The phenomena of depersonalisation/derealisation have classically been associated with the initial phases of psychosis, and it is assumed that they would precede (even by years) the onset of clinical psychosis, being much more common in the prodromal and acute phases of the illness. The aims of the present study are to analyse the differences in depersonalisation/derealisation between patients with initial and multiple episodes and the factors that could influence this.
Material and methodsA descriptive, controlled and cross-sectional study of 48 patients diagnosed with paranoid schizophrenia (20 with an initial episode and 28 with multiple episodes). These patients were assessed using scales such as the Cambridge Depersonalization Scale, the Positive and Negative Symptom Scale, and the Dissociative Experiences Scale.
ResultsParticipants with initial episodes score higher on both the Cambridge Depersonalisation Scale, and the subscale of the Dissociative Experiences Scale that evaluates such experiences. There were no associations between these types of experience and the positive symptoms subscale of the Positive and Negative Symptom Scale.
ConclusionsDepersonalisation/derealisation experiences appear with greater frequency, duration and intensity in patients in the early stages of the illnesses, gradually decreasing as they become chronic.
Los fenómenos de despersonalización/desrealización se han asociado clásicamente con las fases iniciales de la psicosis y se supone que precederían (incluso en años) a la psicosis clínica, siendo mucho más frecuentes en la fase prodrómica y en la fase aguda de la enfermedad. Los objetivos del presente estudio son analizar las diferencias para los fenómenos de despersonalización/desrealización existentes entre los pacientes con primeros o con múltiples episodios de esquizofrenia y los factores que podrían influir en ello.
Material y métodosEstudio descriptivo, controlado y transversal en el que se estudiaron 48 sujetos diagnosticados de esquizofrenia paranoide (20 con un primer episodio y 28 con episodios múltiples). Fueron evaluados mediante la Escala de Despersonalización de Cambridge, la Escala de los Síndromes Positivo y Negativo y la Escala de Experiencias Disociativas, entre otras.
ResultadosLos sujetos con primeros episodios de esquizofrenia presentan mayores puntuaciones tanto en la Escala de Despersonalización de Cambridge como en la subescala que valora estas experiencias en la Escala de Experiencias Disociativas. No encontramos asociaciones entre estas y la subescala de síntomas positivos de la Escala de los Síndromes Positivo y Negativo.
ConclusionesLas experiencias de despersonalización/desrealización aparecen con mayor frecuencia, duración e intensidad en pacientes con primeros episodios de esquizofrenia que en pacientes con múltiples episodios de la enfermedad.
Depersonalisation consists of an alteration in perception or in experience itself, causing the individual to feel detached and distant, as if he or she were an external observer of their body or of their own psychological processes.1,2 The main psychopathological features of depersonalisation are the feeling of being foreign to surroundings, feelings of automation, self-observation, emotional alterations, alterations in body image and alterations in the experience of time.1
From the first descriptions by Krishaber and Dugas towards the end of the 19th century, various theories have been proposed to explain it: alterations in perception, memory, emotions and body image and primary modifications of the conscience of the self. Clinically, depersonalisation can present as an independent category (depersonalisation disorder) or as a symptom of other psychiatric and neurological disorders.3
Various authors have pointed out the presence of depersonalisation in schizophrenia, especially during the prodromal and acute phases of the disease,4–9 while it seems rare in chronic schizophrenia.10 Likewise, depersonalisation has been included among what are called the basic symptoms of schizophrenia11; it is a phenomenon that often precedes (even by years) the appearance of the psychosis.
Depersonalisation may not be so specific to schizophrenia as it is a general feature of prepsychotic stages, independently of their aetiology.2 Several researchers have found that, in the evolution of a psychotic episode, the experiences of prodromal depersonalisation are integrated into the emerging delusions, a process called “psychotic re-personalisation”.2 Classical authors observed a fluid transition from typical depersonalisation to the delusional elaboration of the same experiences in the prodromal stage.4,12–14 For Fish,15 depersonalisation is also a frequent symptom during schizophrenia onset, but one that rapidly evolves towards a delusional character. This would demonstrate that some delusions would be based on the experiences of depersonalisation and that this would serve as an “experiential substrate”; this substrate, modulated by various cognitive frameworks, would crystallise into different delusional phenomena.16
Studies that analyse the relationship between depersonalisation and schizophrenia directly are not abundant. Brauer et al.,17 in 1970, pointed out the high percentage of experiences of depersonalisation in patients with schizophrenia.17 The results of an international pilot study on schizophrenia indicated that the presence of depersonalisation constituted a good prognostic marker for non-hebephrenic schizophrenia.18 In 2002, Maggini et al.19 found that the presence of depersonalisation was linked to a different clinical profile, with greater cognitive compromise, depression, alexithymia and poorly adaptive reaction to stress.
However, from the psychoanalytical perspective, some authors have raised the question whether depersonalisation represents a mild form of schizophrenia.20–23 This is difficult to validate empirically and is based on circular reasoning; that is, the psychodynamic explanations of depersonalisation are derived from psychodynamic models of schizophrenia.
The objective of this study was to analyse whether there were differences in the experiences of depersonalisation between patients with first and multiple episodes of schizophrenia.
Material and methodsThis was a transversal, descriptive, controlled study. The Committee on Ethics at the Hospital Universitario Reina Sofía de Córdoba (Spain) approved its protocol. The study fulfils the principles of the Declaration of Helsinki.
ParticipantsA total of 48 subjects belonging to the mental health area of Cordoba were assessed for the period from 2009 to 2012. The sample consisted of men and women between 18 and 50 years of age, diagnosed with paranoid schizophrenia according to the criteria of the DSM-IV-TR. Subjects with severe brain lesions, mental retardation, neurological disease and/or severe sensory alterations that prevented assessment were excluded. The final total sample was divided into 2 groups, 1 called first psychotic episode (n=20) and the other, multiple psychotic episodes (n=28). The first were included once the diagnosis of schizophrenia had been confirmed.
The participants were assessed during admission to the Hospitalisation Unit after the acute process had been stabilised. That is, once there was a decrease in the psychopathological symptoms and alterations in behaviour (such as anxiety, agitation, hostility or lack of collaboration) preventing administration of the scales or distorting their results. All the patients gave their written consent prior to being included in the study. The clinical and sociodemographic data were obtained through semi-structured interviews carried out by the researchers.
Assessment instrumentsCambridge Depersonalisation Scale (CDS).24 This questionnaire consists of 29 items, each composed of 2 scales with Likert-type scores (frequency and duration). Their sum provides a total score showing the strength of the experiences. In this study, we used the Spanish version25 of the instrument, with a total Cronbach's alpha of 0.94, using a cut-off point of 71. Sierra et al26 pose a factorial model that explains 73.3% of the variance, with extraction of 4 factors: anomalous body experience (Items 24, 15, 20, 27, 23, 3, 6, 11 and 8), emotional numbing (Items 25, 28, 7, 9, 18 and 10), anomalous subjective thoughts (Items 16, 14, 19, 21 and 17) and unreality of surroundings (Items 1, 13, 5 and 2).
Dissociate Experiences Scale (DES)27 in its version validated in Spanish,28 with a Cronbach's alpha of 0.91. This instrument is a 28-item visual analogue scale, with each item having 3 dimensions: absorption, amnesia and depersonalisation/derealialisation. Simeon et al.29 demonstrated the possibility of using the depersonalisation/derealialisation dimension as screening for the disorder.
Lastly, we also used the validated Spanish versions of the Positive and Negative Syndrome Scale (PANSS),30,31 the Beck Depression Inventory, the Hamilton Anxiety Rating Scale and the Mood Introspection Scale-Extended.
Data analysisThe data were analysed using the Statistics Pack for Social Sciences (SPSS version 20). In the first stage, descriptive analyses of the sociodemographic and clinical characteristics of the total sample and both groups separately were carried out. To compare variables, we used the Mann–Whitney U test for independent samples; this test was chosen because the groups had a sample size less than 30 and the test for normality (Kolmogorov–Smirnov) showed a non-normal distribution for some of the scores, unless the opposite was specified. Differences were considered statistically significant at P<.05. The evaluation of the association between the CDS scale and the rest of the instruments used in the study was performed with the Pearson correlation test.
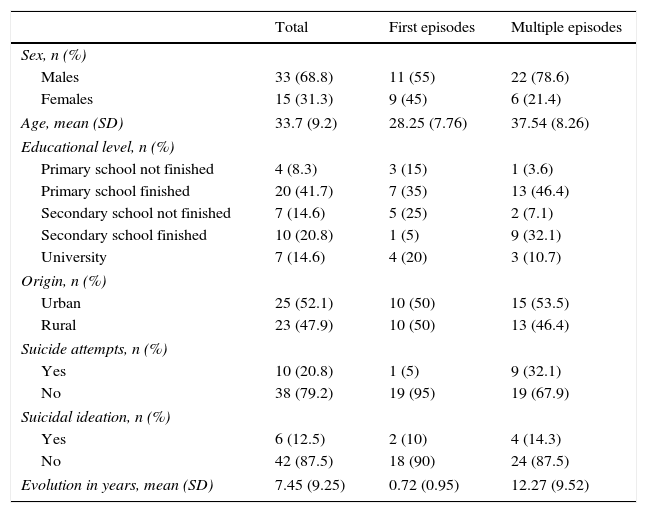
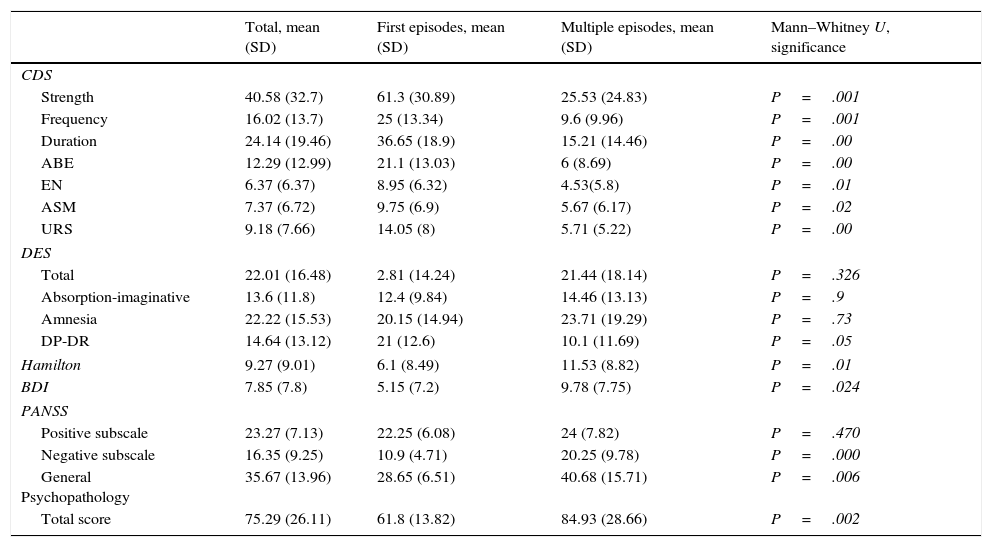
ResultsTable 1 presents the descriptive statistics for the sociodemographic variables gathered, for both the total sample and for both groups separately. Table 2 presents the descriptive statistics for the CDS and DES scales, Hamilton Anxiety Scale, Beck Depression Inventory and the PANSS.
Sociodemographic characteristics of the study sample.
| Total | First episodes | Multiple episodes | |
|---|---|---|---|
| Sex, n (%) | |||
| Males | 33 (68.8) | 11 (55) | 22 (78.6) |
| Females | 15 (31.3) | 9 (45) | 6 (21.4) |
| Age, mean (SD) | 33.7 (9.2) | 28.25 (7.76) | 37.54 (8.26) |
| Educational level, n (%) | |||
| Primary school not finished | 4 (8.3) | 3 (15) | 1 (3.6) |
| Primary school finished | 20 (41.7) | 7 (35) | 13 (46.4) |
| Secondary school not finished | 7 (14.6) | 5 (25) | 2 (7.1) |
| Secondary school finished | 10 (20.8) | 1 (5) | 9 (32.1) |
| University | 7 (14.6) | 4 (20) | 3 (10.7) |
| Origin, n (%) | |||
| Urban | 25 (52.1) | 10 (50) | 15 (53.5) |
| Rural | 23 (47.9) | 10 (50) | 13 (46.4) |
| Suicide attempts, n (%) | |||
| Yes | 10 (20.8) | 1 (5) | 9 (32.1) |
| No | 38 (79.2) | 19 (95) | 19 (67.9) |
| Suicidal ideation, n (%) | |||
| Yes | 6 (12.5) | 2 (10) | 4 (14.3) |
| No | 42 (87.5) | 18 (90) | 24 (87.5) |
| Evolution in years, mean (SD) | 7.45 (9.25) | 0.72 (0.95) | 12.27 (9.52) |
SD: standard deviation.
Scores obtained for the different scales in each group.
| Total, mean (SD) | First episodes, mean (SD) | Multiple episodes, mean (SD) | Mann–Whitney U, significance | |
|---|---|---|---|---|
| CDS | ||||
| Strength | 40.58 (32.7) | 61.3 (30.89) | 25.53 (24.83) | P=.001 |
| Frequency | 16.02 (13.7) | 25 (13.34) | 9.6 (9.96) | P=.001 |
| Duration | 24.14 (19.46) | 36.65 (18.9) | 15.21 (14.46) | P=.00 |
| ABE | 12.29 (12.99) | 21.1 (13.03) | 6 (8.69) | P=.00 |
| EN | 6.37 (6.37) | 8.95 (6.32) | 4.53(5.8) | P=.01 |
| ASM | 7.37 (6.72) | 9.75 (6.9) | 5.67 (6.17) | P=.02 |
| URS | 9.18 (7.66) | 14.05 (8) | 5.71 (5.22) | P=.00 |
| DES | ||||
| Total | 22.01 (16.48) | 2.81 (14.24) | 21.44 (18.14) | P=.326 |
| Absorption-imaginative | 13.6 (11.8) | 12.4 (9.84) | 14.46 (13.13) | P=.9 |
| Amnesia | 22.22 (15.53) | 20.15 (14.94) | 23.71 (19.29) | P=.73 |
| DP-DR | 14.64 (13.12) | 21 (12.6) | 10.1 (11.69) | P=.05 |
| Hamilton | 9.27 (9.01) | 6.1 (8.49) | 11.53 (8.82) | P=.01 |
| BDI | 7.85 (7.8) | 5.15 (7.2) | 9.78 (7.75) | P=.024 |
| PANSS | ||||
| Positive subscale | 23.27 (7.13) | 22.25 (6.08) | 24 (7.82) | P=.470 |
| Negative subscale | 16.35 (9.25) | 10.9 (4.71) | 20.25 (9.78) | P=.000 |
| General Psychopathology | 35.67 (13.96) | 28.65 (6.51) | 40.68 (15.71) | P=.006 |
| Total score | 75.29 (26.11) | 61.8 (13.82) | 84.93 (28.66) | P=.002 |
ABE: anomalous body experience; ASM: anomalous subjective memories; BDI: Beck Depression Inventory; CDS: Cambridge Depersonalisation Scale; DES: Dissociative Experiences Scale; DP-DR: depersonalisation/derealialisation; EN: emotional numbing; PANSS: Positive and Negative Syndrome Scale; SD: standard deviation; URS: unreality of surroundings.
The Mann–Whitney U test for independent samples showed statistically significant differences for the CDS scores and the depersonalisation/derealialisation dimension of the DES. As for the CDS, it is of note that the group of first episodes of schizophrenia obtained significantly higher scores in both the parameters for strength, frequency and duration of the depersonalisation/derealialisation experiences and in the 4 factors that form it: anomalous body experience, emotional numbing, anomalous subjective memories and unreality of surroundings. These results show that there are differences in the distribution of the scores in the 2 groups. Likewise, we also found these differences between the first episode group and the multiple episodes group for the Beck Depression Inventory and the Hamilton scale, as well as the subscales of the PANSS, except for that of positive symptoms.
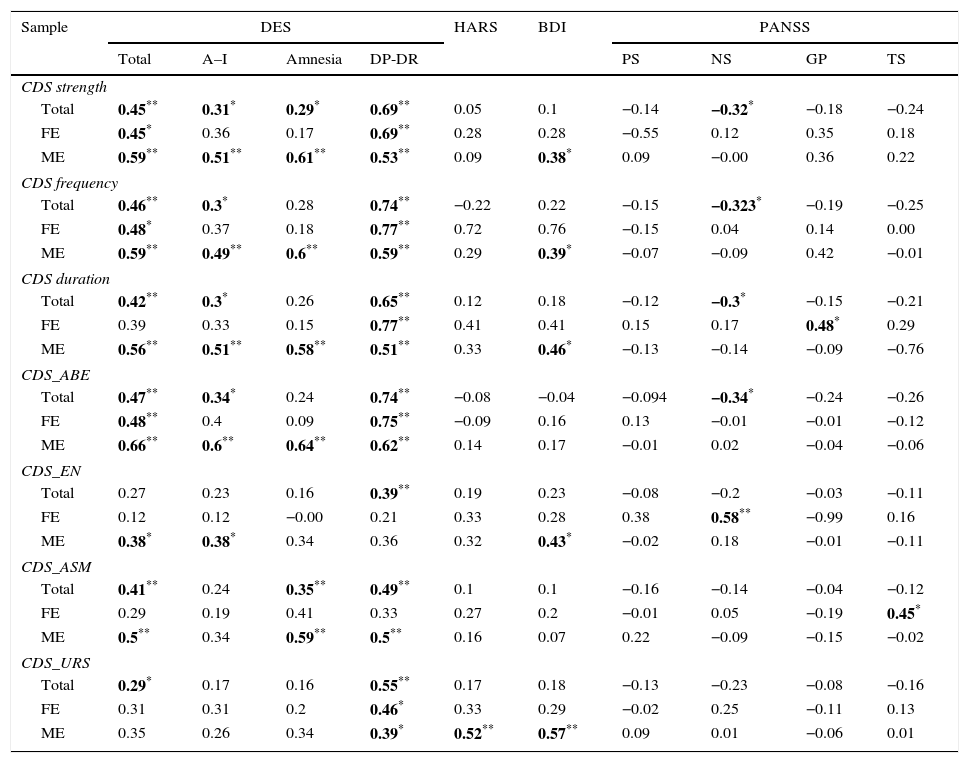
Los results of the association tests–Pearson correlation–between the CDS and the rest of the instruments used are shown in Table 3.
Pearson correlations for the various scales.
| Sample | DES | HARS | BDI | PANSS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | A–I | Amnesia | DP-DR | PS | NS | GP | TS | |||
| CDS strength | ||||||||||
| Total | 0.45** | 0.31* | 0.29* | 0.69** | 0.05 | 0.1 | −0.14 | −0.32* | −0.18 | −0.24 |
| FE | 0.45* | 0.36 | 0.17 | 0.69** | 0.28 | 0.28 | −0.55 | 0.12 | 0.35 | 0.18 |
| ME | 0.59** | 0.51** | 0.61** | 0.53** | 0.09 | 0.38* | 0.09 | −0.00 | 0.36 | 0.22 |
| CDS frequency | ||||||||||
| Total | 0.46** | 0.3* | 0.28 | 0.74** | −0.22 | 0.22 | −0.15 | −0.323* | −0.19 | −0.25 |
| FE | 0.48* | 0.37 | 0.18 | 0.77** | 0.72 | 0.76 | −0.15 | 0.04 | 0.14 | 0.00 |
| ME | 0.59** | 0.49** | 0.6** | 0.59** | 0.29 | 0.39* | −0.07 | −0.09 | 0.42 | −0.01 |
| CDS duration | ||||||||||
| Total | 0.42** | 0.3* | 0.26 | 0.65** | 0.12 | 0.18 | −0.12 | −0.3* | −0.15 | −0.21 |
| FE | 0.39 | 0.33 | 0.15 | 0.77** | 0.41 | 0.41 | 0.15 | 0.17 | 0.48* | 0.29 |
| ME | 0.56** | 0.51** | 0.58** | 0.51** | 0.33 | 0.46* | −0.13 | −0.14 | −0.09 | −0.76 |
| CDS_ABE | ||||||||||
| Total | 0.47** | 0.34* | 0.24 | 0.74** | −0.08 | −0.04 | −0.094 | −0.34* | −0.24 | −0.26 |
| FE | 0.48** | 0.4 | 0.09 | 0.75** | −0.09 | 0.16 | 0.13 | −0.01 | −0.01 | −0.12 |
| ME | 0.66** | 0.6** | 0.64** | 0.62** | 0.14 | 0.17 | −0.01 | 0.02 | −0.04 | −0.06 |
| CDS_EN | ||||||||||
| Total | 0.27 | 0.23 | 0.16 | 0.39** | 0.19 | 0.23 | −0.08 | −0.2 | −0.03 | −0.11 |
| FE | 0.12 | 0.12 | −0.00 | 0.21 | 0.33 | 0.28 | 0.38 | 0.58** | −0.99 | 0.16 |
| ME | 0.38* | 0.38* | 0.34 | 0.36 | 0.32 | 0.43* | −0.02 | 0.18 | −0.01 | −0.11 |
| CDS_ASM | ||||||||||
| Total | 0.41** | 0.24 | 0.35** | 0.49** | 0.1 | 0.1 | −0.16 | −0.14 | −0.04 | −0.12 |
| FE | 0.29 | 0.19 | 0.41 | 0.33 | 0.27 | 0.2 | −0.01 | 0.05 | −0.19 | 0.45* |
| ME | 0.5** | 0.34 | 0.59** | 0.5** | 0.16 | 0.07 | 0.22 | −0.09 | −0.15 | −0.02 |
| CDS_URS | ||||||||||
| Total | 0.29* | 0.17 | 0.16 | 0.55** | 0.17 | 0.18 | −0.13 | −0.23 | −0.08 | −0.16 |
| FE | 0.31 | 0.31 | 0.2 | 0.46* | 0.33 | 0.29 | −0.02 | 0.25 | −0.11 | 0.13 |
| ME | 0.35 | 0.26 | 0.34 | 0.39* | 0.52** | 0.57** | 0.09 | 0.01 | −0.06 | 0.01 |
ABE: anomalous body experience; A–I: absorption-imaginative; ASM: anomalous subjective memories; BDI: Beck Depression Inventory; CDS: Cambridge Depersonalisation Scale; DP-DR: depersonalisation/derealialisation; EN: emotional numbing; FE: first episodes; GP: general psychopathology; HARS: Hamilton Anxiety Rating Scale; ME: multiple episodes; NS: negative symptoms; PS: positive symptoms; TS: total score; URS: unreality of surroundings.
The data indicated in bold refer to the correlations with statistical significance.
The prevalence of experiences of depersonalisation in subjects with schizophrenia is approximately 6.9–36%.32 Our study results indicate that there are differences as to the greater number of symptoms of depersonalisation/derealialisation in patients with first episodes than those shown by subjects that have had multiple episodes. It is recognised that patients with schizophrenia present clear symptoms of depersonalisation, especially in the initial stages of the disease, and that such symptoms would be less frequent in its advanced stages.4 We find these differences are found not only in the scores for frequency, duration and strength, they are also present in the 4-factor model (anomalous body experience, emotional numbing, anomalous subjective memories and unreality of surroundings) of Sierra et al.26,29
The scores obtained for the CDS (Table 2) were similar to those obtained by Molina et al. in their study on the validation original to the Spanish version (43.16±37.35), while the subjects with first episodes scored twice as much in depersonalisation in our study. This might indicate that the experiences of depersonalisation are more frequent in the incipient or pre-onset stages of the psychosis, before the appearance of delusions and hallucinations (as Mayer-Gross4 maintain). Consequently, dimensions such as strength, duration and frequency are not linked to the positive symptoms. Another point is that no relationship was found between the scores on the CDS and those of the subscales of negative symptoms and of general psychopathology on the PANSS, in agreement with the original validation study. The findings reported in the literature mention the association between the experiences of depersonalisation with the basic symptoms, the affective symptoms and the alexithymia of schizophrenia.4,19,33
Likewise, it should be pointed out that the statistically significant differences between the 2 groups on the DES are mainly due to the items forming the depersonalisation subscale and not to those (the items) from absorption-imagination (the subscale); the latter items are considered as the most typical for dissociative phenomena.34
Depersonalisation has been conceptualised as a theoretical construct distributed along a continuum. Given that other phenomena can be present in healthy subjects, who experience them in situations of fatigue, stress and lack of sleep. Likewise, Depersonalisation also appears as a symptom, associated to many other psychiatric disorders (anxiety disorders, affective disorders, schizophrenia). Consequently, a distinction has to be made between depersonalisation as a symptom and as a disorder defined in the international diseases classifications.35
Interest in studying the experiences of depersonalisation/derealialisation in both the clinical and non-clinical populations has increased in the last few years, thanks to the appearance of valid and reliable instruments that make their evaluation easier, such as the CDS.25 Estudios prospective and retrospective studies have posited the presence of anomalous experiences, such as body alterations, depersonalisation, “dissolution of the limits to self” or dysphoria, in the prodromal phases of the psychosis and in predelusional states. These feelings, among which those of depersonalisation/derealialisation would be framed, would cause “feelings of change” in the subject and might be the basis for symptoms such as delusions. In this way, as the psychosis advanced, these experiences would become less important than other psychopathological phenomenon, such as hallucinations and delusions.8,9,16,36,37
The limitations of this study stem primarily from the sample composition and size, which could increase the risk of committing a type ierror. The fact that the sample came from hospitalised subjects made it difficult to pursue further the studies on associations among the different instruments used.
In short, with the results obtained, we can contribute to what has been reported in the literature as to the fact that experiences of depersonalisation/derealialisation are more frequent in patients with first episodes of schizophrenia than in patients with multiple episodes of the disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed conform to the ethical stands of the human experimentation committee responsible and are in agreement with the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed all the protocols at the work centre on publication of patient data.
Right to privacy and informed consentThe authors obtained informed consent from all the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThis study was carried out thanks to the collaboration agreement between the Fundación de Investigación Biomédica de Córdoba (FIBICO) [Cordoba Biomedical Research Foundation] and Janssen-Cilag.
Please cite this article as: Luque-Luque R, Chauca-Chauca GM, Alonso-Lobato P, Jaen-Moreno MJ. Despersonalización y esquizofrenia: estudio comparativo entre primeros y múltiples episodios de esquizofrenia. Rev Psiquiatr Salud Ment (Barc). 2016;9:143–149.