A high comorbidity has been observed among attention-deficit hyperactivity disorder (ADHD) and categorical personality disorders (PD). A study is conducted on the dimensional traits associated with ADHD and PD, in order to determine whether there are any differences.
MethodologyA cross-sectional study was conducted on 78 outpatients attending a Mental Health Clinic in Arganda (Madrid) from January 2013 to June 2015. ADHD diagnosis was evaluated with the CAARS, the CAADID, and the WURS scales, and the PD with the SCID-II-DSM-IV questionnaire. None of the patients were receiving any stimulant or atomoxetine before the study, and all patients signed the informed consent before the study.
ResultsA high comorbidity was found with all PD clusters, especially with hyperactive and combined type ADHD. Depressive PD was associated with inattentive ADHD.
ConclusionsIn spite of using a questionnaire to evaluate PD, some differences can be observed between specific ADHD types and PD. More studies are needed to investigate dimensional personality traits in order to improve the diagnosis and therapeutics goals.
Se ha observado una alta comorbilidad entre el trastorno por déficit de atención e hiperactividad (TDAH) y categorías diagnósticas de trastornos de personalidad (tp). Los rasgos dimensionales del TDAH y de tp asociados están siendo investigados para descubrir si hay una diferenciación entre ambos trastornos o no.
MetodologíaSetenta y ocho pacientes ambulatorios que acuden al Centro de Salud Mental de Arganda (Madrid) fueron evaluados entre enero de 2013 y junio de 2015, en un estudio transversal. El diagnóstico de TDAH se realizó con las escalas CAARS, CAADID y WURS; el de los tp con el cuestionario del SCID-II-DSM-IV. Ningún paciente estaba tomando estimulantes ni atomoxetina previamente al estudio. Todos firmaron el consentimiento informado antes de participar en el estudio.
ResultadosSe encontró una alta comorbilidad con los 3 clusters de personalidad, especialmente con el tipo hiperactivo y combinado. El tp depresivo se asoció con el inatento.
ConclusionesA pesar de utilizar un cuestionario para evaluar los tp, vemos alguna diferenciación entre tipos específicos de TDAH y tp. Es necesario llevar a cabo más investigación sobre los rasgos de personalidad dimensionales para mejorar el diagnóstico y las metas terapéuticas.
Prior research has proven the existence of comorbidity between borderline personality disorder (BPD) and attention deficit hyperactivity disorder (ADHD) in adults. This has been determined through the use of questionnaires and structured psychological interviews: up to 60% of patients with BPD had ADHD criteria in childhood and 38% in adults. The symptoms of impulsivity and traits overlapped.1–8 It is not just BTD that is associated with ADHD in adults, other personality disorders (PD) of clusters B and C are too. Narcisstic PD and avoidance PD, are common.9–11 In the association of ADHD with PD, greater impulsivity was observed, a higher search for novelties, lower regulation of control over rage and a greater number of aggressive reactions.8,12,13
Other studies observed comorbidity with the 3 personality or cluster groups, with the risk of PD and lack of maturity of character increasing when in association with ADHD.14
Personality disorder dimensional orientation sought in the DSM-V classification proposes a model with 5 major personality dimensions: negative emotions or neuroticism; detachment; antagonism; lack of inhibition and psychoticism.15 Neuroticism is suggested to be a factor of general personality dysfunction which has an influence on many PD. It is characterised by emotional instability, impulsiveness and negative emotions. In this sense it is also associated with ADHD, when the underlying personality factors of this disorder are investigated.16–19 However, this dimensional focus is not the aim of this paper, which is the research of categorical comorbidity. Our initial hypotheses are that a high comorbidity of ADHD with the different PD exists and that when differentiating between the types of ADHD, it is the combined type which is associated with the 3 PD groups.
MethodA cross-sectional, observational study was conducted on 78 patients attending the Mental Health Clinic in Arganda (Hospital del Sureste) Madrid, with clinical diagnosis of ADHD. This was conducted between January 2013 and June 2015, and had the approval of the Investigation Committee of this hospital.
Inclusion criteria were: patients with depressive, anxiety, bipolar, and personality disorders, who had not used drugs within the last 6 months and who signed the consent form to participate in the study. All the patients who complied with the previous requisites had to have a positive ADHD diagnosis using the Conners’ Adult ADHD Rating Scale (CAARS) or the Conners Adult ADHD Diagnostic Interview for DSM-IV (CAADID).
The exclusion criteria were: psychotic symptoms, toxic abuse within the last 6 months, organic brain disorders and any clinically significant medical condition with psychological symptoms, mental impairment (IQ<70) or moderate to severe cognitive impairment and the inability to offer their informed consent or to comply with the assessment.
ProcedureThe patients are diagnosed as ADHD through interviews and specific tests which they attend themselves and with a family member who acts as the informing agent, usually the parents. They had not previously received any treatment with stimulants or atomoxetine.
ToolsThe diagnosis of adult ADHD was based on the CAADID interview and the self-administered, long version of the CAARS questionnaire.
CAADID: the Spanish version of the diagnostic interview (CAADID part II) was used for the diagnosis of ADHD.20,21 The CAADID is a semi-structured interview with 2 parts. The first is divided into 4 areas: demographic history, psychomotor development, risk factors and comorbidity. The second is administered by the practitioner to assess the ADHD criteria according to the DSM-IV.
CAARS: this was developed for the assessment and diagnosis of adult ADHD,22 in self-administered format and also informing agent format. The CAARS-Self-Report, Long Form comprises 4 subscales derived from factorial analysis: CAARS-A (inattention/problems with memory), CAARS-B (hyperactivity/restlessness), CAARS-C (impulsivity/mood swing) and CAARS-D (problems with self image); 3 symptomatic subscales of the DSM-IV (4th ed., DSM-IV; American Psychiatric Association, 1994): CAARS-E (symptoms of inattention DSM-IV), CAARS-F (hyperactive-impulsive symptoms DSM-IV) and CAARS-G (total symptoms); an ADHD index (to identify probable ADHD), and an index of inconsistency for random or unreliable responses. This long version contains 66 items, on a five-point Likert scale, which sums up the 8 subscales. We consider a score of >55 as positive diagnosis.
WURS: the reduced version of the Wender-Utah23 assessment scale is used to verify the existence of the ADHD symptoms in childhood, according to a retrospective self-assessment of the patient. A family member of the patient does this, in particular the parents. We use a cut-off point of >46.
Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II).24 for PD diagnosis we usually use the version validated into Spanish of the SCID-II, a semi-structured interview to assess the PD in accordance with DSM-IV criteria. The reliability between examiners varied between k=0.37 and 1, depending on the type of PD. The global kappa scale was of 0.85. For this work we used the questionnaire instead of the interview. This is usually used in the PD which tested positive in the questionnaire.
Statistical analysisData is expressed as frequencies and percentages or as means. The association between qualitative variables is studied with the chi-square and exact Fisher test. All statistics are bilateral and have a p value of <0.05 which is considered statistically significant.
The statistical programme used for all calculations was the IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, U.S.A.).
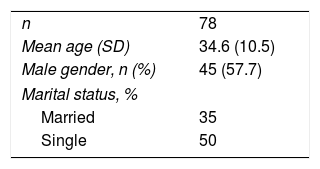
ResultsTable 1 shows the socio-demographic data of the study patients: 58% were male, with a mean age of 35 and half of them were single.
We observed a high comorbidity with PD using the before-mentioned SCID-II questionnaire: 94% with BPD, 78% with obsessive PD, 73% with narcisstic PD, 64% with passive-aggressive PD, 64% with depressive PD, 60% with avoidance PD, 53% with paranoid PD, 51% with schizotypal PD, 35% with dependent PD, 33% with antisocial PD, 26% with schizoid PD and 11% with histrionic PD.
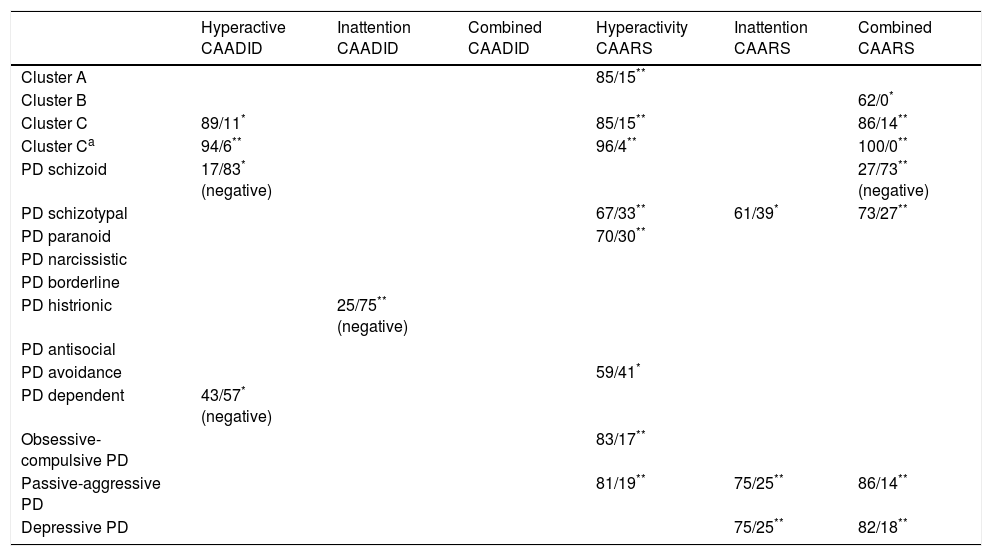
Table 2 shows the results of the search for possible specific association with the personality groups or clusters (A, B and C, including the passive-aggressive PD within this last group), with the respective types of ADHD which tested positively in the CAARS or the CAADID questionnaires.
Associations of ADHD with personality trait according to the CAARS and CAADID scales.
| Hyperactive CAADID | Inattention CAADID | Combined CAADID | Hyperactivity CAARS | Inattention CAARS | Combined CAARS | |
|---|---|---|---|---|---|---|
| Cluster A | 85/15** | |||||
| Cluster B | 62/0* | |||||
| Cluster C | 89/11* | 85/15** | 86/14** | |||
| Cluster Ca | 94/6** | 96/4** | 100/0** | |||
| PD schizoid | 17/83* (negative) | 27/73** (negative) | ||||
| PD schizotypal | 67/33** | 61/39* | 73/27** | |||
| PD paranoid | 70/30** | |||||
| PD narcissistic | ||||||
| PD borderline | ||||||
| PD histrionic | 25/75** (negative) | |||||
| PD antisocial | ||||||
| PD avoidance | 59/41* | |||||
| PD dependent | 43/57* (negative) | |||||
| Obsessive-compulsive PD | 83/17** | |||||
| Passive-aggressive PD | 81/19** | 75/25** | 86/14** | |||
| Depressive PD | 75/25** | 82/18** |
PD: personality disorder.
Data are presented as percentages of yes/no. Cluster A, B and C: from the axis ii of the DSM-IV.
Here we observe how the hyperactive type of ADHD is more associated with cluster A of PD and with C. And the combined type with cluster C and B (tendency to significance). If we look at the PD individually with the types of ADHD, it is of note that: they test negative with schizoid PD (with hyperactivity and combined), histrionic (with inattention) and dependent (with hyperactivity). In other words, the schizoid, histrionic and dependent PDs are less frequent in these patients with ADHD. The inattentive type is more associated with depressive PD and passive-aggressive PD, although we also see this PD in the combined and hyperactive types. The hyperactive type is more specifically associated with paranoiac, avoidance and obsessive PD. However, as we have already seen it is also associated with schizotypal and passive-aggressive PD. The combined type is associated with schizotypal, passive-aggressive and depressive PD.
On inclusion of depressive PD within cluster C no significant associations with any type of ADHD were observed.
DiscussionWe confirmed that the hypothesis of high comorbidity of patients with adult ADHD and PD is present. It is also true that it is higher than in the literature, possibly as a result of the use of the SCID-II questionnaire, instead of the interview as false positives may increases. We agree with the high comorbidity with BPD, narcissistic, obsessive and avoidance PD. Other studies also present high comorbidity with PD, more with cluster C than with B.10,11,25 Similarly to our study, where we observed higher frequency of BPD, in the National Epidemiologic Survey on Alcohol and Related Conditions –NESARC–26 in U.S.A., from 2004 to 2005, the most frequent PD were from cluster B and the schizotypal PD (33.7% BPD, 25.2% narcissistic).
The other hypothesis we considered was the higher association of PD with the combined type of ADHD: we see how in cluster C and A these are more associated with the hyperactive ADHD, cluster B with combined (tendency to significant) and cluster C too with combined ADHD. We observed no association of specific PD as cluster with inattentive ADHD.
If we focus inside each cluster: inattention is associated with depressive PD and passive-aggressive PD, and in a negative sense, with histrionic PD. Schizoid PD shows a negative association with combined ADHD and the obsessive PD with hyperactive ADHD in the positive sense. Other authors also found there was an association with cluster C and the passive-aggressive PD with the emotional disorder type ADHD (combining ADHD in 2 types, emotional disorder and inattention, with the former including the hyperactive type of PD) and cluster A regardless of any type of ADHD.27,28 We also agreed with the association between the combined type and several PD: in other studies the combined type is more frequently associated with ADHD with mood disorders, with anxiety, substance dependence and obsessive PD, passive-aggressive, narcissistic and BPD disorders.9,10
ADHD has been conceptualised as an extreme and maladaptive temperament and/or personality traits,29 but the true scope of this association is unknown. Personality dimensions, PD, neuropsychology and comorbidity diagnosed in the clinical evolution of both disorders overlap.30
We agree with this theory, in view of the high comorbidity of the adult ADHD with PD, despite having used the SCID-II questionnaire.
The BPD was investigated in its dimensions: high neuroticism and low responsibility rates were found, according to the Costa et al. model and the 5 personality traits.31 In 2011 Laporte et al. showed that the temperamental traits of neuroticism, problems of intimacy and impulsivity were predictors of the severity of BPD.32 In a different study we analysed ADHD and PD dimensions and found high rates of neuroticism and low rates of responsibility (Irastorza et al., pending publication).
In 2010, in a sample of patients with BTD, Ferrer et al.6 found 38.1% of ADHD, with a higher rate of substance dependence, antisocial and obsessive PD. In contrast to our study, they only observed patients with avoidance PD in the BTD without ADHD. They support a more impulsive profile in association between BTD and ADHD.
To conclude, we have observed that adult ADHD has a high comorbidity with PD. Due to the limitation of possible false positives, we added greater diagnostic specificity as an advantage when we used 2 tools for measuring hyperactivity, attention deficit and the combined disorder type. This, and hyperactivity are more associated with PD, with inattention being more frequent with depressive and passive-aggressive PD.
Further steps need to be taken to seek the personality dimensions of the PD in its association with ADHD, particularly given the high overlapping of both disorders in adults. In so doing improvements could be made to diagnostic value and possible therapeutic goals.
Ethical responsibilitiesProtection of people and animalsThe authors declare that the procedures followed comply with the ethical regulations of the corresponding committee for human experimentation and the World Medical Association and Declarations of Helsinki.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in this article. This document is in the possession of the corresponding author.
Conflict of interestsThere was no conflict of interests in this study.
Please cite this article as: Irastorza Eguskiza LJ, Bellón JM, Mora M. Comorbilidad de trastornos de personalidad y trastorno por déficit de atención e hiperactividad en adultos. Rev Psiquiatr Salud Ment (Barc). 2018;11:151–155.