This study discusses the treatment of an inflammatory cystic lesion in mixed dentition that was successfully managed by the classical combined surgical–orthodontic approach. The marsupialization technique was used with the dual purpose of carrying out an incisional biopsy and decompressing the lesion. Complementary 4-year orthodontic therapy resulted in the esthetic and functional alignment of the involved permanent teeth. The study also discusses the pathogenesis of this kind of lesion which can be considered either a radicular or dentigerous cyst. The authors raise doubts about the rarity of radicular cysts associated with primary teeth and emphasize that the traditional criteria used for diagnosing radicular cysts of deciduous teeth as well as those of inflammatory dentigerous cysts must be revisited.
Este estudo refere-se a uma lesão cística inflamatória na dentição mista que foi satisfatoriamente tratada por meio por meio da clássica abordagem cirúrgica-ortodôntica. A técnica da marsupialização foi utilizada com o propósito duplo de realizar a biópsia incisional e também promover a descompressão da lesão. O tratamento ortodôntico complementar com duração de 4 anos resultou em alinhamento estético e funcional dos dentes permanentes envolvidos. O estudo também discute a patogénese e a dificuldade para diagnosticar esse tipo de lesão que tanto pode ser considerado um cisto radicular como um cisto dentígero. Os autores levantam uma dúvida sobre a raridade dos cistos radiculares associados ao dentes decíduos e enfatizam que os tradicionais critérios diagnósticos usados para diferenciar esses dois tipos de lesões precisam ser revistos.
Intra-osseous radiolucent lesions can be frequently encountered in jaws of children and adolescents. These lesions can produce signs and symptoms of pain, swelling and facial asymmetry or otherwise they can be detected by routine radiographic examination.1
A recent retrospective analysis of 26 years stated that the most frequent intra-osseous lesions encountered in children were radicular and dentigerous cysts. Keratocysts, apical granulomas, odontomas, fibrous dysplasia and malignant lesions were reported as well in a very low prevalence.2
Most of the osteolytic lesions observed in children have inflammatory origin and arise as consequence of progression of caries in the deciduous teeth. As the primary molars have a great susceptibility to caries, it is quite common to observe periapical radiolucency relating to primary molars, particularly mandibular molars.3 In the transitional dentition, these radiolucencies are located in the interradicular area intimately associated with follicle of premolars. Depending on the time of diagnosis, the radiolucent lesions of transitional dentition can be misdiagnosed as periapical granulomas or radicular cyst of primary teeth or dentigerous cyst from permanent successors.4
The purpose of this paper is to present a cystic maxillary lesion in a child that was successfully treated with combined surgical–orthodontic approach after 4 years of follow-up. Furthermore, we discuss the difficulty to establish the correct diagnosis of these inflammatory cystic lesions of mixed dentition that can be considered either radicular cysts from primary molars as inflammatory dentigerous cysts from permanent premolars.
Case reportA 10-year-old girl was referred to our out-patient clinic with an eight-month history of painless swelling in the right side of the maxilla. The patient's medical history was noncontributory. Extraoral examination showed slight facial asymmetry (Fig. 1). The intraoral examination revealed a bluish swelling in right primary molars region and tilting of the right permanent lateral incisor (Fig. 2). Exploratory punction-aspiration produced a bloody liquid. The first and second primary molars (54 and 55) were restored with amalgam fillings. The pulp vitality test was negative in 54.
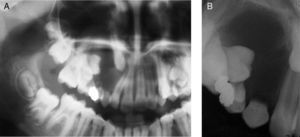
A panoramic and periapical radiographs showed a well-defined radiolucency involving the apices of right maxillary primary teeth, extending from 53 to 55 anteroposteriorly. There was considerable displacement of the permanent teeth, especially the right upper cuspid that was located near to the floor of orbit (Fig. 3). On the basis of clinical and radiographic findings, a provisional diagnosis of inflammatory cystic lesion was made, although the adenomatoid odontogenic tumor was also considered as diagnostic hypothesis.
Bearing in mind the requirement to obtain a fragment of the lesion to microscopic analysis, the major diagnostic hypothesis of inflammatory cyst and the maintenance of the permanent teeth, a conservative approach was planned. Under local anesthesia, the marsupialization technique was performed by: extraction of the right deciduous canine and first and second deciduous molars; and removal of parts of the lesion and suture (Fig. 4). Postsurgical period was uneventful.
Histopathological analysis showed features compatible with inflammatory cyst, revealing a cystic cavity lined by nonkeratinized stratified squamous epithelium, with elongated rete pegs and mixed inflammatory infiltration present in the wall as well in the epithelium. The cystic wall exhibited great amount of collagen fibers, fibroblasts and blood vessels (Fig. 5).
The patient underwent steady 6 months basis radiographic follow-up and orthodontic therapy. After 40 months, there were no clinical and radiographic signs of recurrence of the lesion and the involved permanent teeth could be preserved and kept in an esthetic and functional occlusal relationship (Figs. 6 and 7).
The transitional dentition provides an environment to a very special situation in the field of oral diseases that is the occurrence of radiolucent lesions involving either the periapical area of nonvital deciduous molars as the crown of unerupted permanent premolars. Although the radicular cysts arising from primary teeth are considered rare,5 we can assume that those inflammatory radiolucent lesions can be either radicular cysts from deciduous molars as dentigerous cysts of permanent premolars.
During the years, the osteolytic lesions formed around crown of unerupted premolars in transitional dentition were considered as dentigerous cysts.6–9 These authors regard that these cysts develop by extrafollicular pathway in which stimuli from the overlying necrotic deciduous teeth causes separation of reduced enamel epithelium from the enamel with resultant cyst formation.10 These statements add an inflammatory origin to dentigerous cysts that are characteristically conceived as developmental cysts. The World Health Organization establishes that dentigerous cyst develops by accumulation of fluid between the reduced enamel epithelium and the crown, not by inflammatory stimulus.11
By means of an accurate analysis of ancient and current studies about this issue, we cannot state undoubtedly that all radiolucent lesions described by Bloch-Jorgensen, Azaz and Shteyer, Shaw et al., Benn and Altini, and Shibata et al. can be addressed as dentigerous cysts. Some of them6–8 are reports of few cases in which there are no strong criteria to differential diagnostic between radicular and dentigerous cyst. Shaw et al.8 hypothesized that “If a primary periradicular cyst were to develop in the path of developing successor, it is likely that union of the follicle and cyst would take place, resulting in a continuity of the reduced enamel epithelium and cyst lining” Herein these authors were considering the possibility that “dentigerous cysts” of mixed dentition develop from the progression of preexisting radicular cyst.
Benn and Altini10 performed a clinicopathologic study of fifteen cases classified as dentigerous cysts of inflammatory origin based on clinical, radiographic and microscopic findings. The microscopic findings showed extended parts of cystic wall lined by a 2–3 cell layer thick cuboidal epithelium similar to reduced enamel. This epithelium fused with hyperplastic nonkeratinized stratified squamous epithelium of variable thickness, sometimes with anastomosing rete pegs. Many cases were lined entirely by this hyperplastic epithelium and could not be differentiated from radicular cysts. The authors defended the hypothesis that formation of dentigerous cysts occurred as a result of chronic inflammatory exudate from nonvital primary teeth that caused separation of reduced enamel epithelium in the unerupted teeth. Even so, the article regards the possibility that radicular cysts developed at the apices of the nonvital deciduous teeth enlarged and merged with the follicle of unerupted successors.
Radicular cysts are the most common cysts found in the jaws. They develop when a pulpal inflammation spreads to the periapical or lateral radicular area and cause proliferation of the epithelial residues in the periodontal ligament (rest of Malassez) leading to the formation of an epithelium-lined cystic cavity.11 Although the developmental mechanisms of radicular cysts are identical in the primary and permanent dentitions, radicular cysts arising from primary teeth are considered extremely rare. Lustmann and Shear5 found only 7 cases of them in a series of 1300 radicular cysts (0.5%) over a period of 25 years.
This rarity of occurrence of radicular cyst in deciduous teeth was declined by Mass et al.3 which analyzed 49 primary molars with radiolucent lesions. 73.5% of the lesions were diagnosed as radicular cysts, and 26.5% as granulomas. The authors reinforced that radicular cysts associated with deciduous teeth are not rare, but indeed low reported in the literature. These lesions tend to be neglected and mostly resolve after removal of the tooth, without pathological examination. Several factors can be implicated in the high formation of radicular cyst in the primary molars: High prevalence of caries in primary molars, stimuli originating from pulpal therapeutic agents, the existence of accessory canals in the roots of primary molars, large number of epithelial rests in the environment of the mixed dentition and, finally, high proliferative activity of young people with mixed dentition.12–14
The clinical, radiographic and microscopic features of osteolytic lesion described in this article allow us categorize it as an inflammatory cystic lesion, more probably, as a radicular cyst arising from the nonvital first primary molar. The correct differentiation between a radicular and dentigerous cyst in mixed dentigerous is practically impossible on the basis of clinical, radiographic and microscopic grounds. In addition, we consider that the lack of involvement of the crown of the permanent successor in the cystic cavity must not be used as diagnostic criterion to radicular cyst, as stated by Lustmann and Shear.5 Thereby, we regard that radicular and dentigerous cyst in mixed dentition is in fact the same lesion in different stages of development.
Stoll et al.13 found differences in cytokeratin 7 immunoexpression between radicular and dentigerous which may be useful in differential diagnosis, but this issue deserves further investigation and the laboratory result will not alter the treatment choice. Some authors affirm that the unequivocal differentiation only can be accomplished if the specimen is submitted in entirety to the histopathological analysis.14 This approach requires a radical surgery involving enucleation of the lesion and extraction of permanent teeth that is not warranted in our opinion. In the present case, we successfully treated our patient by means a very conservative management combining marsupialization and orthodontic therapy as has been advocated for many studies.7,8,10,15
ConclusionThis case report describes a cystic lesion in a young patient that was successfully managed with a conservative approach after a long-term follow-up. Beyond of the simpleness of the case, the author discuss the terminology used and the difficulty to make a precise diagnosis of these common inflammatory lesions in the mixed dentition.
Ethical disclosuresConfidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
We are grateful to Dr. Rodrigo Fernando Souza Martins for photographic documentation.