Morbidity and mortality due to cardiovascular causes in patients with schizophrenia are higher than in the general population, a fact that has been observed more since second generation anti-psychotics came into general use.
ObjectivesTo determine the incidence of metabolic syndrome in patients with a previously untreated first psychotic episode, as well as the prospective changes in the parameters that define the criteria of metabolic syndrome.
MethodAn observational study with a prospective cohort design including patients who were admitted to the Acute Unit of Donostia Hospital.
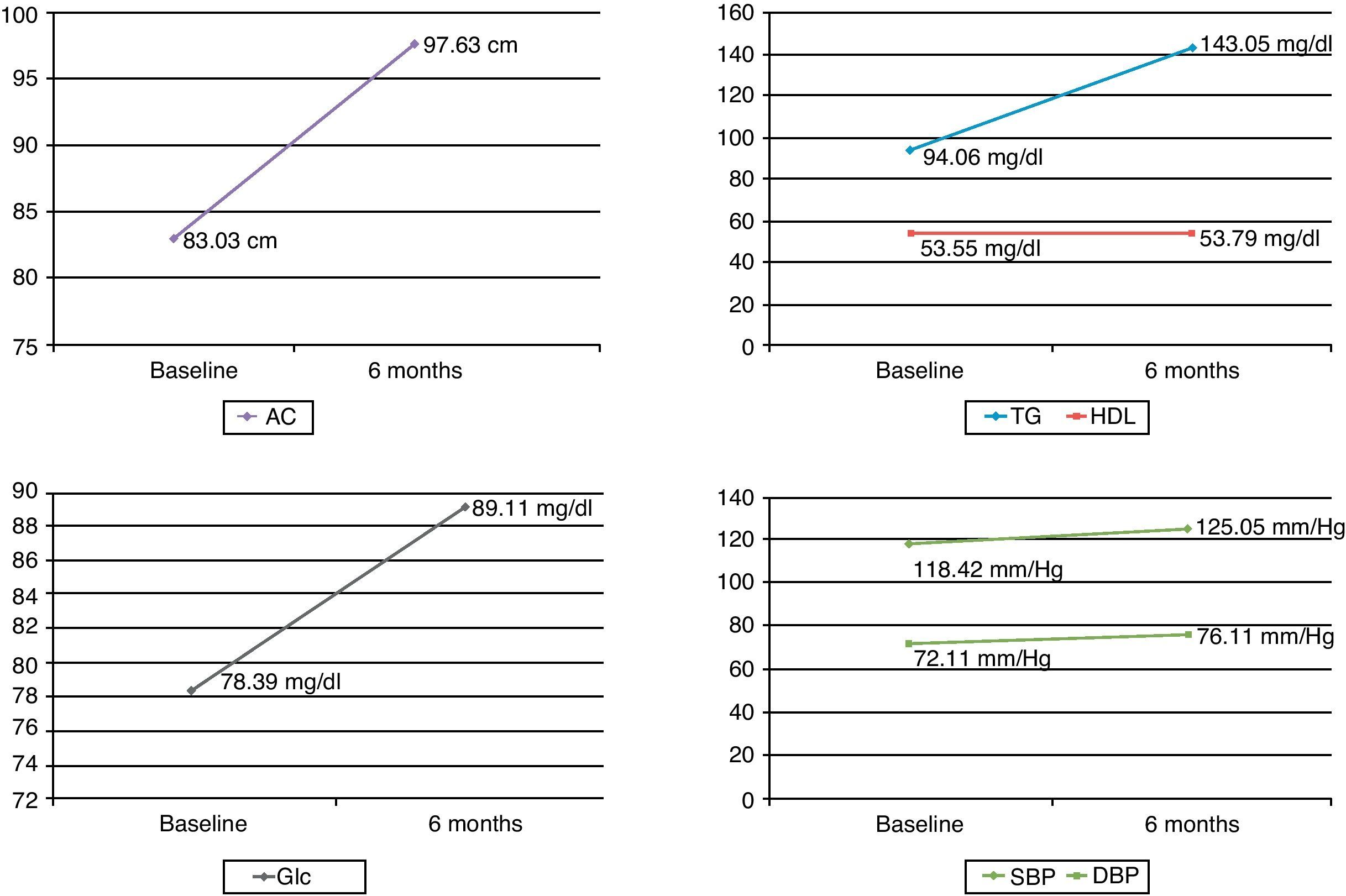
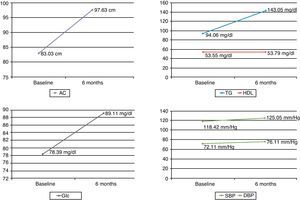
ResultsA total of 21 patients were included in the study, of which 19 completed it. Just over one-quarter (26.3%) of the patients developed a metabolic syndrome at six months. Statistically significant differences were observed in the following parameters: (1) abdominal perimeter measurement with an increase of 14.6cm at six months (P=.001); (2) triglyceride levels with a mean increase over the initial measurement of 48.99mg/dl (P=.039); and (3) fasting blood glucose levels with a mean increase of 10.72mg/dl (P=.001).
ConclusionsSignificant changes were observed in metabolic parameters in a short period with the subsequent risk of associated cardiovascular events in a group of young patients. Actions are required to be directed at ensuring appropriate monitoring of these patients in order to measures to minimise the risks.
La morbimortalidad por causas cardiovasculares en pacientes con esquizofrenia es superior a la de la población general, hecho que se ha puesto más de manifiesto desde la generalización del uso de antipsicóticos de segunda generación.
ObjetivosExaminar la incidencia del síndrome metabólico tras seis meses de tratamiento antipsicótico en pacientes con un primer episodio psicótico no tratado con anterioridad y determinar cambios prospectivos en los parámetros que definen los criterios del síndrome metabólico.
MétodoEstudio observacional con diseño de cohortes prospectivo incluyendo pacientes que ingresaron en la unidad de agudos del Hospital Donostia.
ResultadosVeintiún pacientes fueron incluidos en el estudio, completando el mismo 19. Un 26,3% de los pacientes desarrollaron síndrome metabólico a los 6 meses. Se observaron diferencias estadísticamente significativas en los siguientes parámetros: 1) medida del perímetro abdominal con un incremento de 14,6cm a los 6 meses (p = 0,001); 2) niveles de triglicéridos con un incremento medio sobre la medida inicial de 48,99mg/dl (p=0,039); 3) niveles de glucosa en ayunas con un aumento medio de 10,72mg/dl (p=0,001).
ConclusionesSe observaron importantes cambios en los parámetros metabólicos en un periodo corto con el consiguiente riesgo de eventos cardiovasculares asociado en un grupo de pacientes jóvenes. Son necesarias intervenciones dirigidas a asegurar una correcta monitorización de estos pacientes que permitan llevar a cabo medidas para minimizar riesgos.
Patients with schizophrenia have higher morbidity and mortality rates and greater risk of premature death in relation to medical diseases, especially cardiovascular disorders, than the general population.1,2 The reasons for this greater risk of cardiovascular disorders among patients with schizophrenia are complex and they are not uniform in all cases.3
Without a doubt, the adverse effects of medication, the increase in suicide, as well as a less healthy lifestyle and some self-care deficits, all contribute substantially to the aforementioned increase in morbidity and mortality. However, there is more and more evidence4,5 that even before receiving antipsychotic treatment, there is an increase in metabolic disturbances in schizophrenic patients. Furthermore, it seems that factors such as diet, socioeconomic level and health habits are not enough to justify this risk.6
In this vein, several authors7,8 suggest that schizophrenia is like an “accelerated-aging syndrome”. They propose a broader concept of schizophrenia than the usual, portraying it as a developmental disorder, with anomalies in many brain functions, and not just psychosis. This concept also suggests that schizophrenia affects many parts of the body, not just the brain.
Currently, the introduction and general use of atypical antipsychotics in the clinical field is revealing the relationship between these drugs and adverse endocrine-metabolic and cardiovascular effects. Meanwhile, in the general population, especially in Western countries, a dramatic increase is emerging in the incidence and prevalence of metabolic syndrome. Consequently, metabolic syndrome in patients with schizophrenia constitutes “an epidemic within an epidemic”.
The criteria for metabolic syndrome include abdominal obesity, disturbances in blood glucose levels and in cholesterol and high blood pressure. These symptoms represent a set of risk factors for cardiovascular disease with an increase in mortality.
There are different prospective studies9–15 on patients with their first psychotic episode that evaluate the presence of metabolic disturbances throughout the antipsychotic treatment process. These studies are interesting for different reasons. Firstly, there is no effect from maintaining previous treatments. Secondly, it is likely that the effect that the illness has on patient lifestyle in these initial phases is minimal. Thirdly, to detect impairment in glucose or lipid metabolism, a long-term follow-up is necessary. In this study, we focused on the population of Guipúzcoa (Spain). We examined the incidence rate for metabolic syndrome 6 months after initiating antipsychotic treatment in a sample of patients experiencing their first psychotic episode that had not been treated previously. Furthermore, we determined prospective changes in the parameters that define the criteria for metabolic syndrome in this sample.
Methods and materialsThis is a naturalistic, prospective study with a 6-month follow-up carried out in the Acute Unit of Donostia Hospital, located in the Guipúzcoa province. It is the only acute psychiatric hospital unit and the only 24-h emergency room in the entire province.
The protocol for the study was approved by the Research Ethics Committee at Donostia Hospital and in accordance with the Declaration of Helsinki. The patients selected for the study came from a consecutive sample of psychotic patients who were admitted to our ward over 1 year.
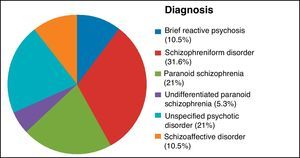
Patients complied with the following criteria: (1) aged between 18 and 55 years, (2) suffering first psychotic episode that fulfilled DSM-IV criteria for brief psychotic disorder, schizophreniform disorder, schizophrenia or schizoaffective disorder and (3) understanding the nature of the study and signing an informed consent document. Exclusion criteria were: (1) fulfilling DSM-IV criteria for drug dependency, (2) fulfilling DSM-IV criteria for mental retardation, (3) suffering a serious medical illness (excluding previous metabolic pathology), (4) negative blood test and (5) starting mood-stabiliser treatment.
Sociodemographic and clinical variables were collected from information given by the patients themselves, their clinical histories, an “ad hoc” questionnaire and psychopathological examination. A physical examination was performed, involving the measurements of: blood pressure, weight, height and abdominal circumference. Blood pressure was taken with the patient seated, after 5min of rest. Abdominal circumference was measured by measuring the midline between the lower part of the ribcage and the crest of the pelvis (antero-superior iliac spine) while the patient was standing. The following complementary tests were also performed: brain CT scan, ECG, blood count, blood chemistry analysis (metabolic profile, measuring glucose, total cholesterol, HDL and LDL cholesterol and triglycerides), blood test (HIV, HCV, HBV and VDRL), hormone profile (TSH, T4 and prolactin) and cortisol. The physical and analytic examinations were carried out before starting antipsychotic treatment.
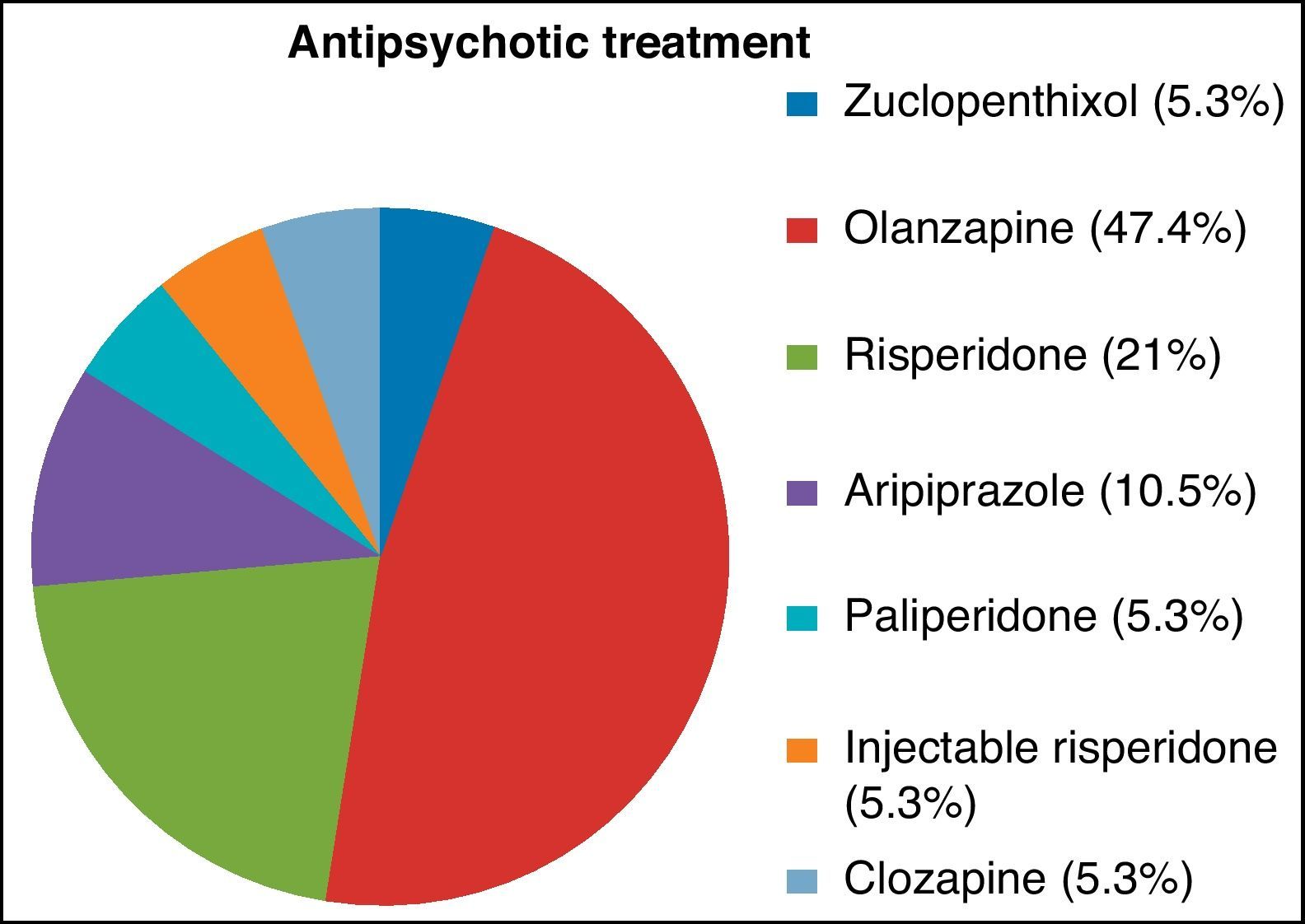
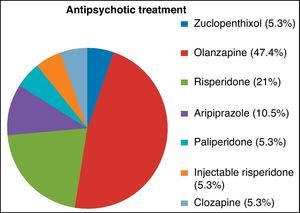
Patients included in this study began antipsychotic treatment according to clinical judgement. Concomitant treatments used included benzodiazepines, anticholinergics and antidepressants. If there were tolerability and/or effectiveness issues, the antipsychotic drug was changed based on clinical judgement.
Measurements of glucose, total cholesterol, HDL and LDL cholesterol, triglycerides, prolactin, cortisol, blood pressure, weight and abdominal circumference were all repeated after 6 months.
When the patients were recruited, we notified them, both orally and in writing, that they were to fast for at least 10h (except for water and medication) before attending this clinical visit 6 months later. One day before the visit, they were reminded of this. Analyses were performed between 8 and 9am.
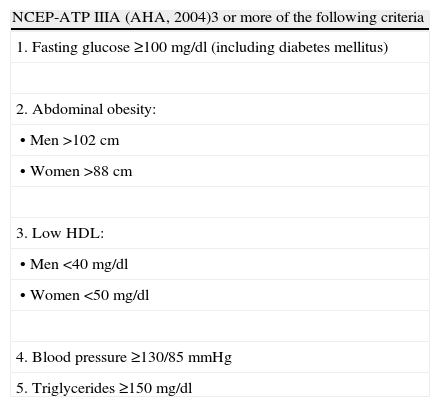
The main assessment variables of the present study were the incident cases and the changes in plasma concentrations from the criteria that define metabolic syndrome according to the modified “National Cholesterol Education Program Adult Treatment Panel (NCEP ATP IIIA)” criteria (Table 1). For the statistical procedure, the Wilcoxon signed-rank test was used. The Statistical Package for Social Science (SPSS) programme, version 12.0, was used for all statistical analyses. The level of significance was established as P=.05 for all tests.
Diagnostic criteria for metabolic syndrome according to the modified “National Cholesterol Education Program Adult Treatment Panel (NCEP ATP IIIA)”, American Heart Association (AHA).
| NCEP-ATP IIIA (AHA, 2004)3 or more of the following criteria |
| 1. Fasting glucose ≥100mg/dl (including diabetes mellitus) |
| 2. Abdominal obesity: |
| • Men >102cm |
| • Women >88cm |
| 3. Low HDL: |
| • Men <40mg/dl |
| • Women <50mg/dl |
| 4. Blood pressure ≥130/85mmHg |
| 5. Triglycerides ≥150mg/dl |
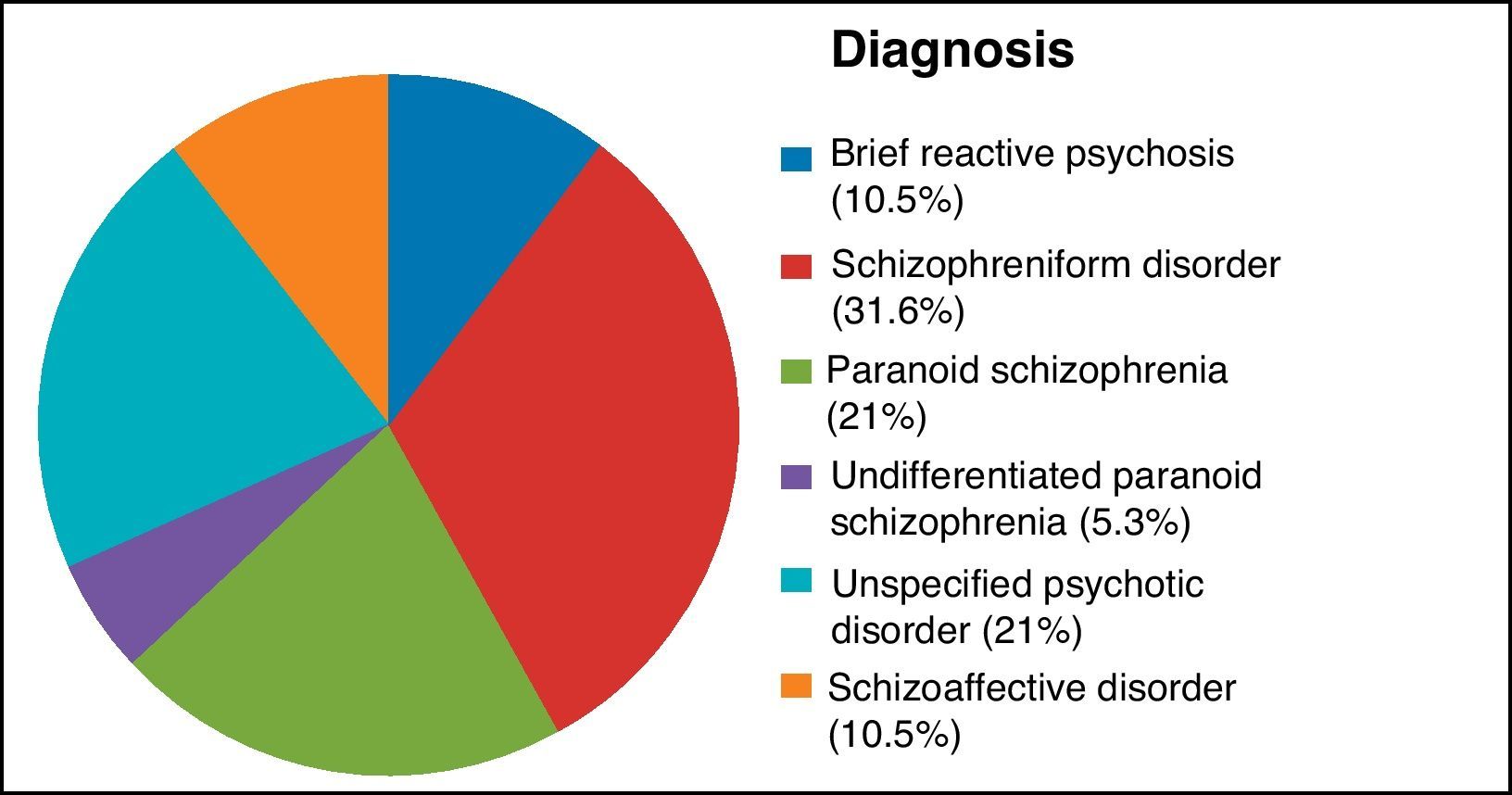
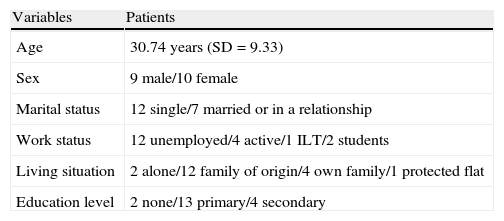
A total of 27 patients were examined for possible inclusion in the study; 2 refusing to participate in the study and 4 not fulfilling inclusion criteria. A total of 21 patients were thus included in the study. Of those, 9.5% left the study (2 patients refused to be evaluated after 6 months). Ultimately, 19 patients (9 men and 10 women) were included in the analysis performed (Table 2), with a mean age of 30.74 years (SD 9.33). Of these patients, there were none who fulfilled criteria for metabolic syndrome at the start of the study, according to ATP IIIA (Figs. 1 and 2).
Sociodemographic variables.
| Variables | Patients |
| Age | 30.74 years (SD=9.33) |
| Sex | 9 male/10 female |
| Marital status | 12 single/7 married or in a relationship |
| Work status | 12 unemployed/4 active/1 ILT/2 students |
| Living situation | 2 alone/12 family of origin/4 own family/1 protected flat |
| Education level | 2 none/13 primary/4 secondary |
SD: standard deviation; ILT: temporary inability to work.
The incidence of new cases 6 months after starting antipsychotic treatment was 26.3%, with a confidence interval of 95%. Of every 100 patients treated, between 6.5 and 46.1 developed metabolic syndrome.
Incidence rateThe number of new patient cases that developed metabolic syndrome every month was 0.044. That is to say, of every 100 patients treated, 4.4 developed metabolic syndrome.
Using a 95% confidence interval, of every 100 patients treated over 1 month, between 1.6 and 11.8 new cases would appear.
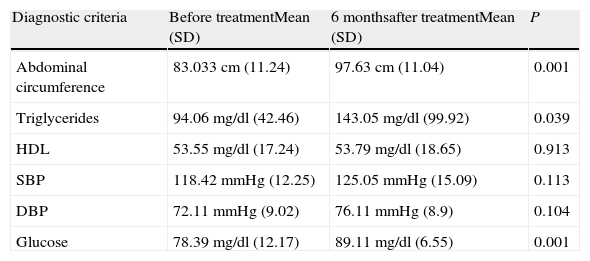
Changes in biometric parameters (Table 3 and Fig. 3)After 6 months of antipsychotic treatment, the concentrations of triglycerides and glucose increased significantly. An increase was also observed in abdominal circumference (Table 3). On the other hand, no change was observed in HDL concentrations (Fig. 3).
Changes in biometric parameters. Wilcoxon signed-rank test.
| Diagnostic criteria | Before treatmentMean (SD) | 6 monthsafter treatmentMean (SD) | P |
| Abdominal circumference | 83.033cm (11.24) | 97.63cm (11.04) | 0.001 |
| Triglycerides | 94.06mg/dl (42.46) | 143.05mg/dl (99.92) | 0.039 |
| HDL | 53.55mg/dl (17.24) | 53.79mg/dl (18.65) | 0.913 |
| SBP | 118.42mmHg (12.25) | 125.05mmHg (15.09) | 0.113 |
| DBP | 72.11mmHg (9.02) | 76.11mmHg (8.9) | 0.104 |
| Glucose | 78.39mg/dl (12.17) | 89.11mg/dl (6.55) | 0.001 |
Regarding both systolic and diastolic blood pressures, they tended to increase but significant differences could not be established.
DiscussionEven before the first antipsychotic treatment appeared, there were already studies that suggested that there was a physiopathological connection between psychosis and metabolic disturbances.16
However, these studies are mixed and there is a lack of consistency among them. Even though some studies have not found previous anomalies11 or have not found them in specific parameters,4,17 there are increasingly more studies concluding that patients recently diagnosed schizophrenia present metabolic disturbances before using antipsychotics4,5 (as do even their relatives18). In order to be able to shed light on this question, studies of patients experiencing their first psychotic episode are useful, as potentially confusing factors that could interfere with these findings are eliminated. In our study, no patient complied with the criteria for a metabolic syndrome diagnosis prior to antipsychotic treatment.
As a result of the generalised use of second generation antipsychotics in clinical practice, the number of studies that evaluate metabolic disturbances in patients suffering their first psychotic episode has increased. However, most of them study short-term changes and many analyse changes in the different parameters individually. Consequently, there are fewer studies that observe the development of metabolic syndrome as a whole. Some of the studies that evaluate incident cases of metabolic syndrome observed a 10% incidence of metabolic syndrome after 6 weeks, and 13.6% after 1 year.12,13 In the present study, the figures were higher, with an incidence of 26.3% after 6 months.
Upon analysing the parameters that define metabolic syndrome in further detail, we were able to highlight that, in the present study, significant differences in abdominal circumference and in mean plasma concentrations of fasting glucose and triglycerides could be observed as early as 6 months. These changes come with the subsequent risk of associated cardiovascular events. It is remarkable that this increase was observed over a relatively short time period and in a group of young patients.
It has been suggested that type 2 diabetes is an illness with a long prodromal asymptomatic period. Consequently, to detect new-onset diabetes, a longer time period is necessary,14 even though the present study observed that time period of 6 months was sufficient to produce an increase in plasma concentrations of fasting glucose.
That the risk of cardiovascular events is different according to sex is known, and these differences are detailed in various works. In the Saddichha12 study, significant increases in fasting glucose were found in men after 6 weeks, but not in women. In the study carried out by Attux,15 significant increases were found in abdominal circumference after 6 months, but only in women.
When selecting which antipsychotic to use in patients experiencing their first psychotic episode, it is necessary to keep in mind the different levels of risk of developing different adverse effects, which are established according to the evidence available.19–22
To date, the mechanisms by which antipsychotics produce their effects in worsening the metabolic profile are poorly understood and vary greatly. For example, when there is an increase in weight, many receptors are thought to be involved. One of these for which the maximum evidence exists is the H1 receptor, despite the fact that the mechanism by which this antagonistic receptor induces weight gain is unknown. Likewise, even though the magnitude of weight gain explains the greatest part of new-onset type 2 diabetes in most cases, as it happens in the general population, there have been some cases in which the onset of diabetes occurred without changes in body weight.23,24 Recent studies25 have suggested that certain antipsychotics affect the glucose transporter, in such a way that direct mitigation of its function would produce elevations in surrounding glucose and compensatory hypersecretion of insulin. More long-term prospective studies of patients experiencing their first psychotic episode are still necessary. They would help shed light on an issue where the current norm is great variability and lack of consistency among the different studies regarding results and mechanisms implicated in producing the disturbances.
The limitations of the current study were the sample size as well as the length of follow-up. Likewise, due to the fact that participants were not in inpatient care upon performing the 6-month visit, it is possible that some patients did not follow the proposed fasting regimen. This variable is difficult to control, beyond checking this compliance right before performing the blood test.
As a general reflection, it should be emphasised that, after the generalisation of second generation antipsychotic use and the emergence of its adverse metabolic effects, different international bodies20 have drafted and published a consensus in which monitoring the physical health of these patients was recommended. In addition, the Spanish Society of Psychiatry and of Biological Psychiatry26 published a consensus in 2007, “Consensus regarding the physical health of patients with schizophrenia”. In this consensus, a protocol is detailed for monitoring physical health.
In 2010, a study at the national level analysed the impact of disseminating this consensus regarding the monitoring of parameters predictive of diabetes and cardiovascular risk. The effectiveness of dissemination was confirmed upon seeing an increase in the collection and documentation of physical health parameters.27 However, there is still a lot of room for improvement, as shown in studies at an international level,28,29 which concluded that monitoring continues to be low. Furthermore, it was observed that the younger the patient, the more the risk there is that monitoring is not carried out.
Several questions arise: How can improvement be achieved, not only in monitoring, but also in the focus on adequate treatment for patients’ physical pathologies? Are we, as mental health professionals, truly conscious of its importance? Could monitoring affect the interventions oriented towards optimal mental health or the therapeutic relationship with fragile patients with projective or paranoid tendencies? Should specialised mental health care or primary health care take responsibility in monitoring physical health?
It is a fact that clients of mental health centres attend fewer consultations compared to patients of other medical specialisations.30,31 Along with missed appointments,31 other predictive variables include: younger age, little insight, low adherence to treatment, substance abuse and forgetfulness. These variables may be present in a large proportion of patients experiencing their first psychotic episode. Furthermore, it is less probable that young patients (between 25 and 44 years old) maintain regular appointments with their primary health care doctors.32 Consequently, important actions that can help to provide better quality care, which translates to better overall health for the patient are: measures focused on improving adherence in these patients and their active participation in their care plan, programmes specifically centred on these patients’ needs, as well as improvement in the degree of coordination and communication between primary and specialised health care.
Ethical disclosuresRight to privacy and informed consentThe authors declare that they have obtained informed consent from the patients and/or subjects mentioned in the article. This document is in the custody of the corresponding author.
Data confidentialityThe authors declare that they have followed the protocols of their work centre regarding the publication of patient data and that all patients included in the study received sufficient information and gave their informed consent in writing to participate in said study.
Protection of humans and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Martín Otaño L, et al. Tras 6 meses de tratamiento antipsicótico: ¿mejoría de la salud mental a costa de la salud física? Rev Psiquiatr Salud Ment (Barc.). 2013;6:26–32.