Optimising ventilation control in the anaesthetic process of electroconvulsive therapy (ECT) can be a method for improving the effectiveness and safety of some treatments. There are several approaches for inducing adequate therapeutic seizures in patients with medical co-morbidity or in those with high seizure thresholds, although all of them present limitations. A new approach is hyperventilation with laryngeal mask, a method that improves oxygenation, achieves hypocapnia, and lowers seizure threshold. Thus, hyperventilation with laryngeal mask could, hypothetically, be useful to decrease the energy needed to obtain adequate therapeutic seizures.
Material and methodsA randomised crossover study was conducted on 14 patients on maintenance ECT, using a laryngeal mask vs a facemask. When laryngeal masks were applied, the energy was reduced by 45% compared with the energy required when ventilated with facemasks (performed with standard dose).
ResultsThe results of the study revealed that, despite a 45% energy reduction with laryngeal mask, there were no significant differences in seizure length in either group.
ConclusionsThese results prompt us to propose ventilation with laryngeal mask as an alternative to decrease energy applied without lowering seizure times. This is a preliminary study with a small sample, which opens new lines of research. Larger samples and other measurements of seizure adequacy are needed in future studies, in order to study possible improvements in ventilation and minimising adverse effects of ECT, especially in patients with medical co-morbidities.
Optimizar el control de la ventilación en el proceso anestésico de la terapia electroconvulsiva (TEC) puede ser una forma de mejorar la efectividad y la seguridad del tratamiento. Existen varios métodos para inducir una convulsión terapéutica adecuada en pacientes con enfermedad médica comórbida o en aquellos con elevado umbral convulsivo, aunque todos presentan alguna limitación. Un nuevo abordaje es la hiperventilación con mascarilla laríngea, que produce una mayor oxigenación e hipocapnia, disminuyendo el umbral convulsivo. Este hecho puede, hipotéticamente, servir para disminuir la energía necesaria para obtener una convulsión terapéutica adecuada.
Material y métodosSe ha realizado un estudio piloto aleatorizado y cruzado con 14 pacientes en TEC de mantenimiento, utilizando mascarilla laríngea versus mascarilla facial. Las sesiones de TEC con mascarilla facial se realizaron con la energía estándar, mientras que en las sesiones de TEC con mascarilla laríngea se disminuyó la energía en un 45%.
ResultadosA pesar de la reducción del 45% en la energía aplicada con el uso de mascarilla laríngea, no se han encontrado diferencias significativas en la duración de la convulsión en ambos grupos.
ConclusionesCon estos resultados se podría proponer la ventilación con mascarilla laríngea como una alternativa para disminuir la energía aplicada sin repercutir en la duración de la crisis. Este es un estudio preliminar con una muestra pequeña, aunque abre nuevas líneas de investigación. Sería necesario aumentar la muestra y valorar otras medidas de calidad de las convulsiones en futuros estudios con el fin de estudiar sus efectos no solo en la dosis de energía necesaria, sino también en una posible mejora de la ventilación y una posible minimización de los potenciales efectos secundarios de la TEC, algo que sería relevante sobre todo en pacientes con comorbilidad médica.
The progress made over more than half a century in practicing electroconvulsive therapy (ECT) has made the technique safer and minimised its side effects. This progress has taken place in the use of anaesthesia, the characteristics of modern ECT equipment and the protocol for use of the therapy.1,2 In spite of this, some aspects of ECT require improvement. It is important to develop methods that are safer, simpler and more effective, to minimise adverse effects, especially cognitive ones.2,3 It is important to find new methods that increase the safety of ECT and minimise its side effects, especially for 2 types of patients: those with medical comorbidities and at high risk under anaesthesia, as well as outpatients in maintenance therapy.2,4–7
Each individual has a different convulsive threshold, and there is a wide range of variability in this respect.8–12 This is due to several factors (age, sex, electrode positioning, the use of psychoactive drugs, anaesthesia doses and type, the number of sessions, oxygenation and carbon dioxide levels, etc.). A high convulsive threshold may lead to a convulsion that is hardly effective, reducing the efficacy of the ECT13 and leading to more adverse effects.
The lack of suitable convulsions, even with the maximum permitted energy,10 is a common problem in clinical practice.13 Several different strategies exist to improve convulsions: electric methods such as changes in pulse amplitude, or in the frequency, intensity and duration of the same, as well as the position of the electrodes.14–17 Other methods seek to reduce the convulsive threshold,18 such as the suppression of benzodiazepines,19 the use of Ketamine as an anaesthetic,9 the addition of Remifentanil,20 light stimulation and muscle relaxants. Adenosine antagonists such as caffeine, theophylline and aminophylline have also been used, although they lead to cardiovascular complications among other risks.21 Another strategy is to use sleep deprivation,22 as this is accompanied by an increase in neuronal excitability. However, the complexity of this technique must be taken into consideration. The majority of the methods used increase side effects or are too complex to be applied in everyday clinical practice.
Hyperventilation gives rise to an increase in pO2 and a fall in CO2, and it may improve the quality of convulsions.20,21,23–25 Hyperventilation prior to electrical stimulation is known to lower the convulsive threshold, and 100% oxygenation is recommended.26 Hypocapnia prior to electrical stimulation is beneficial in preventing failed crises and improving the quality of convulsions.20,23,26,27 Hyperoxygenation-hypocapnia are associated with better convulsions.25,28
There are different methods of assisted mechanical ventilation. The one used the most in everyday clinical practice is ventilation using a face mask (FM). Another method is ventilation using a laryngeal mask (LM).
LM ventilation has been used in anaesthesia since the 1990s, especially for minor surgery, as it is less invasive than traditional intubation.23 A LM gives better management of the supraglottic airway in comparison with a FM, while at the same time it avoids the drawbacks of intubation. A LM is not invasive and may be inserted without any special equipment. It also provides better protection of the airway of the gastrointestinal tract and guarantees more effective ventilation when there are other associated variables, such as obesity or a neck anatomy that may interfere with ventilation. The complexity of managing anaesthesia and the economic cost of LM mean that it may be considered to stand half-way between the use of a FM and intubation.
Few publications exist about the use of a LM in ECT.6,23,29–31 All of them show LM to be safe and effective.
Nishihara et al.31 undertook a study of patients who fulfilled the criteria for difficult ventilation and had been treated using ECT. The patients were divided into 2 groups according to the type of ventilation control: one group with a LM and the other with a FM. The authors found that clinical convulsion time in the FM group was significantly shorter than it was in the LM group.
Haeck et al.23 suggested in their study that a LM could be a good method for controlling hyperventilation, obtaining a longer convulsion time and reducing confusional symptoms.
Published clinical cases were found in which a LM was considered necessary for ECT, with effective and safe results in spite of patient complexity. Brown et al.29 successfully used a LM in 8 sessions of ECT in a pregnant patient with difficulty for management of the airway. Martínez-Amorós et al.6 described the successful use of a LM in patients with pseudocholinesterase deficit. Chow30 used a LM in a 37 year old patient with a family history of malignant hyperthermia. These authors observed a possible reduction in the convulsive threshold due to better control of the PaCO2.
The use of a LM may therefore be a safe and effective method for ventilation in ECT. One of its potential advantages would be the possibility of improving the convulsive threshold with lower stimulus intensity.23,31
The main hypothesis of our study is that, in the same patient and due to the greater effectiveness of ventilation with a LM rather than a FM, less energy would be needed to achieve a similar convulsion time. We selected a 45% reduction in energy on the basis of previous studies23,30,31 and our preliminary personal experience.
Material and methodsA sample of 14 patients in the maintenance ECT programme (mECT) were included in the study. It was decided to include only patients in the mECT programme to minimise variability in the use of ECT for each patient, and to have a series of previous ECT sessions at stable doses of energy. All of the patients were in a stable situation in terms of pharmacological dose as well as the electrical stimulation used. The inclusion criteria were: psychopathological stability over the previous 3 months; evaluation and acceptance of the case by the anaesthetist (individual evaluation of ASA III patients and exclusion of ASA IV patients); acceptance of the study and signing of the informed consent form by the patient. The exclusion criteria were: abuse of alcohol and/or other toxic substances, except for the stable consumption of nicotine and caffeine; and changes in psychopharmacological treatment during the study. The study was approved by the local Ethics Committee and was undertaken according to the ethical standards set by the Helsinki Declaration and its subsequent modifications.
This is a crossed randomised study. For each patient 2 consecutive sessions of mECT were monitored, one with a FM and the other with a LM. The order of the two sessions (with FM vs LM) was randomised. Six patients commenced the study with a FM and 8 commenced with a LM. Previous ECT session were undertaken with the usual procedure of the centre, i.e., with a FM. All concomitant medication was kept stable during the study. The anaesthetic procedure was the same in all cases.
In the case of ECT sessions with facial ventilation, the energy used was predetermined according to the average of the previous 6 sessions, while for the LM a reduction of 45% in the dose of energy used in the same average measurement was given.
Anaesthesia was induced using intravenous Propofol (1mg/kg) and prophylactic intravenous atropine (0.01mg/kg). Intravenous Mivacurium was given (0.1mg/kg) instead of Succinylcholine (0.5mg/kg) to give better and prolonged conditions of muscular relaxation with the ventilation protocol used. This was so in the sessions of ECT with a FM and with a LM.
All of the patients in both experimental groups were preoxygenated with oxygen at 100% during 5min. before the induction of anaesthesia. To ensure better control, ventilation with positive pressure in “volume control” mode was used at 20rpm for 10ml/kg tidal volume during 3min. with Siemens® Servo 900C equipment. In both ventilation methods (FM and LM) there was a wait of 3min with each patient to guarantee proper exchange of their whole residual functional capacity, due to the 100% oxygen administered for inspiration (denitrogenised)32 and to give time for the neuromuscular blocker used (Mivacurium)to begin acting clinically.33 The electrical stimulation was applied just after this period, used MECTA® spECTrum 5000Q equipment, with the electrodes positioned bifrontotemporally (this positioning was carefully marked and the same position was always used for each patient). Convulsions were monitored using 2 recording channels, establishing the locations at a bilateral prefrontal and mastoid level. The equipment automatically makes an electroencephalographic record. The convulsion time, at a motor as well as a central level, was evaluated by the psychiatrists in the study.
Data analysisQuantitative variables are described as averages±standard deviation or a median or interquartile range. Due to the small size of the sample Wilcoxon's non-parametric test was used to analyse paired data in the comparison between ventilation using a LM or a FM. All analyses were conducted bilaterally and with a level of statistical significance of 0.05. The SPSS and R programmes were used for statistical analysis.
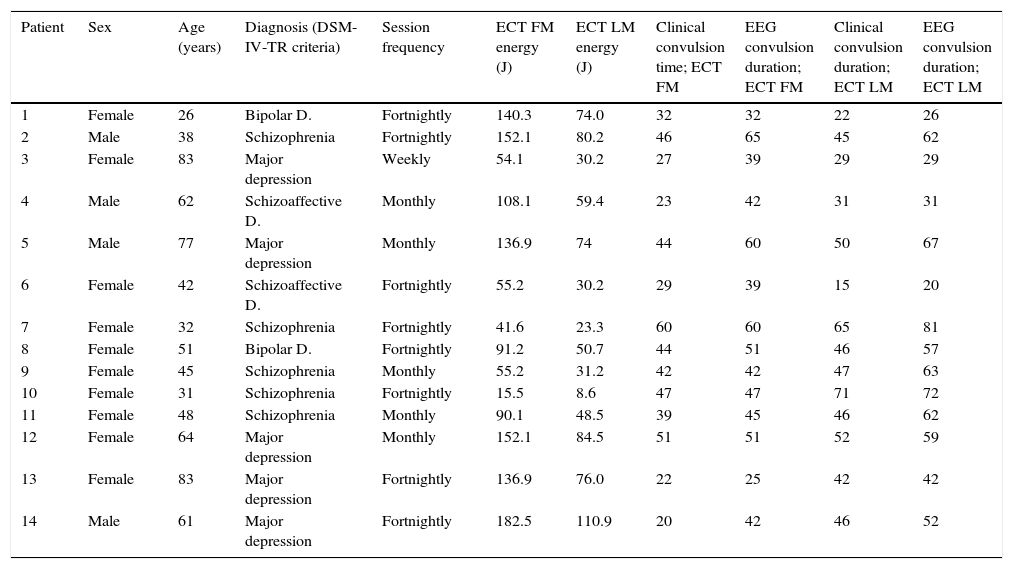
ResultsA total of 14 patients in mECT were studied (Table 1). The ratio of men to women was 4:10 (28.6 vs 71.4%). Participants’ ages varied from 26 to 83 years old, with an average age of 53.07 years old. The diagnoses of the patients were: schizophrenia in 5 patients, major depression in five others, bipolar disorder in 2 and schizoaffective disorder in the remaining 2. The average energy applied using a FM was 100.8J, and the average energy applied using a LM was 55.8J.
Characteristics of the sample.
| Patient | Sex | Age (years) | Diagnosis (DSM-IV-TR criteria) | Session frequency | ECT FM energy (J) | ECT LM energy (J) | Clinical convulsion time; ECT FM | EEG convulsion duration; ECT FM | Clinical convulsion duration; ECT LM | EEG convulsion duration; ECT LM |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 26 | Bipolar D. | Fortnightly | 140.3 | 74.0 | 32 | 32 | 22 | 26 |
| 2 | Male | 38 | Schizophrenia | Fortnightly | 152.1 | 80.2 | 46 | 65 | 45 | 62 |
| 3 | Female | 83 | Major depression | Weekly | 54.1 | 30.2 | 27 | 39 | 29 | 29 |
| 4 | Male | 62 | Schizoaffective D. | Monthly | 108.1 | 59.4 | 23 | 42 | 31 | 31 |
| 5 | Male | 77 | Major depression | Monthly | 136.9 | 74 | 44 | 60 | 50 | 67 |
| 6 | Female | 42 | Schizoaffective D. | Fortnightly | 55.2 | 30.2 | 29 | 39 | 15 | 20 |
| 7 | Female | 32 | Schizophrenia | Fortnightly | 41.6 | 23.3 | 60 | 60 | 65 | 81 |
| 8 | Female | 51 | Bipolar D. | Fortnightly | 91.2 | 50.7 | 44 | 51 | 46 | 57 |
| 9 | Female | 45 | Schizophrenia | Monthly | 55.2 | 31.2 | 42 | 42 | 47 | 63 |
| 10 | Female | 31 | Schizophrenia | Fortnightly | 15.5 | 8.6 | 47 | 47 | 71 | 72 |
| 11 | Female | 48 | Schizophrenia | Monthly | 90.1 | 48.5 | 39 | 45 | 46 | 62 |
| 12 | Female | 64 | Major depression | Monthly | 152.1 | 84.5 | 51 | 51 | 52 | 59 |
| 13 | Female | 83 | Major depression | Fortnightly | 136.9 | 76.0 | 22 | 25 | 42 | 42 |
| 14 | Male | 61 | Major depression | Fortnightly | 182.5 | 110.9 | 20 | 42 | 46 | 52 |
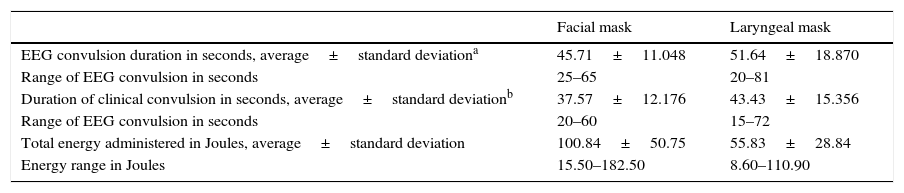
The average electric convulsion times were 45s for the FM and 51s for the LM. No significant differences were found between the two groups in terms of the convulsion time detected by the electroencephalogram (Wilcoxon's test for paired differences, with a value of P=.140) in spite of the 45% less energy administered in the LM ventilation group (Table 2). Nor were any differences found in connection with clinical convulsion times (37s with the FM vs 43s with the LM, P=.059), although there seems to be a tendency towards longer clinical convulsion times with LM ventilation.
Differences in the duration of electroencephalographic convulsion following ventilation with a facial or laryngeal mask.
| Facial mask | Laryngeal mask | |
|---|---|---|
| EEG convulsion duration in seconds, average±standard deviationa | 45.71±11.048 | 51.64±18.870 |
| Range of EEG convulsion in seconds | 25–65 | 20–81 |
| Duration of clinical convulsion in seconds, average±standard deviationb | 37.57±12.176 | 43.43±15.356 |
| Range of EEG convulsion in seconds | 20–60 | 15–72 |
| Total energy administered in Joules, average±standard deviation | 100.84±50.75 | 55.83±28.84 |
| Energy range in Joules | 15.50–182.50 | 8.60–110.90 |
Use of the LM was found to permit at least a 45% reduction in the energy applied by the MECTA® equipment, while keeping a similar duration of convulsion. No significant differences were found in convulsion times between the two groups of the sample studied.
Previous studies found that the use of a LM produces hypocapnia before electrical stimulation, leading to a longer duration of the crisis. These studies also found that hypocapnia before electrical stimulation may prevent an increase in intracranial pressure which in turn causes cephalea, a common side effect.23,27 Other studies find higher quality convulsions under hyperoxygenation and slight hypocapnia, showing that this may lead to a reduction in the energy to be applied.25
There is a known relationship between the dose of electrical stimulation and the appearance of side effects in ECT.34,35 Therefore, any method that has the purpose of reducing the energy applied without lowering the quality of the convulsion characteristics is of high interest in the practice of ECT, especially in the populations at highest risk.3
It has been said that suitable convulsions are not achieved in up to 5% of cases.10 The use of a LM may be considered to be a way of amplifying the crisis. Additionally, studies with LM have shown them to be safe in terms of anaesthetic parameters.6,23,29–31 In this context, it is of interest to consider using LM in patients with a high anaesthesia risk, given the higher level of oxygenation and the possibility of administering practically half of the dose of energy in comparison with FM.
When patients are in an acute phase repeated ECT sessions may raise the convulsive threshold, leading to the need to gradually increase the intensity of the stimulus applied. This gives rise to cognitive side effects, including confusional symptoms.1,2,11 On the other hand, it must be taken into account that patients in a mECT programme will return home after recovering from the anaesthesia. It is therefore of vital importance to prevent or minimise side effect in acute phases as well as during mECT.
Previous studies have used different individuals when making this comparison.23,31 Nevertheless, taking into account the high level of variability between different subjects and the fact that the convulsive threshold is individual, it is important to perform studies using paired data, where each patient is their own control, to reduce differences and confusion factors to a minimum.
This study proposes using LM as an alternative to increase hyperventilation, reduce the amount of energy applied and, probably, to minimise the potential side effects of the technique. However, the fact that this is a preliminary study must be taken into account. Although it opens new lines of research, it also has certain limitations that should be considered in future studies.
Firstly the sample is small, which is inherent in a pilot study, and we have tried to minimise the effect of this by using paired data analysis. New studies with broader samples will be necessary to corroborate the findings here. Secondly, it would be necessary to study not only the duration of crises but also the quality of the convulsion, especially in connection with the amplitude and ictal shape in the electroencephalogram.36,37 Thirdly, more studies with other anaesthetic agents which are less anticonvulsive than Propofol should be conducted.9,18,38 Fourthly, future studies would be justified by the need to study whether adverse effects and most especially cognitive ones really are reduced. And finally, it would be necessary to compare both procedures (LM vs FM) in connection with other aspects (the duration of the procedure, possible undesirable effects, and costs).
Based on this study it can be suggested that (at least with the MECTA® spECTrum 5000Q) 45% less energy be applied in patients ventilated using a LM, compared with the standard use of a FM.
We believe that ventilation using a LM may have three advantages: it ensures good ventilation, reduces possible adverse effects and achieves therapeutic convulsion with a lower dose of energy. Ventilation using a LM is a simple, safe and effective strategy to lower the convulsive threshold in patients with a high threshold.
We consider it to be highly interesting to be able to continue this line of research from an evidence-based viewpoint, as it is more effective and efficient than many other therapeutic strategies which are studied more and have larger research budgets.39 It would also be of interest to study it with a multidisciplinary approach, including the knowledge of psychiatrists and anaesthetists, with the aim of obtaining the best clinical results with the highest possible level of safety.18
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed are in accordance with the ethical norms of the responsible human experimentation committee and the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they followed the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors obtained the informed consent of the patients and/or subjects referred to in this paper. This document is held by the corresponding author.
FinancingThis work was partially financed by the Ministerio de Sanidad, Servicios Sociales e Igualdad, Instituto de Salud Carlos III (PI10/02535).
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank the clinical staff of the ECT Unit in the Hospital Universitario de Santa Maria-GSS.
Please cite this article as: Buj-Alvarez I, Pifarré J, Marco G, de Sousa-Duso M, Martínez M, López-Gómez J. ¿Puede tener un papel la mascarilla laríngea en la práctica de la terapia electroconvulsiva? Un estudio piloto. Rev Psiquiatr Salud Ment (Barc.). 2016;9:203–209.