The Borderline Intellectual Functioning (BIF) is conceptualised as the frontier that delimits “normal” intellectual functioning from intellectual disability (IQ 71–85). In spite of its magnitude, its prevalence cannot be quantified and its diagnosis has not yet been defined.
ObjectivesTo elaborate a conceptual framework and to establish consensus guidelines.
MethodA mixed qualitative methodology, including frame analysis and nominal groups techniques, was used. The literature was extensively reviewed in evidence based medical databases, scientific publications, and the grey literature. This information was studied and a framing document was prepared.
ResultsScientific publications covering BIF are scarce. The term that yields a bigger number of results is “Borderline Intelligence”. The Working Group detected a number of areas in which consensus was needed and wrote a consensus document covering the conclusions of the experts and the framing document.
ConclusionsIt is a priority to reach an international consensus about the BIF construct and its operative criteria, as well as to develop specific tools for screening and diagnosis. It is also necessary to define criteria that enable its incidence and prevalence. To know what interventions are the most efficient, and what are the needs of this population, is vital to implement an integral model of care centred on the individual.
El funcionamiento intelectual límite (FIL) se conceptualiza actualmente como la barrera que separa el funcionamiento intelectual «normal» de la discapacidad intelectual (CI 71-85). A pesar de su magnitud, su prevalencia no puede ser cuantificada y no se ha operativizado su diagnóstico.
ObjetivosElaborar un marco conceptual para el FIL y establecer directrices de consenso que permitan la aplicación de una atención integral centrada en la persona.
MetodologíaSe utilizó una metodología mixta cualitativa que combinaba un análisis del marco conceptual con el desarrollo de grupos nominales. Se realizó una revisión bibliográfica extensiva en bases de datos de evidencia médica, publicaciones científicas y literatura gris. Se estudió la información encontrada y se redactó un documento de marco conceptual sobre el FIL.
ResultadosLas publicaciones centradas en el colectivo de personas con FIL son escasas. El término que mayor número de publicaciones arrojó fue «Borderline Intelligence». Se detectaron una serie de temas sobre los que era necesario alcanzar un consenso y se redactó un documento con las conclusiones del grupo de trabajo.
ConclusionesEs necesario establecer un consenso a nivel internacional sobre el constructo del FIL y sus criterios operativos, y desarrollar instrumentos específicos de detección y diagnóstico. También es necesario elaborar criterios que permitan calcular su incidencia y prevalencia. Saber qué intervenciones son las más adecuadas y cuáles son las necesidades de atención que presenta este colectivo es de vital importancia para implementar un modelo de atención integral centrado en la persona.
“Borderline Intellectual Functioning” (BIF) is an extremely complex clinical entity, which has barely been studied. In fact, there is not even a minimum consensus in the scientific community on what we mean when we speak of BIF and on its relationship to other developmental disorders.1,2 This lack of taxonomic framework should be considered in the current debate over “mental retardation” or “intellectual disability” (ID), where there are 2 apparently contradictory positions represented by the World Psychiatric Association (WPA) and the American Association on Intellectual and Developmental Disabilities (AAIDD).3 The WPA considers that ID is a meta-syndrome analogous to the concept of dementia in the context of neurodevelopmental disorders that should continue to be coded in the International Classification of Diseases (ICD)4; however, the AAIDD and many national and international bodies consider that this entity is a disability and should consequently be coded in the International Classification of Functioning (ICF) instead of in the ICD.5 This is a leading-edge issue, given the coming revision of the ICD (ICD-11) and of the United States Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
The problems of taxonomy and terminology are even greater in the case of BIF than in other clinical conditions. In the bibliography in English terms such as “Borderline Intellectual Functioning”, “Subaverage Intellectual Functioning”, “Borderline Mental Retardation”, “Borderline Intellectual Capacity” and/or “Borderline Learning Disability” have been used more or less indiscriminately. This lack of terminological definition stems from the fact that these days BIF is not included as a diagnostic code in the DSM-IV-TR, the ICD-10 or the ICF.6–8 In the DSM-IV-TR, Borderline Intellectual Capacity” is mentioned in passing as an intellectual quotient (IQ) range between 1 and 2 standard deviations below average (70–84), but it is uncoded in this system and is compared to the residual ICD system diagnostic code R41.8 (ICD-10). However, code R41.8 actually refers to “other symptoms and signs that imply cognitive functions and ‘apperception’ or becoming aware”, a totally non-specific code that covers aspects as different as awareness of disease and intelligence.
The lack of terminological consensus and its absence in the main diagnostic classifications make it especially difficult to calculate the prevalence of BIF among the general population. If we consider the normal IQ distribution, this population group should represent at least 13.6% of the total; in fact, different studies9,10 place the problem in a range lying between 12% and 18% of the population. In this sense, the data from the Spanish survey on disability, personal autonomy and situations of dependence (EDAD-2008 in Spanish) are discouraging.11 This survey improved the information obtained in the previous survey (EDDES, 1999),12 because it separated the information corresponding to BIF and mild ID, which had been appeared accumulated together in the previous survey. However, the EDAD-2009 survey simply confirmed the lack of visibility and assessment for this collective. That survey indicated that there were 11,600 individuals with BIF. The impossibility of that fact becomes evident if you analyse the figures for mild ID (24,700), moderate ID (52,800), and severe and profound ID (47,000). From a Gaussian perspective of intelligence, these figures would clearly be erroneous, given that there could not be more individuals with severe and profound ID than with mild ID; at the same time, the figures would be an example of the lack of rigour that often characterises the collection of information on ID and BIF.
Consequently, BIF turns out to be an invisible clinical entity. Despite its magnitude, its prevalence cannot be quantified, its diagnosis has not been implemented (so it does not appear in current diagnostic systems) and there are no eligibility criteria to ensure explicit access to social or health services, protections and benefits when they are needed. In the same way as patients having mild ID, individuals with BIF represent a significant percentage of the population and require a considerable amount of support and attention at different moments in their lives.5 However, the scientific literature ignores this population, just as the specialised services for ID and the services for developmental disorders do.13,14
To progress in developing an international consensus in this field, the Catalan association Nabiu (ACNabiu) initiated the CONFIL project in 2007. This project brought together a set of professionals from different areas with the following goals: (1) provide the field of BIF knowledge with a conceptual framework within the group of lifelong developmental problems, and from a perspective of comprehensive attention centred on the individual; and (2) establish guidelines of consensus on BIF in Catalonia. The result was the development of a conceptual reference framework on this health condition that would permit later creation of research in this field and the development of a framework for comprehensive attention for BIF (public health, educational, work and legal). In this article, we present the process of consensus and summarise the conclusions reached in the health area by the CONFIL group. The complete documentation can be consulted in the following link: http://tinyurl.com/5vvx4v9.
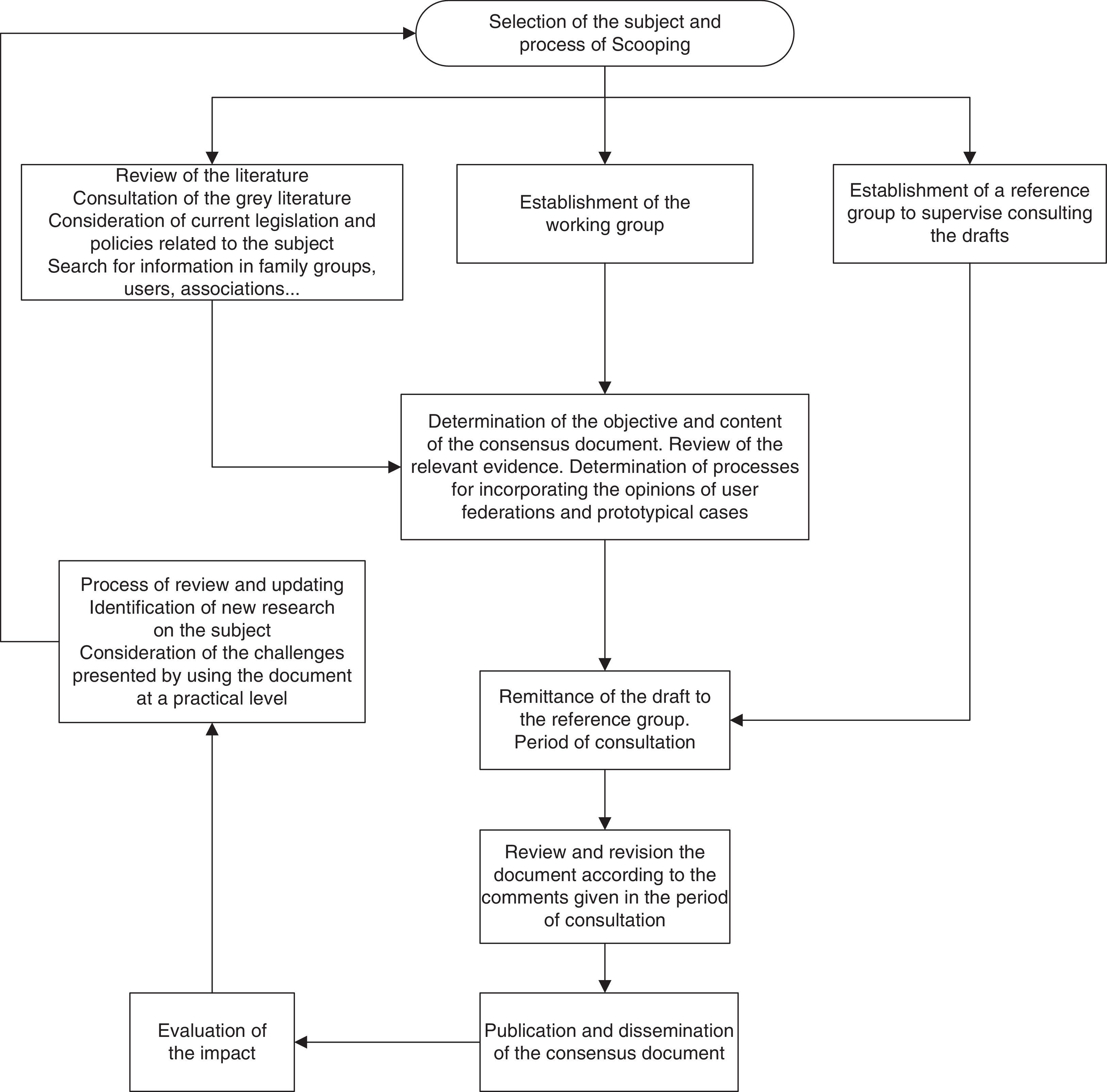
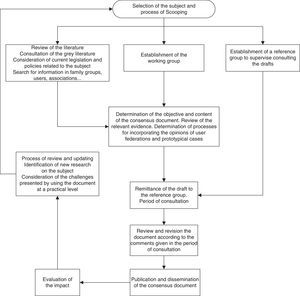
MethodologyTo build the framework for the base of BIF knowledge, an approximation derived from the frame analysis generally employed in social research has been used.15 The usage of conceptual frame analysis methods along with the processes of consensus is especially useful for studying and forming new diagnostic concepts.16,17 In this case, we decided to use this methodology because there had been no prior attempts to implement and classify this health construct. The process that we followed can be seen in Fig. 1.
Step 1 (conceptual framework)To manage an insufficiently-defined health construct (BIF) that, in addition, is related to a poorly categorised attention system (intellectual development disorders), it was necessary to study the current conceptual framework to know the context, terminology and content.
First of all, the scientific literature on BIF was systematically reviewed on Medline, PsycIinfo, TRIPdatabase, along with a manual review of the 10 leading journals in the area of psychology and social sciences in IN-RECS between 1996 and 20 [stet] (later updated in 2011). The following entries were used for the review: “Borderline Intellectual Functioning”, “Subaverage Intellectual Functioning”, “Borderline Mental Retardation”, “Borderline Intellectual Capacity”, “Borderline IQ” and “Borderline Learning Disability”. Likewise, the current legislation and policies related to the subject were reviewed, including the information provided by family groups, users and associations. Finally, a conceptual framework document was written, in which all the relevant bibliography and the sources from it came were included.
Step 2 (working group-nominal panel)A nominal group consisting of 6 members and a rapporteur was formed. The panel functioned following an adaptation of the application of this health methodology18 that turned out to be very useful in attempts to reach consensuses on extremely complex issues in which the information was incomplete. This group reviewed the conceptual framework document and prepared a list of key subjects in each of the BIF spheres in which it was considered necessary to evaluate the evidence and reach a consensus.
Correspondingly, a group of 6 experts was set up. This group performed a critical review of the first draft consensus document and of the successive drafts and participated in writing the final consensus document.
The final consensus group consisted of psychiatrists, psychologists, educators, notaries and members of the Catalan association ACNabiu. All the members of the consensus group were professionals who had prior experience in the treatment, attention or work with individuals that had BIF.
Step 3 (preparation of the consensus document)Three work meetings were held in which the members of the nominal group participated. In the first meeting, the objectives and the content of the consensus document were established and the key topics were decided. The draft was sent to the group of experts and a consultation period of 2 months was established. In this period, the document was reviewed and modified according to the comments given by the group of experts. Once the period of consultation was over, the final document was published and its content was disseminated. Finally, the impact of the publication was evaluated.
ResultsReview of the literaturePublications that focus on BIF are rare. The terms that yielded the greatest number of results were “Borderline Intelligence”, “Borderline Intellectual Functioning”, “Borderline IQ” and “Borderline Mental Retardation”. The terms “Borderline Capacity” and “Borderline Learning Disability” produced only 2 results each, while the term “Subaverage Intellectual” yielded only 1. Even so, the great majority of the studies found did not treat BIF directly; and, in many of the cases, the studies only mentioned the relationship between BIF and some of the genetic or metabolic syndromes in passing, or the studies were duplicated in the different searches. Faced with this lack of extensive scientific evidence, most of the conclusions presented in this article were reached by consensus. Consequently, they represent the lowest level of evidence possible and their level of recommendation should therefore be taken with caution.
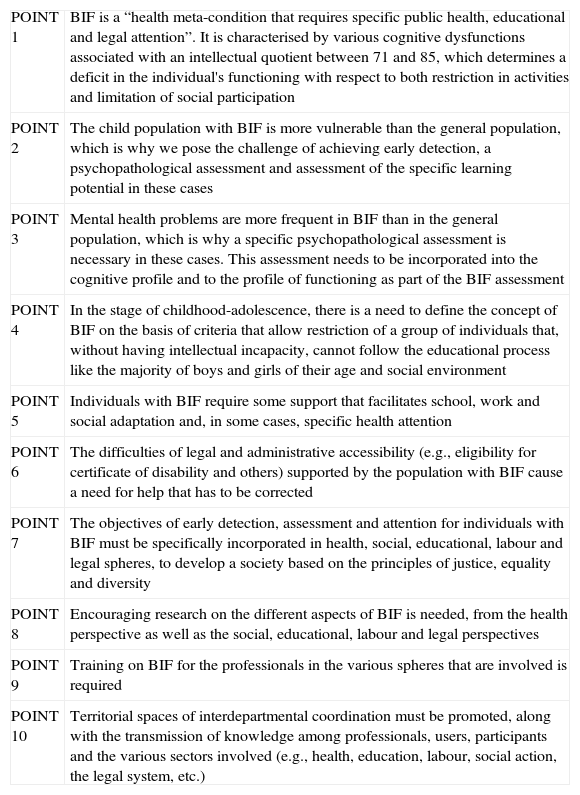
Key topicsIn the conceptual framework document, several key topics on which a consensus was necessary were proposed: Definition and implementation of the concept of BIF; prevalence and diagnostic process; early detection and attention; model for attention and intervention; comorbidity, education and BIF; inclusion and employability; and training and research. The CONFIL 2007 group published a consensus document treating all these topics more extensively19 and agreed to a statement that summarises the main points of the consensus document (Table 1).
Points on the Borderline Intellectual Functioning (BIF) statement prepared by the consensus group.
| POINT 1 | BIF is a “health meta-condition that requires specific public health, educational and legal attention”. It is characterised by various cognitive dysfunctions associated with an intellectual quotient between 71 and 85, which determines a deficit in the individual's functioning with respect to both restriction in activities and limitation of social participation |
| POINT 2 | The child population with BIF is more vulnerable than the general population, which is why we pose the challenge of achieving early detection, a psychopathological assessment and assessment of the specific learning potential in these cases |
| POINT 3 | Mental health problems are more frequent in BIF than in the general population, which is why a specific psychopathological assessment is necessary in these cases. This assessment needs to be incorporated into the cognitive profile and to the profile of functioning as part of the BIF assessment |
| POINT 4 | In the stage of childhood-adolescence, there is a need to define the concept of BIF on the basis of criteria that allow restriction of a group of individuals that, without having intellectual incapacity, cannot follow the educational process like the majority of boys and girls of their age and social environment |
| POINT 5 | Individuals with BIF require some support that facilitates school, work and social adaptation and, in some cases, specific health attention |
| POINT 6 | The difficulties of legal and administrative accessibility (e.g., eligibility for certificate of disability and others) supported by the population with BIF cause a need for help that has to be corrected |
| POINT 7 | The objectives of early detection, assessment and attention for individuals with BIF must be specifically incorporated in health, social, educational, labour and legal spheres, to develop a society based on the principles of justice, equality and diversity |
| POINT 8 | Encouraging research on the different aspects of BIF is needed, from the health perspective as well as the social, educational, labour and legal perspectives |
| POINT 9 | Training on BIF for the professionals in the various spheres that are involved is required |
| POINT 10 | Territorial spaces of interdepartmental coordination must be promoted, along with the transmission of knowledge among professionals, users, participants and the various sectors involved (e.g., health, education, labour, social action, the legal system, etc.) |
The CONFIL 2007 consensus group defined BIF a “health meta-condition that requires specific public health, education and legal attention”. It is characterised by diverse cognitive dysfunctions that are associated with an IQ between 71 and 85, and which determine a deficit in the person's functioning both in the restriction of their activities and in the limitation of their social participation, with the following descriptors:
- 1.
BIF is not a syndrome, nor a disorder, nor a disease. It is a heterogeneous grouping of specific neurodevelopmental syndromes, disorders or diseases and possibly of extreme variations of normality.
- 2.
BIF can be defined as a “health meta-condition that requires specific public health attention”.
- 3.
The cognitive deficits that underlie overall IQ assessment are heterogeneous, so cognitive assessment of the individuals with BIF should not be limited to IQ measurement.
- 4.
Not all the individuals with an IQ between 71 and 85 have limitations in activity and restrictions in participation. Consequently, a specific assessment of capacities and functioning is needed to make a diagnosis of BIF.
In Descriptor “1”, it was decided to incorporate the term “normality” in spite of the conceptual difficulty in applying it to BIF,20 given that we still do not have sufficient evidence to distinguish the cases of BIF clearly related to an alteration in neurodevelopment that require specific attention because of it, from the cases that correspond to variations of normality and do not need such attention. This descriptor requires BIF to be largely associated with neurodevelopmental disorders,1 but the provisional choice was made, faced with a lack of greater level of evidence, to include this denomination in the descriptor and not in the definition.
Descriptor “2” defines the term of “meta-condition”. This is a word derived from the concept of “condition of health”7 and is a significant choice, because it represent the assumption that BIF is not a mere problem of functioning that should be classified in the ICF or not coded at all, it is a set of “conditions of health” that should consequently be classified in the ICD-10.
Descriptor “3” indicates the cognitive deficits of BIF are heterogeneous and can be selective. Consequently, measuring the general intelligence is a necessary but insufficient condition in the neuropsychological assessment of BIF, because specific deficits in language, writing and reading, calculation, visual-spatial abilities and executive functions can alter the individual's functioning at school and work and in social settings.
Descriptor “4” indicates that the presence of an IQ between 1 and 2 standard deviations below the average (71–85) is not a sufficient condition for diagnosis of BIF, given that not all of the individuals in this range have limitations in activities and restrictions on participation.21 Just as in the diagnosis of ID, borderline functioning in the IQ has to be associated with a social, work and academic functioning sufficiently intense to limit the subject's activity and restrict social their participation. Likewise, a deterioration of general functioning does not involve a BIF diagnosis unless it is associated with an IQ between 71 and 85. The selection of the range 71–85 lies above the ID threshold adopted by the WHO (IQ: 69). The consensus group preferred to choose the cut-off point indicated in the DSM-IV-TR. The adverb “generally” was incorporated into the definition to refer to the IQ range until we have greater evidence and/or international consensus.
Prevalence and diagnostic process of Borderline Intellectual FunctioningAs we have previously commented, this is a frequent health condition that, nonetheless, has barely been the object of attention for the public health system. If we look exclusively at the normal distribution of IQ, this population group would represent 13.6% of the total11; other estimates place the problem in a range between 12% and 18% of the population.19 If we take as a reference the school population with problems of academic performance associated with this IQ range, and we bear in mind a possible improvement with age if part of this group adapts to poorly qualified work environments in adulthood, it can be estimated that the population affected would be around 7%. From a conservative perspective, the consensus group estimated that the population in this IQ range could be around 3% of the population, or some 1,350,000 people in Spain. If we evaluate only the group of individuals with a clear need for public health attention in this group, the “floor” would be placed at 1%, or 450,000 people. Even the most conservative estimates indicate that BIF is a hidden problem that has to be put in the focus of public attention.
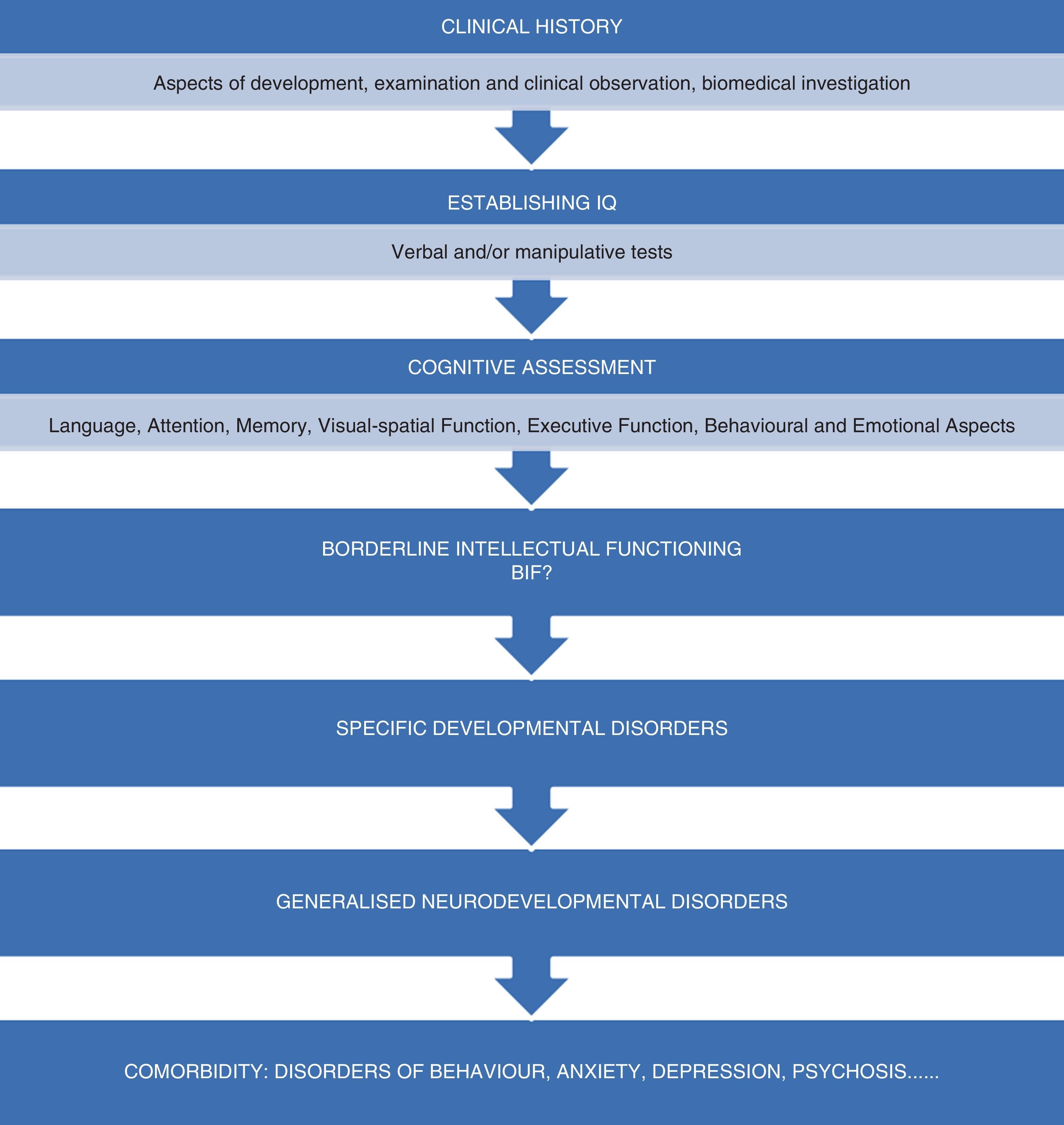
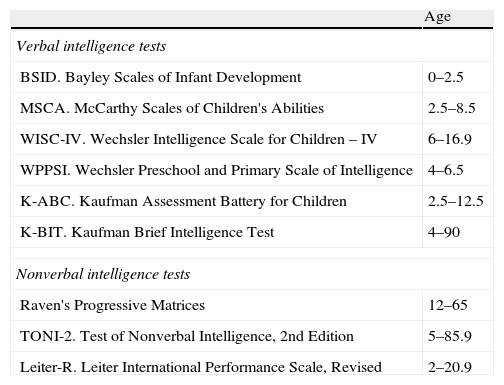
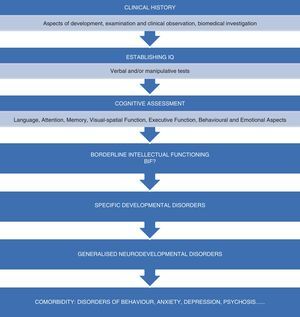
In Fig. 2, you can see the diagnostic process proposed by the CONFIL 2007 consensus group illustrated. As in any other assessment, using a complete clinical history is recommended, focusing especially in developmental aspects, a detailed clinical examination and observation and the pertinent biomedical investigations. Secondly, and although it is not the only or the most important consideration, IQ needs to be established by administering both verbal and non-verbal intelligence tests (Table 2). This assessment of the intelligence level for the individual with BIF needs to be complemented by a complete cognitive assessment of various cognitive functions that will make it possible to obtain information as to the subject's weak and strong points. It has recently been proposed that, given the heterogeneity and multi-causation of BIF, an important number of subject probably have altered executive functions,2 understanding these functions as the group of abilities needed to organise, plan and direct our behaviour towards some objective flexibly and efficiently.22 Consequently, we are going to find alterations in capacities for: generating behaviours with a purpose, solving problems in a planned and strategic manner, paying attention to different aspects of a problem simultaneously, guide attention with flexibility, inhibit spontaneous tendencies that lead to error, retaining in working memory the information required for an action, and capturing what is essential in a complex situation.
Tests proposed by the CONFIL 2007 consensus group for assessing intellectual quotient according to the age range in which they are applicable.
| Age | |
| Verbal intelligence tests | |
| BSID. Bayley Scales of Infant Development | 0–2.5 |
| MSCA. McCarthy Scales of Children's Abilities | 2.5–8.5 |
| WISC-IV. Wechsler Intelligence Scale for Children – IV | 6–16.9 |
| WPPSI. Wechsler Preschool and Primary Scale of Intelligence | 4–6.5 |
| K-ABC. Kaufman Assessment Battery for Children | 2.5–12.5 |
| K-BIT. Kaufman Brief Intelligence Test | 4–90 |
| Nonverbal intelligence tests | |
| Raven's Progressive Matrices | 12–65 |
| TONI-2. Test of Nonverbal Intelligence, 2nd Edition | 5–85.9 |
| Leiter-R. Leiter International Performance Scale, Revised | 2–20.9 |
Next, assessing the presence of a typable neurodevelopmental disorder (TNDD) is recommended. All the TNDDs have in common the fact that a cognitive dysfunction underlies them that gives rise to symptoms with a certain degree of specificity; in addition, BIF is frequently associated with various TNDDs.1
Finally, and given the high psychiatric comorbidity found in BIF, assessing the presence of behaviour, anxiety, affective and psychotic disorders is recommended.
The challenges of early detection and attentionThe possibility of carrying out early detection in cases of BIF and being able to implement the appropriate interventions as soon as possible is impossible during early childhood. This is because neither the knowledge nor the tools required to do so have been available to date. However, the challenge of early detection for BIF cases should be of great importance, for several reasons. The suspicion of the condition in the first years of life would allow us to reduce the barriers to access to services and, consequently, to implement interventions whose objective was to prevent negative evolution of the case (such as, for example, early stimulation programmes). There is evidence that interactions with the environment in the first developmental stages directly influence brain development.23,24 This implies that early interventions could have the potential to modify developmental patterns, improve educational performance and obtain improvements in social functioning. Early interventions have been shown to be effective during the first stages of disorders such as autism,25 Down syndrome,26 children with disabilities in general or at risk of suffering from disability,27 and in attention to premature infants.28 Providing support resources early on can prevent situation of academic failure that could lead to disorders of an emotional type or behaviour disorders.
However, early detection represents today a challenge, given that there are no visible features to identify a child with BIF, nor are there discriminating behavioural phenotypes. The CONFIL 2007 group feels that developing diagnostic and screening batteries for BIF and developing specific training programmes for professionals is an urgent need. However, at present it is difficult to imagine diagnostic and screening batteries for BIF different from the developmental batteries used to diagnosis overall developmental delay, a concept that is used for ages below 5–6 years. It would therefore be necessary to use the existing batteries systematically in situations in which there is a suspicion of BIF. These batteries could be complemented with more specific neuropsychological examinations and with measures focused on behavioural abilities. In short, and despite the difficulties, early detection should be specifically incorporated in health, social and school spheres, to make it possible to ensure that these individuals are integrated in society according to principles of justice, equality and diversity.
Model for attention and interventionThe CONFIL 2007 consensus group backs the creation of territorial spaces for interdepartmental coordination among different sectors of the administration to ensure the transmission of knowledge among professionals, users and the various sectors involved (e.g., health, education, work, social action, legal system, etc.). Diagnostic suspicion of BIF cases can stem from paediatricians and paediatric nursing staff in primary care, from professionals in kindergartens and schools, and from the parents themselves. Once the suspected diagnosis is established, the child should be referred to specialised services offered by mental health attention for children, which will in turn be connected for developmental pathologies with the neuropaediatric services and early attention services.
The intervention requires collaboration among the different professionals and services from the first moment and a fluid contact among the health services and the social and educational resources. Later on, in adulthood, participation will be needed by the work and living arrangement spheres and, sometimes, the legal system. The interventions should not be distinguishable from those used for developmental disorders and they should be directed aimed at BIF. They should include, among others: programmes with the mediation of the parents, interventions of communication support, psychotherapeutic interventions when behavioural or emotional disorders are present, curriculum adaptation in the educational process, programmes for access to the work world and community residential programmes. The possibility of applying pharmacological interventions should be assessed when there are comorbid disorders such as affective, anxiety, hyperactivity, insomnia disorders, etc. In situations of comorbidity, an effort must be made so that these individuals can receive psychotherapeutic attention,29,30 given that different studies have shown that they are more or less often treated with psychiatric drugs (including antipsychotics) without an appropriate prior case history and diagnosis, with the possibility of presenting adverse effects, some of which are more frequent in this population than in general populations (for example, greater extrapyramidal side effects).31
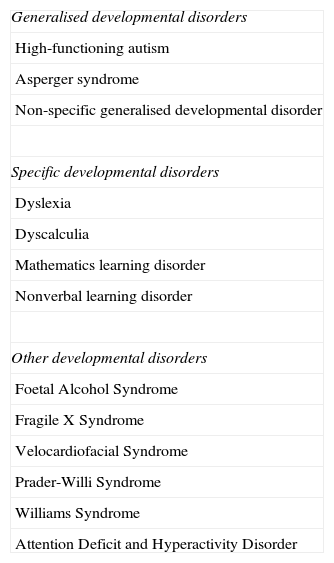
ComorbidityThe disorders most frequently related with BIF are set out in Table 3.
Neurodevelopmental disorders most commonly associated with Borderline Intellectual Functioning.
| Generalised developmental disorders |
| High-functioning autism |
| Asperger syndrome |
| Non-specific generalised developmental disorder |
| Specific developmental disorders |
| Dyslexia |
| Dyscalculia |
| Mathematics learning disorder |
| Nonverbal learning disorder |
| Other developmental disorders |
| Foetal Alcohol Syndrome |
| Fragile X Syndrome |
| Velocardiofacial Syndrome |
| Prader-Willi Syndrome |
| Williams Syndrome |
| Attention Deficit and Hyperactivity Disorder |
As for psychiatric comorbidity, a study30 consisting of a population survey of more than 8000 adults, among which there was a percentage of 12% of BIF, showed that these individuals have more emotional, substance use, personality, adaptation and social problems than the study individuals without BIF. In addition, the BIF population received more drug treatments and made higher use of medical services than the general population. This same pattern is repeated in the child population; a very recent study32 concluded that children with BIF contributed disproportionately to the prevalence of mental disorders in the general child population.
In contrast to the groups with moderate or severe ID, the distribution of psychopathology that appears in BIF is similar to that of the general population general and we find greater frequency of anxiety and behavioural disorders.33,34
The fact that some of the mental disorders appear concurrently with a borderline intelligence range is of great importance in the prognosis. This is because it adds a further feature of severity to the evolution. This has been specifically documented for a population with schizophrenia in a study35 that compared adults with schizophrenia and BIF against adults with schizophrenia and normal intelligence; the study showed that the first group had worse quality of life, more severe psychotic symptoms and worse general functioning.
Children and adolescents with BIF are thus a population at risk, vulnerable, of growing accumulating different developmental mental and social problems. In a study34 that followed adolescents with BIF, it was found that the factors most related with evolution in terms of psychopathology were (in addition to difficulties in social competency) the deficit in daily life abilities, health problems and negative adverse events.
Behavioural disorders appear in 30% of the children with mild BIF or ID. The clear relationship that exists between low verbal intellectual abilities and antisocial behaviour is highly influenced by socio-cultural deprivation.36 There is also a very clear relationship, one that is very difficult to separate, of the influence of low-normal intelligence, low scholastic performance and abandoning school at early ages on later criminal behaviour. This relationship is mediated to a good degree by the presence of hyperactivity.37
Individuals with persistent behavioural disorders, which began early, have an average of 8–12 IQ points below that of the average general population. The presence of problems in the parents, which affect their educational capabilities, together with other risk factors, has an interactive, potentiating effect on the appearance of behavioural problems. In a longitudinal study38 carried out in London, 400 children were followed from 8 to 40 years old; low performance in secondary school and low non-verbal IQ were found to be the main factors of risk for the development of later antisocial behaviour.
There seem to be some gender differences with respect to the relationship between intelligence and behaviour problems. In a general population, a negative relationship between intelligence and behaviour problems was found in boys; however, this relationship was positive in girls, and the higher the intelligence, the greater the behaviour problems they presented.39 These differences were also seen in the case of specific reading disorders, which appeared directly associated with behaviour problems in girls but it seemed that, in boys, the association was mediated by student absenteeism.38
Psychopathology in the parents, having single parents, stressful events and other individual factors such as temperament or the existence of associated hyperactivity have an exponential effect in combination with low intelligence. The effect of various associated risk factors on intelligence is usually greater than the simple sum of the effect of the individual factors. That is to say, the possible effect on intelligence that parental psychopathology combined with single parenthood could have is considerably greater than the sum of the effect of these 2 factors separately.34
Education and Borderline Intellectual FunctioningUnder the label BIF, you can find students with totally different trajectories, having their low scholastic performance in common40: problems with reading, writing or calculation, due to a low level of understanding, poor verbal fluency, difficulties in the reasoning and symbolisation processes, poor attention and concentration, or lack of self-esteem and personal initiative. These characteristics, along with the lack of a clear diagnosis and of early detection, lead to many students who fall into “academic failure” being in reality individuals with undetected BIF.
The majority of these students are not detected to be individuals with BIF until they begin to attend school; they can even reach the end of primary school, when they are 12 years old, without being diagnosed because their apparent normality makes the problem difficult to detect. With the arrival of adolescence, the distances with their classmates in the acquisition of academic competencies increase notably, and imbalances in their behaviour can arise. These individuals can begin to feel rejected socially because of their inadaptation to free time, to affective relationships, to work or to independent living. The absence of a diagnosis deprives them of possible rights and help to make it possible to face a difficult present and a dark future weighed down with rather problematic prognoses.41 However, it is also true that, with the necessary support, especially from classmates, their development can follow more normal pathways. It is important for individuals with BIF attending school to be kept in ordinary educational centres, given that various studies42 have shown that the individuals achieve better academic performance and greater social competence if this happens.
The CONFIL 2007 consensus group prepared a series of recommendation that they hope will be useful to improve the current educational attention for individuals with BIF: (1) systematic collaboration among professionals in the Departments of Education and Health; (2) greater attention to the collective with intellectual limitations at the moments of transition between life stages; (3) creation of educational protocols adapted for attention to students with behavioural disorders; (4) preparation of an individualised educational plan; (5) presence of a specific tutor in each educational stage; and (6) destruction of the myths surrounding the IQ figure as the single, exclusive parameter for diagnosing BIF, along the same lines in that IQ in and of itself is not enough for ID diagnosis.
Inclusion, employability and Borderline Intellectual FunctioningThe end of the school stage represents a new challenge for the individual with BIF to face. Access to the work world takes longer for these people and, if they manage to enter it, they will do so having to face all the difficulties that we have described up to this point. Employment is a determining factor for improving the quality of life of individuals with BIF. On the one hand, these individuals do not receive social aid, given that they are recognised as apt for work, but on the other hand, they have a series of difficulties and limitations in their functioning that makes access to the labour market difficult. In fact, BIF is not conceptualised in workers’ statutes, so going from exclusion to inclusion is extremely hard. Consequently, the generalised acknowledgement that employment is the key to social insertion in the current society43 acquires a special meaning in the population of individuals with BIF.To be able to carry out a complete, reliable assessment of the level of employability of the individuals with BIF, one should bear in mind the complete personal history, the IQ, the use of validated instruments for measuring adaptive capacities, the collection of information from people in the individual's surroundings and the assessment of the environment. The following instruments can be useful to assess individuals’ adaptive capacities: Checklist of Adaptive Living Skills, Adaptive Living Skills Curriculum and Inventory of Client and Agency Planning.44–46
Lastly, if the political powers would design and implement appropriate policies, this could eliminate the obstacles that prevent the integration of individuals with BIF into work and social environments. It would also favour the normalisation of the general social status of individuals with BIF.
Training and researchTraining the professionals responsible for attending individuals with BIF is an especially relevant topic. As we mentioned in the introduction, BIF has been shown to be an unseen condition; these people simply do not exist in a great many areas and services for attention, whether health, social or educational. There is a need for a great labour of dissemination and of training for the teaching professionals and for the psycho-social assessment, so that the school can be converted into a space where children and adolescents with BIF are detected and the support programmes needed can be applied. The same is true of paediatricians, nurses and mental health teams, so that these individuals are detected as early as possible and for the attention programmes to be specific and structured.
Research requires a consensus at the international level on the construct of BIF and the establishment of widely-accepted operative criteria. From that point on, it would be possible to work on developing specific instruments for detection and diagnosis, and on the establishment of criteria that would make it possible to calculate the incidence and prevalence of BIF. We also need answers as to which interventions are most appropriate and effective in the attention to individuals with BIF. We have to know what the needs for attention that these individuals present are, and whether they can be seen in already-existing services with effectiveness, just as has been occurring up until now. Lastly, basic and genetic research could clarify part of the etiological factors associated with this condition, while cost studies could show the true magnitude and repercussion of this problem in society.
Borderline Intellectual Functioning in the context of a system of comprehensive attentionConsidering all of the above, the CONFIL 2007 group proposed a model of comprehensive, holistic attention, seeing to both public health aspects and educational, work and legal-administrative aspects of the individuals with BIF in which any non-included needs exist. The proposed model should consider both negative health aspects (illness and disabilities, risk factors and subjective experience of illness) as well as positive aspects (well-being, recovery, internal and external protection factors, and subjective experience of health and quality of life). It should also consider the assessment throughout the individual's life cycle, with special attention in the critical life transitions (e.g., the steps from childhood to adolescence, from adolescence to adult life, the transition to a job, etc.). Such a model makes it possible to create opportunities in the school and in the community; in addition, in contrast to the classic individual planning, it allows transferring control and responsibility to the individuals themselves.
A system of integrated attention has to include not only the individuals with BIF, but also their families. It must be guaranteed in all geographical areas, promoting the appearance of territorial spaces of interdepartmental coordination. These spaces could encourage coordination, communication, collaboration and knowledge transfer among professionals, users, participants and the various sectors involved (e.g., health, education, labour, social action, the legal system, etc.).
Finally, a model of comprehensive attention for individuals BIF needs to follow the focus on social inclusion in its individual, family and community dimensions. An individual with BIF should be able to have access to their rights and opportunities just like any other citizen, avoiding situations of discrimination and giving rise to policies of equality.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments on human beings or on animals were performed for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis study was funded by theDepartment of Health of the Catalan government (Generalitat de Catalunya) with the approval of the CONFIL 1, 2, 3 and CONFIL 2010 projects, by the Obra Social Caja Madrid and by Asociación Aequitas.
The final version of this work was possible thanks to the POMONA-ESPAÑA project (PI12/01237), funded by the Health Research Fund of Instituto de Salud Carlos III.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Salvador-Carulla L, et al. Funcionamiento intelectual límite: guía de consenso y buenas prácticas. Rev Psiquiatr Salud Ment (Barc.). 2013;6:109–20.
Luis Salvador Carulla is the president of the working group for the Classification of Intellectual Developmental Disorders that reports to the WHO for the Revision of the Classification of Behaviour and Mental Disorders of the ICD-10. The statements of this article correspond to the authors’ point of view and are not the WHO official perspective or policy.