The pandemic caused by the SARS CoV-2 virus has resulted in a world-wide emergency and has transformed our system of healthcare attention in a very short time.1 One of the measures adopted to contain the virus has been to restrict access to health centres. This has caused the cancelation, partial or total, of the face-to-face, on-site practice sessions for health sciences students. This restriction has also catalysed the potential of telemedicine: in just these few months, telemedicine has already become routine in general healthcare and mental health care as well.2
Although on-site practice sessions involve irreplaceable components for health sciences students, the current crisis has made us reconsider adapting teaching methods and management systems for on-site sessions in our setting. In the different mental health schemes associated with our Department of Psychiatry, we receive undergraduate and post-graduate health sciences students from various disciplines (Medicine, Psychology, Nursing, Social Work and Occupational Therapy). On-site practice sessions are organised into rotations of groups of from 5 to 10 students, with a set duration in hours and an order pre-established at the beginning of the course. Students have a tutor who is a clinical health professional, have specific learning objectives established and are evaluated at the end of the practice session period.
The model for on-site practice sessions that we are currently using clashes with the public health recommendations as to the circulation of people in healthcare centres. That is why we are proposing a digital transformation of clinical practice sessions based on decentralised management and the possibility of carrying them out with measures based on telemedicine.
In this paradigm shift, the teaching staff offers learning opportunities throughout the course, not just limited to a pre-set period or checkerboard plan. The learning opportunities are aligned with the educational objectives established for the practice sessions and are assigned credits corresponding to the hours required.
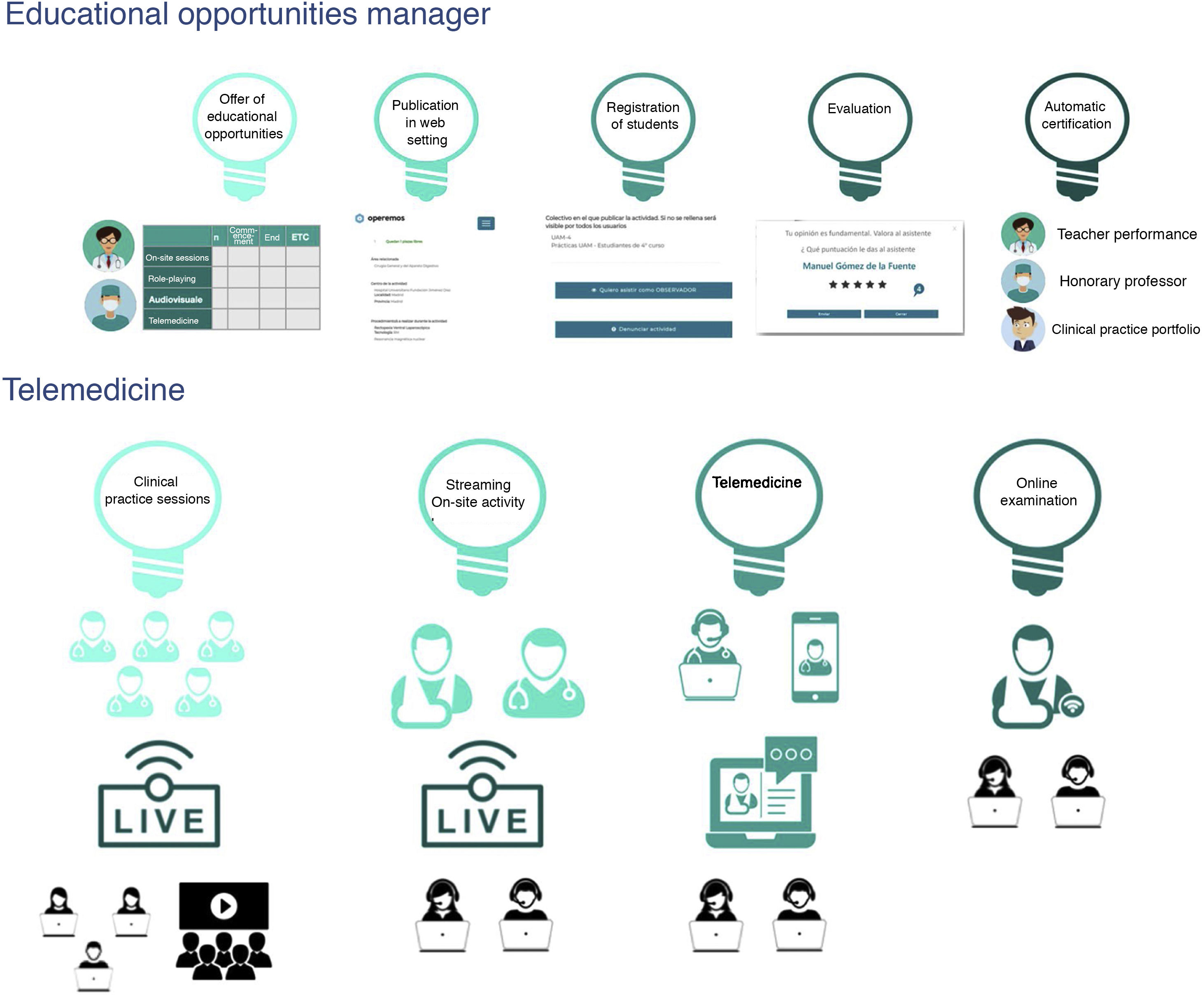
For this model, we use a platform that operates as a manager of educational opportunities (https://www.operemos.es). The platform makes it possible to (Fig. 1):
- •
Publish the educational opportunity, specifying its modality: on-site, simulation (role-playing), audio-visual (clinical material videos) or telemedicine. The educational opportunity lasts a specified period in hours — with its equivalence in European Credit Transfer System (ECTS) credits — and timetable, which may take place over several days).
- •
The students sign up at will until full capacity has been reached and the maximum number of hours/credits corresponding to the subject are completed.
- •
Student activities are not limited to a fixed schedule or a clinical practice group. Instead, students can customise their clinical practice portfolio using the educational opportunities offered throughout the year.
- •
At the end of the activity, the teacher and the student evaluate each other reciprocally using a valuation scale that ranges from 1 to 5.
- •
The system credits both the teacher and the learner with their participation and the evaluation received and specifies how much the teacher facilitated real-time information in the activities carried out.
The clinical practice sessions using telemedicine that we propose include the following (Fig. 1):
- •
Transmission of the clinical practice sessions and therapy group meeting by streaming.
- •
Transmission of the professor’s on-site clinical activity by streaming, using rooms with cameras and microphones, as well as portable emission equipment (smart glasses).
- •
The role of observer (hidden or not) in telemedicine activities (video-consultation, virtual groups).
- •
Interviews with and examination of patients using video-consultation.
We realise that dilemmas can arise with this paradigm shift. On the one hand, there is the resistance to change, the transformation of a scenario in which both students and teaching staff feel comfortable. Secondly, the matter of privacy and patient intimacy is especially pertinent. That is why we understand that this type of practices has to be adapted for professors, students and healthcare professionals, following Ellaway’s3 professional digital principles. It is important to emphasise that the students have to sign a commitment before accessing the clinical practice sessions, a commitment that specifically states that recording or sharing the activities seen, in all or in part, is prohibited.
To sum up, in the face of the restrictions that the COVID-19 pandemic has imposed on the on-site clinical practice sessions in health sciences, we propose a flexible model of clinical practice sessions and their management that also provides added value. We suggest an immersion model for the students in the healthcare practice of telemedicine that encourages tutored self-management and facilitates continuous evaluation of teachers and students.
This education that we have called fluid, following Bauman,4 eliminates checkerboard schedules and facilitates distance learning. In comparison to an exclusively on-site offer, fluid education improves accessibility and increases the quality of educational offer. The following key points are noteworthy:
- ‐
The curriculum becomes more flexible and adaptable to the needs of the various settings and activities in which clinical practice can be developed in mental health.
- ‐
The teaching staff optimise their educational opportunities and possibilities, while obtaining better follow-up and recognition of their teaching activity.
- ‐
The management organisms of the university have the possibility of better quality and more closely monitored educational activity.
All of these proposals are realities in our instructional endeavours. The proposals do not compete with the practical teaching that has been used for over 50 years in our centre, they complement it. We believe that we are facing an opportunity for innovation, complementing what now exists, so that the students and teachers have new tools available to improve their training and deal with future challenges.
FundingThis research has not received specific funding from public sector, commercial or non-profit agencies.
Conflict of interestsHéctor Guadalajara is the designer of the website www.operemos.es. The other authors have no conflicts of interest to declare.
None.
Please cite this article as: Ovejero S, Barrigon ML, Guadalajara H, Pérez-Santos E, Baca-Garcia E. El COVID-19 y la educación de profesionales sanitarios en salud mental: desafíos en la enseñanza práctica. Rev Psiquiatr Salud Ment (Barc). 2021;14:119–121.