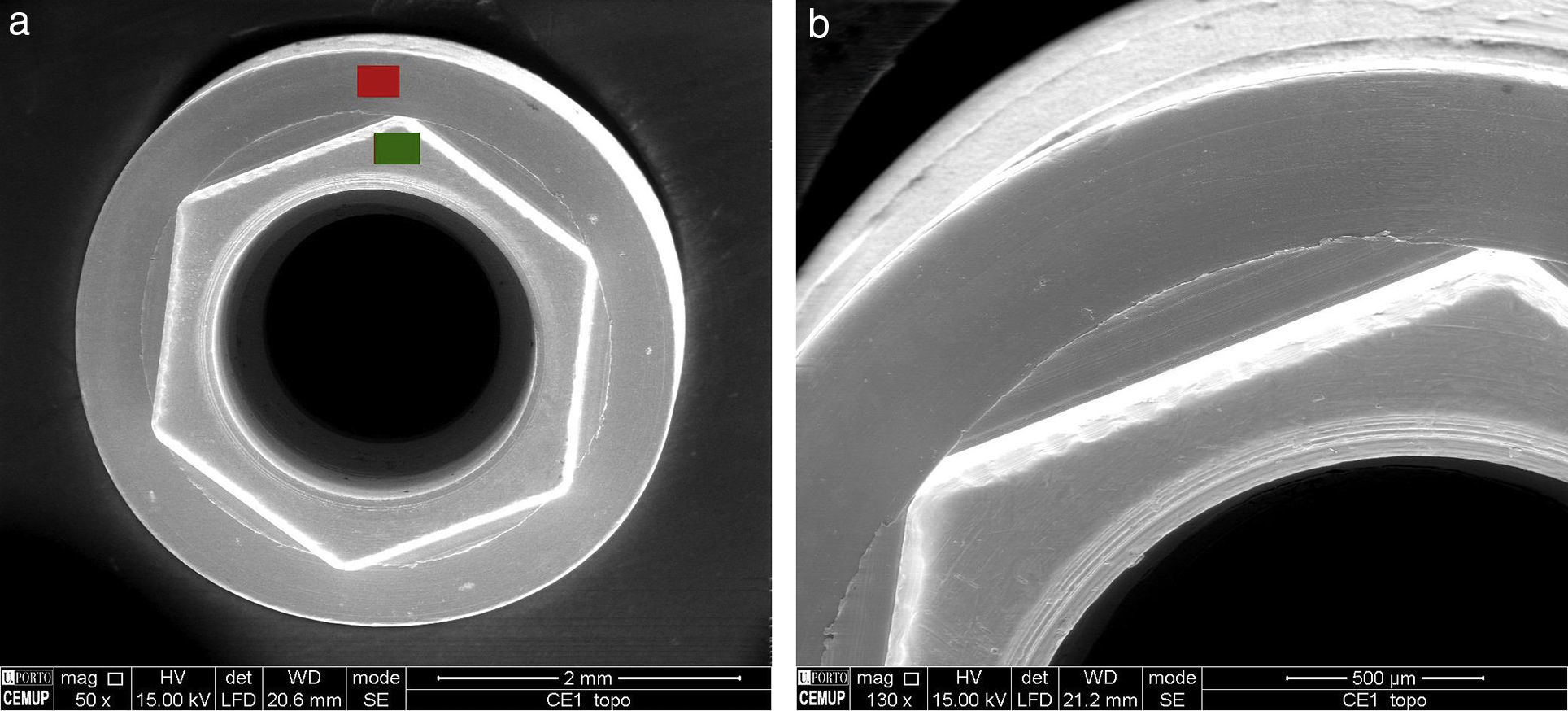
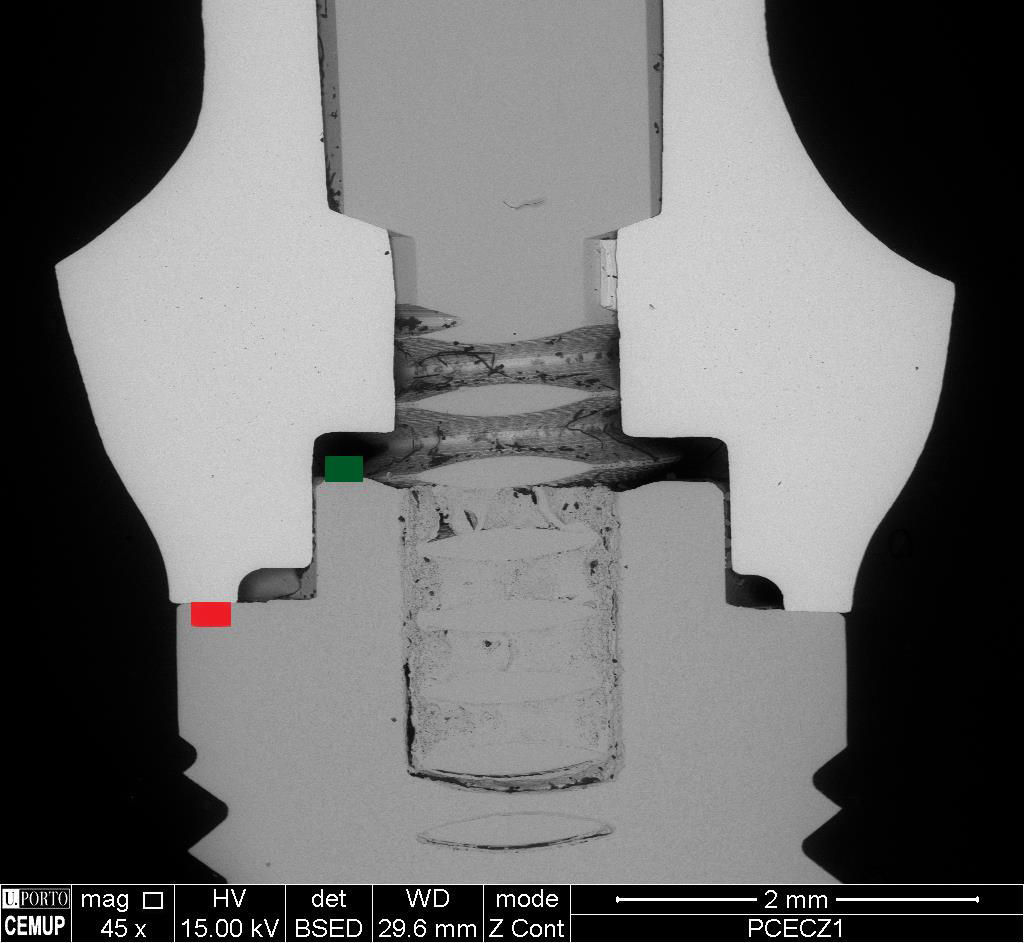
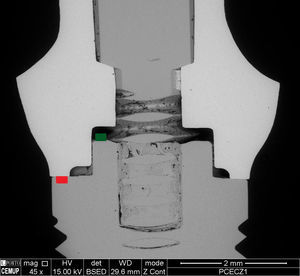
Material and methodsWe randomly selected six externally hexed (CE) implants from a lot of 20 BNT® S4 implants (Phibo® Dental Solutions, Barcelona, Spain). These implants, composed of pure grade 2 titanium, had a connection platform with 4.0mm of diameter, a body with 4.2mm of diameter, and a length of 10mm (Fig. 1a).
We randomly selected three titanium abutments (TiCE, n=3) and three zirconia abutments (ZrCE, n=3) from a lot of ten abutments for each group. Using the Phibo® CAD-CAM system (Phibo® Dental Solutions, Barcelona, Spain), the abutments were designed and produced for external connection platforms in two different materials: titanium and zirconia. Using a digital design program (3Shape's CAD Design, 3Shape, Denmark), a screwed straight abutment was designed to mimic the core of an upper central incisor.
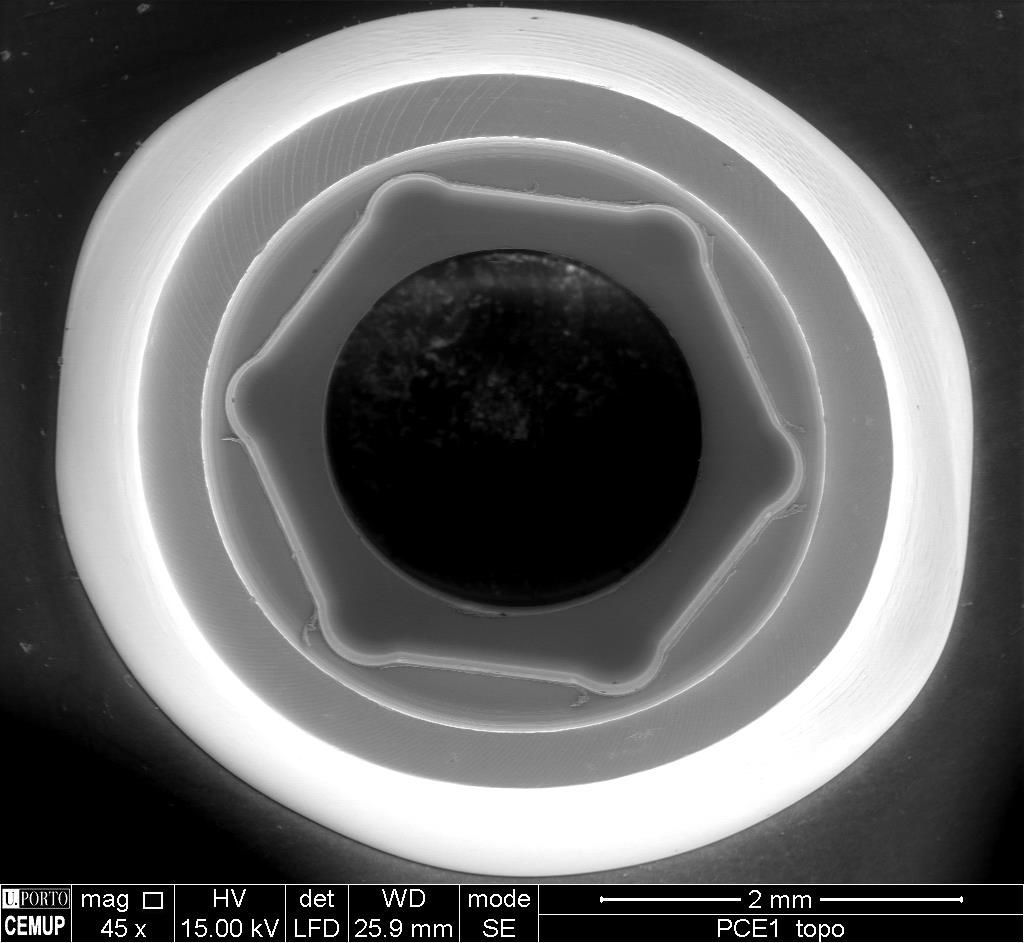
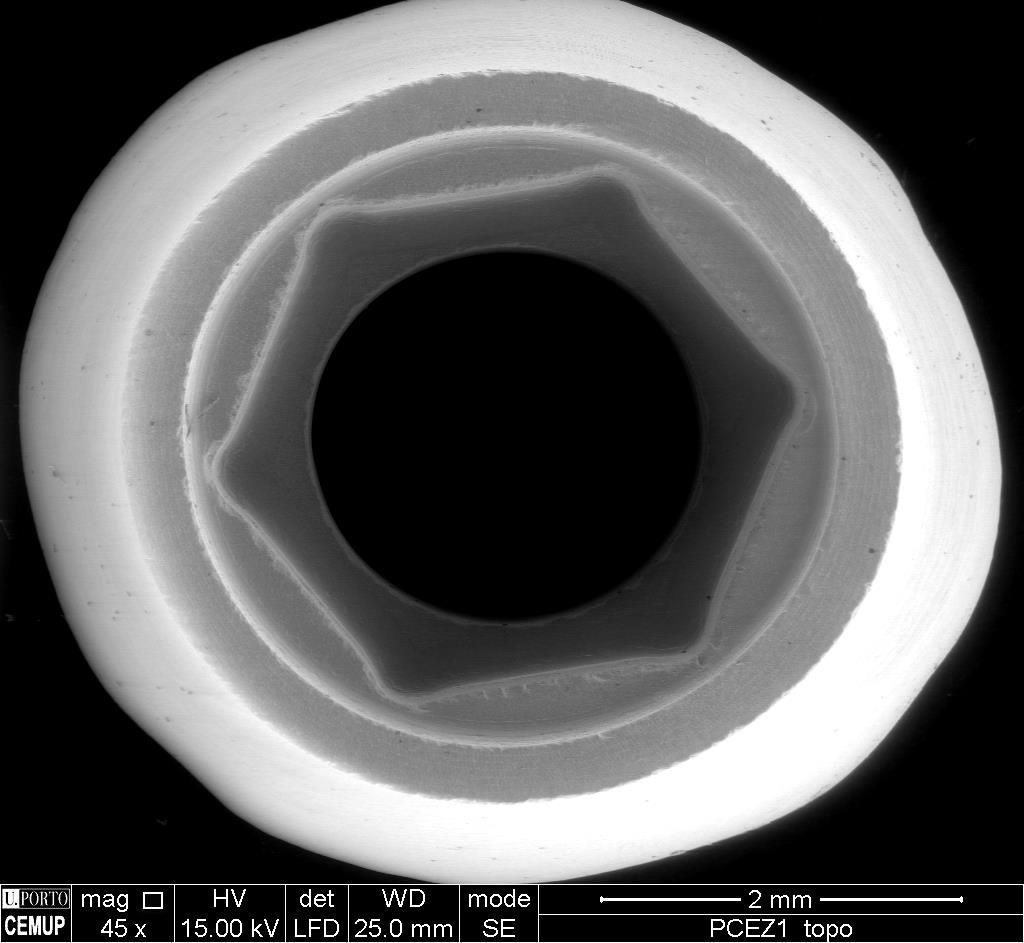
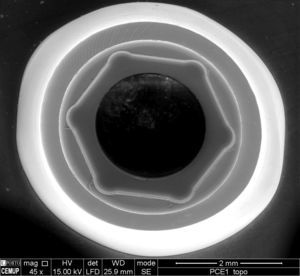
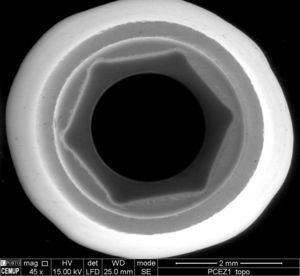
The titanium abutments (Fig. 2) were obtained using a five-axis milling machine on a block of Ti6Al4V (grade 5 titanium) titanium alloy. This alloy is composed of 90% Ti, 6% aluminum, and 4% vanadium. The zirconia abutments (Fig. 3) were obtained by milling a pre-sintered block of yttria-stabilized tetragonal zirconia polycrystals (3Y-TZP), which was then sintered, according to the ISO 6872:2008 and 13356:2008 standards.34
Afterward, the abutments and implants were bathed in ethyl alcohol for 5min in an ultrasound device (Biosonic® UC50BB, Coltène, Switzerland), and were left to dry in the open air.
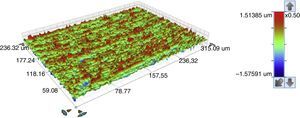
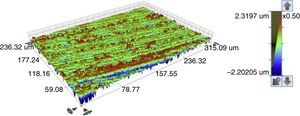
In terms of optical profilometry we selected two reading areas – the top and base regions of the corresponding implant connections (marked respectively with red and green in Figs. 1a and 4). A white light optical interferometer (Bruker NPFLEX™, Karlsruhe, Germany) was used to measure the surfaces’ roughness by 3D profilometry. For each reading in areas of 320μm×240μm, a 10× magnifying lens with a lateral resolution of 1μm was used. The roughness parameters were established with a two-dimensional Gaussian filter of 80μm. The selected roughness parameters were in accordance with the ISO norm 25178-2:2012.35
An upper view was acquired using scanning electron microscopy (SEM, Quanta 400FEG ESEM/EDAX Genesis X4M), with a 45× and 135× magnification, to study the implant connections.
The samples were subjected to 5000 thermal cycles in running water with temperatures ranging from 5 to 55°C, during 25s per bath with 5-s intervals (Ethik Technology 321, São Paulo, Brazil).
To study mechanical loading, the abutment/implant assemblies were individually identified and positioned in a vise. Torque was applied using a torque wrench (Ref. 172.1252, Phibo®) and a digital torquemeter (Lutron, Taiwan), complying with the intensity recommended by the manufacturer: 35Ncm for the Ti/Ti assemblies and 25Ncm for the Zr/Ti assemblies. The abutments were torqued into the corresponding implants with a screw and, after a 10-min waiting period, the screws were retightened with the same torque value.
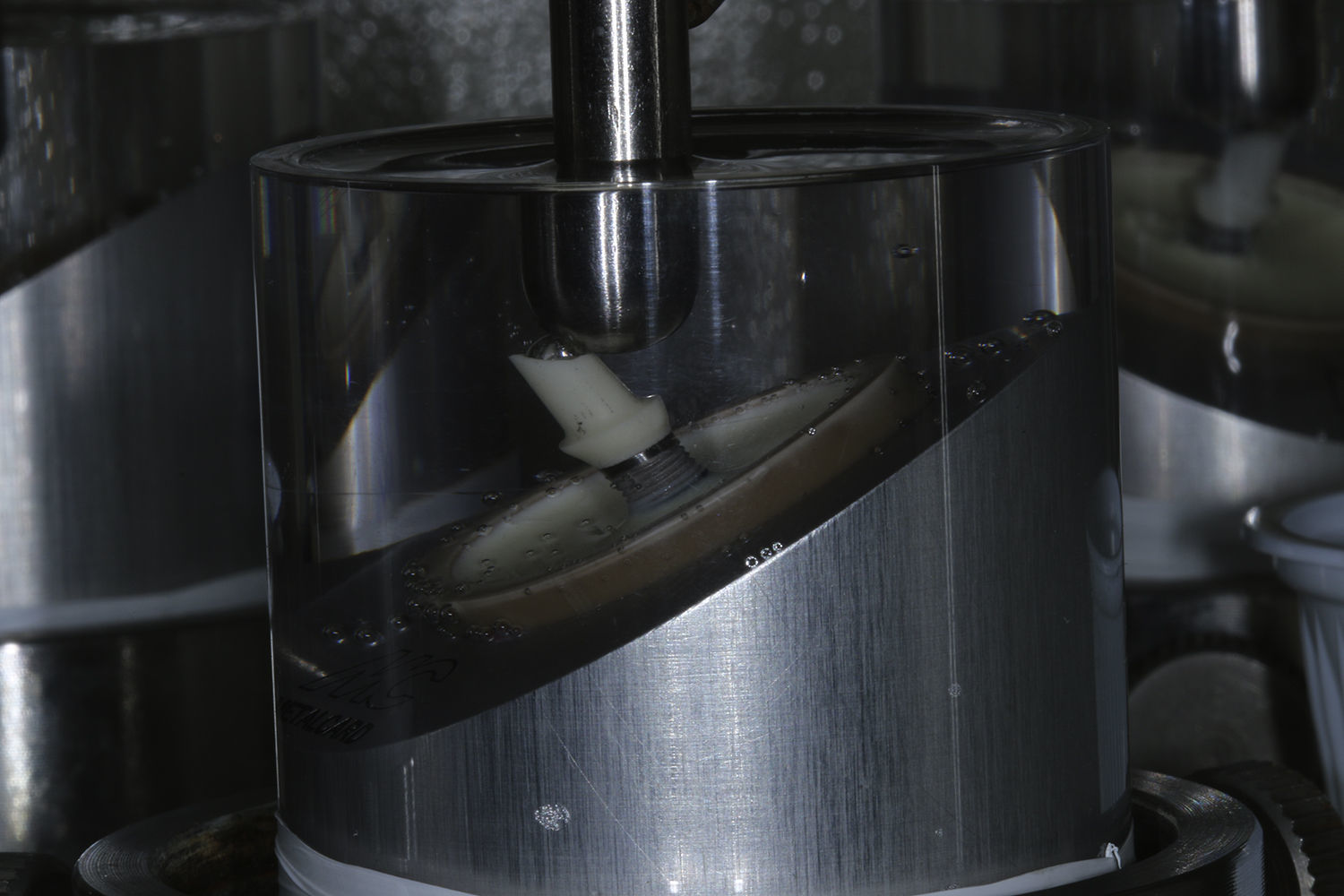
The abutment/implant assemblies were placed in a dental surveyor and vertically positioned in polyurethane resin cylinders (F160, Axson, São Paulo, Brazil) at up to 3mm from the platform, using the mobile rod of the dental surveyor. All samples were subjected to 1.2×106 mechanical cycles with loads from 1 to 88N, with a 4Hz frequency, in a thermomechanical wear equipment (ERIOS 37000, São Paulo, Brazil), thus corresponding to five years of clinical fatigue (Fig. 5).36,37 For that procedure, samples were placed in devices with a 30° angulation in relation to the vertical axis, and loading was applied, using a stainless steel rod with a rounded extremity, in the incisal edge of the palatal surface, in order to mimic the interincisal angle in normal occlusion.38 During this test, the samples were kept in distilled water at 37°C. Instruments and equipment tests were calibrated and suitable for the study.
After the mechanical loading, the abutment/implant assemblies were unscrewed and subjected to 3D profilometry and SEM analyses, using the same protocol as before TCML.
The statistical analysis of the data was performed with the SPSS software (IBM SPSS® Statistics, version 23.0, IBM corp®), using the nonparametric Mann–Whitney test. The decision rule was based on detecting a statistically significant finding to probability values inferior to 0.05.
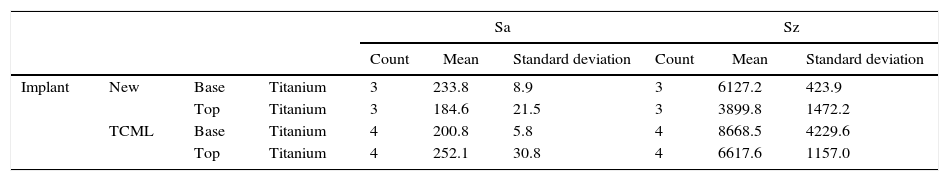
ResultsReadings were performed in the seating platforms of the implants and corresponding abutments before and after TCML. The mean Sa and Sz roughness parameters are presented in Table 1 (in nanometers). The seating platforms of the implants showed a mean Sa value of 193nm and 225nm in the base and top locations, respectively, at the initial state. After TCML, Sa and Sz parameters increased. Implants connected with titanium abutments showed Sa values of 196nm and 265nm and the ones connected with zirconia abutments showed 205nm and 239nm, in the base and top locations, respectively, after TCML.
Results from the 3D profilometry of the seating platforms of the base and top regions of the external connection implant (CE), at the initial state and after TCML, with mean Sa and Sz roughness parameters and standard deviation in nanometers.
| Sa | Sz | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Count | Mean | Standard deviation | Count | Mean | Standard deviation | ||||
| Implant | New | Base | Titanium | 3 | 233.8 | 8.9 | 3 | 6127.2 | 423.9 |
| Top | Titanium | 3 | 184.6 | 21.5 | 3 | 3899.8 | 1472.2 | ||
| TCML | Base | Titanium | 4 | 200.8 | 5.8 | 4 | 8668.5 | 4229.6 | |
| Top | Titanium | 4 | 252.1 | 30.8 | 4 | 6617.6 | 1157.0 | ||
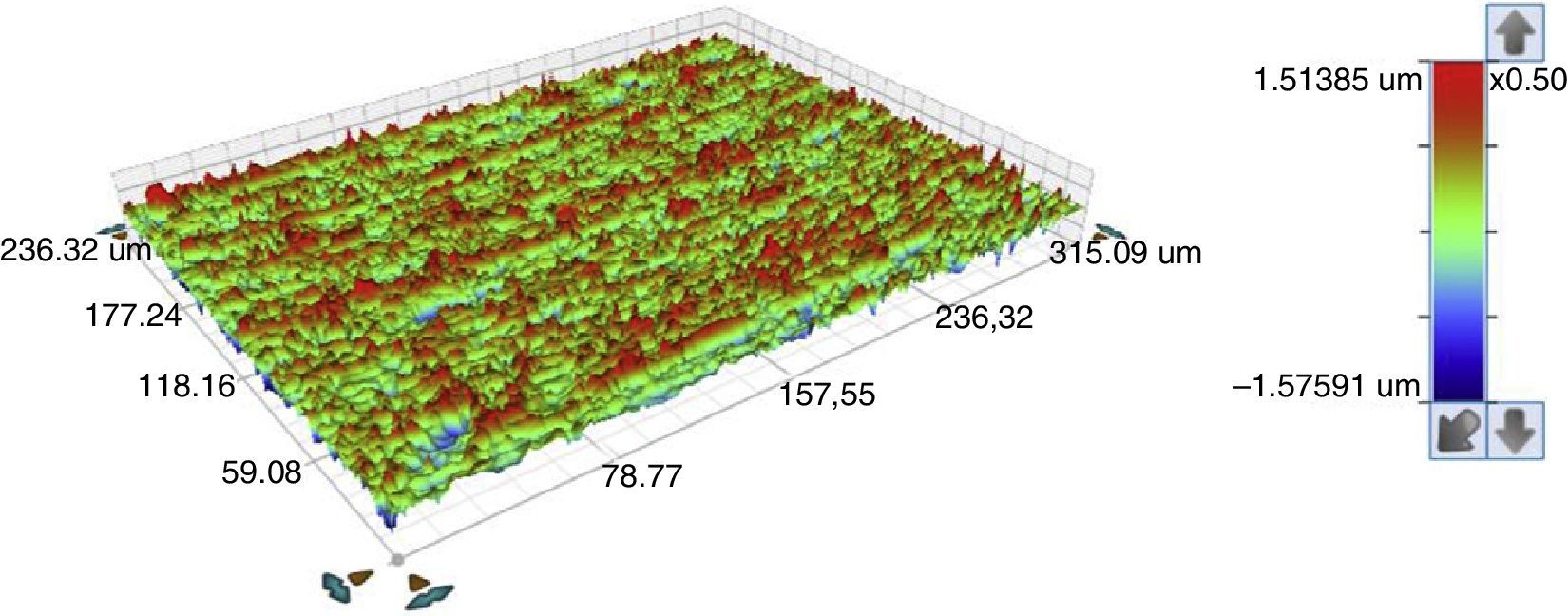
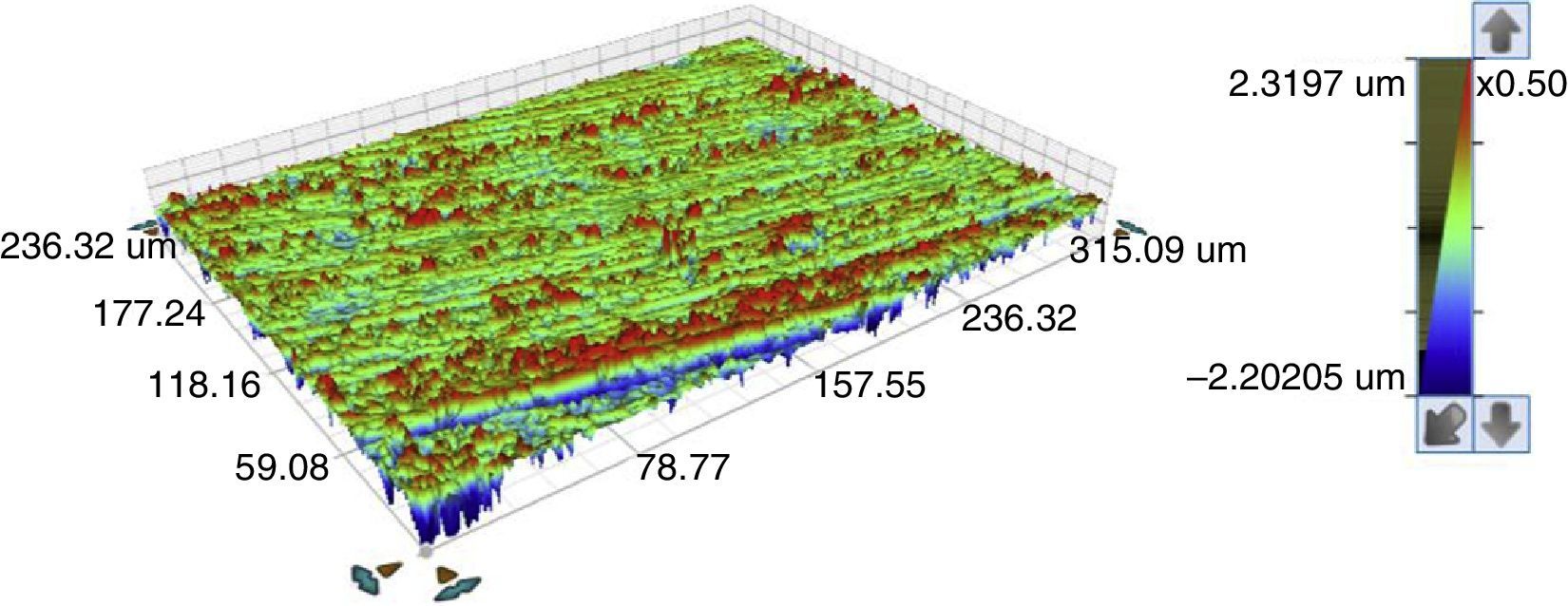
The three-dimensional representation of the surface topography is demonstrated in Figs. 6 and 7, where the legend's color code explains the roughness levels: green for zero roughness, blue for valleys and depressions, and red for peaks.
No statistically significant differences were observed in the Sa and Sz values between the implants at the initial state and after TCML (p=0.573>0.05 and p=0.059). Furthermore, no statistically significant differences were detected in the distribution of the Sa and Sz values of the implants (after TCML) connected to titanium abutments, comparing to implants connected to zirconia abutments (p=0.886>0.05 and p=0.200, respectively).
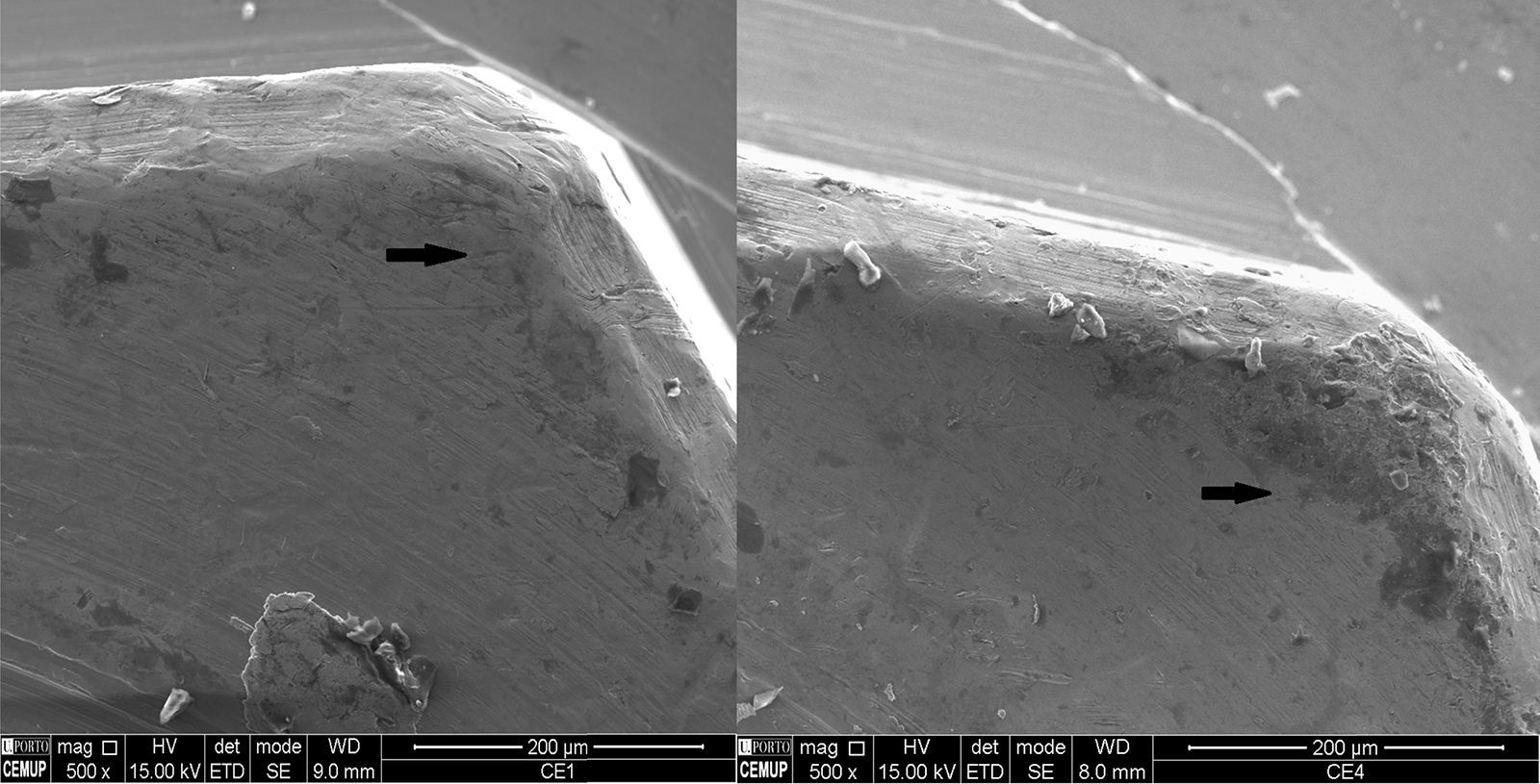
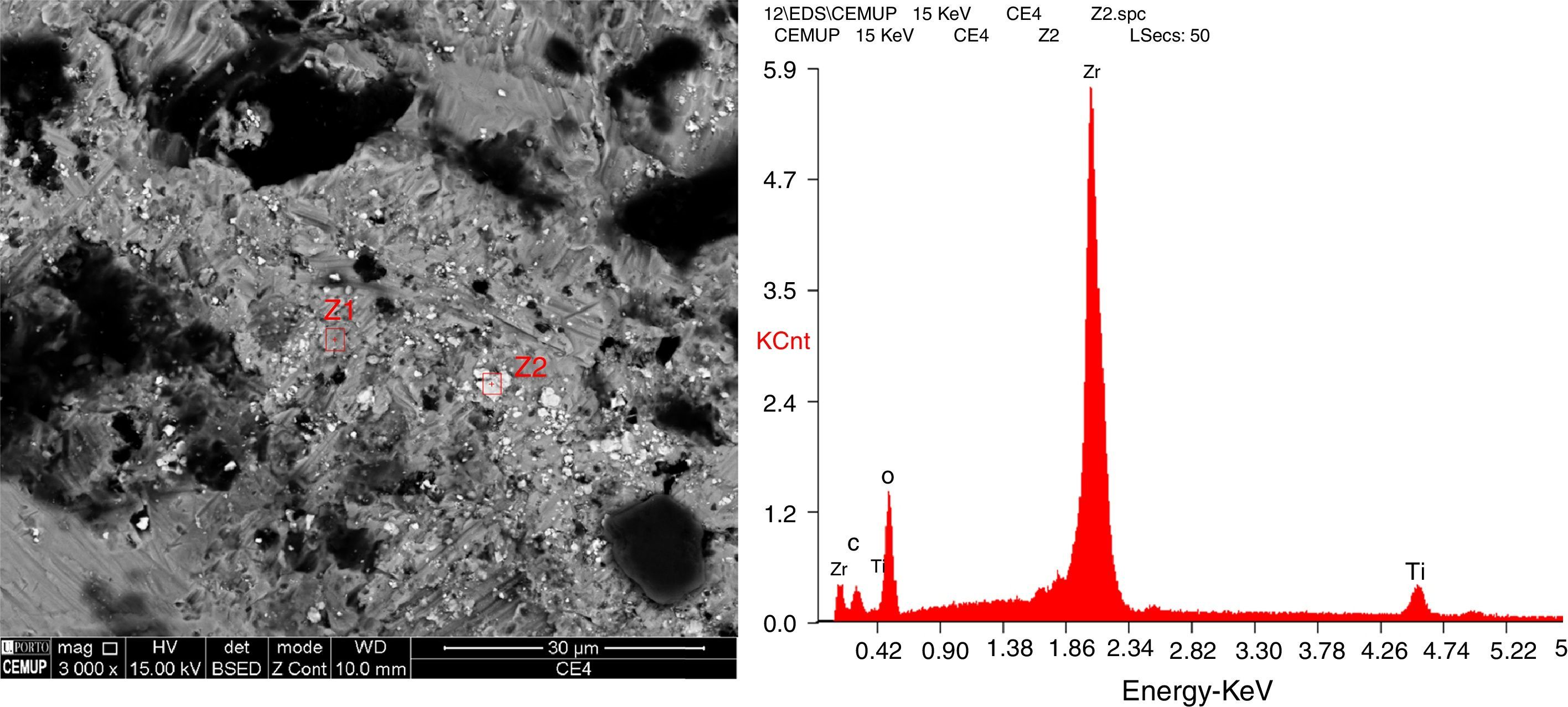
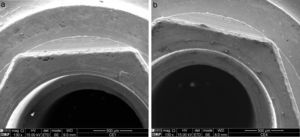
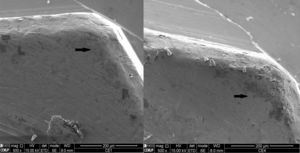
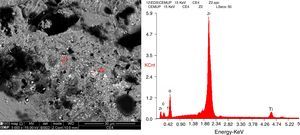
The analysis of the SEM images with 130x and 500x magnification revealed a slight wear at the vertices of the implant's external hex when connected to zirconia abutments (Ti/Zr) after TCML (Fig. 8). Also, small zirconia particles were detected in those same locations (represented by “Z2” in Fig. 9) in the SEM images with 3000× of magnification, and their presence was confirmed by energy dispersive X-ray spectroscopy (EDS) – Fig. 10.
The wear caused by the micromovements of the two contacting surfaces depends on their mechanical properties. An abrasive wear occurs when a hard, rough surface slides on a smoother surface, as in the case of titanium/zirconia or when a material is removed using abrasive paper. On the other hand, an adhesive wear occurs when two surfaces slide on or are pressed against each other, causing material transference between the two surfaces. At initial contact, the surfaces adhere. Posteriorly, a fracture occurs outside the interface, and some fragments of one of the surfaces adhere to the other, due to the strong adhesive interaction between the two surfaces with similar physicochemical properties, such as in the titanium/titanium context, despite the differences in hardness of titanium implants and abutments.
The wear rate is as great as the difference in hardness between the abutment and the implant when micromovements occur. The initial micromovements depend mainly on the adjustment and precision of the components, and at a long-term depend on the wear phenomena in the abutment/implant interface.27
Several studies have reported greater mechanical stability in the abutment/implant interface of implant systems with an internal conical connection, comparing with external connection systems.19,21 However, the stability of abutment/implant assemblies with an external connection has been improved by using Ti alloy screws with a proper head design and by applying an appropriate torque technique, to obtain high preloading values.13,21 This fact might explain the conclusion of one systematic review that the connection geometry had no influence on the incidence of retaining screw loss.22
During the mechanical loading test in our study, no retaining screw loss was reported in any of the sample's components. The 88N load used in this study is within the physiological, clinical load in the anterior region.37,38 The high precision in the adjustment of the abutment connection to the corresponding implant connection, due to using abutments fabricated with the CAD/CAM technique, and the appropriate application of torque have certainly contributed to that result.18
The comparative analysis of the Ti/Ti and Ti/Zr assemblies regarding the topography of the implants’ seating platforms before and after TCML did not reveal statistically significant differences in the Sa and Sz parameters. The roughness parameters describe the features of a surface and never describe a surface completely. We have selected the Sa and Sz parameters because they are the most appropriate to describe the behavior of seating surfaces in this situation. The Sa parameter reflects information on medium roughness and the Sz reflects the maximum defect found on the surface, based on a mean of the five highest peaks added to the five deepest valleys. Therefore, this parameter, instead of analyzing the surface's mean analyzes the surface's extremes.
After TCML, a greater change in the surface topography was expected in the analyzed locations. Our results may be explained by the good stability of the abutment/implant assemblies, in the presence of low-magnitude micromovements, not allowing a significant wear, despite the differences in its properties.
Different geometries induce different patterns of force distribution and different wear areas.28 The analysis of the SEM images revealed a slight wear on the surface of some vertices of the hexes of the implants connected to zirconia abutments (Fig. 8b, blue arrow), and zirconia particles resulting from the abutment's disintegration (Fig. 9). Ceramic materials are harder and more wear resistant but as do not deform plastically reveal low fracture toughness. This situation was not observed in the analysis of the hexes of implants connected to titanium abutments (Fig. 8a). The wear at the vertices of the hex is caused by a 30° tangential force applied to the abutment/implant assemblies, leading to a moment that reaches its maximum in that area. Some particles (Ti, Zr, and Al particles) resulting from wear were detected in the seating platforms. Zirconia abutments were subjected to XRD analysis that revealed absence of crystallographic phase changes, from what there were no signs of aging.5
We partially accept the null hypothesis. The in vitro study analyzed the seating platforms in two locations, in a simulation of five years of fatigue, and did not reveal significant changes in the surface topography. The presence of zirconia particles in the vertices of hexes of implants in Ti/Zr assemblies, as a result from abrasive wear, needs further study. Also, a greater number of locations and observations should be analyzed in further studies.
ConclusionsAfter thermocycling and mechanical loading, the studied externally hexed titanium implants showed wear patterns in the corresponding seating platforms when connected to either zirconia or titanium abutments. According to expected, zirconia, while as a harder biomaterial, can scratch materials considered softer. The vertices of the hexagons of titanium implants were worn when used zirconia abutments. The SEM images showed zirconia being transferred to the implant, which requires further study.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Authors gratefully acknowledge the funding of Project NORTE-01-0145-FEDER-000022 – SciTech – Science and Technology for Competitive and Sustainable Industries, cofinanced by Programa Operacional Regional do Norte (NORTE2020), through Fundo Europeu de Desenvolvimento Regional (FEDER).