To evaluate the reparability of CAD/CAM polymer materials with universal adhesive systems.
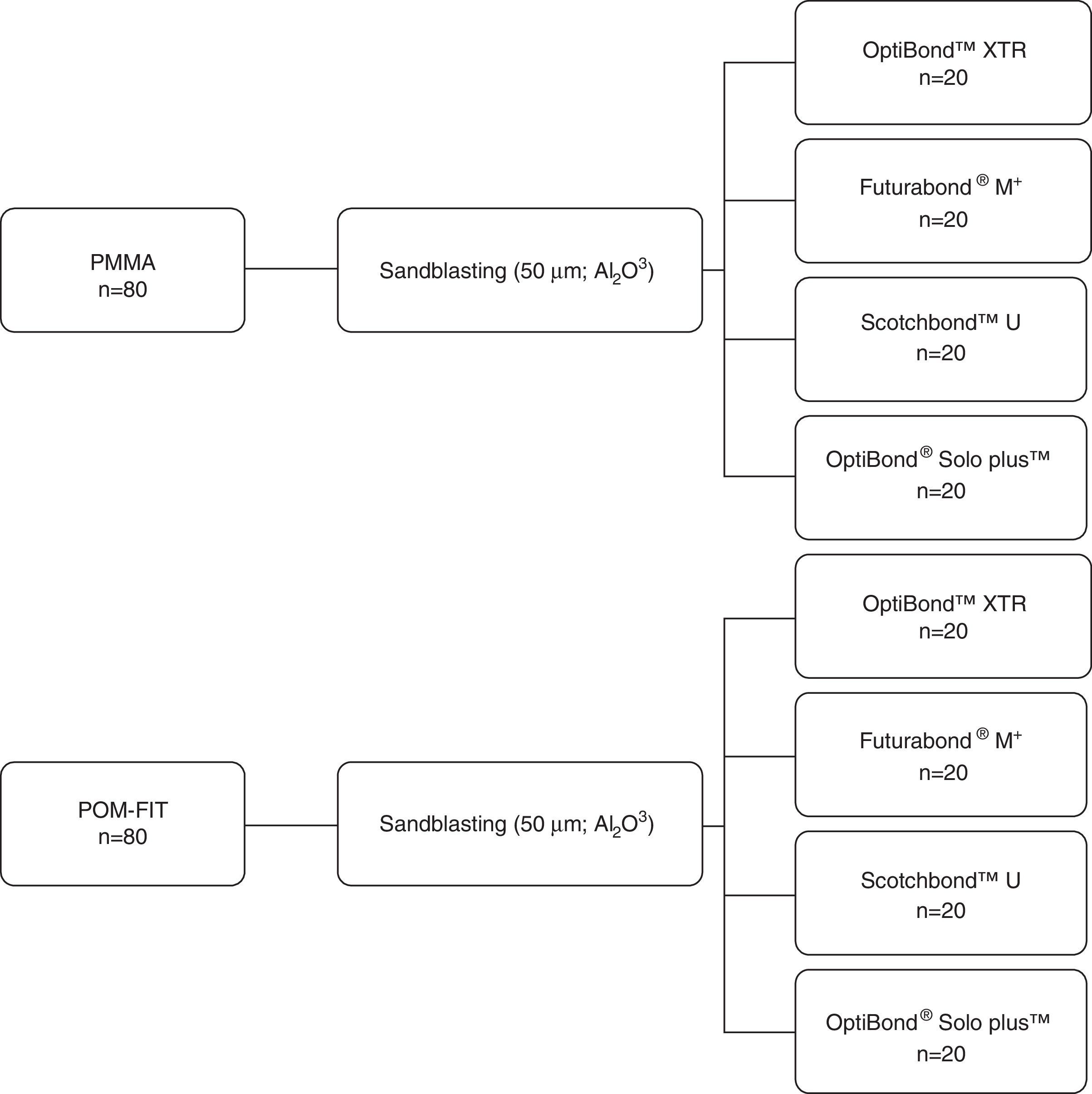
MethodsEighty blocks of polymethyl methacrylate (PMMA) and eighty blocks of polyoxymethylene (POM) were milled by the manufacturer (7mm of diameter and 4mm height). The top surface of all specimens was abraded with 50μm Al2O3. The 80 specimens of each material were randomly allocated to four experimental groups (n=20) according to the adhesive system used: OptiBond XTR, Futurabond M+, Scotchbond Universal or OptiBond Solo Plus. Each adhesive and the repairing composite resin (GrandioSO) were applied according the manufacturer's instructions. Specimens were stored in distilled water at 37°C for 48h and submitted to shear bond strength (SBS) tests. Fracture surfaces were observed and classified as: adhesive, cohesive or mixed type. SBS data were analysed with 2-way ANOVA and Kruskal–Wallis and Mann–Whitney tests were used to failure mode data (α=0.05).
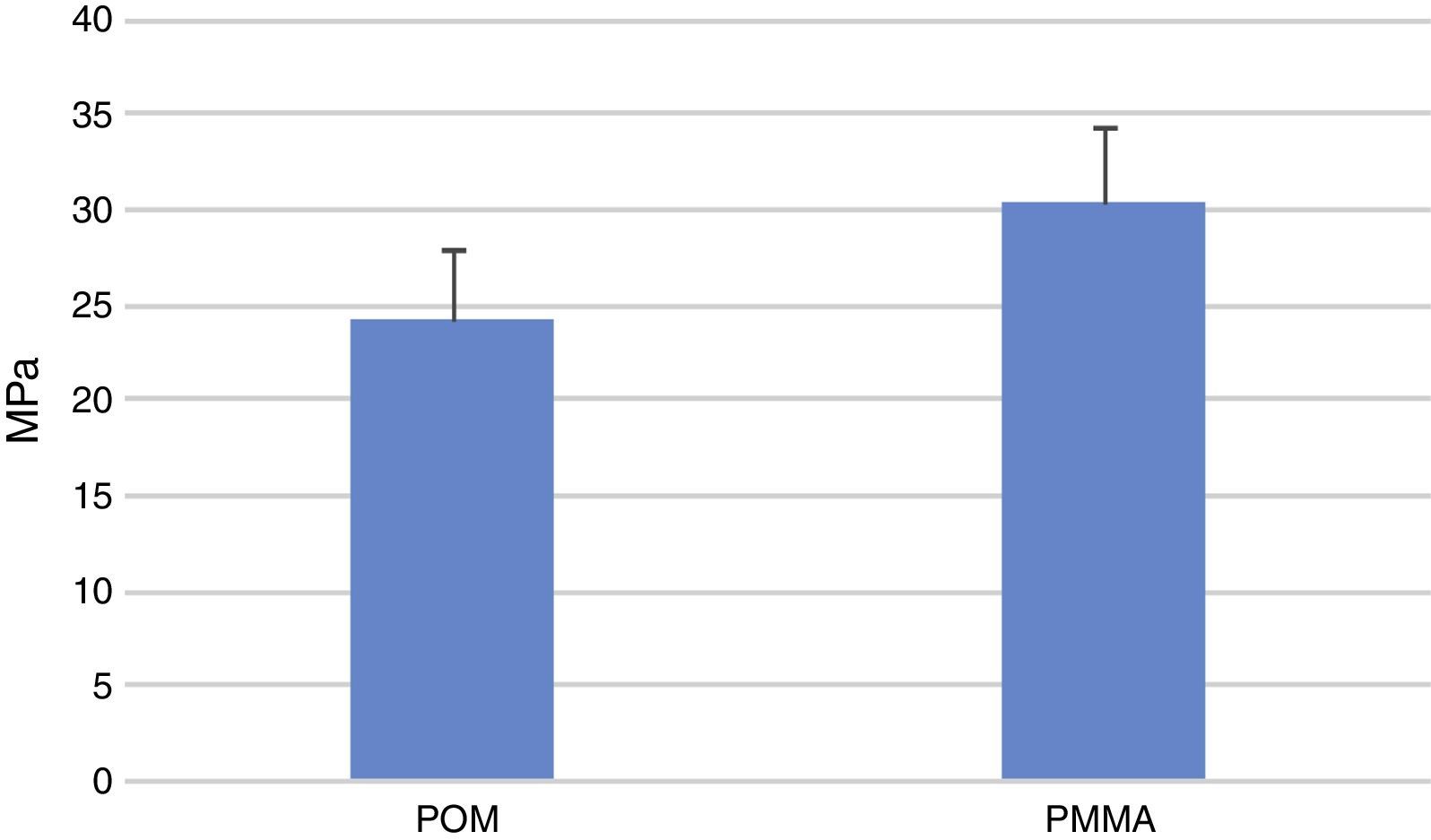
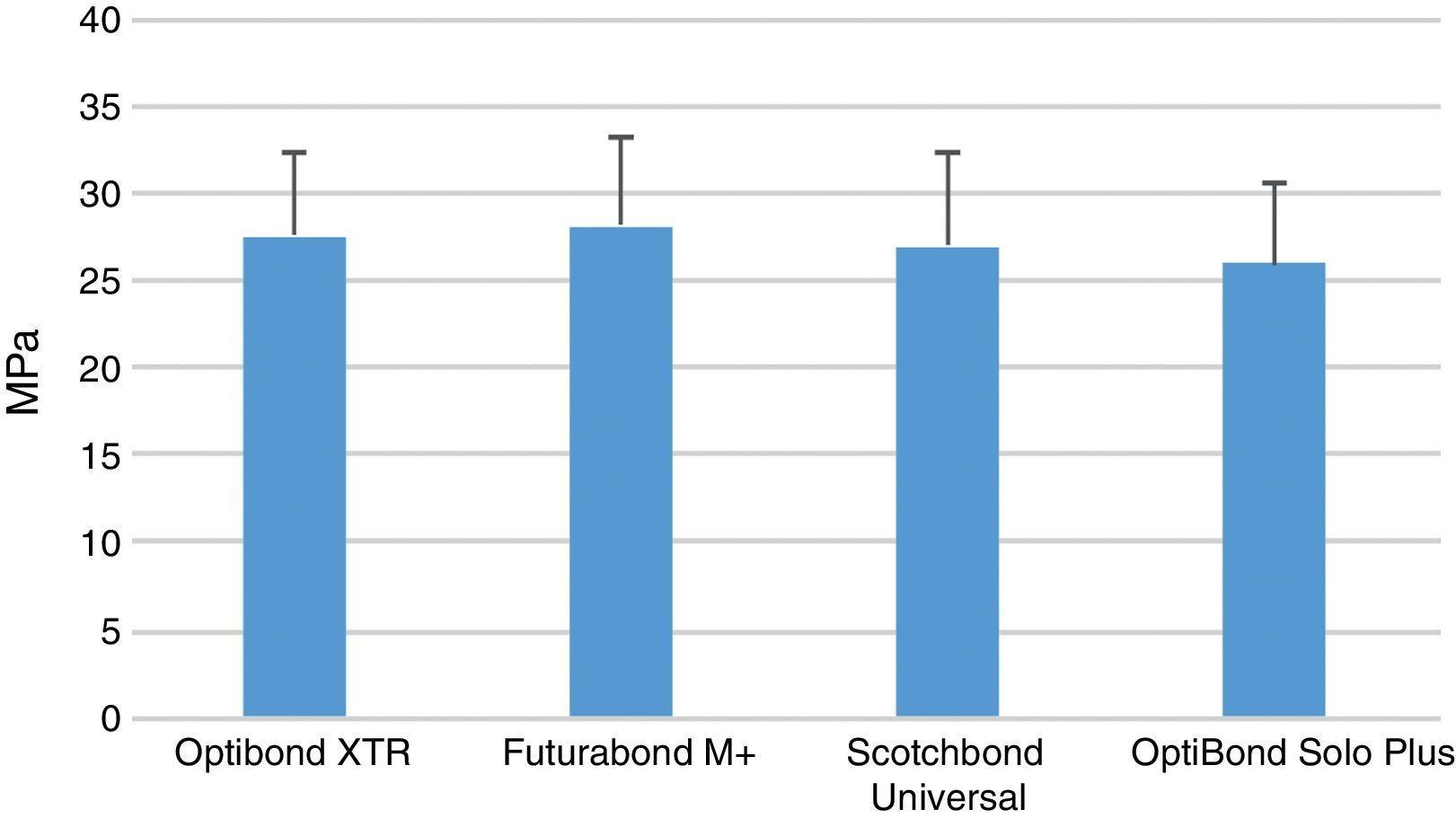
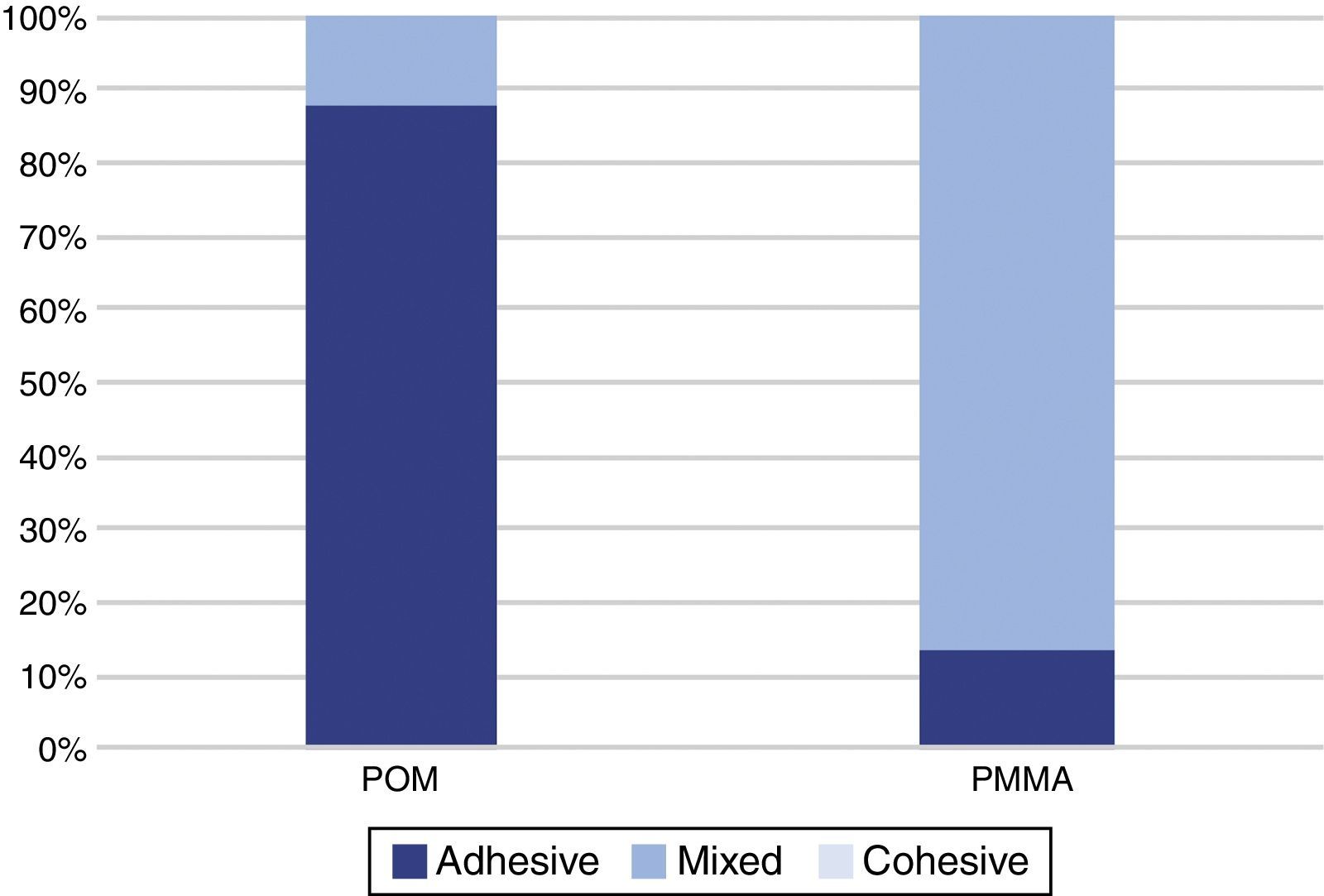
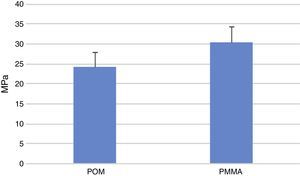
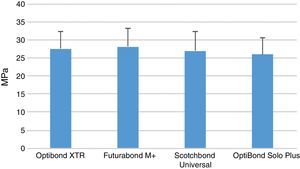
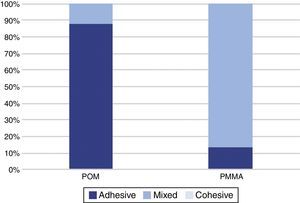
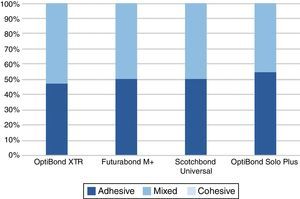
ResultsThe mean SBS yielded with PMMA specimens was significantly (p<0.001) higher than with POM. There were no statistical (p=0.062) differences between adhesive systems. Statistically significant (p<0.001) differences were found between failure mode observed in the two polymeric materials. No cohesive failure was obtained, with the POM specimens having mostly adhesive failures, in contrast with the PMMA with mostly mixed failures. No significant (p=0.925) differences in failure mode were identified between adhesives.
ConclusionIt is possible to achieve an adequate adhesion bond to POM and PMMA. SBS values were higher in PMMA specimens than to POM but no differences were found between adhesive systems.
Avaliar a capacidade de reparação de materiais poliméricos CAD/CAM utilizando sistemas adesivos universais.
MétodosOitenta blocos de polimetilmetacrilato (PMMA) e 80 blocos de polioximetileno (POM) foram fresados pelo fabricante (diâmetro: 7mm – altura: 4mm). O topo dos espécimes foi jateado com Al2O3 (50μm). Os 80 espécimes de cada material foram aleatoriamente distribuídos por 4 grupos experimentais (n=20) segundo o sistema adesivo utilizado: OptiBond XTR, Futurabond M+, Scotchbond Universal ou OptiBond SoloPlus. Os sistemas adesivos e o compósito (GrandioSO) foram aplicados segundo as instruções dos fabricantes. Os espécimes foram armazenados em água destilada, 37°C durante 48 horas, e submetidos a testes de resistência adesiva a tensões de corte. A falha de união foi classificada em: adesiva, coesiva ou mista. Os dados de resistência adesiva foram analisados com ANOVA e os dados do tipo de falha com testes segundo Kruskal-Wallis e Mann-Whitney (alfa=0,05).
ResultadosO tipo de material polimérico utilizado como substrato influenciou os valores de adesão (p<0,001) e o tipo de falha (p<0,001). Com o PMMA foram obtidos valores de resistência adesiva mais elevados e o tipo de falha foi maioritariamente do tipo misto. Nos espécimes fabricados com POM observaram-se maioritariamente falhas do tipo adesivo. Nem valores de adesão (p=0,062) nem no tipo de falha (p=0,925) foram influenciados pelo sistema adesivo utilizado.
ConclusõesÉ possível obter adesão eficaz a qualquer um dos materiais poliméricos de CAD/CAM testados. Os valores de adesão foram mais elevados para o PMMA do que para o POM, independentemente do sistema adesivo utilizado.
Fixed temporary or provisional dental restorations are used for a limited period of time, after which, they are replaced by the definitive ones.1 They are meant to enhance aesthetic, and/or function, protect pulpar and periodontal health, promote guided tissue healing, prevent migration of the adjacent teeth and provide an adequate occlusal scheme.2–4 They are also diagnostic tools, as they permit the evaluation of hygiene procedures and maxillo-mandibular relationships, playing an important role for understanding the treatment outcomes and limitations.5–9
Several types of self or light curing acrylic resins, such as polyethyl methacrylate resin, polyvinyl methacrylate resin, polymethyl methacrylate (PMMA) resin, bis-acryl composite resin, and visible light-cured urethane dimethacrylates, are the most common materials used for the fabrication of interim restorations.10–12
Despite provisional restorations mainly serving for a short period of time, some situations such as comprehensive occlusal reconstructions or oral implantation treatments require a long-term temporary restoration.13–15 Therefore, the material used to fabricate these type of restorations should present improved mechanical properties, adequate colour stability and provide marginal integrity to face extended functional loading.16,17
For this purpose, the use of resin materials for computer aided design/computer aided manufacturing (CAD/CAM) have increased lately.18,19 Nowadays, temporary and even permanent dental restorations can be milled of polymeric materials, such as polymethyl methacrylate (PMMA)-based or polyoxymethylene (POM) CAD/CAM blocks.20
Several studies have shown that the milling technique provide high precision restorations, with a more precise marginal quality than conventionally processed resin, improved colour stability and better physical and mechanical properties compared to the conventionally fabricated ones.3,17,21
Restorations milled of PMMA-based CAD/CAM blocks present better mechanical properties, a wider range of translucency and a higher stability against discolouration compared to the conventionally polymerized ones.22
Polyoxymethylene (POM), also called “acetal resin”, is an alternative to PMMA-based resin. It is a thermoplastic polymer with a monomer-free crystalline structure consisting of a chain of alternating methyl groups linked by an oxygen molecule, and it is produced by the polymerization of formaldehyde.23–26
This material has been brought into medicine in total hip replacement surgeries and temporomandibular joint reconstructions, with its use in dentistry increasing lately due to its mechanical and physical properties such as high wear, fracture and creep resistance and high fatigue endurance and its superior aesthetic features.25,26 Being monomer-free allows it to be used as an innovative and a safe treatment alternative for patients who are allergic to conventional resins, presenting high biocompatibility.27 In addition, is a hydrophobic material, which means that does not absorb water or saliva and has little or no porosity, which reduces the accumulation of biological material like plaque, avoiding odour and stains.26
At the moment is used as a material for pre-formed clasps for partial dentures, as direct retainers attached to a cobalt–chromium removable partial denture framework, removable partial prostheses, partial denture frameworks, provisional bridges and restorations, post-surgery space maintainers, occlusal splints, and even implant abutments.25,26
As they can be used for a long period of time, repairing or relining temporary restorations is common in clinical practice, since fractures may occur intraorally between appointments.11,22,28 Furthermore, those materials should undergo reshaping, addition, removing and repolishing procedures to allow new treatment approaches.11,14,15
Light-cured resin materials have been suggested to repair and reshape provisional restorations, because of their adequate working time, easy procedure and aesthetic advantages.11 However, the strength of this bonding remains questionable and scarce information on the reparability of CAD/CAM polymer-based materials and the preferred repair method is available so far.22
Previous studies showed that mechanical pre-treatment such as surface roughening through air abrasion with aluminium oxide before the bonding procedure increases the bond strength repair of several materials.22,29 Actually, the limiting factor is the low chemical bond strength to the polymeric material since the standardized polymerization under high pressure and high temperature results in a higher degree of conversion and less residual monomer in the material.15 It is necessary to assess if the use of Universal adhesive might be a solution to overcome the difficulty in achieving adequate chemical bonding, since it is known their ability to bond various materials is well known.29,30
Therefore, the aim of the present study was to evaluate the reparability of two different CAD/CAM polymer materials (PMMA and POM) by assessing the shear bond strength (SBS) of a light-cured composite, using four different adhesive systems, according to the following null hypothesis: (1) there are no differences between the bond strength to the CAD/CAM polymer materials; (2) the SBS is not influenced by the adhesive system used.
Materials and methodsBased on a pilot study, the sample size (n=20) was estimated with a power analysis in order to provide statistical significance (α=0.05) at 80% power.
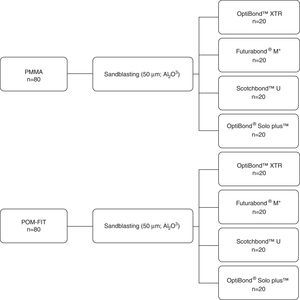
One hundred and sixty blocks of CAD-CAM polymeric materials, with standardized dimensions of 7mm diameter and 4mm height, were milled by the manufacturer. Eighty blocks were made of PMMA (PMMA – GT Medical S.L, Spain) and 80 were made of POM (POM-fit – GT Medical S.L, Spain).
The top surface of all specimens was mechanically conditioned with 50μm Al2O3 (Microetcher II; Danville Engineering) airborne particle abrasion, performed perpendicularly to the block surface with 2.5bar pressure for 15s at 10mm distance. After the sandblasting, the specimens were ultrasonically cleaned in an ethanol ultrasonic bath (Elmasonic One; Elma) for 5min and then cleaned with water-spray and air-dried carefully with oil-free compressed air.
The 80 specimens of each material were randomly allocated to four experimental groups, 20 specimens each, according to the different adhesive system used (Figure 1): OptiBond™ XTR (Kerr™, Scafati, SA 1-84018, Italy) Futurabond® M+ (VOCO GmbH, Cuxhaven, 27472, Germany), Scotchbond™ Universal (3M ESPE, Neuss, 41453, Germany) or OptiBond™ Solo Plus (Kerr™, Scafati, SA 1-84018, Italia) (Table 1).
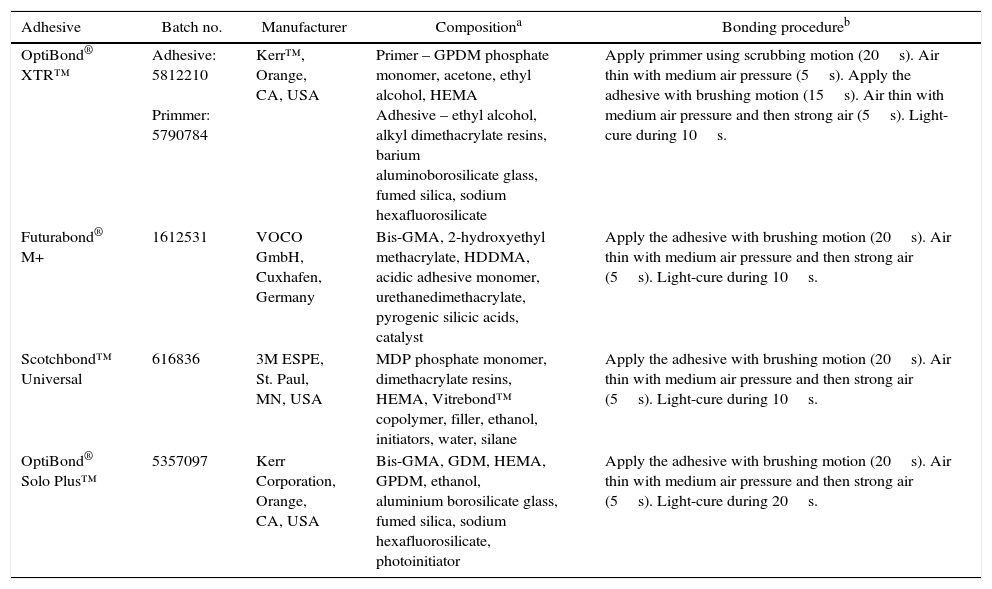
Characteristics of the adhesive systems and the bonding procedure.
| Adhesive | Batch no. | Manufacturer | Compositiona | Bonding procedureb |
|---|---|---|---|---|
| OptiBond® XTR™ | Adhesive: 5812210 Primmer: 5790784 | Kerr™, Orange, CA, USA | Primer – GPDM phosphate monomer, acetone, ethyl alcohol, HEMA Adhesive – ethyl alcohol, alkyl dimethacrylate resins, barium aluminoborosilicate glass, fumed silica, sodium hexafluorosilicate | Apply primmer using scrubbing motion (20s). Air thin with medium air pressure (5s). Apply the adhesive with brushing motion (15s). Air thin with medium air pressure and then strong air (5s). Light-cure during 10s. |
| Futurabond® M+ | 1612531 | VOCO GmbH, Cuxhafen, Germany | Bis-GMA, 2-hydroxyethyl methacrylate, HDDMA, acidic adhesive monomer, urethanedimethacrylate, pyrogenic silicic acids, catalyst | Apply the adhesive with brushing motion (20s). Air thin with medium air pressure and then strong air (5s). Light-cure during 10s. |
| Scotchbond™ Universal | 616836 | 3M ESPE, St. Paul, MN, USA | MDP phosphate monomer, dimethacrylate resins, HEMA, Vitrebond™ copolymer, filler, ethanol, initiators, water, silane | Apply the adhesive with brushing motion (20s). Air thin with medium air pressure and then strong air (5s). Light-cure during 10s. |
| OptiBond® Solo Plus™ | 5357097 | Kerr Corporation, Orange, CA, USA | Bis-GMA, GDM, HEMA, GPDM, ethanol, aluminium borosilicate glass, fumed silica, sodium hexafluorosilicate, photoinitiator | Apply the adhesive with brushing motion (20s). Air thin with medium air pressure and then strong air (5s). Light-cure during 20s. |
The specimens were fixed on Watanabe plates using plaster and to customize and define the bonding area, a perforated adhesive tape (Adhesive vinyl, SRA3; Xerox) with round-shaped orifices (3mm in diameter) was positioned on the surface of the blocks. Each adhesive was applied according to the manufacturer's recommendations.
The repairing composite resin Grandio®SO (VOCO GmbH, Cuxhaven, 27472, Germany), was applied according the manufacturer's specific instructions, in a 2mm layer, using the Watanabe plate as a mould, and polymerized during 10s.
The adhesive and composite were light cured using Ortholux LED Curing Light (3M Unitek, 82171 Puchheim, Germany, Lot nr: 939830000776). The tip of the light curing unit was kept perpendicular to and in contact with the surface in order to receive a maximum curing energy. The intensity of the curing light, 1000mW/cm2, was monitored with a Cure Rite Visible Curing Light Meter (Dentsply, York, PA, USA).
Specimens were stored in distilled water at 37°C for 48h before testing. SBS was measured with a single-plane lap device in a universal testing machine Instron model 4502 (Instron Ltd., Bucks, HP 12 3SY, England) with a 1kN load cell at a cross-head speed of 0.5mm/min.
The mode of failure was analysed with a stereomicroscope (EMZ-8TR, Meiji Techno Co) at 20× magnification. The failure mode was classified as adhesive type, if the failure occurred at the adhesive interface, cohesive when the failure occurred within the composite or CAD/CAM resin, or as mixed if a combination of failures occurred.
Data were statistically analysed with software (IBM SPSS Statistics 20; SPSS Inc.). After assessing normality and homoscedasticity with Shapiro–Wilk and Levene's tests (p>0.05), SBS data were submitted to 2-way ANOVA model (α=0.05). Non-parametric Kruskal–Wallis and Mann–Whitney tests were used to analyse the failure mode data (α=0.05).
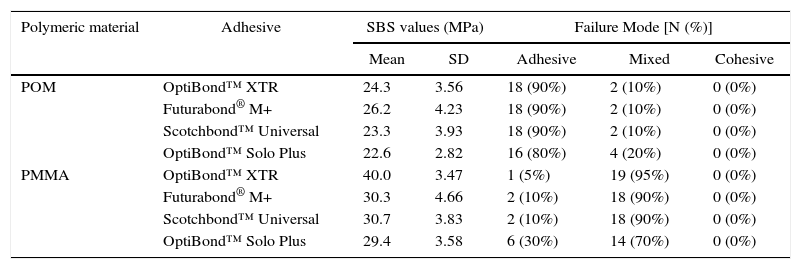
ResultsThe descriptive statistic of the sample is presented in Table 2, with the SBS values (mean and standard deviation) and failure mode distribution (number and percentage) according to each experimental group.
Descriptive statistics of the SBS values and Failure Mode distribution according to the 8 experimental groups.
| Polymeric material | Adhesive | SBS values (MPa) | Failure Mode [N (%)] | |||
|---|---|---|---|---|---|---|
| Mean | SD | Adhesive | Mixed | Cohesive | ||
| POM | OptiBond™ XTR | 24.3 | 3.56 | 18 (90%) | 2 (10%) | 0 (0%) |
| Futurabond® M+ | 26.2 | 4.23 | 18 (90%) | 2 (10%) | 0 (0%) | |
| Scotchbond™ Universal | 23.3 | 3.93 | 18 (90%) | 2 (10%) | 0 (0%) | |
| OptiBond™ Solo Plus | 22.6 | 2.82 | 16 (80%) | 4 (20%) | 0 (0%) | |
| PMMA | OptiBond™ XTR | 40.0 | 3.47 | 1 (5%) | 19 (95%) | 0 (0%) |
| Futurabond® M+ | 30.3 | 4.66 | 2 (10%) | 18 (90%) | 0 (0%) | |
| Scotchbond™ Universal | 30.7 | 3.83 | 2 (10%) | 18 (90%) | 0 (0%) | |
| OptiBond™ Solo Plus | 29.4 | 3.58 | 6 (30%) | 14 (70%) | 0 (0%) | |
The mean SBS ranged between 22.6MPa for the POM specimens repaired with OptiBond Solo Plus and 40.0MPa for the PMMA with OptiBond XTR.
The mean SBS yielded with PMMA specimens was significantly (p<0.001) higher than with POM (Figure 2). Two-way ANOVA showed no statistical (p=0.062) differences between adhesive systems (Figure 3) and an interaction (p=0.212) between the two factors was not detected.
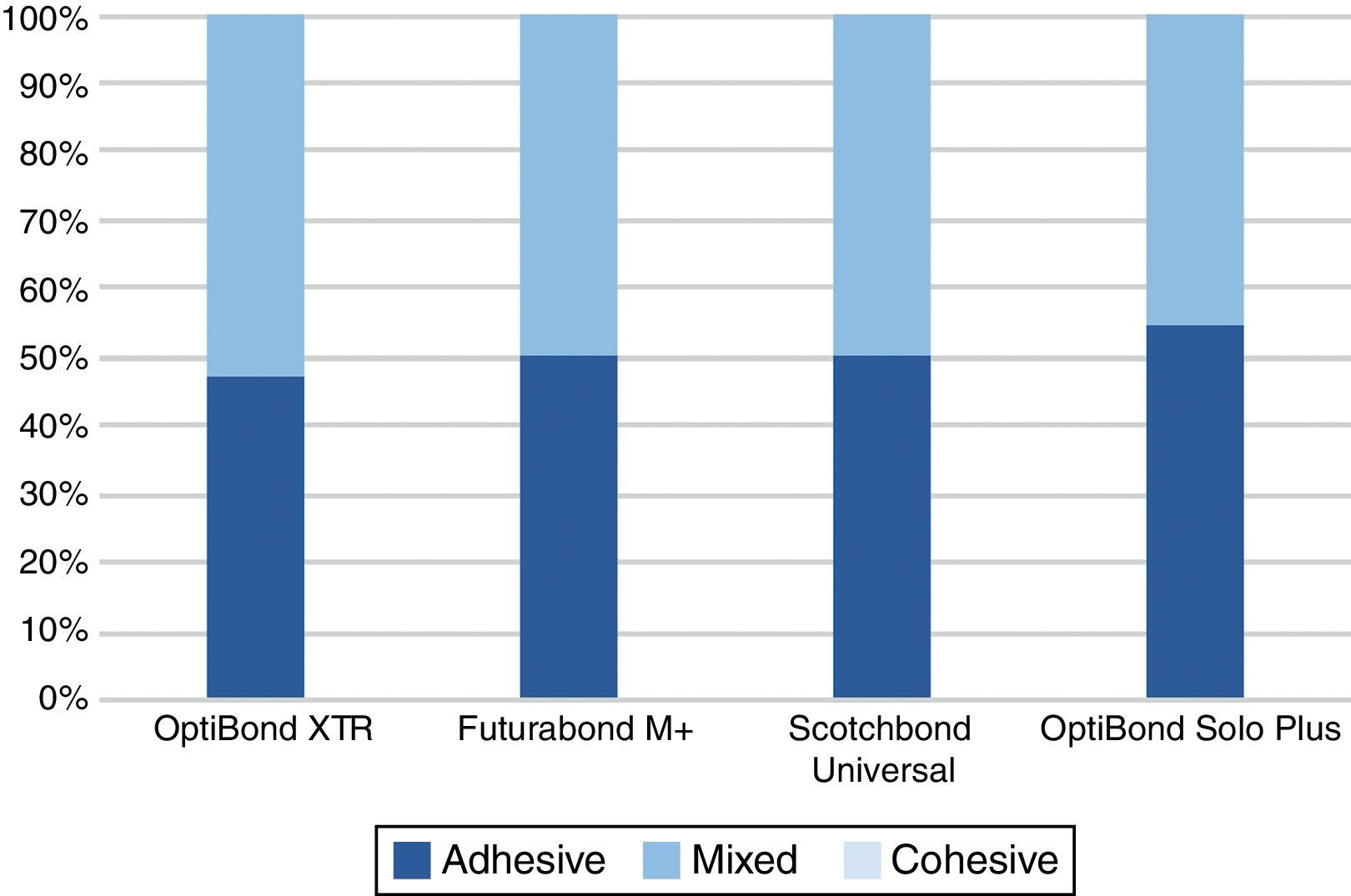
When the failure mode was analysed, no cohesive failure was obtained, regardless of the experimental group considered. A statistically significant difference was detected between the failure mode observed with the two CAD/CAM resins (p<0.001), with the POM specimens having mostly adhesive failures (87.5%), in contrast with the PMMA with mostly mixed failures (86.3%) (Figure 4). No statistically significant (p=0.925) difference was identified between adhesives (Figure 5).
The SBS test has been widely used,31 although some authors suggest there are problems related to the validity of the obtained measurements, sustaining that the stresses are mostly concentrated in the substrate and not in the adhesive interface, thus causing its premature failure prior to the interface itself, resulting in a higher percentage of cohesive failures.32,33 However, even with the high SBS values obtained in the present study, when the failure mode was analysed, no cohesive failure was obtained, regardless the experimental group considered, which might confirm the validity of the measurements. Moreover, this method has been used in most of the recent studies testing the adhesion to CAD/CAM materials, enabling the comparison of the present results.15,22,34
With adhesive dentistry, it has become possible to bond different materials to each other enabling dentists to repair rather than replace restorations in case of chippings, fractures or marginal defects.28,31 Another approach made possible by adhesion is the reshaping of the restorations by adding another material, in case of aesthetic improvements required by the patient.11,14,28
For the CAD/CAM materials considered in this study, no information on the preferred repair method or material is available so far, especially regarding the acetal resin.11,22,35 The chemical composition of the base and the added material, surface characteristics of the interface, and time elapsed since the initial setting of the restoration should be considered before choosing the repair procedure.11
Self-cured acrylic resins made from PMMA, bis-acryl provisional resins and resin composites, are the most common materials used for repair, because they have the ability to easily reconstruct shape defects, allowing for simple and quick manipulation.28 Among those, the use of self-cured acrylic resins is most popular, although direct clinical repair procedures with PMMA can be technically challenging due to the unpleasant odour, significant shrinkage, short working times and a pronounced exothermic setting reaction.11 Moreover, residual methacrylate monomer used as repair or relining materials demonstrates cytotoxicity and potential allergenicity.11,28 More recently, light-cured resin composites have been suggested for the intraoral repair of provisional restorations with the following advantages: availability in numerous shades and viscosities, ease of application and manipulation, adequate working time, minimal odour, low polymerization shrinkage, and increased marginal accuracy.11,28,36
Since several studies showed that previous mechanical conditioning of the substrate is important to achieve high bond strength,11,22,34,35,37 the specimens were all sandblasted with aluminium particles (50μm) before the bonding procedure in the present investigation.
Nevertheless, the ability of achieving an adequate chemical bonding to the substrate remains questionable, since the polymerization under standardized conditions, high pressure and high temperature, of the CAD/CAM materials, results in a higher degree of conversion and less residual monomer in the material.15 Thus, the amount of residual monomer or free radicals is very low or even insufficient to allow co-polymerization and these materials present a low surface energy (and wettability) and resistance to surface modification by different chemical treatments.38 Furthermore, monomers usually present in the adhesive system (Bis-GMA, HEMA; GDMA) and in the composite (Bis-GMA, UDMA, TEGDMA, bis-EMA) might not co-polymerize with PMMA-based materials.22,37
Several possible mechanisms were proposed to explain the role played by the adhesive during the composite resin filling repair. Firstly, the micromechanical interlocking formed by infiltration of the monomer into micro retentions created by the mechanical conditioning should be considered, since the adhesive monomers enable the achievement of better wetting of the surface, due to the solvent and a surfactant that are often added to the bonding agent and the wetting properties of the adhesive monomers themselves, since they have low viscosity.39,40 The POM specimens presented mostly adhesive failures, in contrast with the PMMA with mostly mixed failures, indicating that the bond strength achieved is higher to the PMMA. Thus the first null hypothesis that there were no differences between the two substrates was rejected. Since the micromechanical interlocking plays an important role in the repair bond strength, the differences obtained might be explained by differences in the surface properties of the two substrates: it is known than the POM presents a higher resistance to surface modification.26
In addition to the mechanical interlocking, it was suggested the possibility of a chemical bond formation to the surface fillers and to the matrix.15 Although, as mentioned before, a co-polymerization with the traditional adhesive monomers is not sufficient because the CAD/CAM resins are industrially polymerized and present a higher degree of conversion and low amount of unsaturated C–C bonds, it is known that the new some Universal adhesive systems contain silane or phosphoric acid monomers with high affinity to inorganic filler particles, that may form covalent bond to the unreacted methacrylate groups on the matrix or to the inorganic compound of the CAD/CAM materials.40–42
However, in the present study, for the different adhesives, although there are differences in their composition (OptiBond® Solo Plus™ does not contain phosphoric monomers) no statistically significant difference was reached, indicating that the bonding agent does not influence the failure mode, which means that the second null hypothesis cannot be rejected. Further studies are necessary, with no mechanical conditioning (highly polished specimens), to assess if the chemical bonding alone is sufficient to achieve adequate SBS values.
Also, all surfaces were air-abraded to create a standardized surface with some micromechanical retentions. Different conditioning procedures, like abrasion with alumina-coated silica particles followed by silanization, should also be investigated, since there are several pre-treatment procedures available and described by the literature as efficient to condition CAD/CAM polymeric material.22,38,40,43
From a methodological point of view, a shortcoming of this study is the lack of artificial ageing by thermal cycling or long-term water storage. In previous studies, adhesion between PMMA-based polymer restorations and conventional resin cements, as well as shear bond strength of repaired dimethacrylate-based direct composites, has shown to be impaired by ageing.15,22,44 Several mechanisms were proposed to explain that. Some state that thermal cycling ageing leads to mechanical stress on the bonding area of the repaired substrate and the residual monomer content and consequently the number of carbon-carbon double bonds, but it is also discussed that thermal cycling might increase the repair bond strength by intensifying the process of post-polymerization between polymeric CAD/CAM materials and adhesive resins.15
To the knowledge of the authors, this is the first evaluation of the bonding performance to POM. Therefore, the present results cannot be compared to other available studies. As so, the main goal of the present study was to assess the overall viability of establishing bonding to POM.
Likewise, very few in vitro studies address the reparability of restorations milled of PMMA-based CAD/CAM blocks and consequently, many of the comparisons and conclusions drawn about this matter are based on essays studying the bonding strength to these kind of polymers regarding different conditioning and adhesive procedures for veneering or cementing purposes.
Techniques and materials used in this study should be tested in more demanding laboratory conditions to closer simulate clinical environment.
Although it is difficult to set a clinically relevant SBS value for bond strength after repair, the value of 20MPa has been suggested as a reference.22 In the present study, the mean SBS values obtained were higher than those suggested above, demonstrating that the repairing method tested is efficient, with the PMMA blocks achieving statistically significant higher values than the acetal resin, regardless of the adhesive system used.
ConclusionsIt is possible to achieve an adequate adhesion bond to POM and PMMA. However, SBS values were higher in PMMA specimens than to POM. No differences were found between adhesive systems.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to thank GT Medical S. L., 3M ESPE, KERR and VOCO for providing the materials for this study.