The aim of this study was to perform a systematic review and meta-analysis on the sagittal joint spaces measurements of the temporomandibular joint. An electronic database search was performed with the terms “condylar position”; “joint space” AND “TMJ”. The risk of bias of each study was assessed with “Cochrane risk of bias tool”. The values used in the meta-analysis were the joint space measurements and their differences between the right and left joint.
From the initial search 2706 articles were retrieved. Eighteen articles classified for final review. Only one study was classified as having high level of evidence. Seventeen of the reviewed studies were included in the meta-analysis concluding that the mean sagittal joint space values were: anterior joint space 1.86mm, superior 2.36mm and posterior 2.22mm. However, the analysis also showed high levels of heterogeneity. Right and left comparison has shown statistically significant differences.
O objetivo deste estudo foi realizar uma revisão sistemática e meta-análise sobre os espaços articulares sagitais da articulação temporomandibular. Foi realizada uma pesquisa eletrónica com os termos “condylar position”, “joint space”AND”TMJ”. O nível de evidência de cada estudo foi avaliado com “Cochrane risk of bias tool”. Os valores sumariados na meta-análise foram os espaços articulares e a diferença entre a articulação direita e esquerda.
Da pesquisa inicial resultaram 2076 artigos dos quais 18 foram selecionados para a revisão. Apenas um estudo foi considerado de elevado nível de evidência. Foram incluídos na meta-análise 17 dos artigos da revisão concluindo-se que, os valores médios para os espaços articulares sagitais foram: 1.86mm para o anterior, 2.36mm para o superior e 2.22mm para o posterior. No entanto, a análise revelou ainda grande heterogeneidade nos resultados dos estudos avaliados. Verificaram-se diferenças estatisticamente significativas entre as articulações esquerda e direita.
The mandibular condyle position has been at the centre of a long lasting controversy among gnathologists and orthodontists. The ideal concept of the mandibular condyle position has changed from the most retruded position of the condyle in the glenoid fossa to the most superior position of the condyle. Nowadays it is accepted as the most anterosuperior position of the mandibular condyle in the glenoid fossa with the articular disk placed in between.1–4 The literature also shows a great confusion concerning the relationship between dental occlusion and the temporomandibular joints. It is possible to find articles proving the relationship between these two variables, while others achieved contrary results with no relationship being suggested.5–8 The major focus of the discussion usually is the ideal mandibular condyle position and the effects of its variation.4,9,10 With the evolution of radiographic exams like computerized tomographies (CT), including the new 3D cone-beam computed tomography (CBCT) and magnetic resonance imaging (MRI) it is now possible to radiographically examine the position of the condyle.11–13 The most common method found in the literature to determine this position is the assessment of the joint space measurements, which are the radiographic space found between the condyle and the glenoid fossa where the articular disk is placed.14 A variation on the values of these measurements suggest a displacement of the condyle and so, the determination of the “gold standard” for these values would be a very important tool to determine any variation to the condyle position. The aim of this study is to perform a systematic review and meta-analysis on the sagittal joint space measurements of the temporomandibular joint to assess the mean values for these measurements.
MethodsSearch strategyA comprehensive electronic database search to identify relevant publications was conducted, and the reference lists in relevant articles were searched manually for additional literature. No language restrictions were set, although no attempt was made to explore the informally published literature, like conference proceedings and abstracts of researches presented at conferences and dissertations. The research extended to the following databases: Medline (Pubmed), Lilacs, Scopus, Ebsco (Host by University of Porto) and Cochrane Central Register of Controlled Clinical Trials.
The search terms were “condylar position” and “joint space” AND “TMJ” with no year of publication restriction in order to include the highest number of articles (to 22 April 2014). No restriction to study design was applied.
Faculty of Dental Medicine of University of Porto and Portuguese Society of Dentofacial Orthopedics’ libraries were also consulted for printed articles not available online.
Critical evaluationAt the first stage, two reviewers screened independently the titles of the retrieved records, and only the titles related to TMJ joint space assessment were included. Joint space was defined as the radiographic image between the mandibular condyle and the glenoid fossa where the disk is interposed. Next, the abstracts of the retrieved publications were read by the two reviewers and categorized according to the radiographic procedure used to assess the joint space. An article had only to be justified by one reviewer to be included in the second selection phase. Eligibility of the retrieved articles was determined by applying the following inclusion criteria: (1) tomographic examination of the TMJ (2) determination of sagittal joint space measurements at least on two different points (anterior and posterior). The main reasons for exclusion were: mandible fractures, studies not performed in living humans, surgical interventions, studies with patients with syndromes or chronic diseases (including degenerative pathology of the TMJ), samples containing patients only in the primary or mixed/early permanent dentition, clinical only evaluation of the mandibular condyle position, 2D radiograph or magnetic resonance imaging, previous orthodontic or splint therapy, case reports, discussion or debate articles. All not published studies were also excluded.
The analysis was based on primary materials. When an abstract was considered by at least one author to be relevant, it was read in full text. At the second stage, the full texts were retrieved and critically examined. Reference lists from the articles selected on the second stage were screened and articles related to joint space measurements were hand-searched.
Data gatheringThe following data were extracted from the selected articles: year of publication, study type, study method, sample description, joint space measurements on the sagittal plane, error analysis method, statistical analysis and author's conclusion. This method was pilot-tested on ten randomly selected included articles and then refined. One reviewer author then extracted the mentioned data from the included articles and the second author checked. Any disagreement was resolved with discussion between the two authors until a consensus was reached. The risk of bias was assessed according to the “Cochrane risk of bias tool”15 as suggested by the “PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration”.16
Meta-analysisThe values studied in this meta-analysis were the sagittal joint space measurements (anterior, superior and posterior joint space) and the differences between the right and left joints. As not all the included articles presented the values for all the spaces from the right and left joints, the analysis were performed including all the data presented in each selected study. For the comparative analysis between the right and left joints, mean and standard deviation values from the samples of each article were used. For global joint space assessment, mean and standard deviation of the total sample (including both the values from the right and left joints) were used.
The restricted maximum-likelihood (REML) method was used to estimate de variability between the studies. Inverse variance method was used to assess the weight of each study.
Heterogeneity was determined using the Q Cochran test and the I2 statistics by Higgins and Thompson.17
Statistical analysis was performed using “R”, version 2.15.2 from “The R Project for Statistical Computing”, available from http://www.r-project.org.
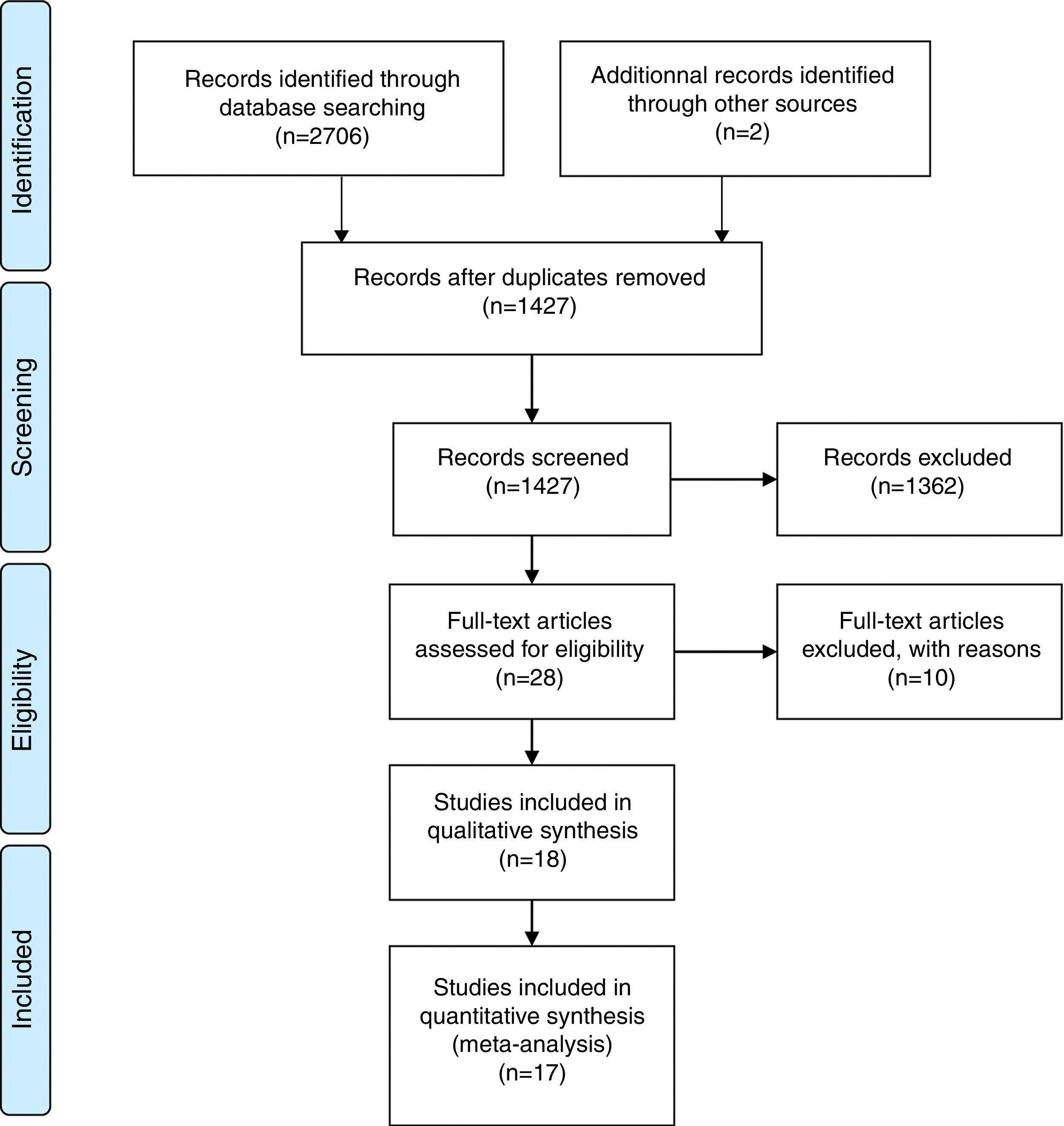
ResultsSearch resultsThe initial search strategy allowed retrieving 916 articles from Medline (Pubmed), 1114 from Scopus, 158 from EBSCOhost, 19 from Lilacs and none from the Cochrane Central Register of Controlled Clinical Trials. The number of articles reviewed in each phase of this systematic review is presented in the PRISMA flow diagram (Fig. 1). After excluding 978 duplicates, 1230 articles remained for review. In the first phase selection, the observers screened the articles by reading titles and abstracts. Articles that were not eligible because of irrelevant aims and were not directly related to this systematic review were excluded, thus 61 articles remained for further reading. 28 articles were assessed for eligibility. After screening all the articles full text according to the inclusion/exclusion criteria, 18 articles classified for final review.
Flow diagram illustrating the search strategy results.
A Randomized Clinical Trial (RCT)18 was found. Aditionally, six prospective19–24 and eleven retrospective25–35 studies were found that fullfilled the elegibility criteria defined for this review. Six of the selected articles22,25,27,32–34 used CBCT to assess the TMJ joint space while nine18–21,23,26,28,30,35 used conventional CT and three 24,29,31 used linear tomography.
Twelve of the selected studies19–21,23,24,26,28–30,32,33,35 assessed the joint space measurements by determining the closest distance between the mandibular condyle and the glenoid fossa surface.
On the other hand, four articles25,27,31,34 used a geometrical construction to assess the joint space measurements. Different authors used the Frankfurt horizontal line or the true horizontal line as a reference plane to determine the most superior point of the glenoid fossa. Following, the distance between this point and the highest point of the condyle (determined by the same method) was measured, resulting the value of the sagittal joint space. After this, starting from the most superior point of the glenoid fossa, two tangent lines were traced to the most anterior and posterior point of the condyle respectively. The distance between each of these points and the point where a perpendicular line to the tangents crosses the surface of the glenoid fossa was the anterior and posterior joint space respectively.
Two studies18,22 used a similar method to the one described above, but used the centre of the mandibular condyle as the reference point.
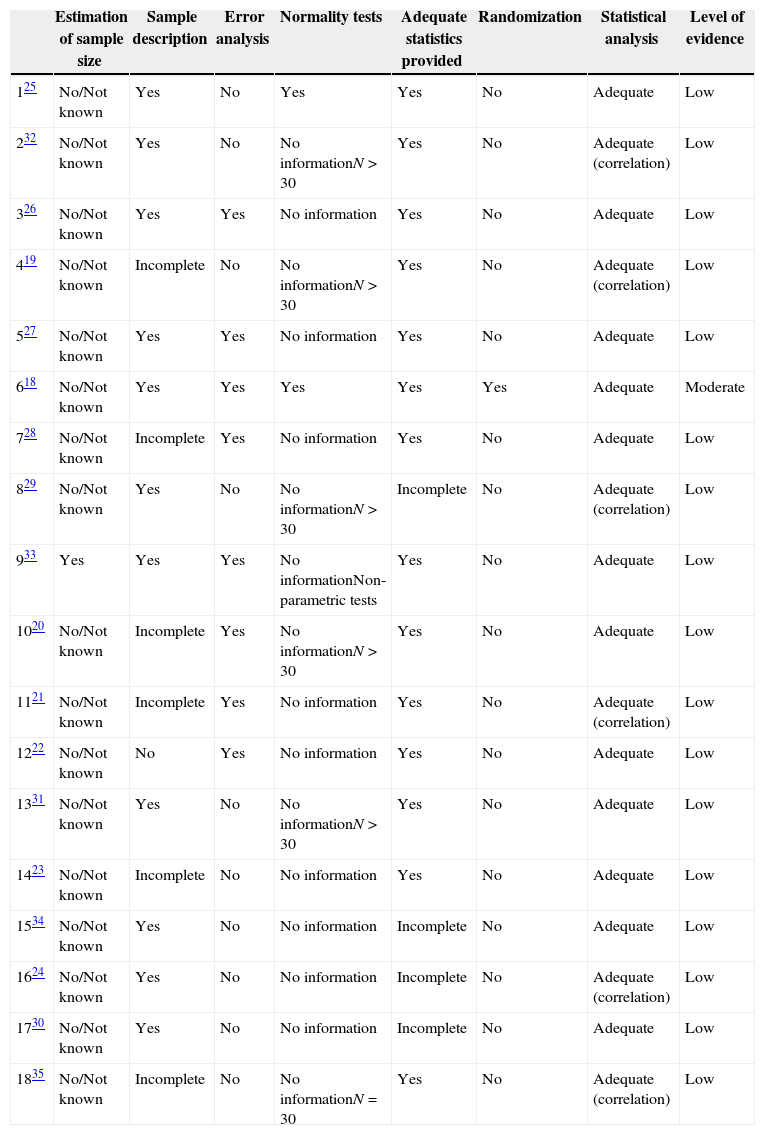
Quality assessmentThe summary of the quality analysis of the selected articles is presented in Table 1.
Summary of the quality analysis of the 18 included studies.
| Estimation of sample size | Sample description | Error analysis | Normality tests | Adequate statistics provided | Randomization | Statistical analysis | Level of evidence | |
|---|---|---|---|---|---|---|---|---|
| 125 | No/Not known | Yes | No | Yes | Yes | No | Adequate | Low |
| 232 | No/Not known | Yes | No | No informationN>30 | Yes | No | Adequate (correlation) | Low |
| 326 | No/Not known | Yes | Yes | No information | Yes | No | Adequate | Low |
| 419 | No/Not known | Incomplete | No | No informationN>30 | Yes | No | Adequate (correlation) | Low |
| 527 | No/Not known | Yes | Yes | No information | Yes | No | Adequate | Low |
| 618 | No/Not known | Yes | Yes | Yes | Yes | Yes | Adequate | Moderate |
| 728 | No/Not known | Incomplete | Yes | No information | Yes | No | Adequate | Low |
| 829 | No/Not known | Yes | No | No informationN>30 | Incomplete | No | Adequate (correlation) | Low |
| 933 | Yes | Yes | Yes | No informationNon-parametric tests | Yes | No | Adequate | Low |
| 1020 | No/Not known | Incomplete | Yes | No informationN>30 | Yes | No | Adequate | Low |
| 1121 | No/Not known | Incomplete | Yes | No information | Yes | No | Adequate (correlation) | Low |
| 1222 | No/Not known | No | Yes | No information | Yes | No | Adequate | Low |
| 1331 | No/Not known | Yes | No | No informationN>30 | Yes | No | Adequate | Low |
| 1423 | No/Not known | Incomplete | No | No information | Yes | No | Adequate | Low |
| 1534 | No/Not known | Yes | No | No information | Incomplete | No | Adequate | Low |
| 1624 | No/Not known | Yes | No | No information | Incomplete | No | Adequate (correlation) | Low |
| 1730 | No/Not known | Yes | No | No information | Incomplete | No | Adequate | Low |
| 1835 | No/Not known | Incomplete | No | No informationN=30 | Yes | No | Adequate (correlation) | Low |
In general, the statistical analysis performed was adequate to the objectives defined on each study and the statistical data are adequately presented in most cases. Apart from this, nine of the included articles21–24,26–28,30,34 used parametric tests (T Student or ANOVA) in small samples (less than 30), with no information on the normality of the data. Pearson correlation was used by six authors,19,21,24,29,32,35 with no mention to the linear relation between the variables, which is necessary to the use and interpretation of this coefficient. Seven studies19–23,28,35 did not present an adequate sample description, with no information about the age or gender. The other eleven18,24–27,29–34 showed at least, the number of patients from each gender and data concerning the age of the included sample (mean, standard deviation, minimum and maximum values). The error analysis was presented in seven of the articles.18,21,22,26–28,33 Only one study presented the estimation of sample size.33 Randomization was used by Tsuruta et al.18 and none of the retrieved articles presented blinding in measurements. Only one18 of the studies was classified as moderate level of evidence, as it presents randomization and adequate statistics but fails to presents blinding in measurements. All the other articles were classified as low level of evidence.
Meta-analysis resultsSeventeen of the studies presented on the review were included in this meta-analysis. One study34 did not present standard deviation values and so, statistical comparison with other studies was not possible.
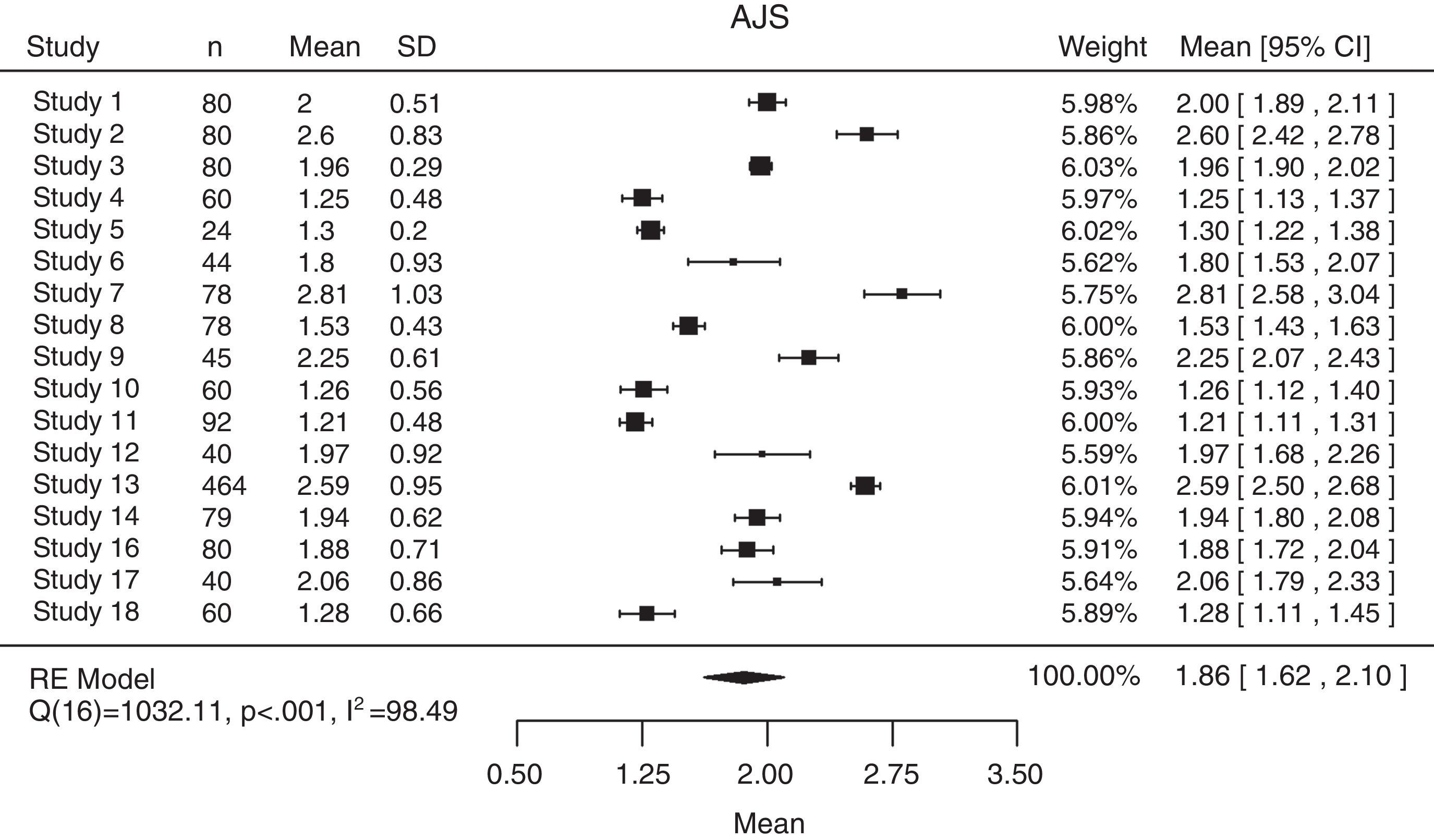
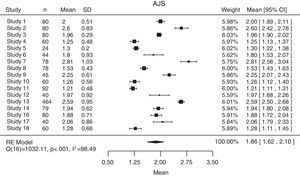
The mean anterior joint space from the 17 considered studies was 1.86mm (95% CI: 1.62–2.10), although high levels of heterogeneity were found among the studies (Q(16)=1032.11; P<0.001; I2=98.49%) (Fig. 2).
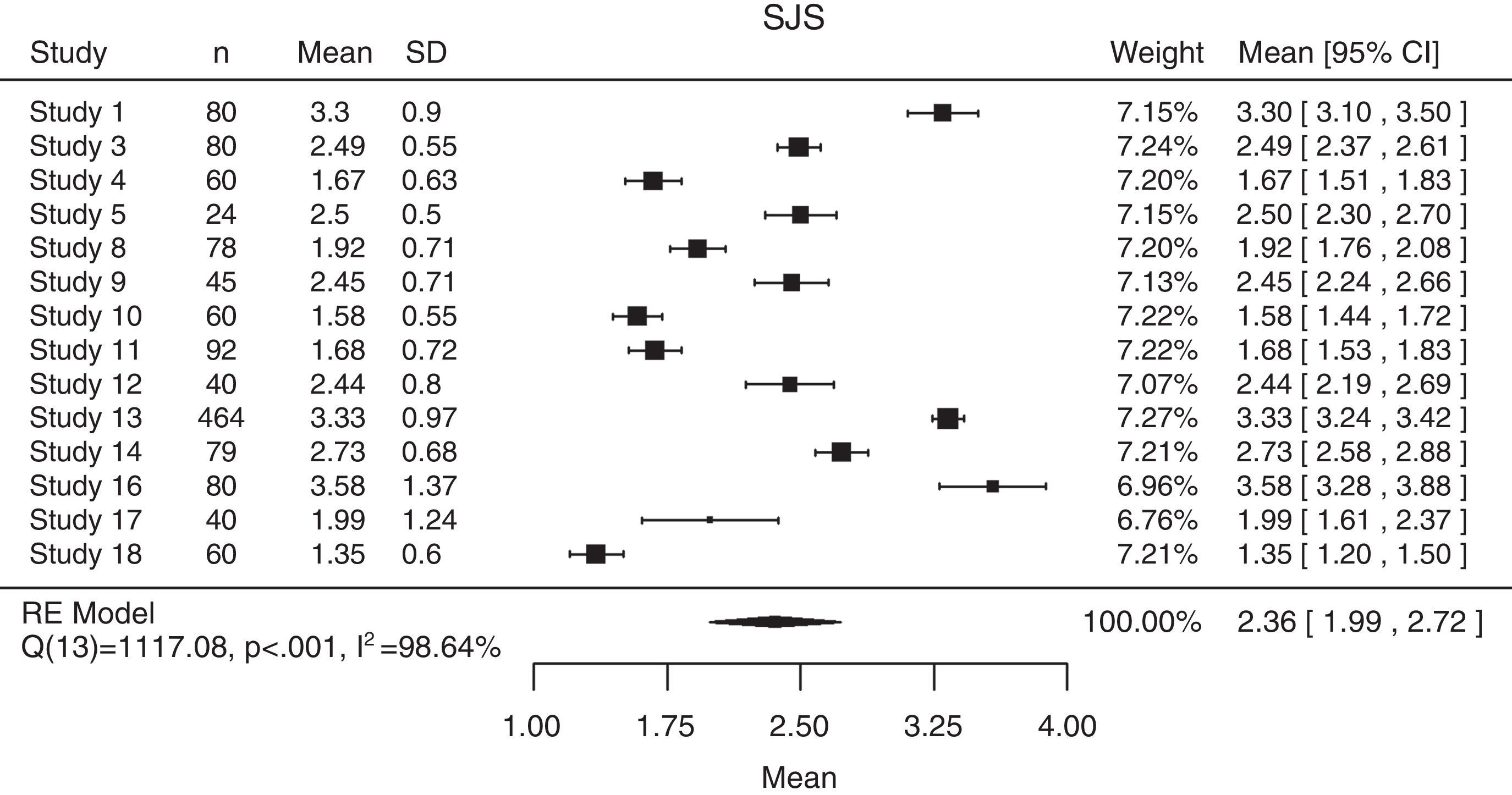
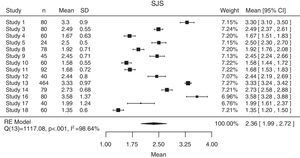
The superior joint space presented a mean value of 2.36mm (95% CI: 1.99–2.72), also with high levels of heterogeneity between the 14 articles that presented this value (Q(13)=1117.08; P<0.001; I2=98.64%) (Fig. 3).
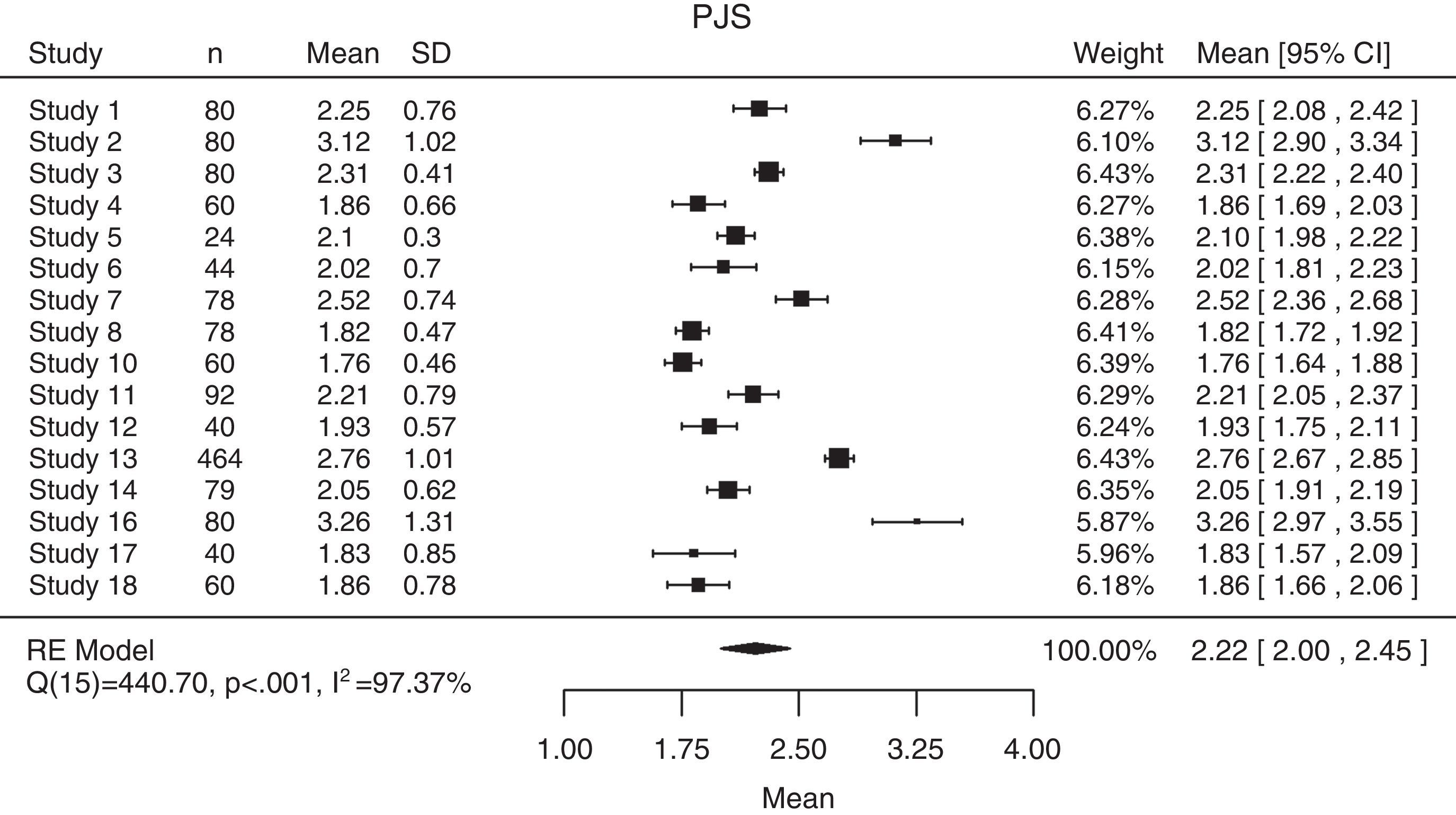
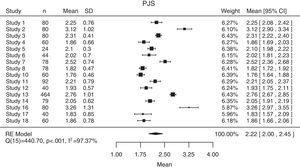
The posterior joint space also presented high heterogeneity among the 16 included samples (Q(15)=440.70; P<0.001; I2=97.37%) with a mean value of 2.22mm (95% CI: 2.00–2.45) (Fig. 4).
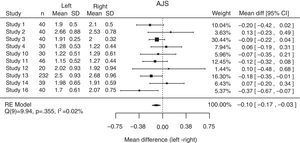
The mean global differences and the differences among the studies between the right and left anterior, superior and posterior joint spaces are show in Figs. 5–7 respectively. In all of the comparisons, the difference is close to zero.
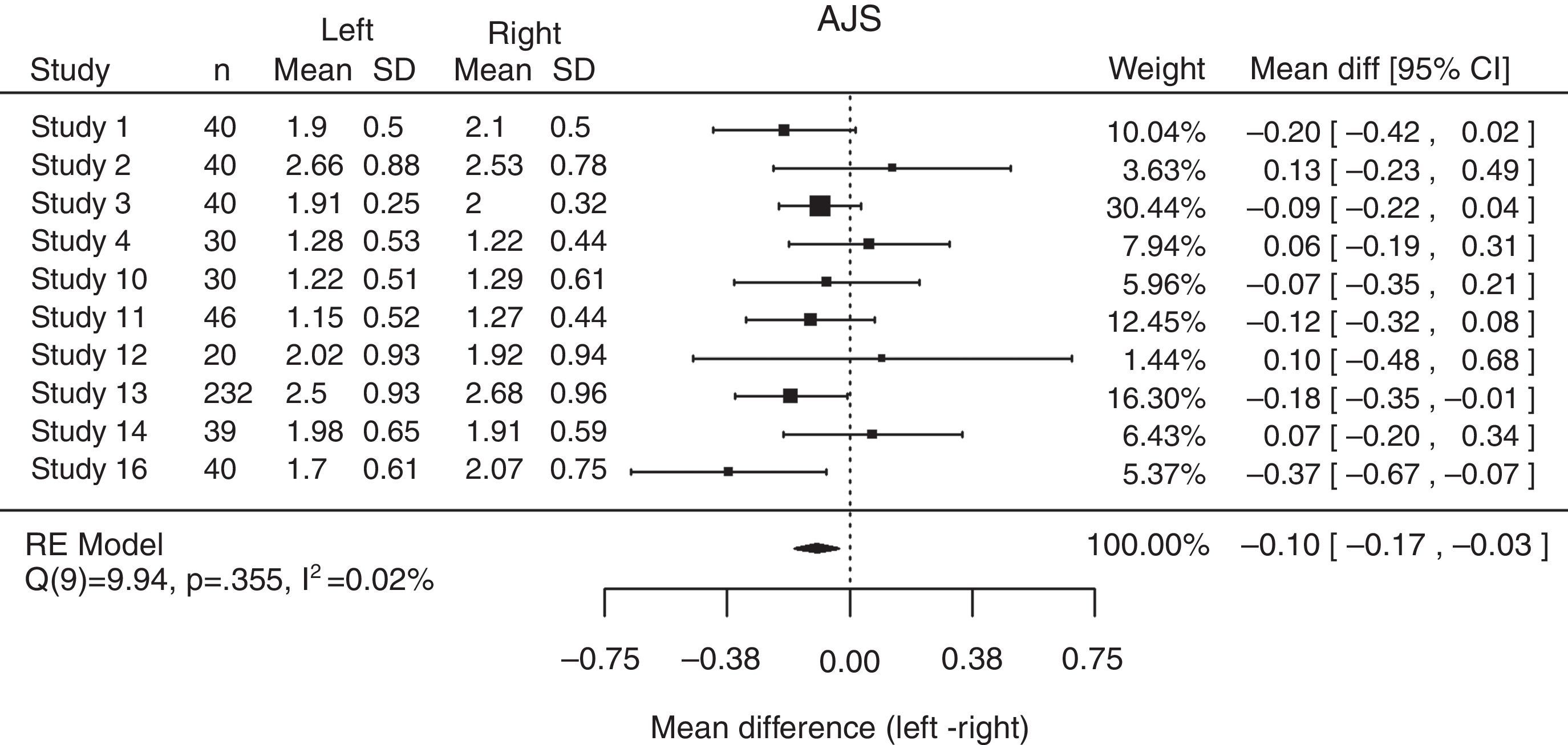
For the anterior joint space, the mean difference is −0.10mm (95% CI: −0.17; −0.03), without heterogeneity between the included samples (Q(9)=9.94; P=0.355; I2=0.02%) (Fig. 5).
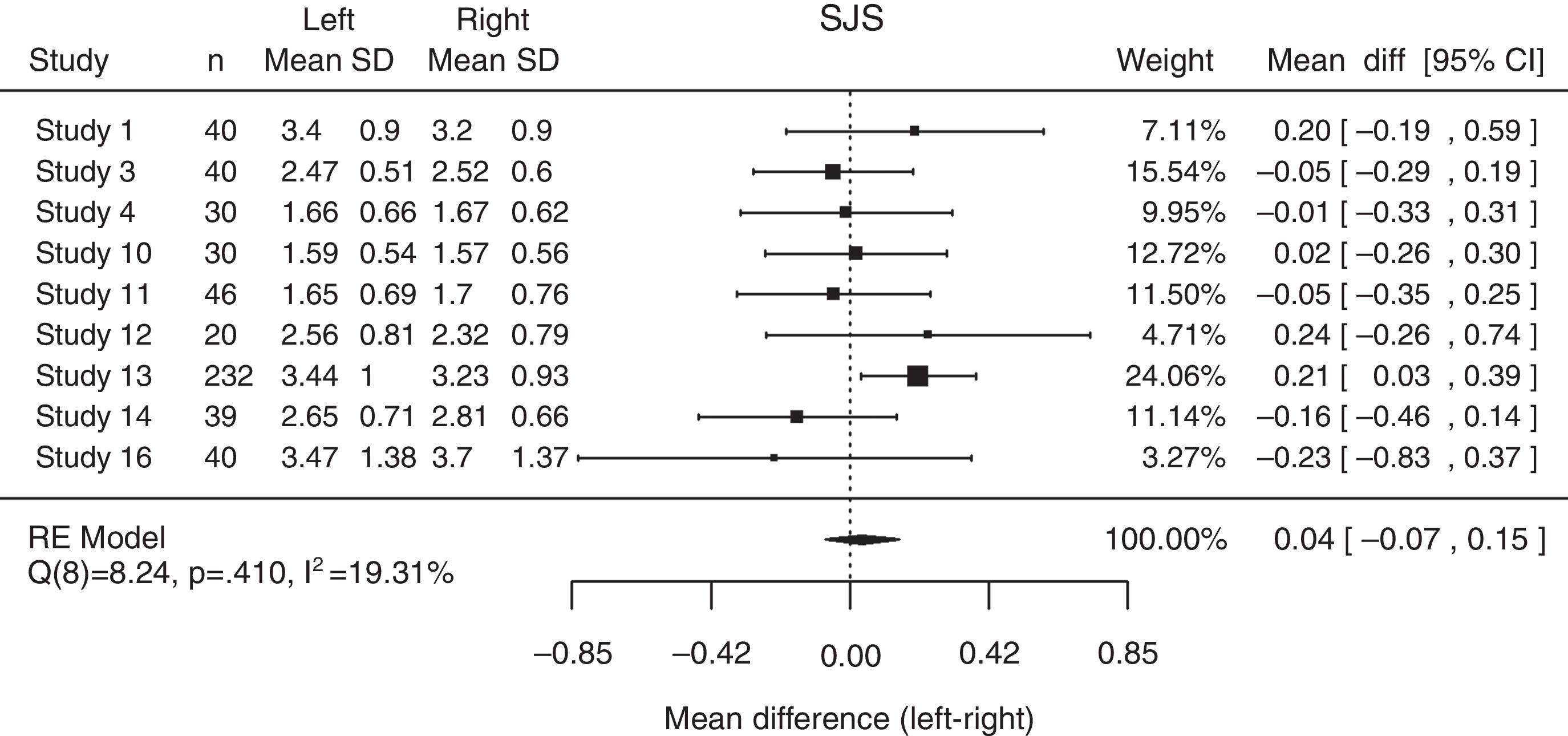
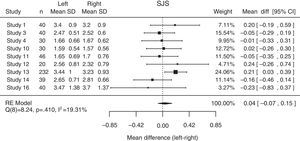
As for the mean difference between the right and left superior joint spaces, the value was 0.04mm (95% CI: −0.07; 0.15), presenting low heterogeneity among the differences found on the different studies considered (Q(8)=8.24; P=0.410; I2=19.31%) (Fig. 6).
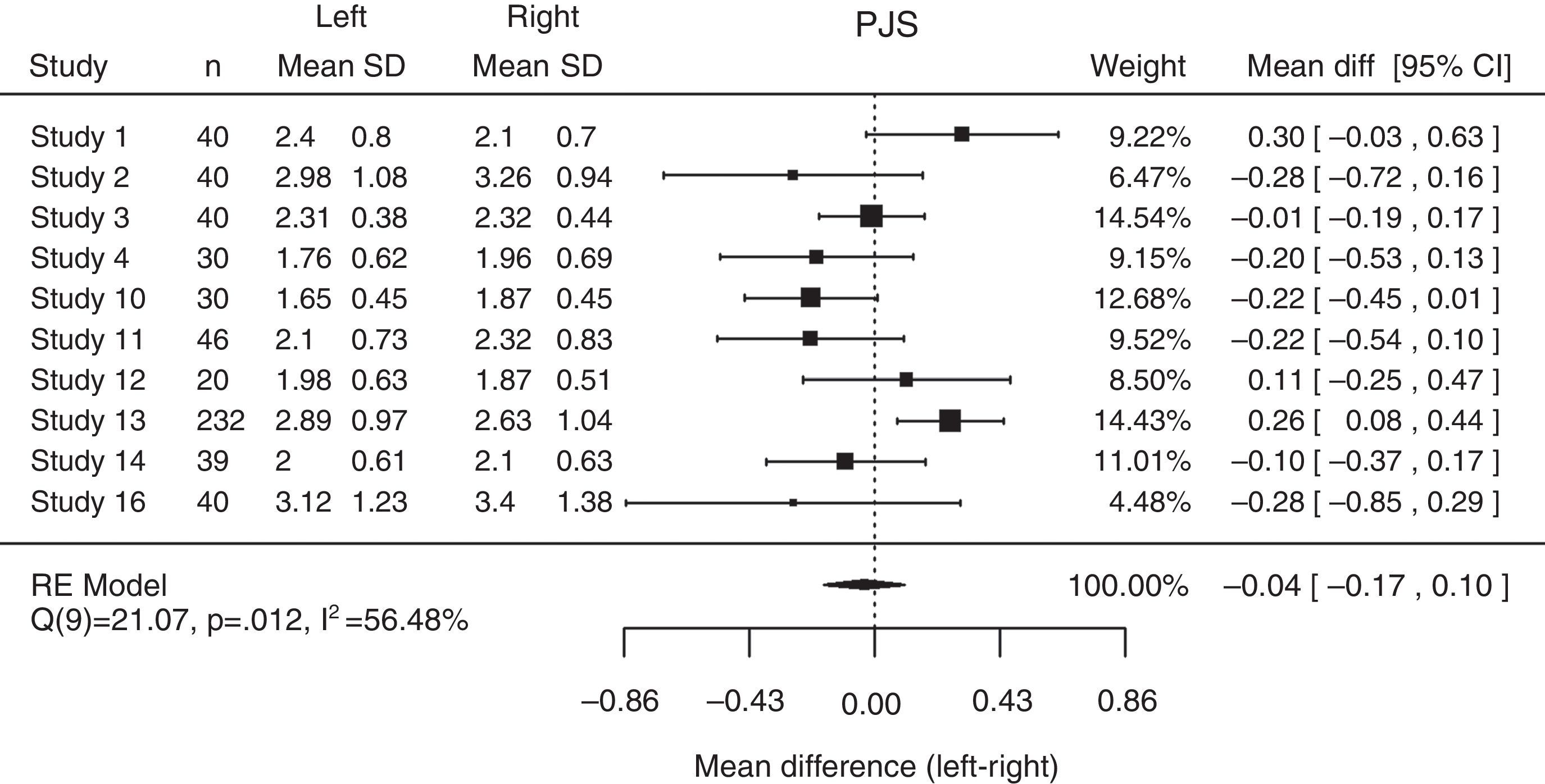
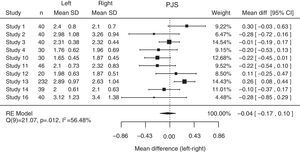
The posterior joint space of the right and left joints showed moderate heterogeneity between the samples (Q(9)=21.07; P=0.012; I2=56.48%) with a mean global difference of −0.04mm (95% CI: −0.17; 0.10) (Fig. 7).
DiscussionJoint space measurements have been used to assess the mandibular condyle position radiographically since this method was used in laminographies.36 Since then the technology has evolved so much that it is now possible to assess the joint space in 3D radiographic imaging with CT, CBCT and MRI. Therefore, a systematic review to assess the relevance of these methods and their scientific evidence is necessary. In the present study, all the articles about joint space assessment on 2D radiographic examination of the TMJ were excluded as these methods have proven lower accuracy both in the image acquisition process and in measurements, than 3D radiographic methods.37 MRI was also excluded because this exam is not indicated to assess hard structures and, as both the mandibular condyle and the glenoid fossa joint space limits are mainly bone and cartilage, this is not the best exam for accurately determine joint space measurements.38 Furthermore, all the articles including extensive treatment that could significantly influence the joint space, like orthodontic treatment and splint therapy, have been excluded. Finally, studies with samples exclusively on the mixed and early permanent dentition were excluded as, according to some authors, the mandibular condyle is not completely formed before the end of the growth, in other words until 15–16 years old.39 The exclusion of studies that only assessed the joint space in less than two separate points of the TMJ was due to the definition of the position of an object in space depending on three coordinates. According to this, joint space analysis done only on one point does not provide enough information to determine the position of the mandibular condyle in the glenoid fossa.
The meta-analysis showed high levels of heterogeneity among the selected studies what is possibly explained by the high heterogeneity between the selected studies: the sample sizes varies between 2427 and 464 patients,31 there are different samples from carefully selected normal joints19,27 to patients presenting malocclusions21,26,31–33,35 or temporomandibular disorders23,24 and different methods19,25,27 were used to determine the joint spaces (as showed during the systematic review). All these factors may have contributed to high heterogeneity between the samples.
The results from this investigation also showed statistically significant differences between the right and left joints for the anterior joint space (AJS), while the opposite was found for the posterior joint space (PJS). However, the mean difference was −0.10mm (95% CI: −0.17; −0.03) and, therefore, it is very close to 0. Moreover, comparison of the AJS and the PJS between the right and left joints was performed on 10 of the retrieved articles, and only two showed statistically significant differences for the AJS. The fact that one of the studies had the biggest sample (n=232) with a power of 16.30% on the meta-analysis might explain the statistically significant result for the AJS. A previous study suggested that this asymmetry would be related to normally asymmetric cranial bases or side preferences during mastication.31 Moreover, most patients show a centric relation-centric occlusion discrepancy, usually caused by a posterior interference that is unilateral in most cases.40–43 As an adaptation, the condyles might move asymmetrically and while the contra-lateral condyle moves sagittaly, the ipsi-lateral rotates to establish a more balanced dental occlusion. The absence of statistically significant differences between right and left joints for the PJS may be explained by stabilization of the TMJ posteriorly by the articular disk.
ConclusionThere is insufficient scientific evidence concerning sagittal joint spaces of the TMJ, as there are no articles with high level of evidence and only one study presents moderate level of evidence.
Although no high level of evidence studies were found, the authors decided to perform a meta-analysis of the mean sagittal joint spaces of the TMJ and the differences between the right and left joints. The mean anterior joint space was 1.86mm (CI 95%: 1.62–2.10), the superior joint space was 2.36mm (CI 95%: 1.99–2.72) and the posterior was 2.22mm (CI 95%: 2.00–2.45). However, a high level of heterogeneity was found, meaning that these results must be considered with care. However, the results of the meta-analysis suggest that the posterior joint space is larger than the anterior joint space. This result is in accordance to the concept in use that the mandibular condyle must be on the most superior-anterior position in the glenoid fossa.5,8–10
The analysis of the difference between the right and left sagittal joint spaces showed statistically significant differences between the two joints in the anterior joint space, but not in the superior and posterior joint spaces.
More research with more solid methodology is needed on this topic.
Conflicts of interestThe authors have no conflicts of interest to declare.