One-appointment procedure is an endodontic therapy protocol that has been growing in popularity among clinicians and patients. It definitely brings many advantages in clinical management and in relating to the patients’ needs. When accepting a one-appointment procedure the clinician assumes that the long term prognosis mirrors the multi-appointment procedure. The aim of this work is to analyze and evaluate if this assumption is correct when bacterial infection is present. The relevant literature on one-appointment versus multi-appointment endodontic treatment on teeth with apical periodontitis up to December of 2010 was reviewed using PubMed database searches. The literature was searched regarding the following topics: periapical healing, bacterial elimination, histological studies, bacterial endotoxins elimination and post-operative pain. An analysis of the treatment protocol and concept differences between both treatments and an overall discussion are also presented. There is a general agreement on the need of an effective bacteriological control. Although more studies are required to support the one- versus multiple-appointment procedure.
Os protocolos em sessões únicas têm crescido em popularidade entre clínicos e pacientes. Definitivamente traz algumas vantagens na gestão da clínica e relacionamento com os pacientes. Parte-se do princípio que quando se decide avançar para um protocolo em sessão única o clínico assume que o prognóstico a longo prazo é similar ao das sessões múltiplas. O objetivo deste trabalho é analisar e avaliar se essa suposição está correta quando uma infeção bacteriana está presente. A literatura relevante sobre sessão única vs sessões múltiplas em tratamentos endodônticos em dentes com patologia apical até Dezembro de 2010 foi revista utilizando a base de dados da PubMed. A pesquisa da literatura focou os seguintes tópicos: cura de lesões apicais, eliminação bacteriana, estudos histológicos, eliminação de endotoxinas bacterianas e dor pós operatória. Uma análise entre as diferenças de protocolo e conceitos de ambos os tratamentos e uma discussão geral são também apresentados. Existe consenso relativamente à necessidade de um eficiente controlo bacteriano. No entanto, mais estudos são necessários para apoiar a sessão única versus sessões múltiplas.
During the past four decades there has been a tendency for choosing the one-appointment procedure instead of the multi-appointment procedure for root canal treatment.1 It became a kind of a criterion of quality for the professionals who work in the endodontic field. But can it really be classified as a criterion of success? It is definitely a criterion of skills, but are those skills being used to achieve the maximum success in the outcomes of the treatments? Rather than debating the effectiveness of endodontic treatment based on number of appointments, we should focus on the biological aspects of treatment effectiveness.2
The best scientific evidence-based documented procedure for the best outcome in endodontic treatment is based on the maximum disinfection of the root canal system.3 Sjögren et al.4 have proposed the following protocol to achieve a reliable result: the full debridement, instrumentation and disinfection of the root canal done at the first appointment, followed by an intracanal application of a dressing of calcium hydroxide for one week and finally the obturation of the root canal system at the second appointment.
Reducing the number of visits to only one brings several practice management advantages. It is less stressful and only one anesthesia is needed, which makes it very well accepted by the patient, is less time-consuming, reduces the risk of inter-appointment contaminations, is less expensive and is more productive for the clinician. But the question is: is the same outcome achieved?
The purpose of this paper is to review some arguments that are the basis for both points of view. A literature search was performed on PubMed database up to December of 2010.
Treatment protocol and concept differences between one- and multi-appointment procedureThe presence of bacteria inside the root canal system results in the development of periapical lesions.5 Are both options, one or multiple appointments, similar concerning the elimination of those bacteria from the root canals?
The traditional multi-appointment protocol is based on the need to use extra disinfecting agents besides the irrigants used during the cleaning and shaping.4 Several intracanal dressings have been proposed, such as iodine potassium iodide, camphorated p-monochorophenol or chlorhexidine gel, but the most researched and widely used is the calcium hydroxide paste.6 There are two main advantages of the use of calcium hydroxide paste: the capacity to act as a physical barrier that blocks the coronal leakage of the temporary fillings, which inhibits the inter-appointment contamination; and the low solubility of the medicine, which allows the slow release of the hydroxyl ions, giving it a longer antimicrobial capacity and prolonging effectiveness for several weeks. In 2004, Law and Messer6 reviewed the published literature about the intracanal medication. It was part of the inclusion criteria for the study that all the papers should have microbiological sampling before the treatment (S1), after cleaning, shaping and irrigation (S2) and after canal medication (S3). Five studies in a total of 164 teeth were included in the research. At S2, 62% of the canals were bacteria positive, and at S3 27% still had bacteria growth. It was concluded that cleaning, shaping and irrigation are not capable of eliminating all the bacteria, and although calcium hydroxide was not fully efficient, it helped to reduce the bacteria remaining in the canal after the irrigation. The same conclusion was achieved in a meta-analysis by Sathorn et al.7
On the other hand the one-appointment protocol eliminates the intracanal medication. This option is based on the entomb theory.8 It is accepted that the cleaning, shaping and irrigation of the root canal system in one session is not enough to eradicate all the bacteria. It is acknowledged that the intracanal medication would improve the disinfection, but is also argued that those bacteria are reduced to a lower level that allows the success. The entomb theory defends that, after the obturation, a low concentration of the surviving bacteria remain inside the canal but stay imprisoned inside the dentinal tubules and isthmus, and with the lack of nutrients, these bacteria finally die.
Periapical healingThe simplest way to compare both treatment options is to analyze them using a healed or not healed outcome. The short- or long-term follow-up of the bone radiographic image and size of the lesion is the most commonly used technique to evaluate the healing, usually based on the PAI score developed by Orstavik et al.9
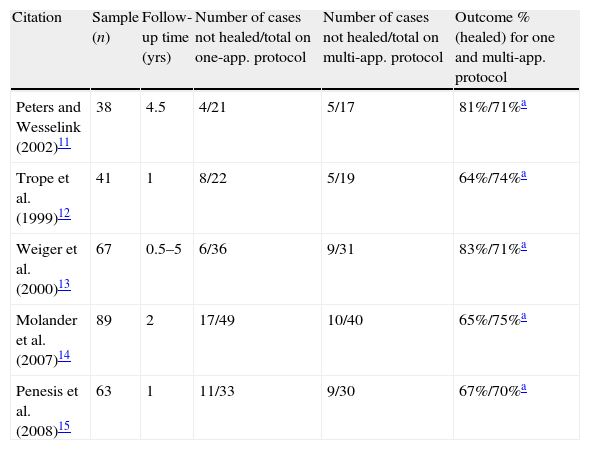
The number of studies that compare both techniques for a legitimate and credible follow-up time are not many compared to the mature evidence base that supports the use of intracanal medicines. With the purpose of reinforcing the statistical power of the few papers published, Sathorn et al.10 produced, in 2005, a meta-analysis about this subject. From the preliminary pool of 196 papers only a small number of 3 were accepted as having all the inclusion criteria needed. The studies selected were the ones of Peters and Wesselink,11 Trope el al.12 and Weiger et al.13 All these studies have small sample numbers, between 38 and 67 cases, and were followed up for a period of 6 months to 5 years. All the three studies individually recognized that it was not possible to find a statistically significant difference in the outcome between both protocols. Trope et al.12 suggests that this probably happens because the number of cases is not big enough to achieve statistical significance.
In Sathorn's meta-analysis the number of cases of the three combined studies was 146 cases. It was still not possible to achieve a statistically significant difference between the outcomes of both protocols. Using these three papers as evidence it is not possible to support the biological advantage of using the intracanal medication over the one-appointment protocol. Other recent studies support these results14,15 (Table 1).
Outcomes comparing one and multiple appointments protocols.
| Citation | Sample (n) | Follow-up time (yrs) | Number of cases not healed/total on one-app. protocol | Number of cases not healed/total on multi-app. protocol | Outcome % (healed) for one and multi-app. protocol |
| Peters and Wesselink (2002)11 | 38 | 4.5 | 4/21 | 5/17 | 81%/71%a |
| Trope et al. (1999)12 | 41 | 1 | 8/22 | 5/19 | 64%/74%a |
| Weiger et al. (2000)13 | 67 | 0.5–5 | 6/36 | 9/31 | 83%/71%a |
| Molander et al. (2007)14 | 89 | 2 | 17/49 | 10/40 | 65%/75%a |
| Penesis et al. (2008)15 | 63 | 1 | 11/33 | 9/30 | 67%/70%a |
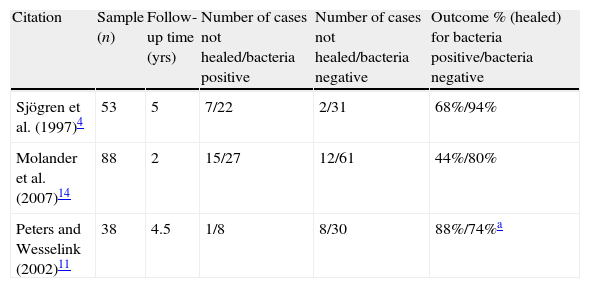
On the other hand, there is microbiological analysis. Sjögren et al.3 published a study where 55 cases of teeth with apical periodontitis were cleaned, shaped and disinfected with 0.5% sodium hypochlorite and filled on one-appointment protocol. Bacterial samples were collected from the canal before the final filling. A 5-years follow-up was carried out. Of the original 55 cases, 22 cases (40%) were still bacteria positive, these 22 cases had a 68% success rate. The other 33 cases (60%) were bacteria negative and had a success rate of 94%. This difference of 26% between outcomes had statistical significance.
It is important to understand that with apical periodontitis, all the canals were bacteria positive even after irrigation and intracanal medication. A canal referred to as bacteria negative means that the bacteria concentration is so small that it may not be possible to collect or culture, but it is possible that the bacteria still remain there.
Molander et al.14 compared both one- and multi-session protocols and conclude that the outcomes are similar and without statistical significance. He also sampled the canals before filling. The bacteria negative cases achieved a favorable outcome of 80%; 30% of the cases were bacteria positive and had a healing outcome of 44%.
Peters and Wesselink's11 study shows no statistical significance between one- and multi-appointment protocols, and no correlation between the healing of periapical lesions and the presence or absence of a positive bacteria growth after the cleaning, shaping and irrigation (Table 2).
Outcomes comparing bacteria positive or negative teeth before filling.
| Citation | Sample (n) | Follow-up time (yrs) | Number of cases not healed/bacteria positive | Number of cases not healed/bacteria negative | Outcome % (healed) for bacteria positive/bacteria negative |
| Sjögren et al. (1997)4 | 53 | 5 | 7/22 | 2/31 | 68%/94% |
| Molander et al. (2007)14 | 88 | 2 | 15/27 | 12/61 | 44%/80% |
| Peters and Wesselink (2002)11 | 38 | 4.5 | 1/8 | 8/30 | 88%/74%a |
The previously discussed papers were all based on a periapical radiograph follow-up analysis. It has been argued that the periapical radiographs give limited information because of the two-dimensional nature of the image and may present anatomic and geometric distortion.16 Recent studies have shown that the cone-beam technology can diagnose periapical lesion more accurately.17,18 A recent work from Paula-Silva et al19 has compared the favorable outcome of the one-visit and two-visit procedures on dog's teeth with apical pathology determined by periapical radiographs and cone-beam computed tomography scans. Favorable outcomes occurred more frequently on the two-visit procedure when determined by cone-beam technology. When the periapical radiograph was used to follow-up the lesion evolution the difference was not statistically significant. It was concluded that the cone-beam technology is superior to periapical radiographs to detect periapical disease, and that the cone-beam was able to show a more favorable outcome on the two-visit therapy compared to one-visit therapy.
Histological studiesThe PAI score9 may be a good measurement technique but it is based on an image of two dimensions, and the same angle of the periapical radiograph shoot may be difficult to reproduce. There was a need to check in situ the evolution of both protocols. The problem arises when checking in situ means doing a biopsy, which is something impossible to do in human clinical studies. Hence, the animal studies are performed.
Holland et al.20 studied the histological healing process of teeth with apical periodontitis after root canal treatments were performed in one and two sessions. Their protocol included the use of 2.5% sodium hypochlorite and EDTA in the irrigation process and the use of calcium hydroxide for 7 and 14 days in the two-session protocol. After 6-months follow-up the animals were killed. The histomorphological analysis showed that the protocol with calcium hydroxide had better periodontal ligament organization and less inflammatory cells. It was concluded that calcium hydroxide dressing contributed to better results in treating dog teeth with apical periodontitis than the protocol of one session.
Katebzadeh et al.21 and Silveira et al.22 performed two other similar studies with similar results.
Bacterial endotoxins eliminationMicrobiological studies report that there is a prevalence of anaerobic gram-negative bacteria population in the root canal system of necrotic teeth with apical periodontitis.23,24 One of the components of the gram-negative bacteria cell wall is the lipopolysaccharide (LPS), a powerful endotoxin capable of having a strong toxic action over the periapical tissues.25–28 LPS has been reported as having a major role in periapical bone resorption process, having a direct effect on the stimulation of prostaglandin E2 secretion25 and inducing the osteoclast formation.26 LPS also stimulates the macrophages to release cytokines such as tumor necrosis factor (TNF) and several interleukins (IL) that are important inflammatory mediators. Signs and symptoms such as spontaneous pain, pain on palpation and tenderness to percussion have also been associated with the presence of endotoxins in the root canal system.27,28
The LPS are released, from the bacterial cell wall, during cell duplication and as result of cell lysis, for example, during bacterial death due to intracanal disinfection.25,29
Therefore, the objective of root canal treatment on necrotic teeth should be not only the elimination of living bacteria but also the inactivation of the toxic effects of bacterial endotoxins.
The main source of toxicity of LPS is a lipid-A component. Safavi and Nichols25,29 have shown that a structure-induced change on this component is able to inactivate it. The ester bonds of the lipid-A may be broken down by alkaline hydrolysis with calcium hydroxide.
Tanomaru et al.30 have tested, in vivo, the effect of different concentrations of sodium hypochlorite, 2% chlorhexidine and calcium hydroxide and concluded that the irrigation solutions were ineffective against LPS, while the intracanal medication dressing with calcium hydroxide appeared to inactivate the cytotoxic effects of the endotoxin. Another other study28 concluded that after the complete chemomechanical preparation with 2.5% sodium hypochlorite a mean reduction of only 59.99% of endotoxins was achieved.
Khan et al.31 decided to test the ability of calcium hydroxide to denature the pro-inflammatory mediators induced by LPS. They reported the ability of calcium hydroxide to denature IL-1α, TNFα and calcitonin gene-related peptide (CGRP) by 50–100%. A recent study by Paula-Silva et al32 showed that the use of calcium hydroxide canal dressing can reduce the expression of matrix metalloproteinases (MMPs), a major class of enzymes responsible for degradation of extracellular matrix components. These MMPs are destructive enzymes that are activated by bacterial components.32
Another other study reports the ability of calcium hydroxide to detoxify the lipoteichoic acid from Enterococcus faecalis.33
The inhibition of the activity of the bone resorption inducer LPS and the denaturation of its pro-inflammatory mediators might be two of the mechanisms by which the intracanal medication with calcium hydroxide may favor the periapical healing.
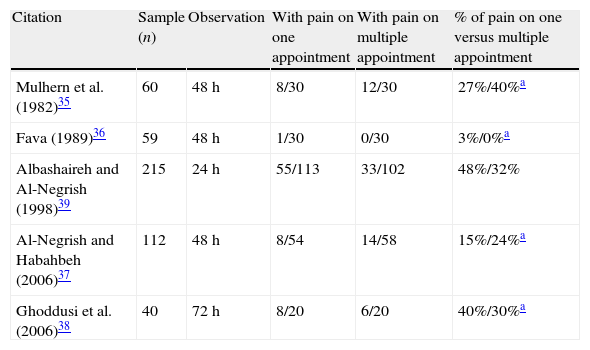
Post-operative painPost-operative pain after an endodontic procedure is usually related to the presence of periapical inflammation, which may be the result of over-instrumentation, over-filling, passage of medicine or infected debris into the periapical tissues, damage of the vital neural or pulp tissues or central sensitization.34
Several studies have found no difference in the incidence of post-operative pain.35–38 Interestingly Mulhern et al.35 stated that there was an equal incidence of discomfort but the type of analgesic used to control that discomfort was stronger during one-appointment treatment when compared to the mild analgesics or no medication taken to control the discomfort on multi-appointment procedure. Ghoddusi et al.38 also stated that the incidence of discomfort was similar in both procedures, but the discomfort during single-appointment protocol was more severe and had more swelling than the multi-appointment procedure. On the other hand, the Al-Negrish and Habahbeh37 study stated that the flare-up incidence between single- and multiple-appointments was non-significant (Table 3).
Post-operative pain on necrotic teeth after one or multiple appointment endodontics therapy.
| Citation | Sample (n) | Observation | With pain on one appointment | With pain on multiple appointment | % of pain on one versus multiple appointment |
| Mulhern et al. (1982)35 | 60 | 48h | 8/30 | 12/30 | 27%/40%a |
| Fava (1989)36 | 59 | 48h | 1/30 | 0/30 | 3%/0%a |
| Albashaireh and Al-Negrish (1998)39 | 215 | 24h | 55/113 | 33/102 | 48%/32% |
| Al-Negrish and Habahbeh (2006)37 | 112 | 48h | 8/54 | 14/58 | 15%/24%a |
| Ghoddusi et al. (2006)38 | 40 | 72h | 8/20 | 6/20 | 40%/30%a |
Apparently there is not much of a difference in the incident of post-operative pain. However some studies state that the pain may be more severe for the one-appointment protocol.
DiscussionIn dentistry and medicine the standard by which treatment methods are compared is the long-term outcome.40 In medical science the cause-effect relationship is the basic theory that justifies the medical procedures that eliminate the cause to achieve the healing of a disease meaning the resolution of the effect. Only in very rare situations the medical objective is not the elimination of the etiology of the pathology. Incurable diseases such as Multiple Sclerosis or AIDS may have therapies that consist of controlling the evolution of the disease. Palliative care also provides a control of the quality of life and not a cure. Besides these specific situations the objective of medicine is always to achieve the resolution of the effect by elimination of the cause.
Having the bacteria inside the canal as the etiology or the cause means having the apical periodontitis as the disease or the effect. The aim of the endodontic therapy to achieve the resolution of the disease means elimination of the etiology, which means elimination of bacteria. There is no room for incurable diseases or palliative care in endodontics. If a tooth is not treatable, the elimination of the cause implicates the extraction of that tooth so that the resolution of the disease, effect, can be achieved. This takes us back to the entomb theory. The idea of closing the bacteria inside the root canal system seems more a control of a disease rather than the cure of a disease.
The idea of retrograde closing is acceptable with apical surgery. The retrograde treatment is performed when the orthograde treatment is not capable of eliminating the etiology of the disease. However the apical surgery has to be faced as an all-or-nothing situation. It should be faced as the last option before the extraction, which is a different idea from the orthograde procedure whose objective is to eliminate the cause of the disease.
Knowing that some bacteria remain inside the root canal system takes us back, again, to the entomb theory. The question is: when to apply it? Or rephrasing the question: when to obturate the root canal system? The answer should be: when the maximum disinfection achievable is achieved, since the bacterial infection is the cause of endodontic pathology. The obturation of the root canal system has the aim of holding in the bacteria that may remain inside the canal after the disinfection, as a good crown restoration has the objective of holding the external bacteria from the saliva outside of the root canal system.
A new question is mandatory: which of the procedures, one or multiple appointments, is able to achieve the maximum disinfection achievable? Law and Messer's6 review paper puts forward the multiple appointments and the use of intracanal medication as a more reliable treatment concerning the elimination of the cause that provokes an apical pathology.
Waltimo et al.41 researched both one- and multi-session protocol and also sampled the canals. Four samples were removed per canal: (S1) on the access opening; (S2) after the final irrigation at the first appointment, of those canals, half were filled, and half were dressed with calcium hydroxide; (S3) after removing calcium hydroxide with saline at the beginning of the second appointment and (S4) after the final irrigation protocol with sodium hypochlorite at the second appointment. The research showed that S2 still had 22% of bacteria growth, S3 after calcium hydroxide had 33% but, after the second irrigation protocol, the final S4 had 0%. This proves that, in this study, the second irrigation protocol helped to destroy the remaining bacteria.
The bio-mathematical analyses are consistent in their reference to the bacteria negative canals having a higher success ratio than the bacteria positive canals4,14 and the multiple appointment procedure is able to achieve more negative canals.4,14 The histological scores also appear to favor the multiple appointment protocol.20–22
On the other hand, several recent studies have shown that the outcome is similar if we just face it as healed or not. These results are also consistent.11–15 These results may be a consequence of using simple root canal system anatomies as samples (single-rooted teeth or one root with a single canal on multi-rooted teeth). Another hypothesis is related to the concentration of bacteria that remain inside the canal: there is a chance that a minimum concentration of bacteria may allow the apical healing and a concentration over that may not. Further studies on minimum concentration of bacteria or more complex root canal anatomies are required. To strengthen the scientific evidence available, more studies with comparable methodologies are required.
Regardless of the number of sessions, an effective bacteriological control is mandatory. The biologic concerns should always be a priority.
Conflicts of interestThe authors have no conflicts of interest to declare.