The Psychosocial Care Center (CAPS) is a community-based mental health service in Brazil, which aims to promote the psychosocial rehabilitation of patients. Accordingly, this study describes the drug use evaluation in a primary mental health service in Northeast of Brazil.
SettingCAPS ‘Valter Correia’, São Cristovão, Sergipe, Brazil.
MethodsA cross-sectional study was conducted between August 2009 and May 2010. Initially, Medical records were reviewed and evaluated. Then, we applied interviews with the patients (and/or their informal/family caregivers) attended at the CAPS. Informations were obtained regarding to demographic and clinical features, diagnoses and drugs prescribed. All patients registered in the CAPS were included in the study. The results were statistically analyzed using the EpiInfo and were compared with results from literature.
ResultsThe CAPS ‘Valter Correia’ consists of 101 registered patients, the majority were male (58.4%), illiterate (51.5%), without monthly income (49.5%) and the average age of them 42.2 years (SD = 12.0). Schizophrenia was the most frequent mental disorder (31.5%). The average number of medications by patients was 3.11 (SD = 1.41), and the older group of patients (75-80 years) presented the largest consumption of medications (5.50 drugs/patient). The psychiatric drug class most frequently prescribed was antipsychotics (44.8%). Angiotensin-converting enzyme inhibitors were the most prevalent non-psychiatric therapeutic class (15.8%). It was detected 133 drug-drug interactions (3.0% mild, 54.1% moderate, 29.3% severe and 13.5% contraindicated).
ConclusionThe results revealed the need for monitoring the pharmacotherapy of patients with mental disorders to encourage the rational use of medications.
O Centro de Atenção Psicossocial (CAPS) é um serviço de saúde mental de base comunitária no Brasil, que visa promover a reabilitação psicossocial dos pacientes. O presente estudo descreve a avaliação do uso de medicamentos em um service de saúde mental primário no Nordeste do Brasil.
AmbienteCAPS «Valter Correia», São Cristovão, Sergipe, Brasil.
MétodosEstudo transversal foi realizado entre agosto de 2009 e maio de 2010. Inicialmente, os registros médicos foram revisados e avaliados. Em seguida, foram realizadas entrevistas com os pacientes (e/ou seus cuidadores) atendidos no CAPS. Informações foram obtidas sobre as características demográficas e clínicas, diagnósticos e medicamentos prescritos. Todos os pacientes cadastrados no CAPS foram incluídos no estudo. Os resultados foram analisados estatisticamente utilizando o programa EpiInfo e foram comparados com os resultados da literatura.
ResultadosO CAPS “Valter Correia” é composto por 101 pacientes cadastrados, a maioria do sexo masculino (58,4%), analfabetos (51,5%), sem renda mensal (49,5%) e a média de idade deles era de 42,2 anos (DP = 12,0). A esquizofrenia foi o transtorno mental mais freqüente (31,5%). O número médio de medicamentos por pacientes foi de 3,11 (DP = 1,41), e o grupo de pacientes mais velhos (75-80 anos) apresentou o maior consumo de medicamentos (5,50 medicamentos/paciente). A classe de medicamentos psiquiátricos mais prescrita foi a dos antipsicóticos (44,8%). A classe dos inibidores da enzima conversora da angiotensina foi a mais prevalente classe não-psiquiátrica (15,8%). Foram detectadas 133 interações medicamentosas fármaco-fármaco (3,0% de severidade leve, 54,1% moderada, 29,3% grave e 13,5% contra-indicada).
ConclusãoOs resultados demonstram a necessidade de acompanhamento da farmacoterapia de pacientes com transtornos mentais para incentivar o uso racional de medicamentos.
Mental disorders represent a health problem of social relevance for their high incidence in populations from different countries and culturally distinct societies. We estimated 17–35% prevalence of mental disorders in Brazilian population. However, these disorders are still far from receiving an adequate importance.1–4
In this context, the introduction of psychosocial care centers (CAPS) were one of some health services created, based on Brazilian psychiatric reform. The CAPS are characterized by a day care service, which is proposed as an alternative to a psychiatric hospital. Its main objective is to offer a psychosocial rehabilitation to their patients.5
The sociodemographic characteristics of CAPS patients have an important influence to improve their assistance.2,6 Moreover, psychotropic drugs cause adverse events, which compromises the adherence to treatment and then the quality of life.7
Some studies have demonstrated the relationship between the process of use of drugs, morbidity and mortality related to drugs and as these may trigger adverse reactions. In these studies, problems such as adverse reactions, non-compliance, overdose or inadequate therapy are factors that lead to failure of therapy. If this is not detected and resolved, it can lead to death.8–15
Thus, it is necessary to evaluate the drug utilization in mental health care in order to assess drug therapy, detect the risk factors associated with the use of medications and promote the rational use of drugs. Drug utilization research are defined, according to WHO, as studies on marketing, distribution, prescription, and use of drugs in a society, with special emphasis on the resulting medical, social and economic consequences. These studies have as their main objective the promotion of the rational use of drugs.16,17
In recent years, literature has highlighted the involvement of the pharmacist in programs to optimize the effects of medications, through monitoring the use of drugs. The application of rational criteria can ensure greater compliance with therapy, effectiveness and safety of medications used by patients.18–20
Aim of studyThe present study aimed to evaluate the use of medications by patients in a primary mental health service located in a city at the Northeast of Brazil.
MethodsWe conducted, in an unprecedented way in Sergipe state, a cross-sectional study between August 2009 and May 2010 at a type I psychosocial care center (CAPS) ‘Valter Correia’ in São Cristovão, Sergipe, Brazil. All patients registered in the CAPS (and/or their informal/family caregivers) were included in the study.
CAPS type I is a unit for own psychosocial care with therapeutic workshops and other forms of care and operational capacity to provide healthcare coverage to a population between 20,000 and 70,000 inhabitants, working under two shifts, developing daily activities in mental health.21
Data was collected from patient medical records, such as sociodemographics, clinical characteristics and pharmacological treatments. Sociodemographic data included patient gender, age, educational status, occupational activity, benefits or pensions, income and marital status. Diagnoses (according to the ICD-10 international classification of mental and behavioral disorders)22 and the patient's psychiatric admission history were the clinical characteristics obtained. Details of all psychiatric prescribed medications were also collected, including dose, frequency, administration routes and therapeutic indications. Drugs were classified according to the anatomical therapeutic chemical (ATC) classification system and the defined daily dose (DDD). The ATC/DDD system is a widely used tool for exchanging and comparing data on drug consumption at international, national or local levels.23
In addition, personal interviews were performed (applied to the patients and/or their informal/family caregivers) and collective interviews (applied to groups of patients and/or their informal/family caregivers), in order to compare informations registered on records, collect the missing data on records, identify features on the use of medications and characterize the perception of patients about their health problems and their treatments. The interviews were conducted by a graduate student in pharmacy, previously trained.
The protocols were approved by the Ethics Committee on Human Research at the Federal University of Sergipe. Patients participating in the study were informed about every step and agreed to participate in the survey through a term of informed consent.
The programs EPI-INFO (version 3.5.1-obtained from www.cdc.gov/EpiInfo) and Excel (Microsoft®) were used to statistical analysis. The study protocol was approved by the Ethics Committee of Federal University of Sergipe.
During the development of this study, it was ministered lectures, home visits, workshops and meetings for patients, informal/family caregivers, and for the multidisciplinary team of the CAPS. The themes approached the rational use of medications, mental disorder, psychopharmacology, medicinal plants, hygiene, handicraft, culture, integration, social inclusion, first aid and use of alcohol, tobacco and others drugs.
Results101 registered patients were distributed in intensive (13.86%), semi-intensive (52.48%) and non-intensive (33.66%) regime at CAPS Valter Correia. Those regimes are defined by their clinical conditions, based on clinical care and therapy of patients. According to their needs, patients belonging to intensive regime require daily care by a specialized multidisciplinary team (up to 25 days/month), patients belonging to semi-intensive regime require frequent care (up to 12 days/month) and patients belonging to non-intensive regime require less frequent attendance (up to 3 days of the month).
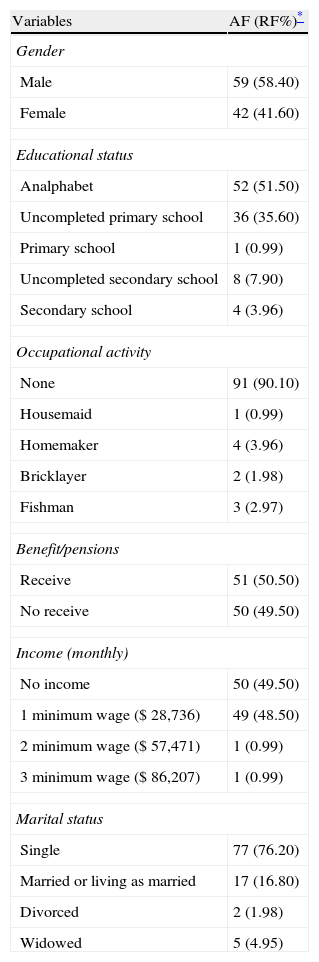
The mean age of patients was 42.18±12.01-years-old, median of 42 years. Table 1 describes the distribution of other important socio-demographic parameters.
Sociodemographics data of patients attended at CAPS Valter Correia (n=101).
| Variables | AF (RF%)* |
| Gender | |
| Male | 59 (58.40) |
| Female | 42 (41.60) |
| Educational status | |
| Analphabet | 52 (51.50) |
| Uncompleted primary school | 36 (35.60) |
| Primary school | 1 (0.99) |
| Uncompleted secondary school | 8 (7.90) |
| Secondary school | 4 (3.96) |
| Occupational activity | |
| None | 91 (90.10) |
| Housemaid | 1 (0.99) |
| Homemaker | 4 (3.96) |
| Bricklayer | 2 (1.98) |
| Fishman | 3 (2.97) |
| Benefit/pensions | |
| Receive | 51 (50.50) |
| No receive | 50 (49.50) |
| Income (monthly) | |
| No income | 50 (49.50) |
| 1 minimum wage ($ 28,736) | 49 (48.50) |
| 2 minimum wage ($ 57,471) | 1 (0.99) |
| 3 minimum wage ($ 86,207) | 1 (0.99) |
| Marital status | |
| Single | 77 (76.20) |
| Married or living as married | 17 (16.80) |
| Divorced | 2 (1.98) |
| Widowed | 5 (4.95) |
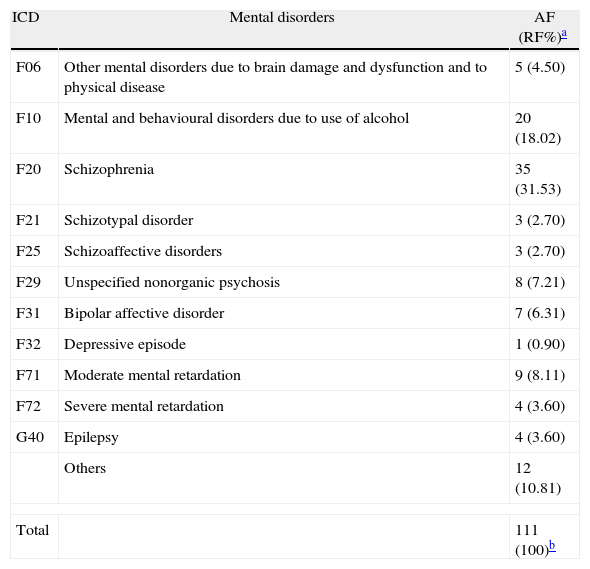
Schizophrenia was the most prevalent mental disorder (31.53%). The mental disorder profile presented by the patients attended on the CAPS, according with the international classification of mental and behavioral disorders (ICD-10)22 is described in Table 2.
Mental disorders diagnosed at CAPS patients according to ICD-10 (n=101).
| ICD | Mental disorders | AF (RF%)a |
| F06 | Other mental disorders due to brain damage and dysfunction and to physical disease | 5 (4.50) |
| F10 | Mental and behavioural disorders due to use of alcohol | 20 (18.02) |
| F20 | Schizophrenia | 35 (31.53) |
| F21 | Schizotypal disorder | 3 (2.70) |
| F25 | Schizoaffective disorders | 3 (2.70) |
| F29 | Unspecified nonorganic psychosis | 8 (7.21) |
| F31 | Bipolar affective disorder | 7 (6.31) |
| F32 | Depressive episode | 1 (0.90) |
| F71 | Moderate mental retardation | 9 (8.11) |
| F72 | Severe mental retardation | 4 (3.60) |
| G40 | Epilepsy | 4 (3.60) |
| Others | 12 (10.81) | |
| Total | 111 (100)b | |
Some patients presented other diseases associated to mental disorders, such as arterial hypertension (18.81%), diabetes mellitus (10.9%), gastritis (10.9%), asthma (4.0%), others heart problems (7.9%) and hypothyroidism (2.2%).
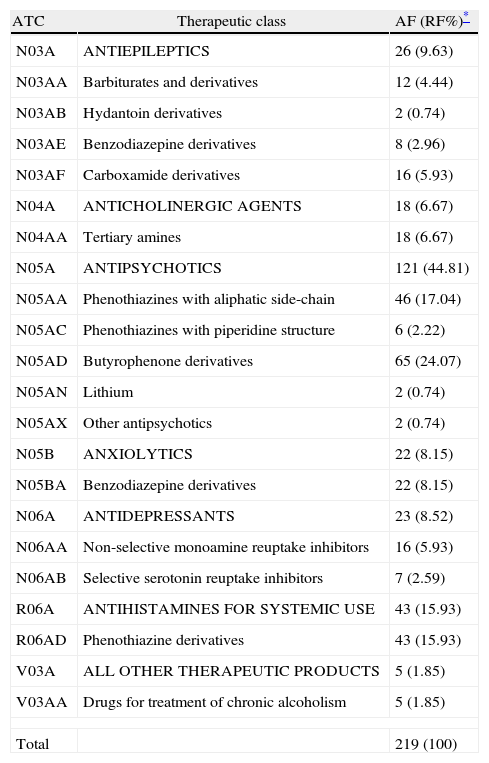
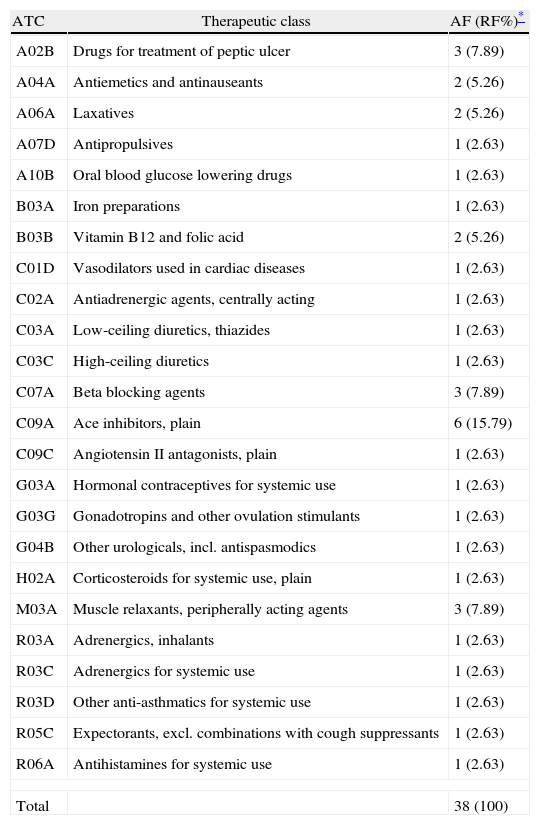
Regarding to the pharmacotherapeutic profile, Table 3 exhibits the therapeutic classes of psychiatric drugs used by patients attended at CAPS. Table 4 describes the therapeutic classes of non-psychiatric drugs used by patients attended at CAPS, according to the WHO-ATC/DDD methodology. The psychiatric drug class most frequently prescribed was antipsychotics (44.8%) and the non-psychiatric drug class most prevalent was angiotensin-converting enzyme inhibitors (15.8%).
Therapeutic classes of psychotropic drugs used by patients attended at CAPS Valter Correia, according to ATC classification.
| ATC | Therapeutic class | AF (RF%)* |
| N03A | ANTIEPILEPTICS | 26 (9.63) |
| N03AA | Barbiturates and derivatives | 12 (4.44) |
| N03AB | Hydantoin derivatives | 2 (0.74) |
| N03AE | Benzodiazepine derivatives | 8 (2.96) |
| N03AF | Carboxamide derivatives | 16 (5.93) |
| N04A | ANTICHOLINERGIC AGENTS | 18 (6.67) |
| N04AA | Tertiary amines | 18 (6.67) |
| N05A | ANTIPSYCHOTICS | 121 (44.81) |
| N05AA | Phenothiazines with aliphatic side-chain | 46 (17.04) |
| N05AC | Phenothiazines with piperidine structure | 6 (2.22) |
| N05AD | Butyrophenone derivatives | 65 (24.07) |
| N05AN | Lithium | 2 (0.74) |
| N05AX | Other antipsychotics | 2 (0.74) |
| N05B | ANXIOLYTICS | 22 (8.15) |
| N05BA | Benzodiazepine derivatives | 22 (8.15) |
| N06A | ANTIDEPRESSANTS | 23 (8.52) |
| N06AA | Non-selective monoamine reuptake inhibitors | 16 (5.93) |
| N06AB | Selective serotonin reuptake inhibitors | 7 (2.59) |
| R06A | ANTIHISTAMINES FOR SYSTEMIC USE | 43 (15.93) |
| R06AD | Phenothiazine derivatives | 43 (15.93) |
| V03A | ALL OTHER THERAPEUTIC PRODUCTS | 5 (1.85) |
| V03AA | Drugs for treatment of chronic alcoholism | 5 (1.85) |
| Total | 219 (100) | |
Therapeutic classes of non-psychotropic drugs used by patients attended at CAPS Valter Correia, according to ATC classification.
| ATC | Therapeutic class | AF (RF%)* |
| A02B | Drugs for treatment of peptic ulcer | 3 (7.89) |
| A04A | Antiemetics and antinauseants | 2 (5.26) |
| A06A | Laxatives | 2 (5.26) |
| A07D | Antipropulsives | 1 (2.63) |
| A10B | Oral blood glucose lowering drugs | 1 (2.63) |
| B03A | Iron preparations | 1 (2.63) |
| B03B | Vitamin B12 and folic acid | 2 (5.26) |
| C01D | Vasodilators used in cardiac diseases | 1 (2.63) |
| C02A | Antiadrenergic agents, centrally acting | 1 (2.63) |
| C03A | Low-ceiling diuretics, thiazides | 1 (2.63) |
| C03C | High-ceiling diuretics | 1 (2.63) |
| C07A | Beta blocking agents | 3 (7.89) |
| C09A | Ace inhibitors, plain | 6 (15.79) |
| C09C | Angiotensin II antagonists, plain | 1 (2.63) |
| G03A | Hormonal contraceptives for systemic use | 1 (2.63) |
| G03G | Gonadotropins and other ovulation stimulants | 1 (2.63) |
| G04B | Other urologicals, incl. antispasmodics | 1 (2.63) |
| H02A | Corticosteroids for systemic use, plain | 1 (2.63) |
| M03A | Muscle relaxants, peripherally acting agents | 3 (7.89) |
| R03A | Adrenergics, inhalants | 1 (2.63) |
| R03C | Adrenergics for systemic use | 1 (2.63) |
| R03D | Other anti-asthmatics for systemic use | 1 (2.63) |
| R05C | Expectorants, excl. combinations with cough suppressants | 1 (2.63) |
| R06A | Antihistamines for systemic use | 1 (2.63) |
| Total | 38 (100) | |
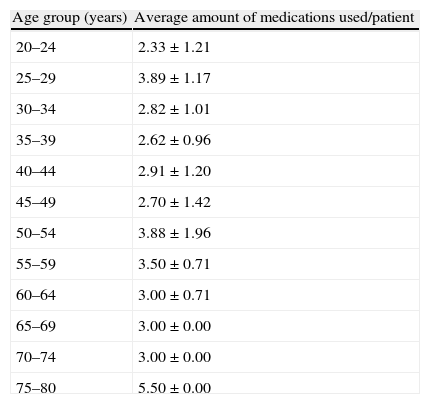
The average number of medications (psychotropic and non-psychotropic) used by patients was 3.11±1.41 medications/patients, median 3 (Table 5).
Mean number of medications (psychotropic and non-psychotropic) used by patients attended at CAPS Valter Correia, according to the age group.
| Age group (years) | Average amount of medications used/patient |
| 20–24 | 2.33±1.21 |
| 25–29 | 3.89±1.17 |
| 30–34 | 2.82±1.01 |
| 35–39 | 2.62±0.96 |
| 40–44 | 2.91±1.20 |
| 45–49 | 2.70±1.42 |
| 50–54 | 3.88±1.96 |
| 55–59 | 3.50±0.71 |
| 60–64 | 3.00±0.71 |
| 65–69 | 3.00±0.00 |
| 70–74 | 3.00±0.00 |
| 75–80 | 5.50±0.00 |
Values are expressed as mean ± standard deviation.
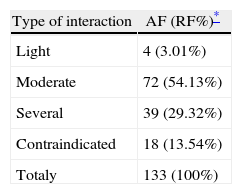
Table 6 shows the percentage of drug interactions presented by pacients of the CAPS, according to the degree of severity.
Drug interactions (drug–drug) presented by patients attended at CAPS Valter Correia, classified by degreed severity.
| Type of interaction | AF (RF%)* |
| Light | 4 (3.01%) |
| Moderate | 72 (54.13%) |
| Several | 39 (29.32%) |
| Contraindicated | 18 (13.54%) |
| Totaly | 133 (100%) |
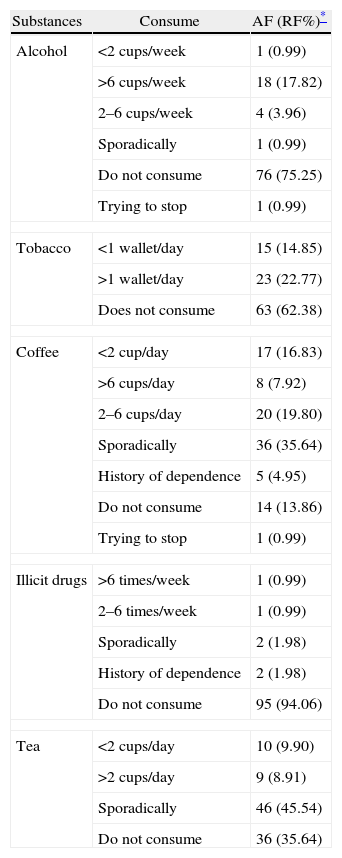
With respect to consumption of others substances, it is observed in Table 7 the profile of use alcohol, tobacco, illicit drugs and teas.
Consume of alcohol, tobacco, coffee, illicit drugs and tea by patients attended at CAPS Valter Correia.
| Substances | Consume | AF (RF%)* |
| Alcohol | <2 cups/week | 1 (0.99) |
| >6 cups/week | 18 (17.82) | |
| 2–6 cups/week | 4 (3.96) | |
| Sporadically | 1 (0.99) | |
| Do not consume | 76 (75.25) | |
| Trying to stop | 1 (0.99) | |
| Tobacco | <1 wallet/day | 15 (14.85) |
| >1 wallet/day | 23 (22.77) | |
| Does not consume | 63 (62.38) | |
| Coffee | <2 cup/day | 17 (16.83) |
| >6 cups/day | 8 (7.92) | |
| 2–6 cups/day | 20 (19.80) | |
| Sporadically | 36 (35.64) | |
| History of dependence | 5 (4.95) | |
| Do not consume | 14 (13.86) | |
| Trying to stop | 1 (0.99) | |
| Illicit drugs | >6 times/week | 1 (0.99) |
| 2–6 times/week | 1 (0.99) | |
| Sporadically | 2 (1.98) | |
| History of dependence | 2 (1.98) | |
| Do not consume | 95 (94.06) | |
| Tea | <2 cups/day | 10 (9.90) |
| >2 cups/day | 9 (8.91) | |
| Sporadically | 46 (45.54) | |
| Do not consume | 36 (35.64) | |
The CAPS is an open and community service of mental health on the unified health system (SUS) in Brazil. Its main objective is to establish a reference place to treatment for people with mental disorders, who need an intensive care related to their severity and/or persistence demand.5
101 registered patients at CAPS ‘Valter Correia’ were distributed in intensive (13.86%), semi-intensive (52.48%) and non-intensive (33.66%) regime. The average age of patients was 42.18±12.01 years. These results were in concordance by other studies, which claim that mental disorders affect people of all ages, with the prevalence on 30–49 years.24,25 The presence of mental disorder at this age group influences the way of life, interrupting productivity as a result of disability caused by disease.24
It is observed in Table 1 that the CAPS consisted mainly of male patients (58.50%), which differs from others studies that indicate the prevalence of females.24,26
Most patients were single (76.20%), childless (54.50%), illiterate (51.50%), without occupation (90.10%), without benefits (49.50%) and without monthly income (49.50%). These results suggest that the presence of mental disorder can influence the cultural background of people and the chance to attend school is low, which can make it difficult to enter at university and gain a good job. According to OMS (2001)2, five from ten causes of inability on the world are mental disorder.
Regarding to the nosological profiles, Table 2 reveals that there are patients with more than one type of mental disorder and that schizophrenia is the most prevalent mental disorder (31.53%).
Schizophrenia is one of the most serious neuropsychiatric diseases and affects about 1% of world population. Currently, there is no specific prevention for this disease. Neuroleptic or antipsychotic drugs are used as the primary treatment for all stages of the disease.27
Depressive episodes are common mental disorders on Brazilian population,28–31 but we found in only 0.90% of our CAPS patients. This difference should be caused due to the introduction of a new model of psychiatric care, which is still suffering transition in Brazil. Part of the population, who suffers from mood and anxiety disorders, is probably under-diagnozed. Another part, even receiving the correct medical diagnosis, chooses to receive ambulatory treatment without resort to the CAPS, which could be in consequence of stigmas fear.
Consumption of alcohol and others drugs is an important cause of disorder. Mental behavioral disorders due the consumption of alcohol were found in 18.02%, due the consumption of multiple drugs and others psychoactive substances in 0.90% and due to the use of cocaine in 0.90%. Those patients should be indicated for an AD type of CAPS.
The psychiatric drug class most frequently prescribed was antipsychotics (44.8%), described in Table 3. Angiotensin-converting enzyme inhibitors (ACEI) were the most prevalent non-psychiatric drug class (15.8%) (Table 4). Those results are in consistence with the most prevalent diseases, schizophrenia for antipsychotics and hypertension for ACEI medications.
There is currently a very large number of antipsychotic medications, with different profile of side effects, but with similar potency when use in equivalent doses. However, there are individual differences on efficacy, tolerance and cost. Particular context should be used to choose the adequate drug.
The average number of medications used by patients was 3.11±1.41 medications/patients. The largest consumption of medications was found in the 75–80 years group, 5.5 medications for patient (Table 5). These data are in with the literature. Elderly population is marked by a higher frequency of chronic degenerative diseases. It has greater demand for health services and medication, which predisposes the geriatric population to great risks with the practice of polypharmacy and adverse effects of medications.32
In regard to drug interactions,33–35 3.0% mild, 54.1% moderate, 29.3% severe and 13.5% contraindicated (Table 6). Those results demonstrate the need to evaluate possible interventions, since drug interactions may, among other things, increase undesired medications effects, lead to ineffective therapy and endanger the life of patient.36–39
It is observed in Table 7 that 24.75% of patients consumed alcohol, 37.62% tobacco, 86.14% caffeine, 5.94% illicit drugs and 64.36% tea. It is necessary a further detailed study, since these substances can interact with several medications.
The medications have an important role in the health system, they can save lives or remove the signs and symptoms of numerous diseases.40 However, the drugs may increase the costs of health care if used improperly.41 According to WHO data, hospitals spend 15%–20% of their budgets to deal with the complications caused by misuse of medications.42
In this context, pharmacists are professionals who can actively participate in the multidisciplinary team, make the management of pharmacotherapy, assess the use of medications, provide guidelines and perform pharmacotherapeutic monitoring of patients, which contribute to the rational use of medications and improve the quality of life of patients.43
ConclusionOur results revealed the need for monitoring the pharmacotherapy of patients with mental and behavioral disorders to encourage the rational use of medications. This monitoring is necessary, since these patients are polymedicated, have other comorbidities, and use drugs that cause adverse effects, which compromise the adherence of treatment and consequently their quality of life.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank the Fundação de Apoio à Pesquisa e à Inovação Tecnológica do Estado de Sergipe/FAPITEC-SE and National Council of Technological and Scientific Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico/CNPq/Brazil) for the fellowship support.