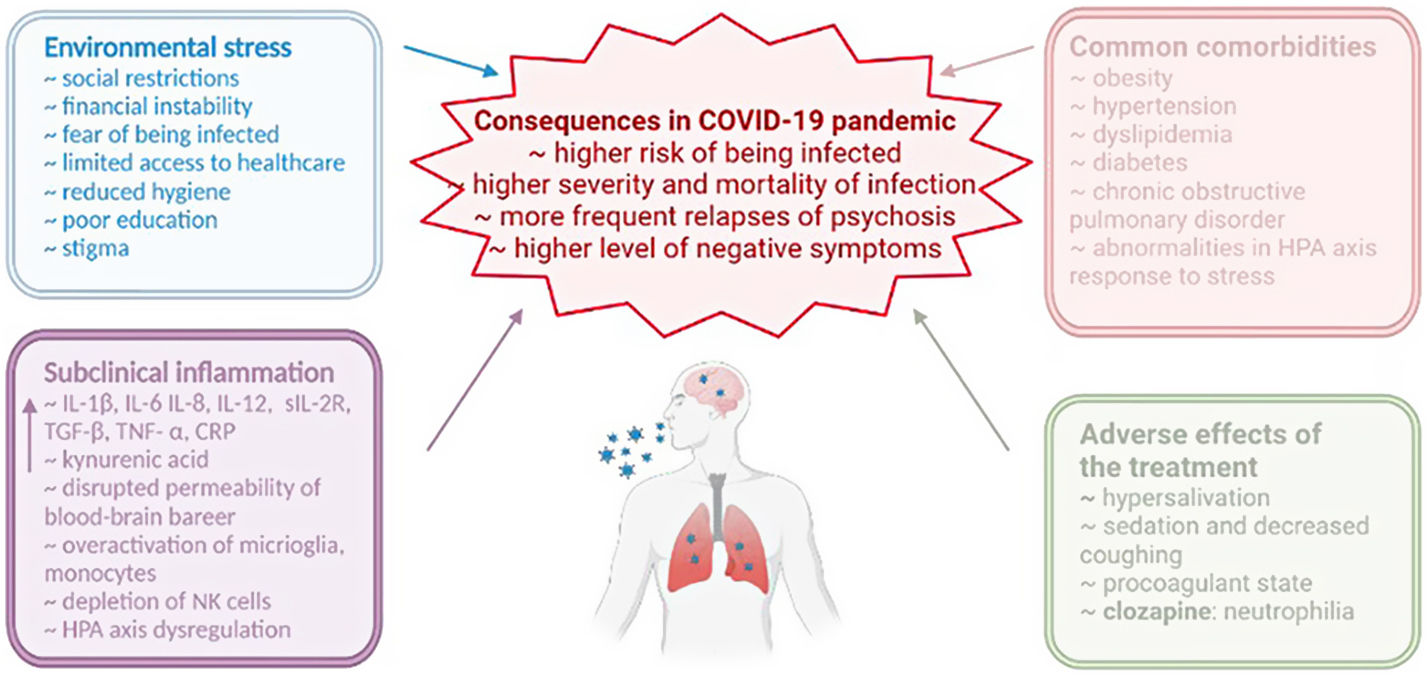
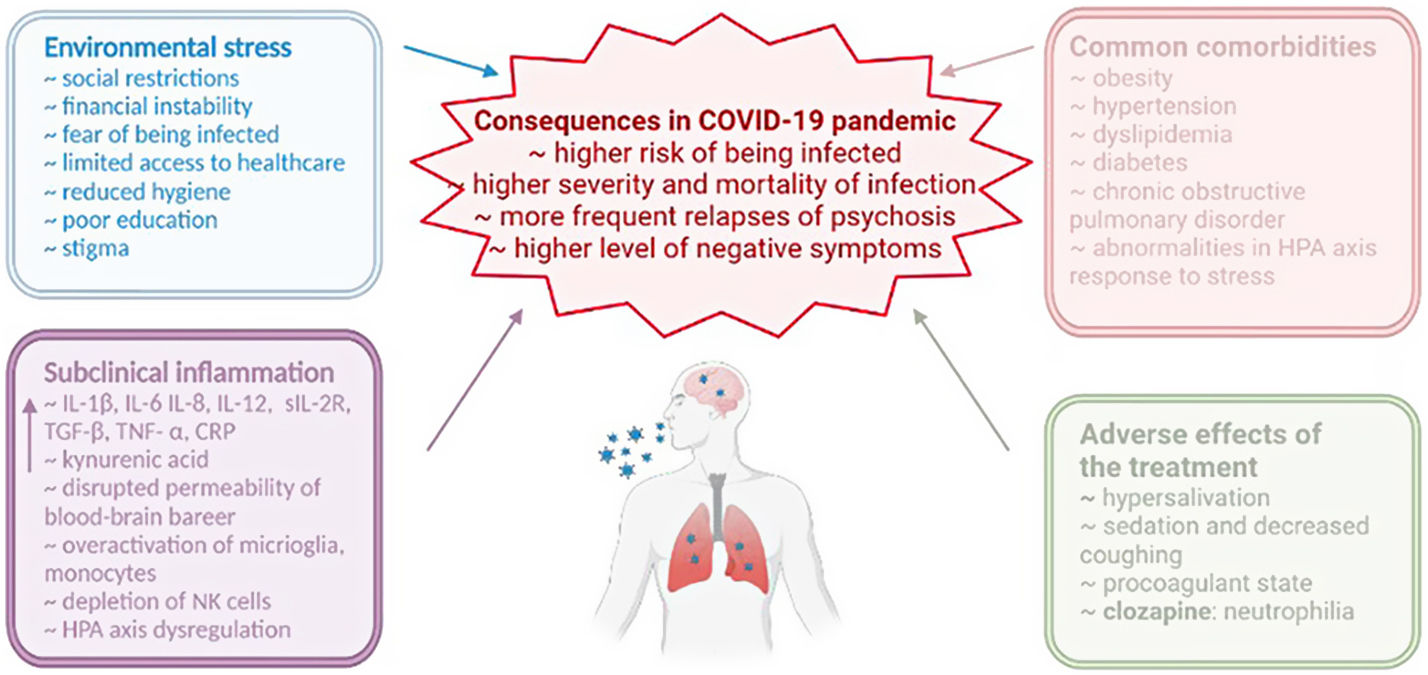
The outbreak of the Coronavirus Disease 2019 (COVID-19) pandemic in 2020 caused a rapid worsening of global mental health. Patients with severe mental disorders, including schizophrenia, are at higher risk of being infected. The neuroinvasive potential of the severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has been confirmed. The aim of this article was to present a narrative and comprehensive review of multidimensional associations between schizophrenia and COVID-19 with special emphasis on common biological pathways. Online searches were performed in the PubMed database and covered the publication period until September 17, 2022. Search terms included “psychosis”, “schizophrenia”, “inflammation” and “COVID-19”. Viewed as a neuroinflammatory state, schizophrenia shares several neurobiological mechanisms with the COVID-19. Environmental stress, common comorbidities of schizophrenia and adverse effects of antipsychotic treatment are associated with the higher severity and mortality of the COVID-19. Additionally, more frequent relapses of psychosis have been observed, and might be related to lower treatment adherence. In the context of clinical manifestation, higher level of negative symptoms has been identified among patients with schizophrenia during the pandemic. Improvements in mental health care policy and treatment adjustment are necessary to protect people with schizophrenia who are the population that is particularly vulnerable to the consequences of the COVID-19 pandemic. Future research will show if prenatal infection with the SARS-CoV-2 increases a risk of psychosis.
The outbreak of the Coronavirus Disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2), contributed to a rapid change in social relations. The enormous impact of the COVID-19 pandemic on the global society, also in terms of mental health, has been observed.1 Mental disorders are associated with the higher risk of COVID-19 infection and poor outcomes.2 Governments have introduced several restrictions soon after the pandemic started (i.e., quarantine, social distancing and isolation, school and business closures as well as border control) which increase psychological stress and might exacerbate psychiatric disorders.3,4 At this point, it is important that individuals with severe mental illness represented by schizophrenia might be particularly vulnerable to the effect of the SARS-CoV-2 infection. Indeed, this population is characterized by high prevalence rates of cardiometabolic comorbidities that are known to increase mortality in the course of COVID-19.5,6 Moreover, individuals with schizophrenia have lower access to healthcare.7 Furthermore, they have higher rates of hospitalization due to the COVID-19 than the general population.8 Therefore, it seems to be crucial to investigate potential associations between the COVID-19 and schizophrenia. Studies in this field may lead to the identification of novel risk factors of psychosis and better understanding of immune-inflammatory mechanisms underlying the development of psychosis. This may enable to employ appropriate prevention and treatment of psychosis during the pandemic.
Schizophrenia, among other psychiatric disorders, has been associated with the highest risk of severe or fatal COVID-19 infection.9–11 They evince deficiencies in oral hygiene which is important in terms of respiratory infections.12 Individuals with schizophrenia are characterized by low socioeconomic and educational status.13 Consequently, they are more likely to stay in nursing homes, night shelters or being homeless. These places are often overcrowded and characterized by reduced hygiene, increasing a risk of the SARS-CoV-2 infection as well as the COVID-19 severity and mortality.2 Similarly, psychiatric inpatient units might also be a place of the rapid SARS-CoV-2 transmission.14 There is some evidence that patients with schizophrenia spectrum disorders might be less likely to stay at home and wear facemasks outside as preventative measures compared to individuals with affective disorders, but not healthy individuals.15 Patients with severe mental illness also report less fear or worry related to the COVID-19 pandemic.16 Accordingly, it has been found that individuals with schizophrenia might be under-vaccinated despite their higher willingness to be vaccinated in comparison with healthy controls.17 Moreover, decreased cognitive and communication skills favor their social isolation and a lack of self-awareness. Patients with schizophrenia poorly comprehend and finally they are do not receive appropriate medical care.18 Similarly, stigma might cause an additional barrier to access health care by making them averse to seek medical assessment due to the fear of discrimination.19 This situation is exaggerated by the pandemic restrictions and may result in delayed and ineffective medical intervention. It has been reported that individuals with schizophrenia, during the pandemic, more frequently miss their scheduled appointments with healthcare providers.20
Although social aspects might largely explain higher COVID-19 morbidity and mortality in patients with schizophrenia, certain aspects related to the pathophysiology of schizophrenia might also point to these phenomena. To date, the majority of review articles have addressed this topic selectively, which makes it difficult for clinicians to reintegrate existing evidence. Therefore, the aim of this article was to present a narrative and comprehensive review of multidimensional associations between schizophrenia and COVID-19 with emphasis on common biological pathways. The building block hypothesis of this review was that multiple pathways involved in the pathophysiology of schizophrenia and the COVID-19 overlap and increase the risk of poor outcomes in individuals with schizophrenia. Furthermore, we hypothesized that this overlap may increase the risk of psychosis in patients with the COVID-19. First, we provide an overview of biological mechanisms involved in the pathophysiology of schizophrenia with particular attention to the role of inflammation, which is widely observed in patients with schizophrenia and might be strongly related to the risk of COVID-19 morbidity and mortality.21,22 Finally, we highlight implications of the COVID-19 pandemic for the treatment of psychosis.
MethodsThe PubMed electronic database was searched using the following terms: (((schizophr*Title/Abstract]) OR (inflamm*[Title/Abstract])) AND ((COVID-19[Title/Abstract]) OR (SARD-CoV-2[Title/Abstract]))). Online searches covered the publication period between March 11, 2020, and September 17, 2022. The 3524 publication records were found. Only articles published in English were reviewed. Online searches were performed by K.K. with the focus on systematic reviews and meta-analyses. Reference lists of publications were searched in order to identify additional articles covering the topics of interest for the present article. The process was supervised by B.M. and the selection of articles was consulted jointly.
ResultsA total of 128 publication records (58 observational studies, 40 narrative reviews and 30 systematic reviews/meta-analysis) were included in this narrative review. Eligible publications were discussed within the five main topics: (1) the immune-inflammatory concept of the schizophrenia and the COVID-19; (2) association between severity of COVID-19 and schizophrenia; (3) psychosis onset during the COVID-19 pandemic; (4) the COVID-19 pandemic and clinical expression of psychosis and (5) the treatment of psychosis in pandemic times.
The immune-inflammatory concept of schizophrenia and the COVID-19Several lines of evidence indicate the involvement of aberrant immune-inflammatory responses in the pathophysiology of schizophrenia. Indeed, immune-inflammatory factors are considered as important factors influencing the early brain development. It has been shown that prenatal infections might be related to higher risk of psychosis in offspring.23 Similar observations have been made with respect to the increased levels of maternal C-reactive protein (CRP), tumor necrosis factor-α (TNF-α), interleukin (IL)-8 and IL-10. Specifically, pro-inflammatory cytokines play a key role in regulating migration, proliferation and differentiation of neurons, their communication with microglia and synaptic pruning.24
Particular attention has been paid to the role of prenatal viral infections due to possible interactions with the early brain development. Initially, the interest in this issue has originated from observations made in ecological research.25 Although initial studies have focused on the influenza virus, more recent studies have also investigated the role of other infections. The convergent seasonality of influenza and births of patients developing schizophrenia thereafter has not been clarified. Albeit, it has been shown that maternal influenza B is associated with poor cognitive performance in the offspring with schizophrenia compared to those whose mothers had not been infected.26 The compelling evidence of higher risk of psychotic disorders in offspring is related to maternal prenatal infection by Toxoplasmosis gondii and the Herpes Simplex Virus – type 2 (HSV-2). In turn, studies investigating the seropositivity of cytomegalovirus should be replicated to draw more reliable conclusions.23,27
In 2003, there was an outbreak of the SARS-CoV-1 pandemic. It occasionally led to psychiatric symptoms and evidence of its neurotropism was partially confirmed. However, follow-up studies of pregnant women infected with the SARS-CoV-1 will require time to test the associations between prenatal COVID-19 and psychosis risk in offspring.28 During the COVID-19 pandemic, it has already been found that the risk of severe COVID-19 course is higher in pregnancy. Vertical transmission is likely to occur; however, it is not common and the exact mechanism remains unknown.29 Moreover, maternal COVID-19 infection is associated with severe adverse outcomes, i.e., preeclampsia or preterm birth.30 Importantly, these pre- and perinatal insults are considered as risk factors for psychosis according to a recent meta-analysis.31 Various mechanisms have been suggested to explain how maternal infection might disrupt the fetus brain development.32 First, multisystemic overload might alter structural and functional integrity of the placenta. Due to its dysfunctional permeability, pro-inflammatory cytokines and neuronal antibodies from the maternal circulatory system might interact and activate the immune system in the fetus.32 However, the neuroinvasive potential of the virus has been confirmed through olfactory pathway by retrograde axonal transport, but not in the fetus yet.33 Moreover, little is known about the influence of the SARS-CoV-2 on the fetal central nervous system but it is plausible that exposure in utero might disrupt its development.34
Importantly, subclinical and systemic inflammatory state occurs in the majority of patients with schizophrenia at various stages of illness.35,36 However, this phenomenon is not specific for patients with schizophrenia as it also appears in patients with other mental disorders, including major depression and bipolar disorder.37–39 Moreover, there is evidence that a certain subgroup of patients with schizophrenia does not show subclinical inflammation, suggesting the existence of interindividual variability with respect to the underlying pathophysiology.40 Nevertheless, it has been revealed that there are two types of markers with dynamics dependent on illness stage. First, state markers, including IL-1β, IL-6 and transforming growth factor-β, refer to those with the levels elevated only during psychotic exacerbations (first-episode or acute relapse of psychosis). Second, trait markers include cytokines with elevated levels regardless of illness stage, and include IL-12, soluble IL-2 receptor (sIL-2R) interferon-γ as well as TNF-α.41 On the other hand, there are also cytokines with increased levels only in patients with multi-episode, but not in first-episode, psychosis (e.g., IL-8, macrophage inflammatory protein-1β and eotaxin-1).42 However, measurements of peripheral cytokines may not directly reflect immunological mechanisms in the brain. Notably, cytokine alterations have also been investigated in the cerebrospinal fluid where elevated levels of IL-1β, IL-6, IL-8 and kynurenic acid as well as decreased levels of sIL-2R have been found in patients with schizophrenia compared to healthy controls.43 Moreover, transcriptome analysis has demonstrated the up-regulation of IL-23 signaling in the dorsolateral prefrontal cortex where the number of microglia is increased.44 Elevated activation of microglia has also been partially confirmed by the meta-analysis of neuroimaging studies in patients with schizophrenia.45 Similarly, psychosis is also considered as a process associated with altered blood brain barrier. Such dysfunction contributes to increased permeability to inflammatory cytokines circulating in the peripheral blood.46 Furthermore, ample evidence shows that neuroinflammation is linked to white matter pathology in patients with schizophrenia, including axonal degeneration, myelin breakdown or reduced density of oligo- and astroglia in some brain regions. Simultaneously, astroglia is responsible for glutamate transmission, which is involved in the pathophysiology of schizophrenia.47 Finally, pro-inflammatory processes cause reduced white matter volume and increased white matter neuronal density, especially in the orbitofrontal part of the brain.48
Severe infection of the SARS-CoV-2 can lead to rapid release of pro-inflammatory cytokines which is called “the cytokine storm”. It is the first-line response of innate immune system against the viral infection.49 As similar to subclinical inflammation in schizophrenia, it is related to increased levels of IL-1β, IL-6, TNF-α and other cytokines. In cases with the SARS-CoV-2 infection, increased level of CRP has been reported in more than half of patients with first-episode psychosis, and inflammation has been found to be the key pathogenetic factor.50 Accordingly, excessive release of cytokines might be destructive, leading to the apoptosis of lung epithelial and endothelial cells.51 Moreover, the SARS-CoV-2 has been found in the cerebrospinal fluid (CSF) and might directly affect the central nervous system. Interestingly, murine models inoculated by the SARS-CoV-1 are characterized by up-regulated levels of TNF-α, IL-1β, IL-6 in neurons and astrocytes. These cells express the angiotensin-converting enzyme 2 (ACE2) that is crucial for the SARS-CoV-2 invasion.52 However, further studies are required to verify if the SARS-CoV-2 may result in respiratory failure via infection of the medullary cardiorespiratory center in humans.33
Transcriptomic studies have revealed a number of pathways related to the COVID-19 that overlap with those that might be involved in the pathophysiology of schizophrenia in some patients. These include: cellular response to dopamine, IL-1 signaling as well as T-helper cell differentiation and immunological synapse formation.53 Additionally, altered tryptophan metabolism tends to appear both in schizophrenia and the COVID-19. In response to inflammation, there is an elevated level of kynurenic acid which acts as an anti-excitotoxic factor.54 Nevertheless, it is also considered to induce psychotomimetic effect as the NMDA receptor antagonist and increase the activity of the midbrain dopamine neurons.47 In parallel, it has been reported that the COVID-19 may induce psychosis, at least in some cases, through the development of the anti-NMDA receptor encephalitis according to the theory of molecular mimicry of the SARS-CoV-2.55,56 Interestingly, it has been shown that the activation of monocytes through the toll-like receptor 3 (TLR-3) and depletion of natural killer cells, which are associated with early antiviral response, appear both in schizophrenia and anti-NMDA receptor encephalitis.57,58 In the COVID-19, the TLR-3 pathway is linked to tissue-destructive senescence-associated secretory phenotype related to short- and long-term complications.59 These observations lead to the conclusion that subclinical inflammation observed in schizophrenia might make the patients more prone to develop severe course of the COVID-19.
Association between severity of COVID-19 and schizophreniaThere are several states that are associated both with the prevalence of schizophrenia and severe COVID-19 manifestation. Almost one third of patients with schizophrenia meet the criteria of metabolic syndrome, characterized by the co-occurrence of central obesity, high blood pressure, lipid profile disturbances and hyperglycaemia.5,60 In addition, patients with schizophrenia show high rates of cigarette smoking and, as a consequence, more often have reduced lung capacity in the course of chronic obstructive pulmonary disease.61,62 Moreover, there are various alterations of the hypothalamic–pituitary–adrenal axis response that include blunted cortisol awakening response, blunted cortisol response to stress and reduced mRNA levels of glucocorticoid receptors.63–65 Epidemiological studies have also revealed that specific autoimmune disorders and resulting drug-induced immunosuppression co-occur with schizophrenia.66 Nonetheless, there is limited number of studies analyzing the severity or mortality of the COVID-19 in patients with schizophrenia and metabolic syndrome or its elements with patients with schizophrenia but without metabolic problems. However, on the basis of a meta-analysis,10 it has been revealed that mortality from the COVID-19 in patients with schizophrenia cannot be fully explained by hypertension, diabetes and obesity. This observation was also confirmed by the recent large-scale retrospective cohort study conducted in 25539 individuals with schizophrenia.67 Interestingly, medical comorbidities have been associated with higher vaccination rates in patients with schizophrenia.8
A recent study by Goyal et al. revealed that patients with schizophrenia under the age of 55 years are more frequently admitted to intensive care unit (ICU) due to the COVID-19 than patients without a diagnosis of severe mental illness. This group was predominated by males with comorbidities. Therefore, young patients with schizophrenia should be treated as a group of special risk for which early intervention is important.68 On the other hand, patients with schizophrenia between the age of 65 and 80 had less ICU admissions but also higher risk of death than controls. However, this sample was overrepresented by females with co-occurring dementia.69 At this point it is important to note that hypoxia, a frequent state in the course of COVID-19, might worsen the dementia symptoms and increase the risk of aggressive behaviors in institutionalized patients.70,71 It is worth to emphasize the fact that ICU patients with schizophrenia have a higher risk of acute organ dysfunction and death, regardless of the reason for admission. Such findings have been associated with suboptimal physical care and delayed diagnosis in those patients related to inadequate training of the physicians, a deficient integration of the health system and insufficient help-seeking behavior of the patients.72
Altogether, these comorbidities that are more frequent in patients with schizophrenia are linked to the development of acute respiratory distress syndrome and death during the COVID-19 infection.73–75 This might lead to the conclusion that most common comorbidities in schizophrenia might be directly associated with worse outcome during the COVID-19. However, little is known about clinical and sociodemographic characteristics of patients with schizophrenia who are more prone to develop severe manifestation of the COVID-19. A recent meta-analysis by Ref. [10] demonstrated that older age and cigarette smoking are associated with higher COVID-19 mortality in patients with schizophrenia.
Psychosis onset during the COVID-19 pandemicIncreased stress is undoubtedly one of the effects of the pandemic and also a well-known trigger of psychosis. Moreover, teenagers and young adults might be more frequently exposed to severe family problems and domestic violence during the pandemic.76 This is important due to the fact that childhood trauma increases a risk of psychosis.77 Similarly, social restrictions favor transition from clinical high risk (CHR) state to overt psychosis.78 This might be explained by impaired stress tolerance in CHR individuals.79 There are numerous case reports of psychosis during the course of the COVID-19 or even related to the fear of the COVID-19 pandemic. At the beginning of pandemic patients with first-episode psychosis avoided professional care according to one cohort study.80 Overall, the incidence of first-episode psychosis increased during the pandemic in many countries, seemingly in the older group of people.81–83 Some of severe clinical cases were caused by the use of high doses of corticosteroids in the acute phase of illness. Furthermore, delirium should be considered in the differential diagnosis of these patients.84
However, little is known from cohort studies about the risk of psychosis after the SARS-CoV-2 infection. A large analysis of 2-year cohort studies of individuals with COVID-19 demonstrated transiently increased incidence rates of mood and anxiety disorders. Importantly, the authors noted that the increased risk of psychosis persisted over time.85 In turn, the most recent Mendelian randomization study found that genetic liability to hospitalized COVID-19, but not just SARS-CoV-2 infection, was associated with an increased risk for schizophrenia.86 All of these observations point to the fact that both the SARS-CoV-2 infection and social aspects of the pandemic are considered as important phenomena that might trigger the onset of psychosis. Nevertheless, longer observation periods are needed to provide unequivocal insights into causal associations.
The COVID-19 pandemic and clinical expression of psychosisSome studies, mainly case reports, have addressed specific manifestation of psychosis attributable to the SARS-CoV-2 infection or stress related to the pandemic. Specifically, the mean age of patients (43.9) was higher than expected for first-episode schizophrenia.87 In turn, other studies investigated the impact of the pandemic on psychopathology in patients with established diagnosis of schizophrenia. Patients with the SARS-CoV-2 infection have reported significantly more often visual hallucinations, confusion and an acute onset of illness, and less frequently depression or a delusional content related to the pandemic.50 Additionally, patients with schizophrenia more frequently reported delusional conspiracy theories and psychotic-like experiences associated with the COVID-19 crisis.88 For instance, they developed obsessional fear and delusions of infecting other people with the SARS-CoV-2 or being controlled by the virus.89,90 Delusions with the COVID-19 contents have also been reported in people experiencing first-episode psychosis.91 Currently, due to the change in the perception of schizophrenia, one of the major challenges is the diagnosis and treatment of negative symptoms. They include: alogia, blunted affect, anhedonia, avolition, and asociality.92 These symptoms often lead to social exclusion and job loss, which are particularly important during the economic uncertainty associated with the pandemic.93 Indeed, it has been shown that the level of negative symptoms in several domains might increase due to widespread environmental deprivation.20 Furthermore, it has been noticed that a lack of adherence to safety restrictions is related to more severe negative symptoms.15 It is important to note that deficit schizophrenia (characterized by primary and enduring negative symptoms) is more significantly associated with increased levels of IL-6, TNF-α than the non-deficit subtype which might be of importance to the association of schizophrenia with the course and outcome of the COVID-19.94
The treatment of psychosis in pandemic timesIt has been observed that taking antipsychotic drugs worsens the course of respiratory tract infections. This is due to sedation, decreased coughing and swallowing reflexes, excessive salivation, and decreased muscle tone in the pharynx or larynx (hypomotility).95 In the context of life-threatening coagulation abnormalities in severe COVID-19 cases, it is worth to mention that psychopharmacological treatment of schizophrenia has also been associated with increased coagulability. Procoagulant properties of antipsychotics might be related to their effects on the level of plasminogen activator inhibitor.96
Specific attention has been paid to clozapine. Clozapine is dedicated for patients with more severe clinical manifestation and treatment resistance. Due to a broad receptor profile, it might cause several side effects. Despite the fact of high efficacy of this drug (reduction of rehospitalizations, overall mortality and suicide risk), it is not used as the first-line treatment due to a risk of agranulocytosis.97 Nevertheless, it has been identified that even the three fourth of patients receiving clozapine during the pandemic period may not have access to blood count analysis.98 Importantly, absolute neutrophils count has been found to decrease in patients treated with clozapine during the SARS-CoV-2 infection.99 Clozapine also interferes with the immune system in other ways. Recently, it has been observed that clozapine significantly reduces immunoglobulin levels in comparison with other antipsychotics.100 Clozapine is metabolized by the CYP1A2, which is inhibited by pro-inflammatory cytokines (IL-1β, IL-6, TNF-α and IFN-α).101 The observational cohort study by Veerman et al. found that this effect might be of importance during the SARS-CoV-2 infection due to a risk of intoxication.102 However, a recent meta-analysis revealed that reduction of absolute neutrophil count (ANC) in patients treated with clozapine during COVID-19 is mild and transient.103 Moreover, clozapine is also associated with high risk of developing metabolic syndrome components that might potentiate risks associated with the COVID-19.104,105 Furthermore, the use of clozapine might increase a risk of community-acquired pneumonia, and this has also been confirmed in case of the COVID-19.106,107 Notably, patients treated with more than one psychotropic drug are at the highest risk of severe course and lethal outcome of the COVID-19.9 At this point it is important to note that clozapine is commonly combined with other antipsychotics, mostly long-acting injectable risperidone.98 The use of risperidone has been associated with immunosuppression and increased susceptibility to infections.108 Hence, the use of clozapine during the COVID-19 pandemic requires special caution and, if necessary, reducing the dose of the drug. Moreover, it is worth to emphasize that the Treatment Response and Resistance in Psychosis Working Group states that the frequency of ANC may be reduced to every 3 months in patients with continuous clozapine treatment for more than 1 year who have never had the ANC <2000/μL and have no safe or practical access to the ANC testing.109
Moreover, some antipsychotics, especially quetiapine, haloperidol, ziprasidone, levomepromazine might interact with antiviral and immunomodulatory drugs and result in the prolongation of the QT interval or Torsade de Pointes.110 There are also promising findings with respect to the use of some antipsychotics during the COVID-19 pandemic. For instance, aripiprazole seems to have beneficial potential in the treatment of patients with schizophrenia and the COVID-19. Indeed, one transcriptomic study indicated that aripiprazole might revert altered gene expression in some pathways related to the Th1, Th2 and Th17 differentiation, B-cell receptor and the NF-kappa B signaling pathways related to the SARS-CoV-2 infection.111 Also, one of the most recent studies on a relatively large population indicated that the use of paliperidone was associated with decreased odds of COVID-19.112 The recent meta-analysis has reported that exposure to antipsychotic and anxiolytic drugs (especially benzodiazepines) initiated before contracting COVID-19 in patients with severe mental disorders was associated with severe COVID-19 outcomes.113 In sum, it leads to the conclusion that even more caution should be taken in the use of antipsychotics now than before the pandemic times. Decisions should be taken on a case-by-case basis and circumspectly balanced. This might be of particular importance due to recent observations that almost 60% of patients with schizophrenia take medications during the pandemic from the pharmacy with a medicine report without prescription.98
The COVID-19 pandemic has hindered the possibilities of psychological treatment for patients with schizophrenia due to the development of specific restrictions and social distancing. However, the situation has provided grounds for the development and/or improvement of digital mental health interventions.114 It has been reported that patients with severe mental illness, including schizophrenia, did not differ from other patients in adapting to teletherapy, regardless of whether it was the transition from conventional, in-person therapy or the beginning of therapy via telehealth platforms.115 Furthermore, telemedicine interventions may improve adherence to treatment.116 Some of the forms of therapy used so far have been adapted to the teletherapy. For instance, group teletherapy for first-episode psychosis has gained high satisfaction ratings by patients. Such techniques are considered as non-stigmatizing by patients and support their interpersonal comfort. However, in the context of patients with psychosis, suspiciousness may be worsened by virtual contact in some cases.117 Moreover, the study of Metacognitive Insight and Reflection Therapy as an integrative treatment revealed promising results. It appeared to develop individual sense of psychiatric and social challenges that are being faced during the pandemic.114 Another study compared the efficacy of virtual reality therapy (VRT) and cognitive behavioral therapy (CBT) in treatment-resistant schizophrenia. Both methods were found to be beneficial in controlling auditory verbal hallucinations. On the other hand, patients after CBT reported more depressive symptoms while patients after VRT reported more anxious symptoms.118 A recent systematic review on the use of mobile health applications by people with schizophrenia also raises ethical considerations (privacy, confidentiality, and the potential to reconfigure the patient–physician relationship).119 Additionally, it should be noted that some patients have limited access to technology due to low socioeconomic status.120,121 However, in the case of pandemic restrictions, the use of online tools seems to be necessary to support a good therapeutic alliance and enhance recovery.
Conclusions and future directionsClinical perspectivesThe risk of COVID-19 among patients with schizophrenia depends on the severity of their disease, comorbidity and the degree of their functioning. Following these observations, it is imperative to highlight that increased mortality due to the COVID-19 in individuals with schizophrenia indicates the necessity to rethink our approach to primary and secondary prevention of comorbid cardiovascular disease in this population. Although it is now clearly apparent that individuals with schizophrenia are more likely to develop cardiovascular disease, several findings are alarming. These include the following observations: (1) screening for the presence of cardiovascular risk factors in people with severe mental illness, including schizophrenia, appears to be less frequent than it should be according to existing recommendations; (2) primary prevention after the identification of cardiovascular risk factors is less frequent in this population compared to people without severe mental illness in both the primary and secondary care settings; (3) specialized cardiovascular diagnostic and therapeutic procedures are initiated less frequently in people with severe mental illness; (4) apparent disparities exist in the rates of prescriptions for pharmacological treatments of physical diseases (for a comprehensive review see122). Adequate control of respiratory, cardiovascular and metabolic disorders is now perceived as the most important prophylactic measure of the COVID-19 mortality in people with schizophrenia.73 In this regard, integrated health care developed in specialized clinical settings needs to be provided. The existence of integrated health care settings in other medical specialties, e.g., in oncology, suggests that this approach might also be effective in decreasing mortality due to physical diseases, including the COVID-19, in people with schizophrenia.
The situation is particularly difficult in the pandemic times due to low adherence to psychiatric treatment.18 Taking into account all the mechanisms underlying consequences of the COVID-19 pandemic for patients with schizophrenia (see Figure 1 for summary), numerous failures in therapy are not surprising. In one cohort study, nearly 40% of patients had a relapse during the first year of the pandemic.98 Thus, it is worth to consider using long-acting injectable antipsychotics and remote healthcare in preventing discontinuation of treatment.123 Improvements in mental health policy through increasing finances for community care are required to ensure appropriate medical surveillance, prioritization in vaccination and to reduce disparities in this vulnerable population. A positive aspect is the increased emphasis on psychoeducation in the field of mental health nowadays, which reduces stigmatization and ensures a dignified life for patients, but this is still an insufficient scope of activities.124
In the outpatient care, special attention should be paid to CHR individuals and those who experience suicidal thoughts because additional stress related to the pandemic might result in unfavorable outcome. The psychiatric care and psychotherapy for stable patients can be carried out online successfully, as 70% of them were found to be willing for such a solution.98 On the other hand, patients hospitalized at ICU suffer from complications that worsen their long-term quality of life. Rehabilitation that allows to regain mental and physical health is especially recommended for patients with schizophrenia after severe COVID-19.125
Immune-inflammatory hypotheses and shared mechanismsViewed as a neuroinflammatory process, psychosis shares various immunological disturbances with the COVID-19 which might interfere and enhance complications of both conditions. However, it is important to note that biological mechanisms underlying the development of schizophrenia and their association with the COVID-19 morbidity and mortality remain largely unknown. Indeed, several biological alterations (including, i.e., subclinical inflammation) and comorbidities show some level of interindividual variability among patients with schizophrenia. Also, there is evidence that the COVID-19 pandemic might increase a risk of psychopathological responses that fall beyond the psychosis spectrum, e.g., depressive symptoms, anxiety and insomnia.87,126 Similarly, the outcome of the COVID-19 might differ between patients with schizophrenia.
Future studies focusing on animal models investigating immune-inflammatory hypotheses could provide valuable insights into the underlying mechanisms of both schizophrenia and COVID-19. Such studies can help to establish causality and identify potential targets for treatment. For instance, researchers could explore the effects of anti-inflammatory drugs on both conditions in animal models to determine their efficacy in reducing symptoms and improving outcomes. Moreover, the use of animal models can also help to better understand the complex interplay between genetic, environmental and lifestyle factors that contribute to the development of both conditions.127 On the other hand, progress in research based on human pluripotent stem cells technology and neural progenitor cells as viral infection models will shed further light on neurotropism of the SARS-CoV-2.128 Moreover, prospective birth cohort studies of offspring of women who suffered from COVID-19 during pregnancy will answer the question whether prenatal infection with the SARS-CoV-2 increases a risk of psychosis. Longitudinal monitoring of unaffected individuals and people with schizophrenia who developed COVID-19 will allow us to learn more about neuropsychiatric complications. Finally, long-term observations are needed to unravel the impact of the COVID-19 pandemic on the occurrence of psychosis spectrum disorders.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestsNone declared.