Clinically it appears that some patients with etiological factors (dental pathology in the maxillary sinus) exhibit sinus disease and others do not. The aim of this paper is to present the case of a female patient, with a periapical lesion, with symptoms of sinus pathology and the possibility of genetic influence on exacerbated response in the presence of the maxillary sinus pathology of dental origin, through genetic sequencing of IRAK4 gene.
The surgical procedure was performed under general anaesthesia. The cyst was enucleated, the dental roots were extracted, a curettage and an irrigation with physiologic saline 0.9% were performed.
This work opens new perspectives for research on the role of a specific polymorphism in the IRAK4 gene in the host response. Thus, it may provide valuable data for understanding the phenomena that underlie the recurrence of maxillary sinus pathology and also advance knowledge to improve therapeutic decisions.
Clinicamente parece que alguns pacientes com fatores etiológicos de origem dentária apresentam patologia sinusal e outros pacientes não. O objetivo deste trabalho é apresentar um caso de uma paciente do sexo feminino, com lesão periapical e sintomas de sinusite, e a possibilidade de influência genética sobre a resposta exacerbada na presença de patologia do seio maxilar de origem dentária, através da sequenciação do gene IRAK4.
O procedimento cirúrgico foi realizado sob anestesia geral. O cisto foi enucleado, as raízes dentárias foram extraídas, foi realizada curetagem e irrigação do seio maxilar com soro fisiológico 0,9%.
Este trabalho abre novas perspectivas sobre o papel de um polimorfismo específico no gene IRAK4 na resposta do hospedeiro. Assim, pode fornecer dados valiosos para a compreensão dos fenómenos que estão na base da recorrência da patologia do seio maxilar e também promover o avanço no conhecimento nas decisões terapêuticas.
The odontogenic maxillary sinusitis comprises a sinus mucosa inflammation. Dental pathology is considered to be the etiologic factor in 10% to 12% of the maxillary sinusitis cases.1
The paranasal sinuses mucosa exhibits specific features: it is much thinner and composed by ciliated and nonciliated pseudostratified columnar epithelium.2 The cilia act in mass, producing co-ordinated sequential beating and thus, creating a wave-like motion, generally in the direction of the ostium. Obstruction of the ostium may cause decreased ciliary activity, promoting the bacterial growth.3,4 The mentioned reasons for the anaerobic bacteria multiplication include: reduced blood supply to the sinus mucosa, decreased amount of oxygen in the maxillary sinus, decreased ciliary activity and low pH.5
The displacement of bacteria from infected periapical tissue often results in acute or chronic sinusitis. The infected periapical tissue can originate from apical periodontitis, periodontal diseases, implant therapy, tooth extraction, foreign bodies and odontogenic cysts.6
The possible radiographic changes present in a sinusitis include: thickened sinus mucosal membrane, an air-fluid level or complete opacification.7 Therefore, to get a correct odontogenic maxillary sinusitis diagnosis a detailed medical history is required; a complete physical examination and specific imaging probes are also required.5
Some authors believe that there is a considerable interindividual variability in the degree of activation of the innate immunity and inflammatory responses to infection.8–10 Some of these authors, particularly in recent studies, have related some genetic variations in the Interleukin-1 receptor-associated kinase-4 (IRAK4) gene with the rhinitis susceptibility and with the prevalence of Gram-positive infections in critically ill adults.9,10
IRAK4 is a serine-threonine kinase that was considered to be a key player in the signalling of the MyD88-depending pathway of the Toll-like/IL-1-receptor (TIR) and in other Toll-like receptor (TLR) signalling, except for the TLR320.11 The study of Sutherland et al. suggested that the IRAK4 haplotype clade marked by 29429A (428Thr) alters the susceptibility to Gram-positive bacteria infections, by decreasing cellular response to TLR ligands.9
The authors intend to present a case of an infected root accompanied by an odontogenic cyst, with connection with the maxillary sinus, present in a 35-year-old patient. The main purpose of this paper is to explain the possibility of a genetic influence on the exacerbated response present in this case concomitant with odontogenic maxillary sinus pathology, through IRAK4 gene sequencing.
Case reportA 35-year-old woman presented complaints of left and right facial swelling at a general medicine query. She was diagnosed with an “acute bilateral maxillary sinusitis and left ethmoid sinusitis”, for which a 10-day course of cefprozil (250mg twice a day) was prescribed. After this period, the patient still mentioned the presence of symptoms: headache, several episodes of facial brownish and foul-tasting fluid (draining from her left naris and mouth). In the presence of such symptoms, a treatment for allergic rhinitis and sinusitis was adopted that consisted of administering oral antihistamine, oral antibiotic (Amoxicillin/clavulanic acid – 875/125mg) and intranasal steroid. Due to the persistence of symptoms and because of the occurrence of an odontogenic pain, the patient attended a dental appointment. She had left facial swelling, which was painless and firm, with no fluctuation or discoloration of the overlying skin, apparently with no warmth and with a bony consistence.
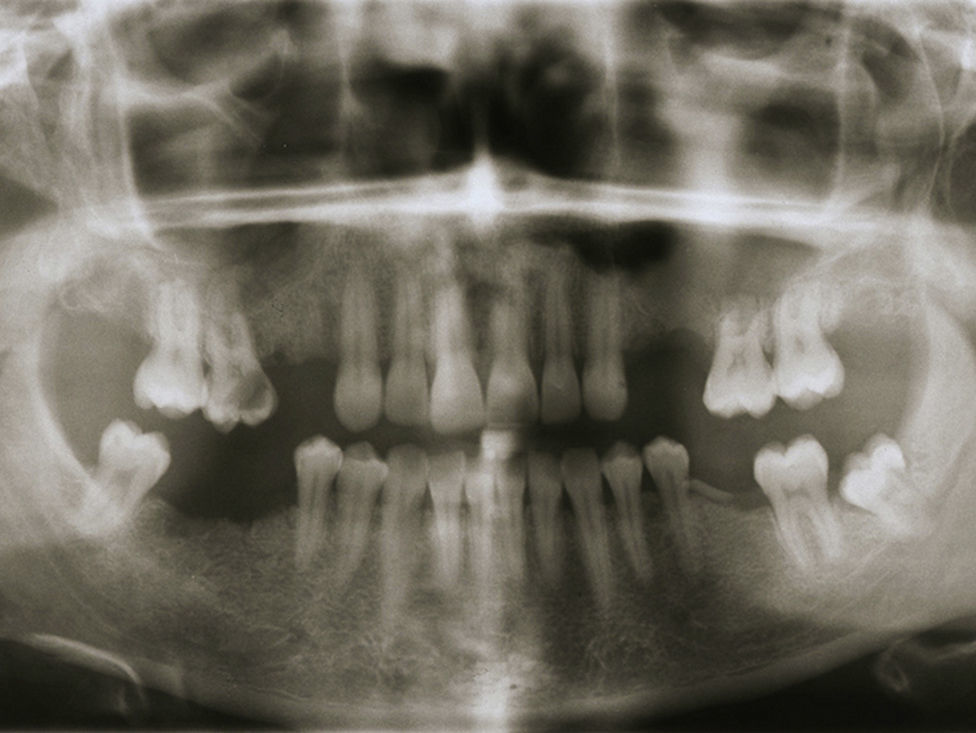
The intra-oral exam revealed the presence of root fragments, corresponding to the first and the second maxillary pre-molars, of the right (teeth 14 and 15) and left (teeth 24 and 25) side (Fig. 1).
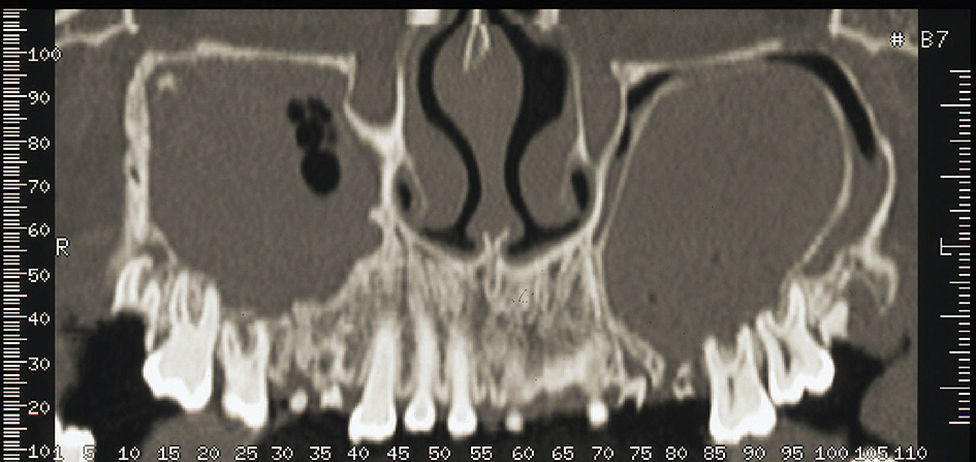
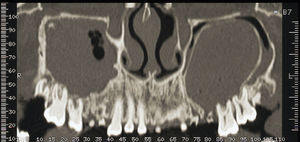
The patient underwent additional imaging, in which (panoramic radiograph: Fig. 2) a communication between the root tips and maxillary sinus was suggested. Computed tomography (CT), acquired with GE Healthcare Light Speed Ultra Pro® (EUA), revealed a low-density and well-circumscribed lesion occupying the entire left maxillary sinus.
The coronal slice of the CT showed the right and left maxillary sinus completely filled. On the left maxillary sinus, the loss of the alveolar cortical bone in correspondence with the root fragments region and, therefore, a direct communication between the oral cavity and the maxillary sinus was also evident. In this location we could also identify an encapsulated lesion, opacification and fluid. On the right side of the maxillary sinus, the CT slice exposed the presence of teeth with apical periodontitis, a severe mucosal thickening, fluid and opacification (Fig. 3). The axial slice of the CT showed a new cortical alveolar bulging, probably as a result of the cystic lesion and was also related with the facial asymmetry. The CT sagittal slice confirmed the presence of the oro-antral fistula.
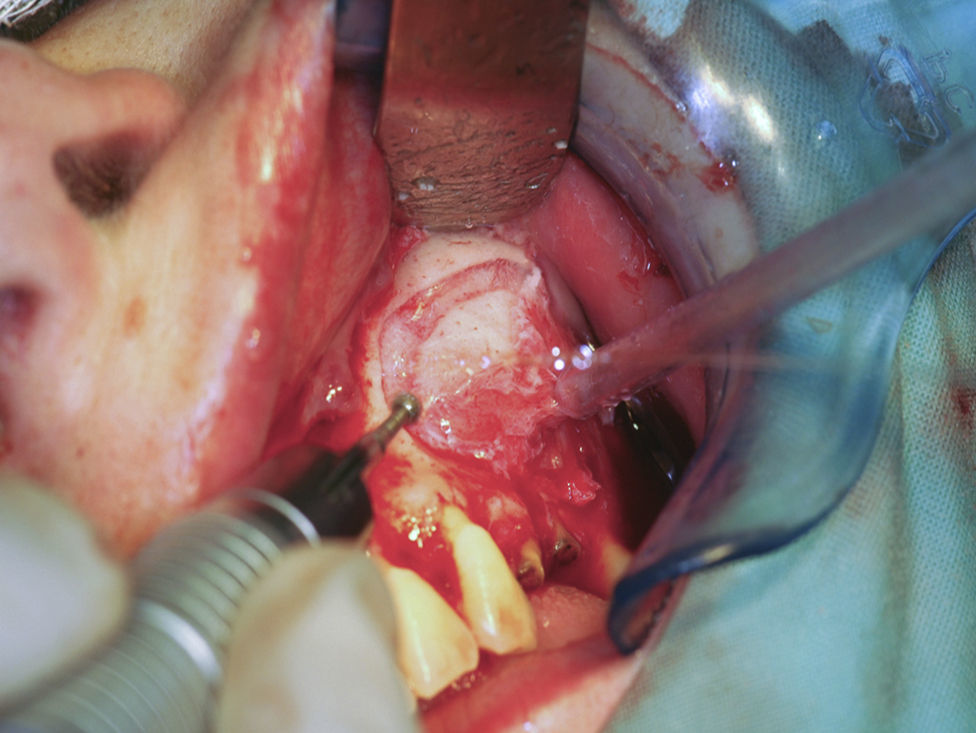
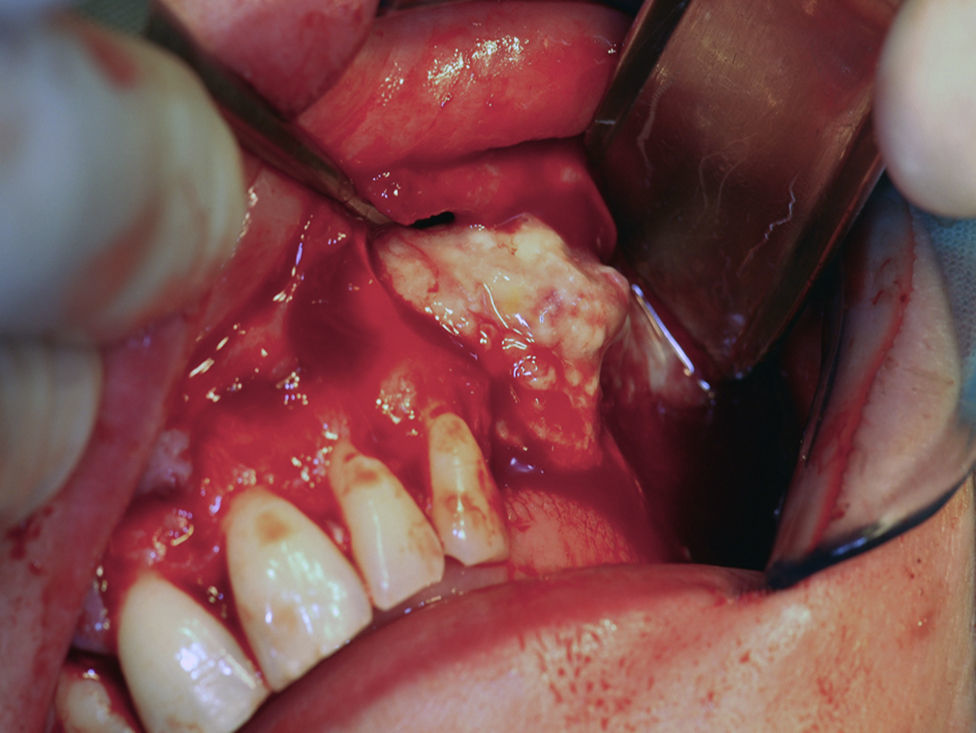
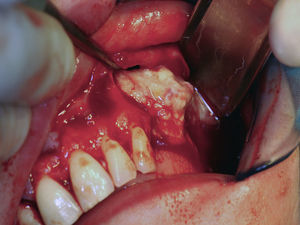
The surgical procedure to remove the cystic lesion was performed under general anaesthesia. The planned surgical approach was of the Newmann type or triangular type, with a sulcular incision, from the first maxillary right incisor (tooth 11) to the root fragment of the third maxillary left molar (tooth 28). After the detachment of a full-thickness mucoperiosteal flap, the lesion was located and a buccal osteotomy was performed with bone drills, in order to promote an osseous window (Fig. 4). The latter allowed the cystic lesion enucleation (Fig. 5), followed by curettage; the pus drainage was present within the sinus and the cleansing of the region through abundant irrigation with physiologic saline 0.9% Ecotainer® (B|Braun®, Sharing Expertise, OEM Division, Melsungen, Germany) was performed. Subsequently, bone regularization was performed, with a wear spherical drill, to eliminate any contaminated tissue that could interfere with the healing process of the surgical region.
During surgery, the extraction of the root fragments was also performed (on left and right sides) using the atraumatic extraction technique. The suture was done with no resorbable suture material – Supramid® 3-0 (B|Braun®, Sharing Expertise, Aesculap AG & Co. KG, Tuttlingen, Germany).
The collected biological material, a cyst-like mass, measuring 3.0cm×5.0cm, was sent for histopathological analysis (Fig. 6) which revealed a radicular cyst.
The patient was medicated with a systemic antibiotic by oral administration (amoxicillin 1000mg – in 12/12h for a period of 15 days), an anti-inflammatory (ibuprofen – in 8/8h for a period of 5 days), an analgesic (paracetamol 1000mg – in 6/6h and/or case of pain) and a topical nasal decongestant (sodium chloride 3% – in 4/4h for a period of 30 days) was also used for medication.
A month after the surgical procedure, the facial swelling of the patient decreased considerably and she had no symptoms of maxillary sinusitis. A panoramic radiograph, on one-year follow-up, presented no recurrence of the radicular cyst (Fig. 7) and the intra oral exam showed the absence of oro-antral fistula.
A buccal swab was also performed in order to collect biological material for DNA extraction and sequencing of the IRAK4 gene. The latter procedure was made in the Molecular Diagnostics Laboratory of CGC Genetics (Portugal).
The IRAK4 gene sequencing identified the polymorphism c.1882G>A (p.Ala428Thr) in heterozygosis.
DiscussionIn the presented clinical case, the patient had some of the symptoms that defined sinusitis, according to American Academy of Otolaryngology-Head and Neck Surgery,12 and exhibited also peculiar maxillary sinus features, such as the presence of fluid and a cyst. The maxillary sinus fluid has been reported to be correlated with a higher incidence (up to 29%) of odontogenic sinusitis in adult patients, particularly in the presence of severe CT imaging findings.13 These authors considered an odontogenic sinus infection based on the presence of three imaging characteristics: projecting tooth root into the sinus, periapical abscess and oroantral fistula.13
The presence of anaerobic bacteria in odontogenic sinusitis defines that the antibiotic prescription in this patient should not be limited to an empiric antibiotic management. In fact, the knowledge of the host susceptibility to the development of exacerbated inflammatory reactions in the presence of anaerobic bacteria may provide an added value in predicting the clinical outcome and to assist in prescribing the most appropriate antibiotic. In our opinion, and according to recent data,9,14,15 that point out recurrent infections related with genetic variations in IRAK4 gene, there are probably individuals who have different host responses to the bacterial challenge. If we analyze the mechanism of the molecular interaction cell, we can easily understand how the IRAK4 gene may play a crucial role in the inflammatory response. Otherwise, it should be noted that: (1) pattern recognition receptors of the innate immune system, most importantly Toll-like receptors (TLRs), recognize conserved domains of pathogens, or pathogen-associated molecular patterns (PAMPs); (2) upon interaction with a PAMP, TLRs interact with a network of intracellular signalling molecules through their Toll-like/interleukin-1 receptor (TIR) domain, leading to the activation of the inflammatory response.9
Moreover, it was reported that paediatric patients, with rare mutations on the IRAK4 gene, experienced recurrent Gram-positive infections and that their leukocytes were hyporesponsive to TLR ligands in vitro.16
The fact that, in this particular case, the same polymorphism variation on IRAK4 gene [(c.1882G>A (p.Ala428Thr) in heterozygosis] was found (and that it was previously described as being associated with an increased risk of Gram positive infection at admission to an Intensive Care Unit of a Central Hospital in Canada9) raises interesting questions and doubts about the role of genetics in the host response and infection of the maxillary sinus.
We should be aware that the main therapeutic target is to restore disturbed sinus function and eliminate local infection.2,5 The maxillary sinus infection treatment procedures recommended by classical literature include: cleaning and sinus puncture (from the inferior meatus and in some situations by ostium) and intra-nasal antrostomy, enabling drainage and air-flow through an orifice (when there is failure in the above method).2,17
Endoscopic sinus surgery should be the most indicated surgical procedure to treat maxillary sinusitis of dental origin. However, this procedure implies several risks, including injury to vital structures. Therefore, according to other authors, it should be mandatory for a dentist to seek the participation of an experienced and trained otolaryngologist.18
In this case, we chose this approach in order to have an atraumatic and conservative, as possible, surgery allowing the total excision of the cyst.
Despite the odontogenic treatment and the surgical drainage establishing an important part of the entire therapeutic attitude, the antimicrobial therapy should be also an essential part in the management of patients with odontogenic sinusitis, and antibiotics are mandatory for 14–21 days.19
ConclusionCT requirement must be considered in patients with persistent maxillary sinus symptoms, in order to identify an odontogenic reason for the sinusitis. The treatment of odontogenic origin sinusitis comprehends the abolition of the dental underlying factors and the management of the maxillary sinus infection. More studies are needed, with larger samples, to clarify the role of the genetic variations in the IRAK4 gene on the host response to bacterial challenge in the odontogenic sinusitis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.