Psychosocial functioning is a key factor determining prognosis, severity, impairment and quality of life in people who have a mental disorder. The mini-ICF-APP was developed to provide a standardised classification of functioning and disability. However, despite its gaining popularity little is known about its structure and performance. This paper examines the structure of the mini-ICF-APP using factor analysis techniques.
Materials and methodsIn a clinical sample of 3178 patients, with psychiatric diagnoses from several ICD-10 categories, we analysed internal consistency, item inter-correlations and the factorial structure of the data, with reference to ICD-10 diagnostic categories; Neurocognitive Disorders; Alcohol Use Disorders; Substance Use Disorders; Schizophrenia and Psychotic Disorders; Bipolar Disorder; Major Depressive Disorder; Anxiety Disorders; Personality Disorders; and Neurodevelopmental Disorders.
ResultsWe found good internal consistency and item inter-correlations (Cronbach alpha=0.92) for the mini-ICF-APP. We were able to identify pivotal domains (flexibility, assertiveness and intimate relationships), which demonstrate sub-threshold influences on other domains. The factor analysis yielded a one-factor model as ideal for the whole sample and for all diagnostic categories. For some diagnostic categories the data suggested a two or three-factor model, however, with poorer fit indices.
ConclusionsThe factor structure of the mini-ICF-APP appears to modify according to the main diagnosis. However, a one-factor model demonstrates better fit regardless of diagnostic category. Consequently, we consider the mini-ICF-APP to be a trans-diagnostic measurement instrument for the assessment and grading of psychosocial functioning. The use of the mini-ICF-APP sum score seems to best reflect the degree of impairment in an individual, even taking into account that affected domains may lead to sub-threshold effects on other domains.
El funcionamiento psicosocial es un factor clave que determina el pronóstico, la gravedad, el deterioro y la calidad de vida de las personas con trastornos mentales. La escala Mini-ICF-APP fue desarrollada para aportar una clasificación estandarizada del funcionamiento e incapacidad. Sin embargo, a pesar de su creciente popularidad, se conoce poco su estructura y desempeño. Este documento examina la estructura de Mini-ICF-APP, utilizando técnicas de análisis factoriales.
Materiales y métodosEn una muestra clínica de 3.178 pacientes, con diagnósticos psiquiátricos de diversas categorías ICD-10, analizamos la consistencia interna, inter-correlaciones de ítems y estructura factorial de los datos, con referencia a las categorías diagnósticas ICD-10, trastornos neurocognitivos, trastornos de abuso de alcohol, trastornos de consumo de substancias, esquizofrenia y trastornos psicóticos, trastorno bipolar, trastorno depresivo mayor, trastorno depresivo, trastornos de ansiedad, trastornos de personalidad y trastornos neuroevolutivos.
ResultadosEncontramos buena consistencia interna e inter-correlaciones de ítems (alfa de Cronbach=0,92) para Mini-ICF-APP. Pudimos identificar dominios fundamentales (flexibilidad, asertividad y relaciones íntimas), que demostraron influencias subumbrales en otros dominios. El análisis factorial produjo un modelo unifactorial ideal para la muestra total y para todas las categorías diagnósticas. Para algunas de estas, los datos sugirieron un modelo de dos o tres factores, aunque, sin embargo, con peores índices de ajuste.
ConclusionesLa estructura factorial de la escala Mini-ICF-APP parece modificarse con arreglo a los principales diagnósticos. Sin embargo, un modelo unifactorial demuestra un mejor ajuste, independientemente de la categoría diagnóstica. Por tanto, consideramos que la escala Mini-ICF-APP es un instrumento de medida trans-diagnóstico para la evaluación y clasificación del funcionamiento psicosocial. El uso de la puntuación de sumas de la escala Mini-ICF-APP refleja mejor el grado de deterioro en un individuo, aun teniendo en cuenta que los dominios afectados podrían llevar a efectos subumbrales en otros dominios.
Psychiatric disorders are accompanied by limitations in psychosocial functioning and adjustment. Psychosocial functioning is a more important determinant for prognosis, severity, impairment and quality of life for those suffering from mental disorders than psychiatric diagnosis itself.1,2 Currently, psychiatric diagnoses rely principally on symptoms experienced and observed behaviour.3–5 Despite the importance of psychosocial functioning, the correlation between diagnosis, symptom load and psychosocial impairment is weak.6,7 This has led to an ongoing discussion about the reliability and validity of psychiatric diagnosis in general and scales measuring symptomatology in particular.5,8 In order to close this gap, the WHO (World Health Organization) designed and developed the ICF (International Classification of Functioning), recognising psychosocial functioning as a key element for health and well-being.8,9
The ICF focusses on the resources and potential of humans beings to engage in activities and participate in life, regardless of mental (or physical) condition.9 Despite its importance, the ICF is not frequently used in day to day clinical practice; due mainly to the duration and complexity of the assessment.5,6 Several instruments have been developed in order to bridge this gap10; including the mini-ICF-APP.11,12 It is a 13-item scale, developed for the assessment of psychosocial functioning in people with mental health problems, regardless of diagnosis.12 It describes and classifies disorders of activity and capacity, which may lead to restrictions in social participation.12 Since its development publications, including the first publication, on the mini-ICF-APP have demonstrated it possesses good psychometric properties together with reliability and validity across the spectrum of psychiatric diagnoses.13–17
Since its development the mini-ICF-APP has been regularly implemented by health care providers, insurance companies and pension funds to assess disability and work impairment.18,19 It is one of the routine instruments used to determine access to services and financial support (e.g. disability pension).18,20 Evaluation with the mini-ICF-APP should reflect the ability of an individual to function in their own personal and social context.12,21 The mini-ICF-APP can be interpreted at both item or sum score levels; with illness severity associated with more significant limitations in activity and capacity.17 The use of the mini-ICF-APP sum-score should however be treated with caution since it cannot be considered a global incapacity index. Patients with limitations in pivotal dimensions may experience impairment due to the impact of these on other domains.10,12
For a psychometric instrument to establish itself in clinical practice, and in particular as part of routine clinical assessment, its performance and interpretation must be known in advance. This can only be achieved through scientific scrutiny.10,18 Although the mini-ICF-APP shows good reliability and validity, several of its psychometric properties have not been thoroughly investigated.10 The mini-ICF-APP sum score is frequently reported as an outcome, and does seem to relate to severity (i.e. incapacity), independent of psychiatric diagnosis.17,21 Therefore, we are interested in identifying whether individual items of the mini-ICF-APP show different performance patterns according to diagnosis, using an exploratory factor analysis, in order to describe its factorial structure according to the main ICD-10 diagnostic categories.3
Materials and methodsMeasuresClinical Global Impression Scales (CGI)Severity was rated using the Clinical Global Impression Scales.22 The CGI scale is a pragmatic, self-explanatory, assessment tool for psychiatric disorders. Due to its straightforward implementation and comprehensibility it is widely used in clinical practice and research .22–27 The CGI consists of three subscales: 1. Severity of Illness (CGI-S), 2. Global Improvement (CGI-I), and 3. Efficacy Index (CGI-E).22 Both CGI-S and CGI-I are rated on a seven-point Likert scale; the CGI-S from “1” (healthy subject) to “7” (extremely ill subject); the CGI-I from “1” (significant improvement) to “7” (most severe deterioration), whereby a score of “4” indicates no change.22 The CGI-S and CGI-E take into account the past week, whilst the CGI-I rating relates to the time elapsed since the first/previous CGI-S assessment.
Mini-ICF-APPThe mini-ICF-APP consists of thirteen items, each one evaluating ONE capacity or domain of functioning: (1) adherence to regulations and routines; (2) planning and structuring of tasks; (3) flexibility; (4) competency/efficacy; (5) endurance; (6) assertiveness; (7) contact with others; (8) group integration; (9) family and intimate relationships; (10) leisure activities; (11) self-care; (12) mobility; and (13) competence to judge and decide.
The evaluation of each item must take into account the patient‘s personal and social context.12 Comprehensible anchor-point definitions are provided for every item,10,12 which are rated on a five-point Likert-scale from 0 (no disability) to 4 (total disability). Items rated with either three or four are considered to merit/require clinical intervention.4,12 Correspondingly, we consider items rated three or more as clinically relevant (positive). The sum score of the mini-ICF-APP ranges from 0 to 52 points; with cut-off values defining severity: mild from 3 to 7 points; moderate from 8 to 15 points; marked from16 to 24 points; severe 25 to 37; and extremely severe 38 or more points.17,21
Sample and procedureThe Centre for Integrative Psychiatry is part of the Psychiatric University Hospital of Zurich. It offers an integrative psychiatric and psychotherapeutic treatment programme for adult patients (aged 18–65 years) with a psychiatric disorder. As part of the routine clinical care and quality assessment patient and health-related data is collected; including the assessment of psychosocial functioning using the mini-ICF-APP. We analysed the mini-ICF-APP data from a five-year cohort of consecutive patients hospitalised for treatment (n=3295). Around four per cent (3.55%, n=117) of the sample were excluded due to two or more missing items from the mini-ICF-APP. Patients excluded due to missing data did not differ from those with a complete data set regarding sex, age, education, civil status and main diagnosis. The final sample used for subsequent analyses comprised 3178 patients. The competent ethics committee approved the use of the data for further analysis and publication [KEK-ZH BASEC-Nr.: 2017-01766]. This data set was also used in a previous publication, although with a different aim and statistical analysis.12
Raters and trainingRaters were either psychiatrists, psychiatry residents or clinical psychologists. All raters received regular training in the use of the measurement instruments. The study instruments assess the seven days prior to admission. Ratings were conducted within the first 72h of hospitalisation. Ratings were based on information obtained from clinical interview and direct behavioural observations; together with information provided by nursing staff, social workers and others involved in the treatment process.
Diagnosis and diagnostic groupsDiagnoses were made by a psychiatry resident according to ICD-10 criteria3 and were confirmed or corrected by a senior psychiatrist. According to ICD-10 diagnostic categories we defined nine diagnostic groups21: NCD: Neurocognitive Disorders (ICD-10: F0); AUD: Alcohol Use Disorders (ICD-10: F10: SUD: Substance Use Disorders (ICD 10: F11-19); SPD: Schizophrenia and Psychotic Disorders (ICD-10: F2); BPD: Bipolar Disorder (ICD-10: F30-31); MDD: Major Depressive Disorder (ICD 10: F32-33); AXD: Anxiety Disorders (ICD-10: F4-F5); PD: Personality Disorders (ICD-10: F6); and NDD: Neurodevelopmental Disorders (ICD-10: F7-F9).
Statistical analysisThe analysis included only participants with a complete data set at admission (one missing item on the mini-ICF-APP was acceptable). Simple descriptive statistics were used to represent the demographic and clinical characteristics of the sample; an analysis of variance (ANOVA) was performed to analyse differences between diagnostic groups. We used multivariate regression to determine the correlation between demographic (i.e. gender, age, civil status, education) and clinical variables with main diagnosis, mini-ICF-APP sum score and CGI-S. The internal consistency of the mini-ICF-APP was assessed using Cronbach's alpha.
For item correlation we used the complete spectrum of severity for every item, as well as dichotomous variables. Therefore, each response item was transformed into a dichotomous variable according to clinical relevance; items rated three or four were considered positive, with values ranging from zero to two as negative.11,12 For the exploratory factor analysis (EFA), we chose to use only the dichotomous rating of the items in order to reduce multicollinearity and determine possible latent factors.28 The Principal Component Analysis (with a Varimax rotation method) determined the number of factors to be extracted, as well as determining dimensionality and factor structure.
An eigenvalue greater than one is a prerequisite for factor extraction. The Kaiser–Meier–Olkin (KMO) index was used to measure sampling adequacy. For the assessment and comparability of the fit of the possible models we used: Eigenvalues; Chi-Square, the Comparative Fit Index (CFI); the Root Mean Square Residual (RMSR); Root Mean Square Error of Approximation (RMSEA) and the Tucker Lewis Index (TLI). Cut-off values considered indicative for a good fit were: an Eigenvalue>1; a Chi-square p value >0.05; a CFI value ≤0.90; a RMSR value <0.08; a RMSEA <0.08; and a TLI≥0.95.29,30
All statistical analyses were conducted using the statistical software “R” (v3.6.1), for multivariate regression analysis we used the package “np” (v0.60-9); for analysis of the Likert scales we used the package “Likert” (v1.3.5), and for psychometric tests including the exploratory factor analysis we used the packages “psych” (v1.9.12) and “lavaan” (v0.6-5).
ResultsThe sample included for analysis was aged between 16 and 77 years (43.50±11.88) years; with 66.36% males. The majority of the sample was single, had completed an apprenticeship or college/university education. Patient admission was mostly voluntary (94.93%), with a mean length of stay of 41.49±44.73 days; with a right skewed distribution. The CGI-S value for severity was 5.27±0.91. The total sum score of the mini-ICF-APP was 18.53±10.34, with a mean sum of positive items of 2.30±3.08 with a right skewed distribution.
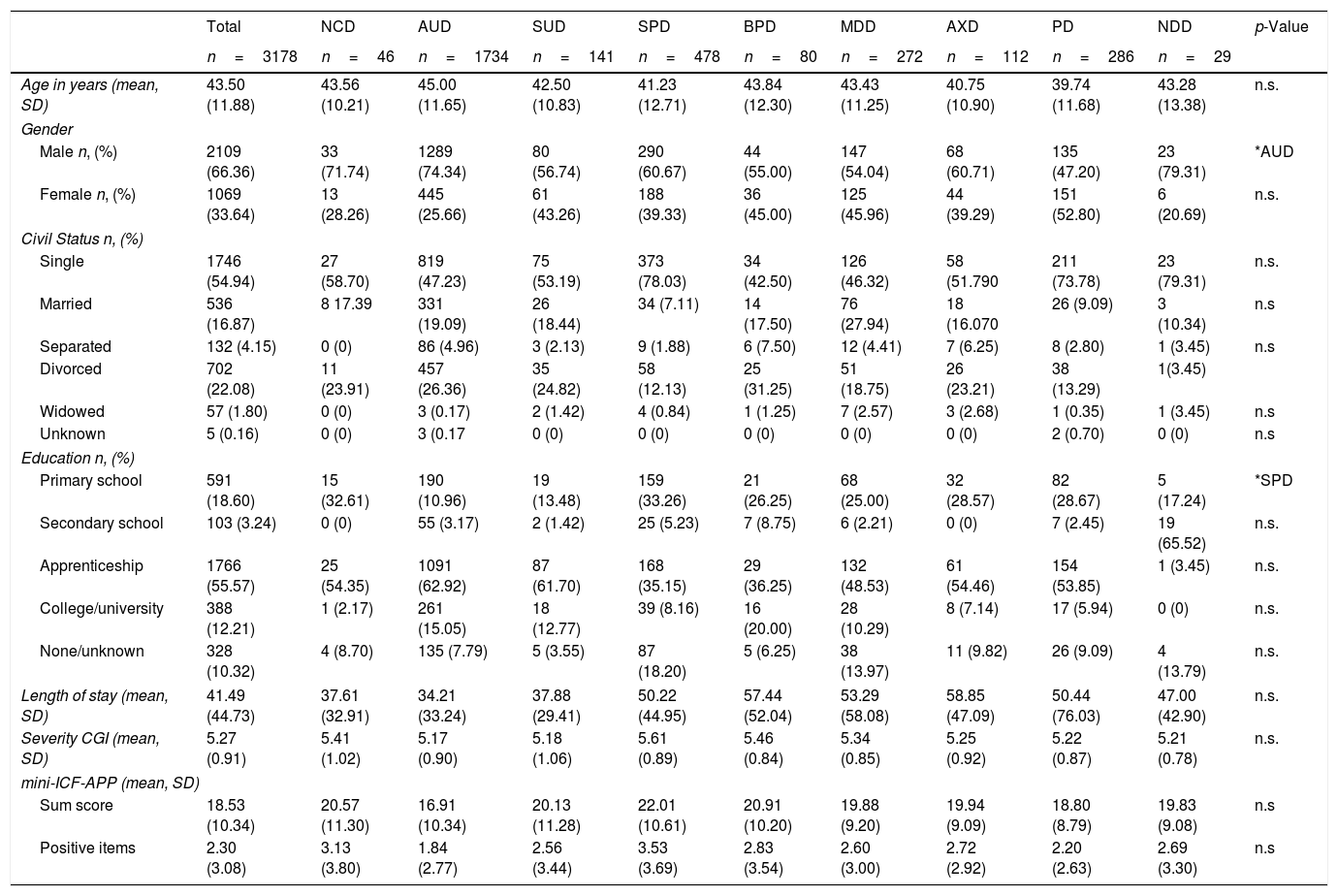
Gender distribution reached statistical significance for patients with AUD; this may be an artefact of the large sub-sample size. The shift in gender distribution for PD is also noteworthy although not clinically significant. Patients with SPD were more likely to have only completed primary school education (showed a higher proportion of primary education), reaching marginal significance. There were no further clinically significant differences between the diagnostic groups. For further details, see Table 1.
Demographic and clinical characteristics of the study sample.
| Total | NCD | AUD | SUD | SPD | BPD | MDD | AXD | PD | NDD | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n=3178 | n=46 | n=1734 | n=141 | n=478 | n=80 | n=272 | n=112 | n=286 | n=29 | ||
| Age in years (mean, SD) | 43.50 (11.88) | 43.56 (10.21) | 45.00 (11.65) | 42.50 (10.83) | 41.23 (12.71) | 43.84 (12.30) | 43.43 (11.25) | 40.75 (10.90) | 39.74 (11.68) | 43.28 (13.38) | n.s. |
| Gender | |||||||||||
| Male n, (%) | 2109 (66.36) | 33 (71.74) | 1289 (74.34) | 80 (56.74) | 290 (60.67) | 44 (55.00) | 147 (54.04) | 68 (60.71) | 135 (47.20) | 23 (79.31) | *AUD |
| Female n, (%) | 1069 (33.64) | 13 (28.26) | 445 (25.66) | 61 (43.26) | 188 (39.33) | 36 (45.00) | 125 (45.96) | 44 (39.29) | 151 (52.80) | 6 (20.69) | n.s. |
| Civil Status n, (%) | |||||||||||
| Single | 1746 (54.94) | 27 (58.70) | 819 (47.23) | 75 (53.19) | 373 (78.03) | 34 (42.50) | 126 (46.32) | 58 (51.790 | 211 (73.78) | 23 (79.31) | n.s. |
| Married | 536 (16.87) | 8 17.39 | 331 (19.09) | 26 (18.44) | 34 (7.11) | 14 (17.50) | 76 (27.94) | 18 (16.070 | 26 (9.09) | 3 (10.34) | n.s |
| Separated | 132 (4.15) | 0 (0) | 86 (4.96) | 3 (2.13) | 9 (1.88) | 6 (7.50) | 12 (4.41) | 7 (6.25) | 8 (2.80) | 1 (3.45) | n.s |
| Divorced | 702 (22.08) | 11 (23.91) | 457 (26.36) | 35 (24.82) | 58 (12.13) | 25 (31.25) | 51 (18.75) | 26 (23.21) | 38 (13.29) | 1(3.45) | |
| Widowed | 57 (1.80) | 0 (0) | 3 (0.17) | 2 (1.42) | 4 (0.84) | 1 (1.25) | 7 (2.57) | 3 (2.68) | 1 (0.35) | 1 (3.45) | n.s |
| Unknown | 5 (0.16) | 0 (0) | 3 (0.17 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (0.70) | 0 (0) | n.s |
| Education n, (%) | |||||||||||
| Primary school | 591 (18.60) | 15 (32.61) | 190 (10.96) | 19 (13.48) | 159 (33.26) | 21 (26.25) | 68 (25.00) | 32 (28.57) | 82 (28.67) | 5 (17.24) | *SPD |
| Secondary school | 103 (3.24) | 0 (0) | 55 (3.17) | 2 (1.42) | 25 (5.23) | 7 (8.75) | 6 (2.21) | 0 (0) | 7 (2.45) | 19 (65.52) | n.s. |
| Apprenticeship | 1766 (55.57) | 25 (54.35) | 1091 (62.92) | 87 (61.70) | 168 (35.15) | 29 (36.25) | 132 (48.53) | 61 (54.46) | 154 (53.85) | 1 (3.45) | n.s. |
| College/university | 388 (12.21) | 1 (2.17) | 261 (15.05) | 18 (12.77) | 39 (8.16) | 16 (20.00) | 28 (10.29) | 8 (7.14) | 17 (5.94) | 0 (0) | n.s. |
| None/unknown | 328 (10.32) | 4 (8.70) | 135 (7.79) | 5 (3.55) | 87 (18.20) | 5 (6.25) | 38 (13.97) | 11 (9.82) | 26 (9.09) | 4 (13.79) | n.s. |
| Length of stay (mean, SD) | 41.49 (44.73) | 37.61 (32.91) | 34.21 (33.24) | 37.88 (29.41) | 50.22 (44.95) | 57.44 (52.04) | 53.29 (58.08) | 58.85 (47.09) | 50.44 (76.03) | 47.00 (42.90) | n.s. |
| Severity CGI (mean, SD) | 5.27 (0.91) | 5.41 (1.02) | 5.17 (0.90) | 5.18 (1.06) | 5.61 (0.89) | 5.46 (0.84) | 5.34 (0.85) | 5.25 (0.92) | 5.22 (0.87) | 5.21 (0.78) | n.s. |
| mini-ICF-APP (mean, SD) | |||||||||||
| Sum score | 18.53 (10.34) | 20.57 (11.30) | 16.91 (10.34) | 20.13 (11.28) | 22.01 (10.61) | 20.91 (10.20) | 19.88 (9.20) | 19.94 (9.09) | 18.80 (8.79) | 19.83 (9.08) | n.s |
| Positive items | 2.30 (3.08) | 3.13 (3.80) | 1.84 (2.77) | 2.56 (3.44) | 3.53 (3.69) | 2.83 (3.54) | 2.60 (3.00) | 2.72 (2.92) | 2.20 (2.63) | 2.69 (3.30) | n.s |
Significance levels: n.s.: non-significant; *: p<0.5; **: p<0.01; ***: p<0.001.
A general linear model found no statistically significant correlation between the mini-ICF-APP scores (sum score or total items with clinically relevant scores) and the main diagnosis, after correction for demographic parameters (age, gender, civil status, education). The correlation between the mini-ICF-APP sum score and the CGI-S score was statistically significant, for the whole sample and all diagnostic groups.
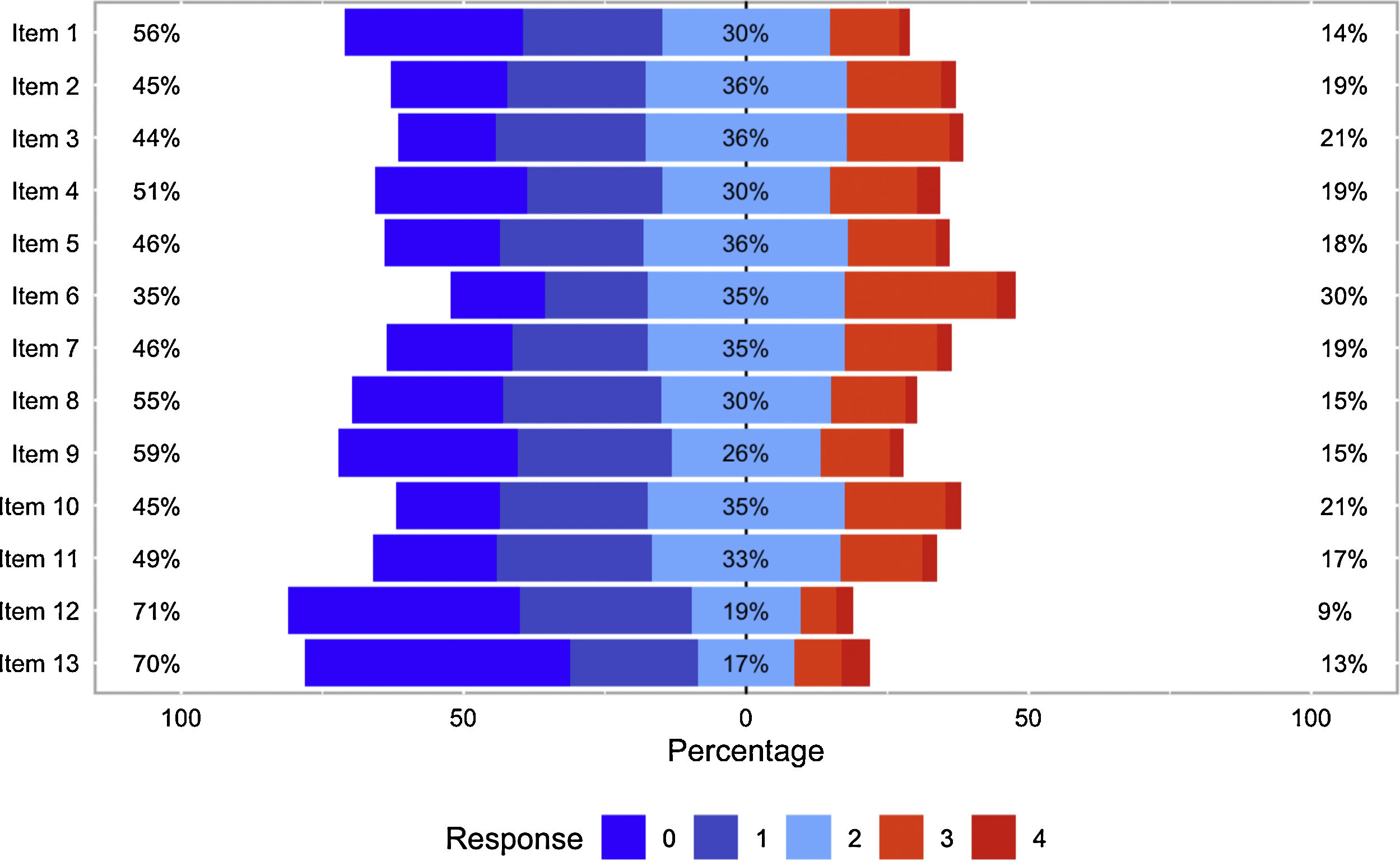
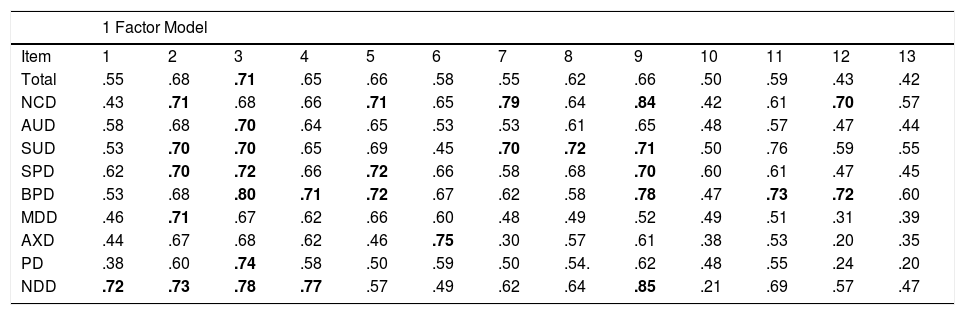
Item performance, internal consistency, and IntercorrelationThe distribution of severity for each mini-ICF-APP item is shown in Fig. 1. The internal consistency for the mini-ICF-APP ratings for the whole spectrum of severity yields a Cronbach's alpha value of 0.93. The dichotomous mini-ICF-APP scale yields a Cronbach's alpha value of 0.87. Cronbach alpha values>0.80 indicate good levels of internal consistency; however, values>0.90 might indicate multicollinearity.31 The higher Cronbach alpha value yield for items covering the whole spectrum of severity (i.e. from none to severe) suggested multicollinearity, which was confirmed when analysing the correlation between single items.31
Response to each Item (Item 1: adherence; Item 2: planning; Item 3: flexibility; Item 4: competency; Item 5: endurance; Item 6: assertiveness; Item 7: contact; Item 8: group; Item 9: relations; Item 10: leisure; Item 11: self-care; Item 12: mobility; and Item 13: judgement) for the whole spectrum of severity (Likert type scale: 0=none; 1, minimal; 2=mild; 3=moderate and 4=severe).
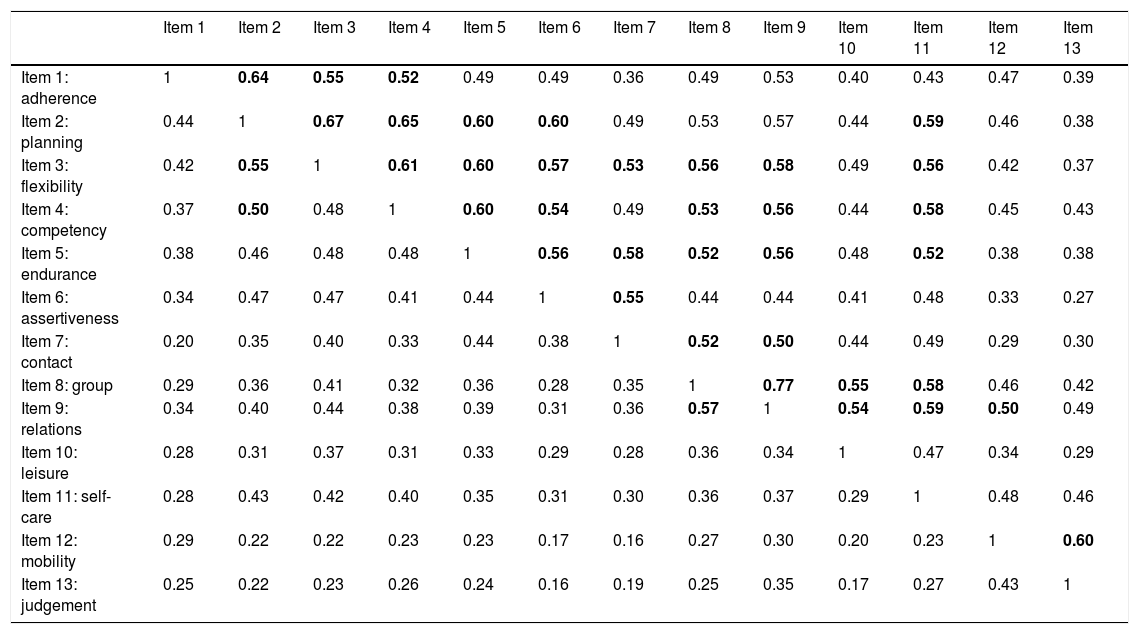
The inter-correlation of the mini-ICF-APP items is shown in Table 2. In the upper half, the inter-correlation for the whole spectrum of severity (from none to severe); in the lower for clinically relevant items (i.e. items with a rating of three or four). We considered correlation indices>0.50 as relevant.32 The inter-correlation of items was higher when using the whole spectrum of severity, as foreseen in the mini-ICF-APP manual.12
Inter-correlation between Items. In the lower half the dichotomous ratings are presented. In the upper half the ratings using the whole spectrum of severity are presented (inter-correlations>0.50 are bold).
| Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Item 12 | Item 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item 1: adherence | 1 | 0.64 | 0.55 | 0.52 | 0.49 | 0.49 | 0.36 | 0.49 | 0.53 | 0.40 | 0.43 | 0.47 | 0.39 |
| Item 2: planning | 0.44 | 1 | 0.67 | 0.65 | 0.60 | 0.60 | 0.49 | 0.53 | 0.57 | 0.44 | 0.59 | 0.46 | 0.38 |
| Item 3: flexibility | 0.42 | 0.55 | 1 | 0.61 | 0.60 | 0.57 | 0.53 | 0.56 | 0.58 | 0.49 | 0.56 | 0.42 | 0.37 |
| Item 4: competency | 0.37 | 0.50 | 0.48 | 1 | 0.60 | 0.54 | 0.49 | 0.53 | 0.56 | 0.44 | 0.58 | 0.45 | 0.43 |
| Item 5: endurance | 0.38 | 0.46 | 0.48 | 0.48 | 1 | 0.56 | 0.58 | 0.52 | 0.56 | 0.48 | 0.52 | 0.38 | 0.38 |
| Item 6: assertiveness | 0.34 | 0.47 | 0.47 | 0.41 | 0.44 | 1 | 0.55 | 0.44 | 0.44 | 0.41 | 0.48 | 0.33 | 0.27 |
| Item 7: contact | 0.20 | 0.35 | 0.40 | 0.33 | 0.44 | 0.38 | 1 | 0.52 | 0.50 | 0.44 | 0.49 | 0.29 | 0.30 |
| Item 8: group | 0.29 | 0.36 | 0.41 | 0.32 | 0.36 | 0.28 | 0.35 | 1 | 0.77 | 0.55 | 0.58 | 0.46 | 0.42 |
| Item 9: relations | 0.34 | 0.40 | 0.44 | 0.38 | 0.39 | 0.31 | 0.36 | 0.57 | 1 | 0.54 | 0.59 | 0.50 | 0.49 |
| Item 10: leisure | 0.28 | 0.31 | 0.37 | 0.31 | 0.33 | 0.29 | 0.28 | 0.36 | 0.34 | 1 | 0.47 | 0.34 | 0.29 |
| Item 11: self-care | 0.28 | 0.43 | 0.42 | 0.40 | 0.35 | 0.31 | 0.30 | 0.36 | 0.37 | 0.29 | 1 | 0.48 | 0.46 |
| Item 12: mobility | 0.29 | 0.22 | 0.22 | 0.23 | 0.23 | 0.17 | 0.16 | 0.27 | 0.30 | 0.20 | 0.23 | 1 | 0.60 |
| Item 13: judgement | 0.25 | 0.22 | 0.23 | 0.26 | 0.24 | 0.16 | 0.19 | 0.25 | 0.35 | 0.17 | 0.27 | 0.43 | 1 |
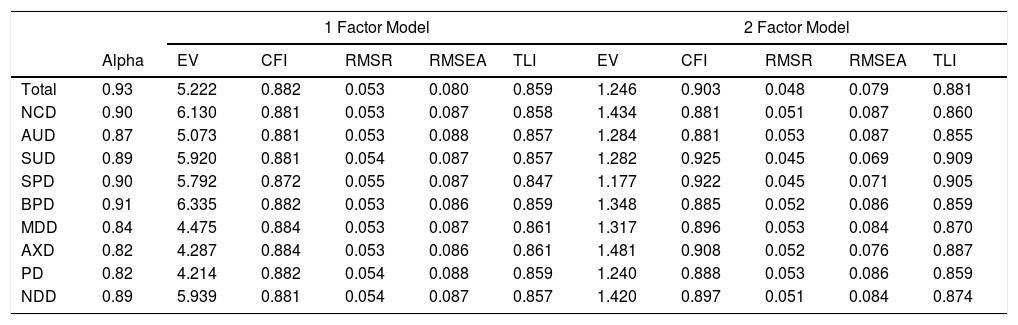
The KMO calculated was 0.92, supporting the adequacy of sampling for factor analysis. We calculated possible EFA models for the total sample and all diagnostic categories, based on the eigenvalues presented. In our opinion only eigenvalues greater than one are indicative of the presence of a meaningful model. For the total sample and for most diagnostic groups, a one or two-factor structure seems to be the preferred model. However, MDD, AXD and PD had values suggesting a three- or even four-factor model. Table 3 summarises the eigenvalues obtained together with fit indices for all possible models. Due to the large sample size Chi-square was positive for all models,28,33 therefore we consider this non-informative.
Cronbach's Alpha. Eigenvalues and fit indices for the different factor models, according to diagnostic group.
| 1 Factor Model | 2 Factor Model | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Alpha | EV | CFI | RMSR | RMSEA | TLI | EV | CFI | RMSR | RMSEA | TLI | |
| Total | 0.93 | 5.222 | 0.882 | 0.053 | 0.080 | 0.859 | 1.246 | 0.903 | 0.048 | 0.079 | 0.881 |
| NCD | 0.90 | 6.130 | 0.881 | 0.053 | 0.087 | 0.858 | 1.434 | 0.881 | 0.051 | 0.087 | 0.860 |
| AUD | 0.87 | 5.073 | 0.881 | 0.053 | 0.088 | 0.857 | 1.284 | 0.881 | 0.053 | 0.087 | 0.855 |
| SUD | 0.89 | 5.920 | 0.881 | 0.054 | 0.087 | 0.857 | 1.282 | 0.925 | 0.045 | 0.069 | 0.909 |
| SPD | 0.90 | 5.792 | 0.872 | 0.055 | 0.087 | 0.847 | 1.177 | 0.922 | 0.045 | 0.071 | 0.905 |
| BPD | 0.91 | 6.335 | 0.882 | 0.053 | 0.086 | 0.859 | 1.348 | 0.885 | 0.052 | 0.086 | 0.859 |
| MDD | 0.84 | 4.475 | 0.884 | 0.053 | 0.087 | 0.861 | 1.317 | 0.896 | 0.053 | 0.084 | 0.870 |
| AXD | 0.82 | 4.287 | 0.884 | 0.053 | 0.086 | 0.861 | 1.481 | 0.908 | 0.052 | 0.076 | 0.887 |
| PD | 0.82 | 4.214 | 0.882 | 0.054 | 0.088 | 0.859 | 1.240 | 0.888 | 0.053 | 0.086 | 0.859 |
| NDD | 0.89 | 5.939 | 0.881 | 0.054 | 0.087 | 0.857 | 1.420 | 0.897 | 0.051 | 0.084 | 0.874 |
| 3 Factor Model | 4 Factor Model | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Alpha | EV | CFI | RMSR | RMSEA | TLI | EV | CFI | RMSR | RMSEA | TLI | |
| Total | 0.93 | 0.907 | - | - | - | - | 0.702 | - | - | - | - |
| NCD | 0.90 | 1.131 | 0.885 | 0.052 | 0.086 | 0.860 | 0.830 | - | - | - | - |
| AUD | 0.87 | 0.881 | - | - | - | - | 0.769 | - | - | - | - |
| SUD | 0.89 | 0.924 | - | - | - | - | 0.845 | - | - | - | - |
| SPD | 0.90 | 0.865 | - | - | - | - | 0.770 | - | - | - | - |
| BPD | 0.91 | 1.017 | 0.896 | 0.050 | 0.082 | 0.873 | 0.843 | - | - | - | - |
| MDD | 0.84 | 1.202 | 0.948 | 0.036 | 0.061 | 0.933 | 0.926 | - | - | - | - |
| AXD | 0.82 | 1.171 | 0.924 | 0.049 | 0.076 | 0.899 | 1.104 | 0.924 | 0.046 | 0.071 | 0.904 |
| PD | 0.82 | 1.140 | 0.849 | 0.036 | 0.083 | 0.936 | 0.904 | - | - | - | - |
| NDD | 0.89 | 1.206 | 0.847 | 0.051 | 0.081 | 0.870 | 0.995 | - | - | - | - |
EV: Eigenvalue; CFI: Comparative Fit Index; RMSR: Root Mean Square Residual; RMSEA: Root Mean Square Error of Approximation; TLI: Tucker Lewis Index.
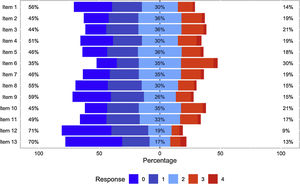
We calculated the factor loadings for both one- and two-factor models, for the total sample and for each diagnostic category. Loadings>0.70 were considered relevant.17 The results are presented in Table 4. Overall, we found a robust loading for each item in the one-factor model; the distributions of items on the different factors in the two-factor model were not consistent across diagnostic groups as previously outlined (data not shown).
Factor loading for every possible factor model according to diagnostic category (values >0.70 are bold); with the exception of the one factor model, the superscript denotes the factor each item is loading to.
| 1 Factor Model | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
| Total | .55 | .68 | .71 | .65 | .66 | .58 | .55 | .62 | .66 | .50 | .59 | .43 | .42 |
| NCD | .43 | .71 | .68 | .66 | .71 | .65 | .79 | .64 | .84 | .42 | .61 | .70 | .57 |
| AUD | .58 | .68 | .70 | .64 | .65 | .53 | .53 | .61 | .65 | .48 | .57 | .47 | .44 |
| SUD | .53 | .70 | .70 | .65 | .69 | .45 | .70 | .72 | .71 | .50 | .76 | .59 | .55 |
| SPD | .62 | .70 | .72 | .66 | .72 | .66 | .58 | .68 | .70 | .60 | .61 | .47 | .45 |
| BPD | .53 | .68 | .80 | .71 | .72 | .67 | .62 | .58 | .78 | .47 | .73 | .72 | .60 |
| MDD | .46 | .71 | .67 | .62 | .66 | .60 | .48 | .49 | .52 | .49 | .51 | .31 | .39 |
| AXD | .44 | .67 | .68 | .62 | .46 | .75 | .30 | .57 | .61 | .38 | .53 | .20 | .35 |
| PD | .38 | .60 | .74 | .58 | .50 | .59 | .50 | .54. | .62 | .48 | .55 | .24 | .20 |
| NDD | .72 | .73 | .78 | .77 | .57 | .49 | .62 | .64 | .85 | .21 | .69 | .57 | .47 |
| 2 Factor Model | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
| Total | .481 | .671 | .711 | .621 | .641 | .631 | .521 | .461 | .512 | .451 | .501 | .632 | .632 |
| NCD | .652 | .581 | .581 | .551 | .911 | .691 | .801 | .541 | .632 | .612 | .491 | .622 | .482 |
| AUD | .481 | .651 | .681 | .631 | .641 | .581 | .521 | .461 | .512 | .451 | .521 | .682 | .682 |
| SUD | .531 | .581 | .731 | .611 | .731 | .491 | .561 | .592 | .602 | .392 | .601 | .742 | .722 |
| SPD | .531 | .731 | .671 | .601 | .661 | .691 | .491 | .632 | .682 | .452 | .472 | .532 | .552 |
| BPD | .542 | .501 | .751 | .642 | .661 | .571 | .831 | .521 | .731 | .401 | .531 | .832 | .772 |
| MDD | .501 | .671 | .621 | .561 | .621 | .681 | .362 | .672 | .682 | .472 | .462 | .271 | .301 |
| AXD | .471 | .771 | .591 | .531 | .352 | .741 | .532 | .742 | .752 | .312 | .511 | .271 | .262 |
| PD | .381 | .611 | .741 | .581 | .501 | .591 | .501 | .602 | .621 | .471 | .541 | .241 | .20 |
| NDD | .741 | .801 | .631 | .732 | .441 | .641 | .541 | .622 | .642 | .151 | .631 | .792 | .582 |
| 3 Factor Model | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
| Total | - | - | - | - | - | - | - | - | - | - | - | - | - |
| NCD | .833 | .581 | .591 | .561 | .801 | .771 | .781 | .481 | .551 | .553 | .662 | .622 | .742 |
| AUD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| SUD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| SPD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| BPD | .552 | .571 | .661 | .612 | .641 | .611 | .771 | .823 | .633 | .313 | .452 | .802 | .752 |
| MDD | .441 | .651 | .661 | .521 | .621 | .671 | .372 | .682 | .652 | .472 | .452 | .623 | .543 |
| AXD | .421 | .591 | .691 | .461 | .531 | .661 | .512 | .732 | .712 | .34 | .683 | .323 | .243 |
| PD | .451 | .681 | .631 | .591 | .441 | .541 | .372 | .922 | .502 | .352 | .392 | .483 | .393 |
| NDD | .771 | .731 | .543 | .792 | .623 | .571 | .813 | .582 | .622 | .231 | .531 | .732 | .532 |
| 4 Factor Model | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
| Total | - | - | - | - | - | - | - | - | - | - | - | - | - |
| NCD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| AUD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| SUD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| SPD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| BPD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| MDD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| AXD | .491 | .631 | .691 | .471 | .451 | .701 | .684 | .474 | .833 | .272 | .89 | .272 | .433 |
| PD | - | - | - | - | - | - | - | - | - | - | - | - | - |
| NDD | - | - | - | - | - | - | - | - | - | - | - | - | - |
The findings of our exploratory factor analysis of the mini-ICF-APP in a clinical population support the validity of the mini-ICF-APP for the assessment and categorisation of patients with a psychiatric disorder according to their level of functional impairment. Our results do not support the search for sub-factors relating to the functionality of patients with a given diagnosis. Furthermore, our results support the use of the scale as a whole for this purpose; confirming the usefulness of the sum-score for evaluation purposes.
The results we obtained are comparable to results from previous studies, yielding similar sum-scores for the mini-ICF-APP and similar severity gradings according to the CGI-S; moreover, values for internal consistency are identical.13–16,34 In contrast to previous publications examining the mini-ICF-APP, we were able to study a large clinical population. Furthermore, we included psychiatric disorders underrepresented in previous publications; including alcohol and substance use disorders; personality disorders and neurocognitive/neurodevelopmental disorders.17 This allows for a broader interpretation of the results obtained.
In our exploratory factor analysis, the one-factor model showed the best-fit indices for all diagnostic groups as a whole as well as for each diagnostic group considered individually.28,32,33 For several diagnostic groups, a two- or three-factor model was suggested by the data; however, their fit indices were not consistently superior to the one-factor model,28,33 whilst having generally lower item-loadings for each possible factor (Table 4). Taking into account the parsimony criterion, we consider the one-factor model preferable.29,30
Previous analyses of the factor structure of the mini-ICF-APP report two- and a three-factor solutions.16,34 Neither the factor structures nor the item distribution were replicated in our analysis. This may result from differences in sample size and diagnoses compared to previous studies.16,28,34 We see this corroborated in our analysis, as different factor structures and item loadings were generated for different diagnostic categories.
The analysis of the loadings and inter-correlation of the different items of the mini-ICF-APP, showed that certain items hold a pivotal position. The rating of “flexibility” (Item 3), “assertiveness” (Item 6) and “intimate relationships” (Item 9) yield a high correlation with the remaining items (particularly when the whole spectrum of severity is considered). Furthermore, these items hold high loading values across diagnostic categories. We consider this finding unsurprising since these elements are important for coping with challenges in life and adapting to circumstances as well as overcoming adversity.35,36
Although our sample size was large, some diagnostic categories (NCD, BPD, AXD and NDD) were underrepresented (<130, ratio 1:10) which is suboptimal for factor analysis.32 Therefore, the analysis conducted for these diagnostic categories should be interpreted with caution, the data is however included for the sake of completeness. Furthermore, several diagnostic categories used (i.e. NCD, PD and NDD) include an extremely heterogeneous group of diagnoses. This may explain the lack of difference in age for those with a neurocognitive disorder (NCD), since the group includes not only patients with a form of Dementia (ICD-10: F00 to F03) but also with other organic brain disorders (e.g. Delirium-ICD-10: F05).
Our analysis has confirmed the development and design of the mini-ICF-APP,11,12 as an instrument for measuring psychosocial functioning in patients suffering from a psychological disorder. Furthermore, although patterns of functioning, (i.e. impairment) vary across the different psychiatric diagnoses, some pivotal domains remain constant. In accordance with our results, we consider the mini-ICF-APP to be a universally applicable tool for the assessment and grading of psychosocial functioning.
When interpreting our results, it must be taken into account that the study data was collected from patients requiring hospitalisation for treatment; a higher symptom load is likely which may influence certain domains of psychosocial functioning, particularly at the time of admission.37–40 The distinct influence of symptoms on psychosocial functioning could be accountable for the latent factor structure found for the different diagnostic groups. We consider the use of the sum-score an easy and intuitively understood method; taking into account that symptoms as well as psychosocial functioning domains seem to have a sub-threshold impact on others;17 consequently, increasing the total degree of impairment. In conclusion, we would encourage the use of the mini-ICF-APP to determine levels of psychosocial impairment in people suffering from a mental disorder in order to shape therapy accordingly, with a view to reestablishing the ability to cope with life and overcome adversity.41
ConclusionsThe mini-ICF-APP is an assessment and rating tool to assess psychosocial functioning, in people with a mental disorder regardless of psychiatric diagnosis. We identified a one-factor model, including all items, as the one with the best-fit values, irrespective of diagnostic category. Accordingly, we consider the mini-ICF-APP as a trans-diagnostic measurement instrument for the evaluation of all aspects of psychosocial functioning. The use of the mini-ICF-APP sum score seems to reflect the degree of impairment suffered by an individual, even taking into account that pivotal domains may lead to sub-threshold effects on others.
Lorna McBroom: for proofreading and language editing.