Little is published about the impact of the 2008 economic crisis on mental health services in Spain.
MethodAn interrupted time series analysis was conducted to investigate a potential short-term association between the 2008 economic crisis and the number of psychiatric hospital admissions. The timing of the intervention (April 2008) was based on observed changes in Gross Domestic Product (GDP). Data on 1,152,880 psychiatric inpatients from the national Hospital Morbidity Survey, 69 months before and after the onset of the economic crisis (April 2008), were analyzed.
ResultsAge-adjusted psychiatric (ICD9 290–319) hospital discharge rates significantly increased from April 2008, matching the onset of the crisis, especially for inpatients aged 15–24 years old and to a less extend for inpatients aged 25–34 years old. Other age groups were not affected. There was a significant increase in diagnoses for disturbance of conduct and emotions, depression, neurotic and personality disorders and alcohol and drug disorders; however, diagnoses for mental retardation and organic psychosis for 15–34 years old inpatients were unaffected.
ConclusionsPsychiatric hospital admissions abruptly increased in April 2008, coinciding with the onset of the economic crisis. We identified age groups and diagnoses affected. Increased hospitalizations were found only at the age-ranges most affected by the rise in unemployment. The diagnoses affected were those most sensitive to environmental changes.
Se dispone de escasa literatura científica sobre el impacto de la crisis económica de 2008 en los servicios de salud mental en España.
MétodoSe ha realizado un análisis de serie temporal interrumpido para examinar una posible asociación a corto plazo entre la crisis económica y el número de hospitalizaciones psiquiátricas. El momento de la intervención (abril del 2008) se fijó sobre la base de los cambios observados en el Producto Interior Bruto (PIB). Se analizaron los datos de 1.152.880 hospitalizaciones psiquiátricas proporcionados por la Encuesta Nacional de Morbilidad Hospitalaria, 69 meses antes y después del inicio de la crisis económica (abril del 2008).
ResultadosLas tasas de altas hospitalarias psiquiátricas (ICD9.290-319) ajustadas por edad aumentaron significativamente a partir de abril del 2008, coincidiendo con el inicio de la crisis: las hospitalizaciones aumentaron especialmente en pacientes en el rango de edad 15-24 y en menor medida en el rango de edad 25-34. Los restantes rangos de edad no se vieron afectados. Se observa un aumento significativo en los diagnósticos relativos a la alteración de conducta y emociones, depresión, trastornos neuróticos y de personalidad y trastornos de alcohol y drogas; los diagnósticos relativos al retraso mental y psicosis orgánica no se vieron afectados.
ConclusionesLas hospitalizaciones psiquiátricas aumentaron abruptamente a partir de abril del 2008, coincidiendo con el inicio de la crisis económica. Se han identificado los grupos de edad y diagnósticos afectados. El aumento de las hospitalizaciones se observó solo en los rangos de edad más afectados por el desempleo. Los diagnósticos afectados fueron los más sensibles a los cambios ambientales.
The Spanish economy was greatly affected by the 2008 economic crisis, which resulted in a sudden downward trend in national Gross Domestic Product (GDP)1 and a skyrocketing of the unemployment rate (9.6% vs. 26.94% in the first quarter of 2008 and 2013, respectively).2 All age groups were affected by unemployment, but the youngest age groups were especially harmed. In the first quarter of 2013, unemployment reached high levels in those aged 16–19 years old (men 75.3%, women 76.2%), 20–24 years old (men 55.6%, women 51.0%), 25–29 years old (men 36.0%, women 34.1%) and 30–34 years old (men 27.1%, women 26.4%). Rates were below 25% in higher age ranges for both sexes.2 There was also increased income inequality, number of evictions and numbers of poor people at risk of exclusion in Spain.3,4
Observational studies show an association between economic downturn and poor mental health.5 The economic crisis can increase the incidence of psychiatric pathologies, the consumption of psychiatric drugs and suicides.1,5-10 Spain experienced an increase in suicide rates beginning April 20081 as well as an increase in antipsychotics consumption from 2009.6 Hospitalization rates are reliably registered in most countries because of economic and legal implications. An association between unemployment and psychiatric admissions has been repeatedly corroborated. Economic indicators have been found to correlate with the rate of psychiatric admissions11,12 and readmissions.13-15 The recession could not only affect the incidence and prevalence of mental illness. Austerity measures taken by the government in order to control public deficit, such as cutbacks in financing of community support for severe mental disorders, could also foster the number of psychiatric admissions without any increase in the real incidence of mental disorders.
Undoubtedly, the recession could lead to a large increase in the use of health services and health expenditures. However, it is surprising that there are few studies that analyzed the impact of recession on the use of mental health services.16 The purpose of this study was to investigate the impact of the 2008 economic crisis on the number of psychiatric hospital discharges.
MethodologyWe conducted an interrupted time series analysis to investigate a potential short-term association between the 2008 economic crisis and the number of psychiatric hospital admissions by identifying any change in psychiatric hospitalization trends that occurred during the onset of the economic downturn in Spain. The timing of the intervention (April 2008) was based on observed changes in GDP. Data from the Spanish Hospital Morbidity Survey, 69 months before and after the onset of the economic crisis (April 2008), were analyzed from 1,152,880 inpatients. Data collection and sampling.
We analyzed all psychiatric (International Classification of Diseases-9th Edition Codes 290–319) hospital discharges records (n=1,152,880) from the Hospital Morbidity Survey (HMS) annual cross-sections from 2002 through 2013. The HMS is a national survey conducted by the National Statistics Institute of Spain that contains nationally representative data on hospital discharges. All Spanish hospitals are obliged by law to facilitate the information contained in the HMS. The National Statistics Institute collects the information, reviews the collected information and corrects and validates the data before providing the database to the public. Thus, no missing data was found.
The HMS collects information from the registers of all Spanish hospitals (public and private, general and monographic), including sex, age, and cause of hospitalization at the time of discharge that is coded by the three-digit diagnosis of the International Classification of Diseases-9th Edition (ICD9). The survey provides a number of hospital discharges, including readmissions rather than data on individuals. The demographic series used to calculate hospitalization rates were obtained from the National Statistics Institute of Spain.
Variables and outcomes. Age-range targeted and grouping 106 of pathologies. We analyzed age-adjusted hospitalization rates associated with all psychiatric pathologies; hospitalizations rates associated with all psychiatric pathologies for twelve different age ranges (5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–54, 55–64, 65–74, 75+); and hospitalization rates by diagnosis for a targeted age range. Ten principal outcomes were considered for those age ranges previously identified as affected during the time of the economic crisis:
- 1.
all psychiatric diseases together (ICD9 290–319);
- 2.
organic-psychosis (OP) (ICD9 290, 293–294);
- 3.
functional-psychosis (FP) (ICD9 295–298);
- 4.
neuroses and personality disorders (ICD9 300–302);
- 5.
adjustment reaction and acute reaction to stress (ICD9 308–309);
- 6.
depression (ICD-9, 311);
- 7.
substance-related disorder (ICD9 291–292, 303–304);
- 8.
mental retardation (CIE9, 317–319);
- 9.
childhood and adolescence disturbance of conduct and emotions (CIE9 312–314), which includes disturbance of conduct not elsewhere classified, disturbance of emotions specific to childhood and adolescence and childhood Hyperkinetic syndrome;
- 10.
any other psychiatric pathologies (ICD9 299, 306–7, 310, 315–6), including psychoses with origins specific to childhood (autism spectrum pathologies), physiological malfunction arising from mental factors, special symptoms or syndromes not elsewhere classified, specific non-psychotic mental disorders following organic brain damage, specific delays in development, and psychic factors associated with diseases classified elsewhere.
All psychiatric (ICD9 290–319) hospitalization rates were age and sex adjusted. Monthly psychiatric hospitalization rates were calculated by the direct method according to the Scandinavian (“European”) Standard Population of the World Health Organization.17 Rates were calculated per 10,000 inhabitants.
We conducted an interrupted time series analysis. Interrupted 131 time series analysis are used frequently in this type of studies.1,5,16,18,19 The analysis first objective is to identify patterns in the monthly hospital rates over time by modeling the sequence of observations (monthly hospital rates). The model obtained is a mathematical function that represents the observations over time. The purpose when modeling is to make the model fit the data as well as possible. The model conducted for our analysis is self-regressive (“AR”), integrated (“I)”, moving average (“MA”), called ARIMA (p, d, q) model. ARIMA models are represented by three parameters (p, d, q) where p value is the order of the autoregressive component (number of time lags), d value is the differencing (number of times the data have had past values subtracted) and q values is the order of the moving-average model. The notation for seasonal models is ARIMA (p, d, q)(P, D, Q)c, where P, D and Q refer to the seasonal component parameters of the model and c is the seasonal cycle. The second objective in the analysis is to test and estimate the impact of the intervention event for which interrupted time series analysis were conducted. Interrupted time series analysis is a special kind of time series in which we know the specific point in the series at which an intervention (also called interruption) occurred.
By conducting an interrupted time series analysis, we estimate the effect of an intervention on an outcome variable. The hypothesis is that observations after the intervention will have a different level or slope from those before the intervention. As a result of this analysis it is given an estimated value for the slope change, a confidence interval and a p value. The hypothesis (observations have a different slope after the intervention) is accepted when the p value is less than 0.05 (for a confidential interval 95%). Detailed information on time series analysis and ARIMA models has been published and is available on the Internet.19
Time series (repeated observations over time) is divided 156 into 2 segments. Intervention time-series were used to compare hospitalization rates before and after the economic crisis. The intervention of interest in this study was the so-called 2008 economic crisis. First, the timing of the intervention was established and then time series analysis was conducted for different inpatient age intervals and groups of psychiatric pathologies.
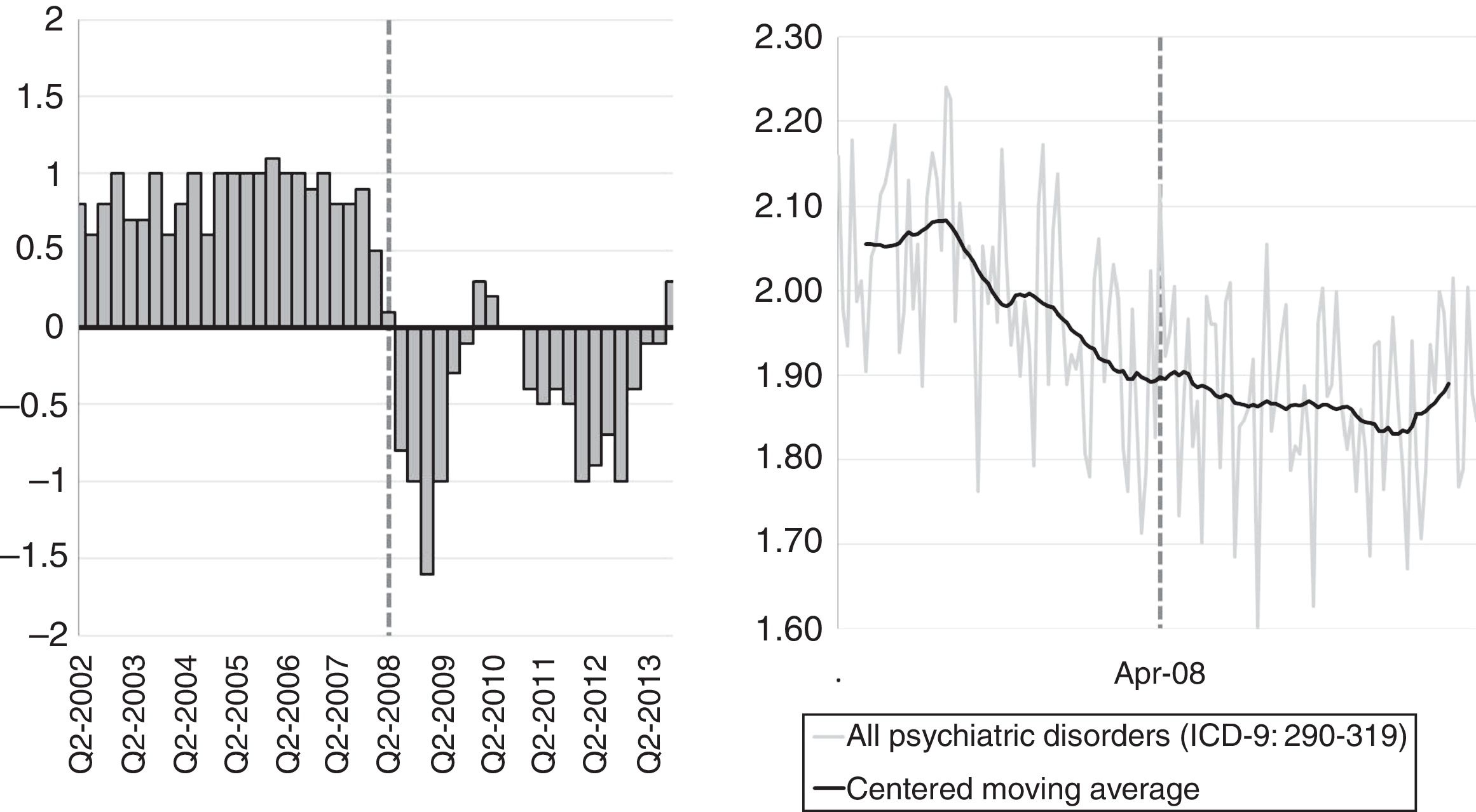
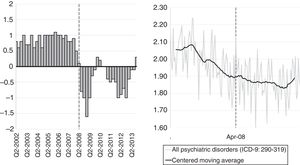
The timing of the intervention was based on registered changes in GDP, which in Spain began to contract starting in the second quarter of 2008.1 Data on GDP (Fig. 1) is available from the Organization for Economic Co-operation and Development (OECD). Timing of the crisis was established at April of 2008, as in a previous study.1
Most recent available hospital data at the time the analysis was started corresponded to year 2013; the post economic crisis period consisted on 69 months (April 2008–December 2013). Thus, the 10-year time series (138 months) consisted of two periods of 69 months, a pre-economic crisis period (July 2002–March 2008) and a post economic crisis period (April 2008–December 2013). SPSS Statistics software (version 23, IBM, Armonk, NY, USA) was used to conduct all analysis.
ResultsWe analyzed population representative data from the Spanish Hospital Morbidity Survey (HMS) for 2002–2013 (n=1,152,880 inpatients). A time series analysis for psychiatric hospital discharge rates was conducted in order to understand the impact of the 2008 economic crisis on national mental health care. We first identified the timing of the intervention based on observed changes in GDP and analyzed the national age-adjusted psychiatric hospital rate (ICD9 290–319) (Fig. 1). Secondly, we analyzed psychiatric hospitalization rates for twelve different age ranges (Figs. 2 and 3) and subsequent hospitalization rates by diagnosis for a targeted age range (Fig. 4).
The quarterly GDP growth and monthly psychiatric hospitalization rate are displayed in Fig. 1. The GDP began to contract in the second quarter of 2008. Thus, April 2008 was established as the beginning of the economic crisis. The decrease in the rate of psychiatric hospitalization in the pre-economic crisis period (July 2002–March 2008) changed during the post-economic crisis period (April 2008–December 2013). The 69-month pre-intervention time series was used to identify a seasonal ARIMA (2 1 0) (1 0 0)12 model. The intervention parameter for the intervention timing (April 2008) was strong and statistically significant; a 13.3% (CI95% 7.8–19.1%; p=0.013) increase was found in the monthly hospitalization rate for all psychiatric conditions, above the trend expected for the 69-month preintervention time series. An additional increase in hospitalizations and psychiatrists during the last two years of time series was found, as displayed in Figs. 1 and 3.
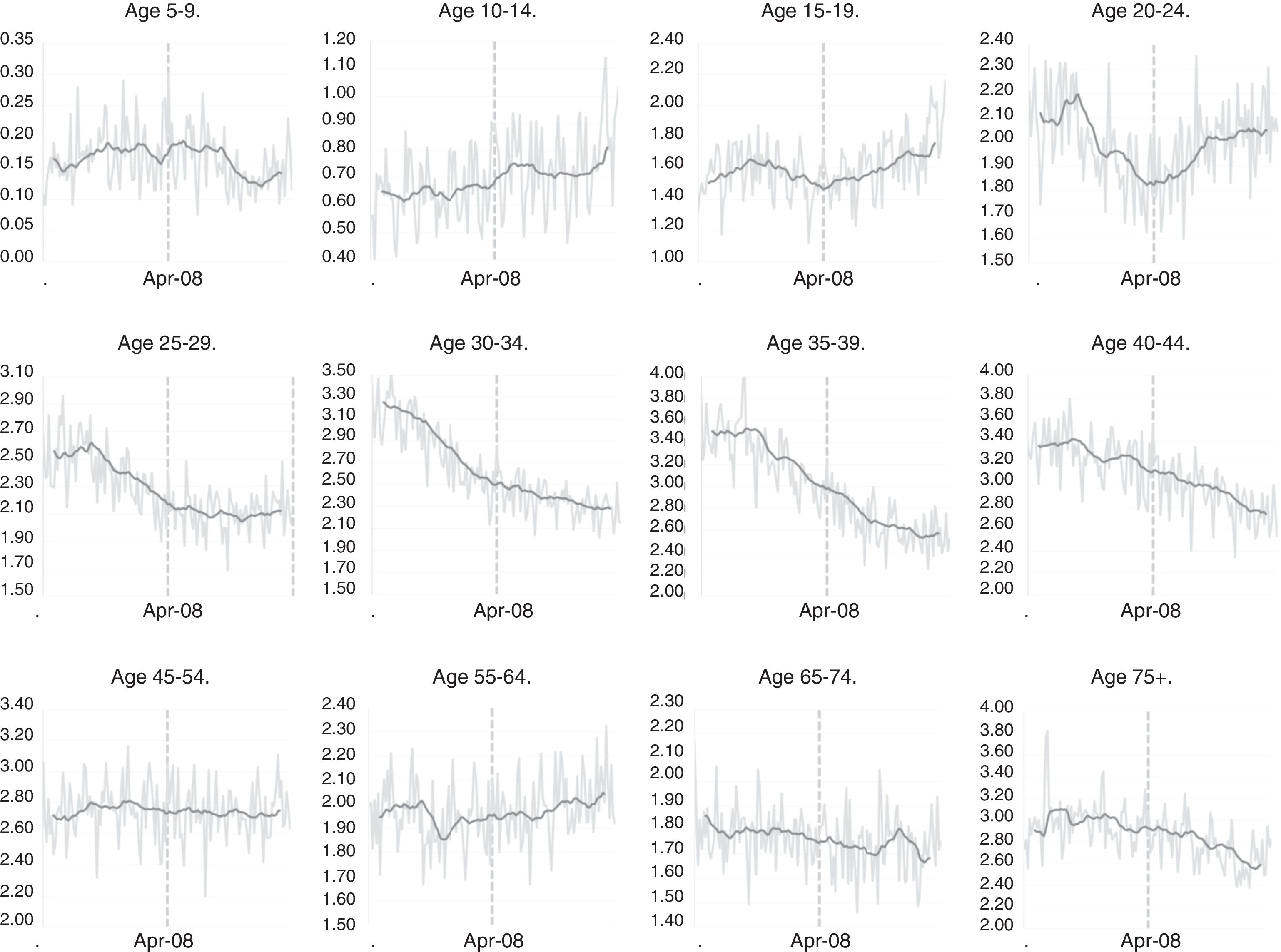
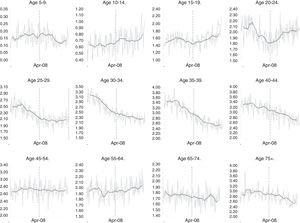
Fig. 2 shows the monthly hospitalization rate for all psychiatric conditions by age range. Four age ranges, 15–19, 20–24, 25–29, and 30–34, showed a change on trend in psychiatric hospitalization rates that correlated with the April 2008 199 economic crisis time-point. The other age groups did not do this.
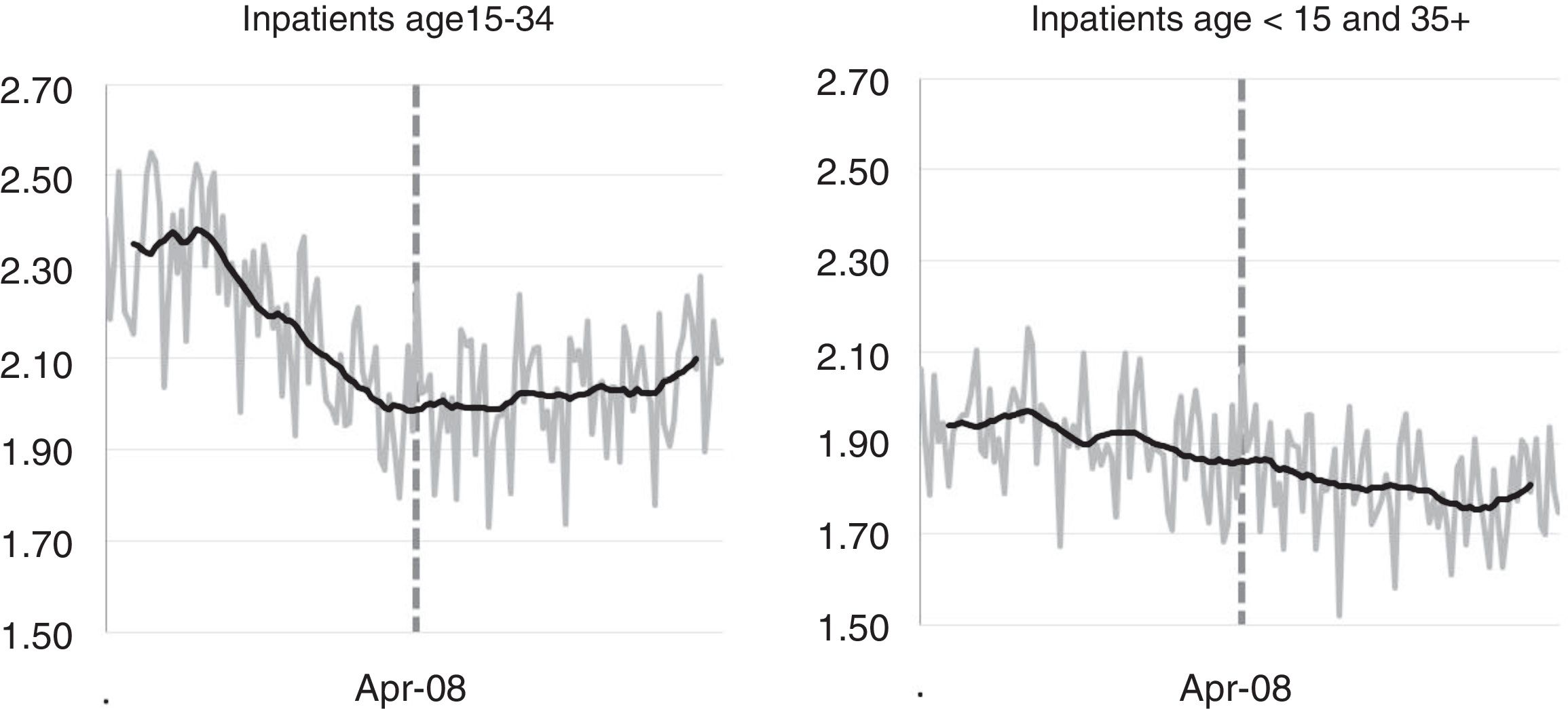
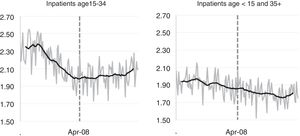
Fig. 3 displayed the monthly psychiatric hospitalization rate for inpatients aged 15–34 years and for those inpatients less that 15-year-old and 35 years old and older.
Psychiatric hospitalization rates for those in the 15–34 year age group stopped declining at the April 2008 time-point and remained steady for the next years. In contrast, there appeared to be a steady decline in the psychiatric hospitalization rate between July 2002 and December 2013 for the other age groups taken together. The 69-month pre-intervention time series was used to identify a seasonal ARIMA (2 1 0) (1 0 0)12 model for the inpatients age 15–34. The intervention parameter was strong and statistically significant for the age range 15–34, suggesting that the Spanish psychiatric hospitalization rate in the age range 15–34 increased by 18.2% (CI95% 9.1–28.0%; p=0.039) per month above the underlying trend found for the pre economic crisis period (July 2002–March 2008).
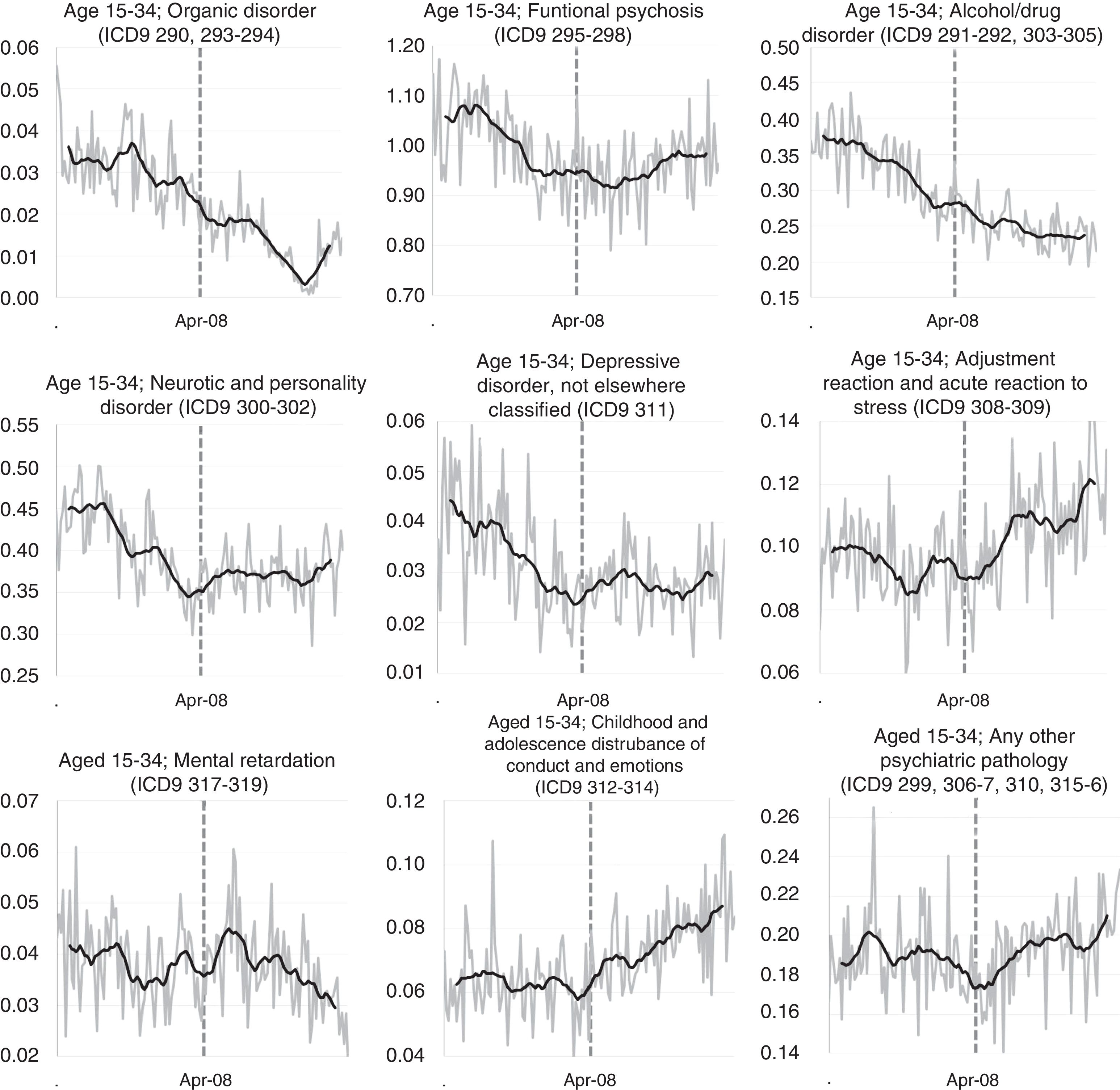
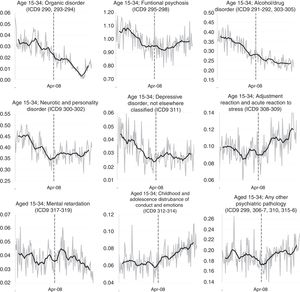
Fig. 4 shows the monthly hospitalization rate by psychiatric diagnosis for inpatients ages 15–34. While organic psychosis and mental retardation hospitalization rates remained stable, hospitalization rates for alcohol/drug disorder, neurotic and personality disorders, depression, and childhood and adolescence disturbance of conduct and emotions abruptly changed in April 2008. Functional psychosis as well as adjustment reaction and acute reaction to stress changed during the next few months. A seasonal ARIMA (0 1 1) (1 1 0)12 model was identified for neurotic and depressive personality disorders for the 69-month pre-intervention time series. In addition, a seasonal ARIMA (0 1 1) (1 0 0)12 model for alcohol/drug disorder and childhood and adolescence disturbance of conduct and emotions was found. The intervention parameter was strong and statistically significant for the above four diagnosis groups. The intervention parameter suggested an increase of 51.6% (CI95% 24.2–85.1; p=0.039) per month for depression and an increase of 46.1% (CI95% 24.7–71.2; p=0.018) for hospitalizations caused by childhood and adolescence disturbance of conduct and emotion for those aged 15–34 years.
Neurotic and personality disorders increased by 26.6% (CI95% 14.2–40.3; p=0.024) and alcohol/drug disorder increased by 26.2% (CI95% 13.6–40.3; p=0.029) per month from the onset of the economic-crisis.
A seasonal ARIMA (0 1 1) (1 0 0)12 model for functional psychosis and a seasonal ARIMA (0 1 1) (1 1 0)12 model for adjustment reaction and acute reaction to stress, and for any other psychiatric pathology, were identified. The intervention parameter for April 2008 was not statistical significant for inpatients 15–34 years old for functional psychosis; adjustment reaction and acute reaction to stress, and any other psychiatric pathology (ICD9 299, 306–7, 310, 315–6). However, the value of the rate gradually increased over time some months after the onset of the crisis for those hospitalizations related to adjusted/acute reaction to stress and functional psychosis (Fig. 4), as well as in the category of pathologies not included in the main diagnosis-related groups (ICD9 299, 306–7, 310, 315–6).
DiscussionTo understand the impact of the 2008 economic crisis on national mental health, a time series analysis for age-adjusted psychiatric hospital discharge rates was conducted based on data from the Spanish Hospital Morbidity Survey (HMS) from 1,152,880 inpatients (2002–2013). The timing of the intervention (April 2008) was based on observed changes in GDP.
The study produced three main findings. First, psychiatric hospitalizations abruptly increased in 2008 above the underlying previous trend. Second, the increase in the hospitalization rate was limited to ages 15–34. Third, hospitalizations associated with organic psychosis and mental retardation did not change the underlying previous trend in inpatients age 15–34; however, interrupted time series analysis proved an abrupt increase on inpatients age 15–34 for the following diagnoses: alcohol/drug related disorders, depression, disturbance of conduct and emotions, and neurotic and personality disorders. The rate value gradually increased some months after the onset of the crisis for those hospitalizations associated with adjusted/acute reaction to stress, functional psychosis and all other diagnoses not included in the above categories.
The GDP started to drop in the second quarter of 2008 and continued to do so in the following quarters, thus the intervention timing was established as April 2008. This time frame is consistent with previous studies that related the economic downturn in Spain with an increase in suicides from April 2008 by using intervention time series analysis.1 The onset time for the increase in psychiatric hospitalizations for all ages as well as for ages 15–34 perfectly match in time with the drop in GDP. The interrupted time series analysis unequivocally proved an abrupt increase on inpatients from April 2008 and strongly suggest a relationship between the economic downturn and the increased psychiatric hospitalizations. Determining whether there was a parallel increase in the national demand for psychiatric outpatient 266 services would be advisable. Unfortunately, a study on psychiatric outpatient services is not feasible given the very limited data availability on outpatient care in Spain. The “Statistics of Health Centers of Specialized Care” (SHCSC), a national register conducted by the Spanish Health Ministry, provides the annual number of psychiatric visits at hospitals and outpatients centers; however, it does not disaggregate information by psychiatric pathology, age and gender.20
The economic downturn in Spain caused a dramatic increase in unemployment, poverty and social inequality.3,4 Housing instability, large number of evictions, unresolvable debts, and economic strain are social expressions of the economic downturn. As described in the introduction, the unemployment rate increased in all age groups but particularly for 15–34 year olds,2 which were found to have a change in psychiatric hospitalization trends starting April 2008. This age group had the most marked increase in hospitalizations, especially for those psychiatric disorders that are most sensitive to environmental changes (disturbances of conduct and emotional disorders, neurotic and personality disorders, depression and problems related to substance consumption) in contrast to organic psychosis and mental retardation, which were not found to change. The increase in psychiatric hospitalizations during this time period may be due to a change in mental health morbidity caused by the stress associated with the economic recession or may be due to a change in the use of health services as a result of the economic crisis. Austerity measures taken by the government to control public deficit, such as cutbacks in financing of community support for severe mental disorders, could also foster the number of psychiatric admissions without any increase in the real incidence of mental disorders. An additional increase in hospital discharges and psychiatric visits occurred in 2013 (Figs. 1 and 3), for which no explanation other than a possible association with the cutbacks in social and health services can be found.
Unemployment may increase the use of health services independently of the rate of mental disorders.21 In countries with high unemployment rates, men tend to consult with their general practitioner for mental complaints more frequently, irrespective of their mental health status. This association has been called “medicalization of unemployment”.22,23 Distress caused by the negative social and economic consequences of unemployment may be interpreted by the unemployed as a manifestation of ill health and coded in DSM or ICD terms and treated as a psychiatric disorder by the general practitioner. Notwithstanding, it has been reported that over a quarter of psychiatric hospitalizations are inappropriate and only caused by adverse social factors.24,25 However, it is unlikely that such a mechanism could explain psychiatric hospitalizations, where a substantial degree of clinical severity and specificity are required for admission. Another hypothesis put forward to account for the increase in psychiatric hospitalizations independently of the rate of mental health morbidity is that in times of economic contraction community tolerance toward deviance is reduced. Frustration induced by economic contraction leads to intolerance toward those viewed as deviant in the social order, such as people with mental disorders, particularly those suffering from psychosis.26 Here, this hypothesis can hardly explain the increase in psychiatric hospitalizations of people suffering from common mental disorders, but it could be applied to people with psychosis. Despite these alternative explanations, a recent systematic literature review found deterioration of mental health as a result of the economic crisis in Europe.5 A positive association between unemployment and psychiatric admissions has been repeatedly corroborated by previous studies. Nineteen papers published between 1974 and 1984 report on the association between unemployment and help-seeking behavior, and the majority confirmed the expected positive relationship.27 Fluctuations in economic indicators correlate with the rate of psychiatric admissions11,12 and readmissions13-15 in the vast majority of studies, although not in all.28-30 In a study comparing the unemployment rate and standardized psychiatric admissions in different geographic areas, the unemployment rate explained over 90% of the variation in admissions.11
Contrary to our expectations, hospital admissions caused by functional psychosis, adjusted/acute reaction to stress and diagnoses not included in another category did not significantly change in April 2008, but rather increased a few months later. In keeping with this finding, previous research has pointed out that there may be two peaks in the rate of hospitalizations following an economic downturn, one coming immediately after the onset of the crisis and a second one following few months later. A lag from two to six months between unemployment onset and change in rates of admission has been described.31,32 Consistent with our results, Barceló et al.6 found an increase in consumption of antipsychotics in Catalonia (Spain) from 2009 to 2012. The delay in the rise of rates of functional psychosis found in our study may be accounted for by the “intolerance hypothesis” during economic contraction mentioned above. It may take some time after the onset of economic crisis for the frustration in the population to develop and to consolidate and generate intolerance against behavior deviation.25 An alternative explanation may be that the 2008 crisis first triggered the rise in admissions by aggravating the clinical state of young adults already suffering from common mental disorders or by precipitating an episode in those predisposed. 341 A few months later, the persisting poor economic conditions may have eventually wore down the personal, economic and instrumental resources of some healthy young adults who then came to develop adjustment reactions, and some were admitted to hospital.
There are weaknesses and limitations in the HMS pertaining to our study. It must be noted that the database used in this study does not distinguish between hospital admissions and readmissions; thus, the volume of hospitalization rather than the hospital incidence was analyzed. On the other hand, either an increase in incidence or an increase in readmissions could suggest a worsening of patients’ mental health.
Overall, the rising number of hospitalizations leads to an extraordinary pressure on mental health services and, therefore, an increase in health spending. In this regard, it is recommended that an analysis related to increasing hospital costs as the result of the economic downturn in Spain be conducted to provide further information to public health policy makers. Ecological studies have substantial limitations. We unequivocally proved an abrupt increase on inpatients from April 2008. Such increase strongly suggests a relationship between the economic downturn and the increased psychiatric hospitalizations since the increase on hospitalizations and the onset of the economic crisis coincides in time and the hospitalization increase was found for those psychiatric disorders that are most sensitive to environmental changes in contrast to organic psychosis and mental retardation. However, the coincidence in time and the fact that we found no increase in organic psychosis and mental retardation in contrast to the increase found for the pathologies more sensitive to social changes does not conclusively prove the relationship between economic crisis and increased hospitalization. Thus, future research based on information at the individual level, including personal or familiar situation, are recommended. Finally, the analysis of psychiatric hospitalizations on men and women separately would be also highly recommended since previous publications found relevant gender differences.5
To conclude, the dramatic increase in hospitalizations necessarily entails extraordinary pressure on mental health services and an increase in health spending. Therefore, our study certainly suggests not only a deterioration of mental health in Spain but also a significant increase in health care costs in psychiatric care.
Conflict of interestNone declared.
We would like to thank Emily Brooke Felt and Suzette Smiley-Jewell for their editing work and their useful suggestions regarding our manuscript language and structure.
Please cite this article as: Medel-Herrero A, Gomez-Beneyto M. Impacto de la crisis económica del 2008 en el número de jóvenes hospitalizados por patología psiquiátrica. Rev Psiquiatr Salud Ment (Barc). 2019;12:28–36.