To validate the quantitative method used in the evaluation of microleakage and to evaluate the microleakage of dental restorations using GCP Fill. The null hypothesis was that the restorative system doesn’t have any influence regarding microleakage.
MethodsSixty noncarious extracted human molars were cut in two equal halves occlusogingivally and Class V cavities were prepared on the buccal or lingual surfaces of each tooth. The specimens were randomly divided into 4 groups. Two were restored with GCP Fill, while another was restored with Filtek Supreme. The control group was not restored. The specimens were stored in distilled water at 37°C for 7 days before 500 cycles of thermocycling between 5°C and 55°C, dwell time of 30s. The specimens were submersed in a solution of 99mTc-pertechnetate for 3h and the radioactivity was determined. The nonparametric Kruskal–Wallis and Mann–Whitney test with Bonferroni correction at a significance level of 5% were used for statistical analyses.
ResultsThere were statistically significant differences between experimental groups and control groups (p<0.05). Apart from these differences, a significant difference was observed between negative and positive control groups (p<0.001). In the control+group there was a large microleakage, and the control-group received minimum counts.
ConclusionThe GCP Fill and the Filtek Supreme XTE do not differ as regards microleakage; this technique proved to be simple, quick and fulfilled the objective of a quantitative method in the evaluation of microleakage. Long-term clinical studies need to be carried out to substantiate these results.
Validar um método quantitativo de medição da microinfiltração e avaliar a microinfiltração de restaurações dentárias realizadas com GCP Fill. Considerou-se como hipótese nula que o material de restauração não tem influência na microinfiltração.
MétodosCortaram-se 60 molares humanos hígidos em duas partes iguais no sentido oclusogengival.e prepararam-se cavidades Classe V em cada metade. Os espécimes foram divididos aleatóriamente em 4 grupos. Em dois, foram restaurados com GCP Fill, noutro, com Filtek Supreme e no grupo controlo positivo não foram restaurados. Armazenaram-se os espécimes durante 7 dias em água destilada 37°C antes de serem termociclados em 500 ciclos (5°C e 55°C, 30 segundos em cada imersão). Submergiram-se numa solução de 99mTc-Pertechnetate durante 3 horas e contou-se a radioatividade. A análise estatística realizou-se recorrendo aos testes não paramétricos Kruskal-Wallis e Mann-Whitney com correção de Bonferroni, considerando-se o intervalo de significância de 5%.
Resultadosexiste diferença estatisticamente significativa entre os grupos de estudo e os grupos controlo (p<0.05). Existe diferença estatisticamente significativa entre o grupo controlo positivo e o grupo controlo negativo (p<0.001). A maior microinfiltração verificou-se no grupo controlo positivo enquanto que o grupo controlo negativo apresenta menores valores de contagens.
ConclusõesNão existem diferenças na microinfiltração entre as restaurações com GCP Fill e Filtek Supreme XTE; esta técnica provou ser simples e rápida e permite a avaliação quantitativa da microinfiltração. São necessários mais estudos clínicos para suportar os resultados deste trabalho.
Nowadays the use of minimal invasive cavities and aesthetic fillings are possible due to improvements in the techniques of adhesive dentistry.1 Composites and glass ionomer cements (GICs) have also been considerably improved in their aesthetic and mechanical properties.1,2
Composites fulfil a lot of basic requirements, such as aesthetics, good optical characteristics, wear resistance, and radiopacity; furthermore they are easy to handle and polish, tasteless, biocompatible and bondable to dental tissue.3 However, some clinical and material limitations have restricted the universal use of composites as posterior restorative material.4 When compared with GICs, they are more aesthetic and easy to polish and demonstrate better mechanical performances and surface integrity in the long term.5–8 However, GICs have some advantages.9,10 They allow marginal good sealing without microleakage,7,11,12 are less susceptible to moisture than composites and the rubber dam can be dispensed with.13–16 The use of these materials is reported with very few cases of postoperative sensitivity7,17,18 and they can release fluorides inducing remineralization of the surrounding calcified dental tissues.19–23 On the other hand some studies have demonstrated that GICs self-adhere to dental tissues, and this is also the case for resin modified glass ionomer cement (RMGIC), but this adhesion may be less effective than that obtained with a composite with adhesive systems.23–28 Also, several studies have tested RMGICs bonded to dentine with a self-etch adhesive system and concluded that the association enhanced bond strength.1,26,28 However, on analysing the systematic reviews of clinical trials there are some errors, which make some of these studies less reliable.29
Recently, a resin-modified glass-ionomer cement (RMGIC) was introduced in the market. GCP™ Fill (First Scientific Dental GmbH, Robert-Bosch-Strasse 26 D-25335 Elmshorn) incorporates fluoroaluminosilicate glass and polyacids, but has a different component embedded than the RMGICs, which is apatite.30
Microleakage is the clinically undetectable passage of bacteria, fluids, molecules and ions between the cavity wall and the restorative material4,31,32 and is considered to be a major factor influencing the longevity of dental restorations.4
One of the objective methods for microleakage rating is the use of radioactive isotopes. Technetium is an artificial element, obtained by the radioactive decay of molybdenum, which is a radioactive metallic element belonging to the transition metals with an atomic radius of 135.8pm. It is element 43 of the periodic table, and the radioactive element with the lowest atomic number. This presents a half-life of 2.6h. Its decay occurs by isometric transition and emission of 140.5keV of gamma radiation.33
The purpose of this study was to assess a quantitative method in the evaluation of microleakage and evaluate the microleakage of dental restorations using GCP Fill. The null hypothesis was that the type of restorative system does not have any influence regarding microleakage.
Materials and methodInstitutional Ethics Committee approval was obtained for this study. 30 noncarious extracted human molars were hand scaled, disinfected with chloramine-T and stored in normal saline solution 0.9% (B. Braun, 11496403, Queluz de Baixo) at 5°C no more than 4 months after extraction. The teeth were cut with an Exakt System 300 saw (Exakt System, 22851 Norderstedt, Germany) in two equal halves occlusogingivally. One standardized class V cavity was prepared with burs on the surface of each specimen. The cavity had the following dimensions 4mm mesiodistally, 3mm occlusogingivally and 3mm in depth. An internal line angle of 90 degrees was maintained to create occlusal and gingival margin walls with 1mm surrounded enamel. The burs FG 835/010 (Proclinic, 34/09, Nyon, Swiss) were replaced after every 5 preparations.
The specimens were divided in to four groups:
G1: a GCP™ Fill (lot n° 7107532, First Scientific Dental GmbH, Robert-Bosch-Strasse 26, D-25335 Elmshorn) shade A3 activated was used to restore the class V cavities of 20 specimens. The GCP Fill was placed in one bulk increment followed by shaping the buccal surface and light-curing for 60s using light-curing unit BluePhase™, 1500mW/cm2±10% (Ivoclar Vivadent, 5VDC, Liechtenstein). Restorations were polished using Sof-Lex Disc System (Brown/Orange/Light Orange/Yellow, 3M ESPE, N301289, St. Paul, MN, USA).
G2: a Filtek™ SupremeXTE (lot n° N339166, 3M ESPE, N339166, St. Paul, MN, USA) shade A2 was used to restore the class V cavities of 20 specimens. The enamel was conditioned for 30s with 35% phosphoric acid gel and washed immediately after with an air/water spray for 30s. A self-etch bond agent, Clearfil™ SE BOND (Kuraray, 041872, Okayama, Japan) was used according to manufacturer's instructions. Clearfil™ SE BOND primer was applied to the enamel/dentine using a scrubbing motion and dried thoroughly with mild airflow. Clearfil™ SE BOND was later applied to the enamel/dentine surface using a light brushing motion, dried with gentle air flow and cured for 10s using a light cure Blue Phase™ G2, 1500mW/cm2 and cavities were restored using the incremental technique. Restorations were polished as in the G1.
G3 (positive control group): the class V cavities of 10 specimens were not restored.
G4 (negative control group): a GCP™ Fill (First Scientific Dental GmbH, Robert-Bosch-Strasse 26, D-25335 Elmshorn) shade A3 activated was used to restore the class V cavities of 10 specimens as in G1. Restorations were polished using the same disc system.
After restorative procedures, that were performed by the same operator, the specimens were stored in distilled water at 37°C for one week and then they went through thermocycling with 500 cycles between 5°C and 55°C with a dwell time of 30s, and no further treatment. The specimens of groups 1, 2 and 3 were covered with two layers of red nail varnish up to 1mm from the margins around the restorations. The specimens of G4 were covered over the entire surface. The specimens of all groups were immersed in 99mTc-pertechnetate solution, for 3h. After which the varnish was removed. The radioactivity released by the specimens was detected by the gamma camera. Statistical analysis was done using the software IBM® SPSS® Statistics, version 20.0 (IBM, Armonk, NY, USA). After acquiring the values of the average counts of each tooth, descriptive analysis for quantitative variables was represented as arithmetic mean±standard deviation. For inferential analysis, comparison between all groups was performed using the nonparametric Kruskal–Wallis test, since, although there was a normal distribution of the values obtained, there was no homogeneity of variances in order to apply one factor analysis of variance (ANOVA) test. Mann–Whitney test was used for pairwise comparisons, with a p-value correction according to Bonferroni. A statistical significance level of 0.05 was established.
ResultsThe means values of the microleakage average counts of each tooth ranged between 0.07±0.02cpm (G1 and G2) and 0.31±0.09cpm (G3).
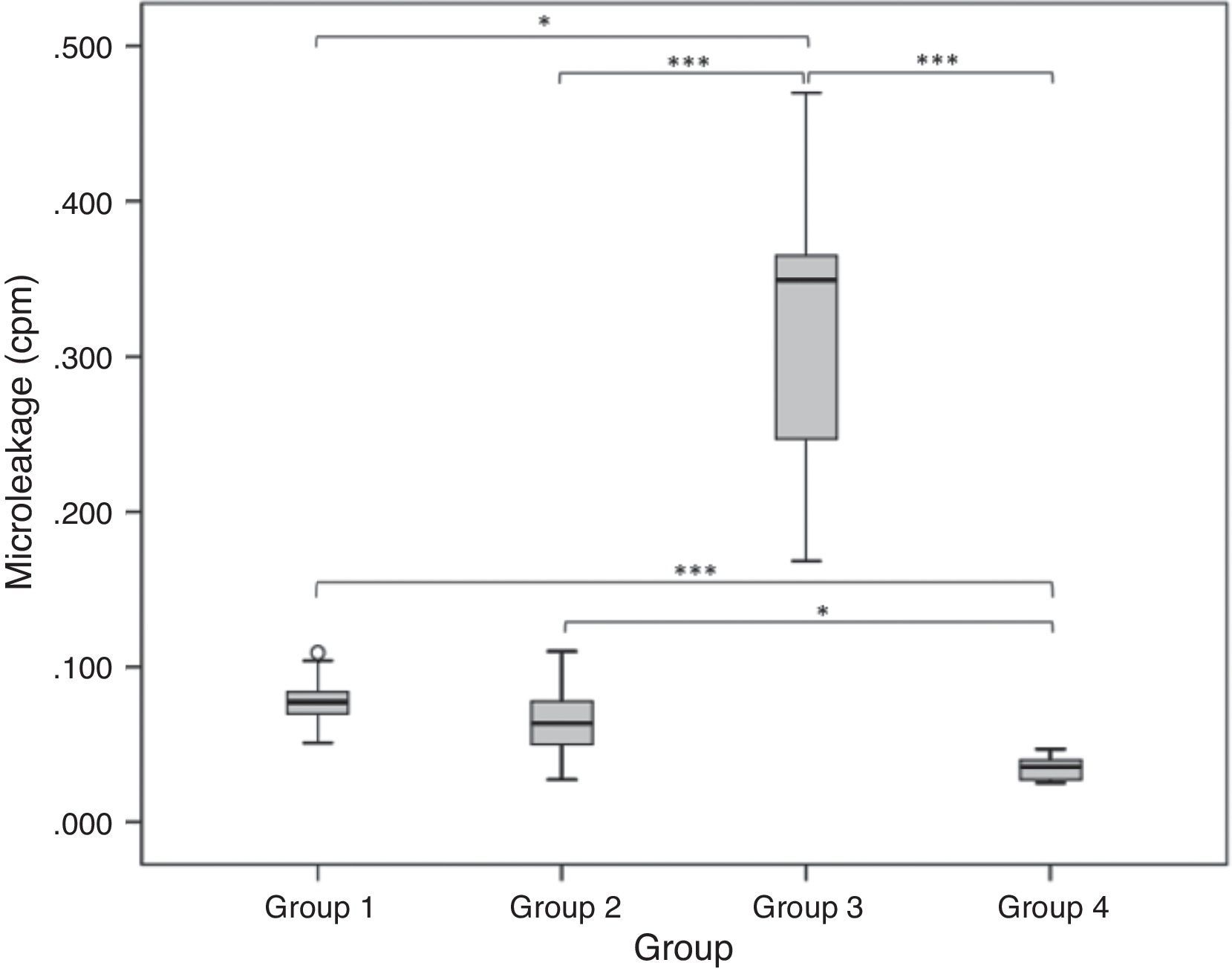
Data analysis presented statistically significant differences between experimental and control groups (p<0.05) (Fig. 1). Apart from these differences, a significant difference was observed between negative and positive control groups (p<0.001). In the positive control group there was a large count of 0.31±0.09cpm, and the negative control group received minimum counts 0.04±0.01cpm.
Regarding the comparison of scores obtained from G1 (0.07±0.02cpm) and G2 (0.07±0.02cpm), a significant statistical difference was not observed (p>0.05) (Fig. 1). The null hypothesis that the type of restorative system does not have any influence regarding microleakage was confirmed.
DiscussionThe integrity of the marginal seal is essential to increase the longevity of the restoration.34 That integrity is compromised when microleakage occurs resulting from polymerization shrinkage. As previously mentioned, polymerization shrinkage is the most common cause of failure of direct posterior composite restorations. Polymerization shrinkage is a very complex phenomenon dependent upon the boundary conditions, the amount of material in the polymerization reaction and the material's formulation.2
Different composites have different formulations and consequently different polymerization shrinkage. Many studies have suggested the use of an incremental layering technique to reduce this shrinkage.2,4,35 Nowadays, traditional placement techniques for composite resins include this technique.2 Most practitioners recommend placing composites in 2mm increments. However, every dentist who places posterior composite needs a material that can be used using a bulk fill technique.
The magnitude of the stress depends upon other factors, such as the configuration factor (C-factor) of the cavity and also the effect of light-curing mode. In our study the cavities had the same dimensions, the same C-factor, and the light-curing mode was the same for all the restoration specimens.36
In this study we use a composite, Filtek™ SupremeXTE, and a RMGIC bulk fill material GCP™ Fill. Filtek™ SupremeXTE is a nanocomposite that contains nanometric particles and nanoclusters, and presents high translucency, high polish and polish retention similar to microfilled composites and physical properties and wear resistance equivalent to several hybrid composites.37 GCP™ Fill incorporates fluoroaluminosilicate glass and polyacids, but has a different component embedded than the RMGICs, which is apatite.30
The success of composite restorations depends on the adhesion of restorative materials to hard tooth tissue. The adhesives have different tooth composite interface morphologies, different bond strengths and different abilities in microleakage prevention.38 To promote adhesion of the composite to enamel and dentine, a two-step self-etch adhesive was chosen, Clearfil™ SE BOND. Self-etch adhesive systems promote the dissolution of the inorganic phase of dentine using an acidic monomer, with simultaneous infiltration of adhesive monomer around the collagen network that results in fewer exposed collagen fibrils.39 According to previous studies these adhesive systems have the advantage of saving time, reducing procedural errors and with their lower etching ability, decreasing the potential for iatrogenic damage to dental hard tissue.40 Some authors advocate that Clearfil™ SE BOND presents significantly higher bond strengths than other self-etching adhesives.41 The enamel was etched previously with 35% phosphoric acid gel, increasing the bond strengths significantly.42
Posteriorly, cavities in G1 and G4 were restored with a single increment of GCP™ Fill, as recommended by the manufacturer; and cavities in G2 were restored with Filtek™ SupremeXTE using the incremental technique, recommended by several authors.2,43,44 According to previous studies, the use of an incremental filling technique reduces the cuspal deflection resultant from polymerization shrinkage. Nevertheless the literature is not conclusive concerning the advantages promoted by the incremental technique. Others authors45–47 argue that the incremental filling technique produces higher polymerization stresses at the restoration interface compared with bulk fill. In spite of that, GICs and RMGIs allow a good marginal sealing without microleakage.7,11,12,23,26,27
The same operator performed all restorative procedures, to reduce human operator error, as some authors have recommended.31,35,48,49 The specimens were stored in distilled water at 37°C for one week3,33 before 500 cycles thermocycling between 5°C and 55°C with a dwell time of 30s.31,39,47,50,51 The materials’ restorations are exposed to various influences in the oral cavity, and therefore to evaluate microleakage, methods to reproduce these features are required. Storage in water is the most common artificial ageing technique.39,40 Another widely used method is thermocycling.32,40 Thermocycling is the only in vitro test for stimulating thermal stress in teeth,1 simulating the introduction of hot and cold extremes in the oral cavity and shows the relationship of the linear coefficient of thermal expansion between tooth tissues and restorative materials.52,53 The International Organization for Standardization (ISO) TR 11450 standard (1994) indicates a thermocycling regimen comprising 500 cycles in water between 5°C and 55°C. However, some authors report that this number of cycles is probably too low to achieve a realistic ageing effect.39,40
In order to prevent the infiltration of the isotope, two coats of varnish were placed on the surface of the tooth up to 1mm from margins around the restorations, except in group 4 where the entire surface was sealed.4,54,55 The negative control in this experiment was intended to evaluate the reliability of the varnish, with regard to sealing, and this has been proven by the low scores in this group.
There are several methods by which microleakage can be studied such as the use of dyes, chemical tracers, radioactive isotopes, artificial caries, scanning electron microscopy, neutron activation analysis, and electrical conductivity.32 In this study the radionuclide 99mTc was used due to the fact that this is the most widely used radionuclide in the field of nuclear medicine. This radionuclide was selected as it is the most used among the cold kits in the field of nuclear medicine for single photon emission, in addition to the fact of its half-decay time being approximately 6h.33,54,55 The immersion time of the teeth in the solution of sodium pertechnetate was set at 3h in order to have time for the foregoing procedures to measure the radiation by gamma camera. The samples were carefully prepared for quantification by gamma camera after immersion to prevent possible contamination after the immersion time. A gamma camera provided accurate radioactivity results in each sample.
When analysing the results, a statistically significant difference was observed between the control groups and study groups, demonstrating that they were effective.
Both restorative materials tested presented microleakage. In this study there was no statistically significant difference between the study groups. However, more microleakage occurred in G1. Between the negative control group and positive control group a highly significant difference was found. Analysing the mean and standard deviation reveals that the negative control group presented the lowest values, while the positive control group showed the highest values.
ConclusionsWithin the limitations of this study, it can be concluded that: the GCP™ Fill and the Filtek™ Supreme XTE do not differ as regarding microleakage; this technique proved to be simple, quick and fulfilled the objective of a quantitative method in the evaluation of microleakage.
Long-term clinical studies need to be carried out to substantiate the results of this study.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
To our colleagues Pedro Ambrósio, Carlos Marto, Diana Rebelo and Joana Marques for their help, during the experimental work.