Bipolar disorder (BP) is one of the major causes of disability in the world. Epidemiological studies suggest that this disorder could be under-diagnosed owing to the difficulty in detecting hypomania episodes. The detection of present and past episodes of hypomania could help in the diagnosis and appropriate treatment of this disorder. The Hypomania Check List (HCL-32) is a questionnaire validated into Spanish and designed to detect past and present hypomania episodes in the psychiatric patient population.
Materials and methodsA total of 128 patients over 18 years old and diagnosed with type I bipolar (BP-I) disorder (n=1), type II bipolar (BP-II) disorder (n=30), major depression (MD) (n=57), anxiety disorders (AD) (n=15) were selected, along with a control group (C) (n=25). The patients were diagnosed according to the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IVTR). Screening for hypomania episodes was carried out by applying the HCL-32 scale.
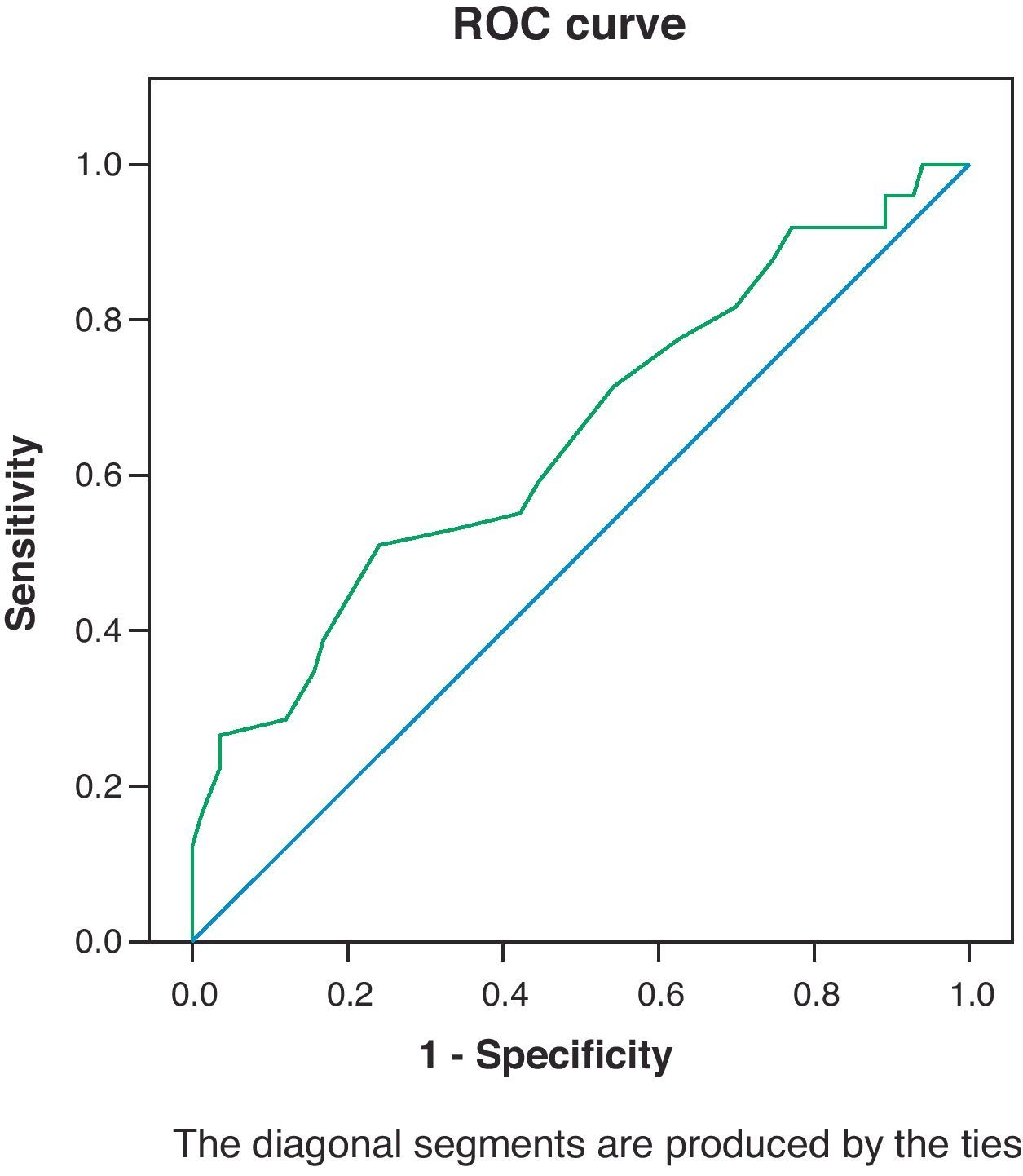
ResultsThe area under the ROC curve was 0.65 with a 95% confidence interval (CI) of 0.55–0.75. The chosen cut-off point of the HCL-32 was 15. The values for the sensitivity (Se), specificity (Sp), positive predictive values (PPV) and negative predictive values (NPV), and the prevalence (P) of hypomania episodes in the patients of the UP depression, for a cut-off point of 15 were: Se=71.4%, 95% CI; 57.8, 85.1, Sp=45.8%, 95% CI; 34.5–57.1, PPV=43.75%, 95% CI; 32.25–55.25, NPV: 73.08%, 95% CI; 60.06–86.09 and P=67.2%.
ConclusionsThe HCL-32 is a very sensitive, but not very specific, screening tool. This could partly explain the high proportion of hypomania episodes detected in our sample. Unlike previous studies, our sample is heterogeneous (from different environments) and at a more severe and unstable clinical level. Future research should develop more specific measuring tools, and with greater external validation, for hypomania episodes.
El trastorno bipolar (TBP) es una de las causas más importantes de discapacidad en el mundo. Estudios epidemiológicos sugieren que este trastorno podría estar infradiagnosticado debido a la dificultad de detección de episodios de hipomanía. La detección de episodios de hipomanía, tanto actuales como pasados, permitiría el diagnóstico y tratamiento adecuados de este trastorno. La Lista de Valoración de Hipomanía (HCL-32) es un cuestionario validado al español diseñado para la detección de episodios de hipomanía, pasados y presentes. Con este estudio se pretende comprobar la utilidad de la HCL-32 para detectar los episodios de hipomanía en la población psiquiátrica.
Material y métodosSe seleccionan 128 sujetos mayores de 18 años diagnosticados de trastorno bipolar tipo i (TBP-I) (n=30), trastorno bipolar tipo ii (TBP-II) (n=1), depresión unipolar (DM) (n=57), trastornos de ansiedad (TA) (n=15) y un grupo control (C) (n=25) de acuerdo con los criterios diagnósticos del Manual Diagnóstico y Estadístico de los Trastornos Mentales, cuarta edición, texto revisado, (DSM-IVTR). El cribado de episodios de hipomanía se realiza mediante la aplicación de la escala HCL-32.
ResultadosEl área bajo la curva ROC=0,65 IC95% (0,55-0,75). El punto de corte de la HCL-32 elegido es el 15. Los valores de sensibilidad (S), especificidad (E), valores predictivos positivo (VPP) y negativo (VPN) y prevalencia de episodios de hipomanía en los pacientes del grupo de depresión (P) para el punto de corte 15 son: S=71,4%, IC95% (57,8, 85,1), E=45,8%, IC95% (34,5-57,1), VPP = 43,75%, IC95% (32,25-55,25), VPN: 73,08%, IC95% (60,06-86,09) y P=67,2%.
ConclusionesLa HCL-32 constituye un instrumento de cribado muy sensible, aunque poco específico. Esto explicaría, en parte, la elevada proporción de episodios de hipomanía que detectamos en nuestra muestra. A diferencia de estudios previos, nuestra muestra es heterogénea (procede de diferentes ámbitos) y a nivel clínico es más grave e inestable. Futuras investigaciones deberían desarrollar instrumentos de medición de episodios de hipomanía más específicos y con mayor validez externa.
Bipolar disorder (BP) is a source of morbidity and mortality, with serious detriment to quality of life for those who suffer from it. In addition, due to its severity and chronicity, it involves a great social and economic expense.1–3
In the past, population studies demonstrated that, according to DSM-IV-TR criteria, BP has a prevalence of approximately 0.5–1.5%.4,5
Epidemiological studies from the western world suggest that BP may be under-diagnosed. This is attributed to the overdiagnosis of unipolar depression and the underdiagnosis of hypomanic episodes.6 The most recent evidence suggests that the true prevalence rate lies between 5 and 5.5% of the population,7–17 due in part to the underdiagnosed manic and hypomanic episodes.
It is estimated that the prevalence of major depression (MD) finally diagnosed as type I bipolar disorder (BP-I) rarely exceeds 5–10%.18
The rates oscillate between 30 and 61% for patients initially diagnosed with MD that are finally diagnosed with type II bipolar disorder (BP-II).7,19–25
The presence of hypomanic episodes is essential for the diagnosis of BP-II, establishing a differential diagnosis with MD. BP-I may also present hypomanic episodes, but the episodes differ from those of BP-II.
Over the course of the illness, patients diagnosed with BP-II seem more similar to those with bipolar disorder than those with a unipolar disorder, with respect to family history and response to treatment. In addition, BP-II responds better to treatment with mood stabilisers. Using antidepressants in these patients involves a higher risk of triggering an induced manic episode or rapid cycling.26 Incorrect diagnosis could delay the start of adequate treatment, consequently worsening the prognosis.17 Hence, the importance of an early diagnosis.
In an effort to improve the recognition of BP, instruments such as the Mood Disorder Questionnaire (MDQ)27 and the Hypomania Checklist (HCL-32)28 have been developed.
The HCL-32 is a self-administered questionnaire, serving as a tool designed to detect hypomanic components in patients with major depressive disorder.28 This scale has recently been validated in Spanish. In the study performed for its validation, its usefulness over the MDQ scale for retrospectively diagnosing hypomanic episodes was highlighted.14
The objective of this study was to evaluate the validity of the HCL-32 scale in detecting hypomanic symptoms in a psychiatric population divided into 4 groups (MD, BP, AD and control), establish the best cut-off point for the scale and compare these results with those obtained in previously published studies.
Materials and methodsPatients and controls were recruited consecutively for the study between 2006 and 2010 in various areas: 2 mental health centres from Area 6 of the Madrid Community (Majadahonda and Villalba), and the emergency, short-stay and bipolar disorder units at the Puerta de Hierro University Hospital Psychiatry Department in Majadahonda.
The ethics committee from the Puerta de Hierro University Hospital in Majadahonda approved the study. Informed consent was obtained in writing from all patients before their inclusion in the study.
SubjectsThe subjects who participated in this study were 18 years old or older, and diagnosed with BP-I, BP-II or MD, in accordance with DSM-IV-TR criteria. An anxiety disorder (AD) group was added, as some authors have affirmed that between 20 and 30% of patients who present anxiety symptomatology could have BP.33 This way, we were able to assess whether there were significant differences from the rest of the groups. The AD group included patients who fulfilled DSM-IV criteria for generalised anxiety disorder. Patients were assigned to each group using the Mini-International Neuropsychiatric Interview (MINI).
The control group was selected among patients who came for consultation at the psychiatry department in mental health centres in Majadahonda and Villalba and at the emergency unit in the psychiatry department at the Puerta de Hierro University Hospital. Patients were included in this group if they were diagnosed with adjustment disorder and abnormal personality traits that did not compromise their overall functioning. Patients were excluded from this group if they fulfilled DSM-IV criteria for mood disorders, psychotic disorders or generalised anxiety disorder. We also excluded those with a score higher than 7 on the Hamilton Rating Scale for Depression (HRSD-17).
Initially, 131 patients were included; all of them provided their informed consent in writing. Of the total sample, 3 patients were excluded, as they did not fulfil inclusion criteria for any of the groups.
In a sample size of 133 subjects with unipolar depression, the expected prevalence of patients with hypomanic symptoms is 2/3 (66.7%), with an error of ±8% and a 95% confidence interval (58.3–75.2%).
Among the 128 patients selected, 31 were diagnosed with BP (only 1 of them with BP-II), 57 with MD, 15 with AD and 25 were control subjects.
Patients were excluded from the study if they had previously been diagnosed with cognitive impairment or mental retardation. They were also excluded if they had a main diagnosis of alcohol or substance use disorder.
ProcedureAfter informing the patients about the study and obtaining their written informed consent for the study, the interviewer collected sociodemographic and clinical data. The interviewer applied the MINI, the HRSD-17, the Young Mania Rating Scale (YMRS) and the Clinical Global Impression Scale modified for bipolar disorder (CGI-BP) with each patient. The interviewer also gave each patient the HCL-32 questionnaire. The patients completed the International Personality Disorder Exam (IPDE) from the DSM-IV to study the relationship between personality disorders and hypomanic symptoms.
Hypomania screening among patients diagnosed with unipolar depression was performed by applying the HCL-32 scale. In this study we also aimed to corroborate the validation of the scale in Spanish, created by Vieta et al.14 in 2007. To this end, the HCL-32 scale was applied to the control group and the group of patients diagnosed with BP.
MeasurementsThe HCL-32 scale is a self-administered questionnaire developed by Angst et al.28 in 2005 and validated later in different countries and languages (German, English, Swedish, Italian, Chinese, Polish and Spanish). This scale consists of a list of possible hypomanic symptoms (32 items) to which the patient responds yes or no. In addition, it has 8 other sections that assess severity and impact of the symptoms on different aspects of the patient's life: (1) present state compared to normal state; (2) normal state compared to other people; (3) frequency of hypomanic periods; (4) socio-family and work consequences of said states; (5) others’ reactions to these states; (6) general duration of these states; (7) existence of elevated mood in the last year; and (8) number of days with elevated mood in the last year. Total score for the HCL-32 is obtained by adding up the affirmative responses to the 32-hypomanic symptom list. The scale was accepted and validated in Spanish by Vieta et al.14 who proposed 14 as the cut-off point for detecting hypomanic symptoms and discriminating between bipolar disorder and other groups (MD and healthy subjects). This cut-off point had a sensitivity of 0.85 with a 95% CI (0.78–0.91) and a specificity of 0.79 with a 95% CI (0.72–0.87).
Statistical analysisThe initial variables are described in tables with percentages and means, according to the variable type. Quantitative variables were summarised by mean and standard deviation (SD). In all cases, distribution of the variable was found according to theoretic models. An analysis of normality was performed using the Kolmogorov test. Confidence intervals were calculated at 95% (CI 95%) for the diagnostic tests, sensitivity, specificity and predictive values. The cut-off points for the HCL-32 scale were calculated using the ROC curve, with the MINI scale serving as a reference. With this analysis, different decision levels were established for various cut-off points. The cut-off point established the total score value based on the positive presence of hypomania. In addition, Student's t-test was used to compare 2 independent samples and the chi-squared test, corrected for continuity, was used to contrast proportions. The results of the main variables were described with 95% confidence intervals. The comparisons were performed with bilateral contrasts, with levels of significance established as equal to or lower than 0.05.
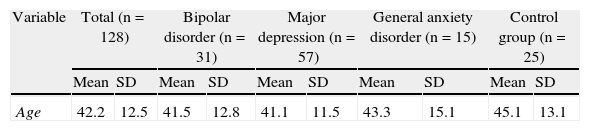
ResultsThe distribution of participants in each diagnostic category was as follows: 31 participants diagnosed with BP (30 BP-I and 1 BP-II), 57 with MD and 15 with AD. The control group consisted of 25 participants. Table 1 gives the sociodemographic characteristics of the sample, as well as the scores on the scale for each of the subgroups. The possible relationship between scores on the HCL-32 scale and the sociodemographic characteristics of the sample was analysed. The only statistically significant differences found were in the inverse relationship between the HCL-32 scores and 3 factors: age, patients born in rural environments and low socio-economic and cultural level.
Sociodemographic data.
| Variable | Total (n=128) | Bipolar disorder (n=31) | Major depression (n=57) | General anxiety disorder (n=15) | Control group (n=25) | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age | 42.2 | 12.5 | 41.5 | 12.8 | 41.1 | 11.5 | 43.3 | 15.1 | 45.1 | 13.1 |
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| Area | ||||||||||
| Emergency | 49 | 38.0 | 1 | 3.2 | 33 | 56.9 | 8 | 53.3 | 7 | 28.0 |
| MHC | 54 | 41.9 | 4 | 12.9 | 25 | 43.1 | 7 | 46.7 | 18 | 72.0 |
| SSU | 15 | 11.6 | 15 | 48.4 | 0 | 0 | 0 | 0 | 0 | 0 |
| BPU | 11 | 8.5 | 11 | 35.5 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sex | ||||||||||
| Male | 50 | 38.8 | 14 | 45.2 | 20 | 34.5 | 4 | 26.7 | 12 | 48.0 |
| Female | 79 | 61.2 | 17 | 54.8 | 38 | 65.5 | 11 | 73.3 | 13 | 52.0 |
| Place of birth | ||||||||||
| Rural | 16 | 13.8 | 3 | 9.7 | 7 | 15.2 | 2 | 14.3 | 4 | 16.0 |
| Urban | 100 | 86.2 | 28 | 90.3 | 39 | 84.8 | 12 | 85.7 | 21 | 84.0 |
| Education level | ||||||||||
| Primary | 16 | 12.5 | 4 | 12.9 | 6 | 10.5 | 5 | 33.3 | 1 | 4.0 |
| Secondary | 67 | 52.3 | 14 | 45.2 | 28 | 49.1 | 6 | 40.0 | 19 | 76.0 |
| University | 45 | 35.2 | 13 | 41.9 | 23 | 40.4 | 4 | 26.7 | 5 | 20.0 |
| Socioeconomic level | ||||||||||
| Low/lower middle | 17 | 15.0 | 3 | 10.0 | 7 | 15.6 | 4 | 30.8 | 3 | 12.0 |
| Middle | 80 | 70.8 | 21 | 70.0 | 30 | 66.7 | 7 | 53.8 | 22 | 88.0 |
| Upper middle/upper | 16 | 14.2 | 6 | 20.0 | 8 | 17.8 | 2 | 15.4 | 0 | 0 |
BPU: bipolar disorder unit; MHC: mental health centre; SSU: short-stay unit.
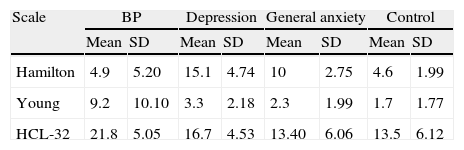
The results concerning clinical stability of the sample through scores on the HRSD and YMRS scales are shown in Table 2. Patients from the major depression group obtained higher scores on the HRSD scale, while higher scores on the YMRS scale corresponded to the BP group. The modified CGI-BP scale was applied to assess the clinical stability of the patients during the 6 months before the study, with the results indicating a general condition between normal and slightly ill on each of the subscales for most subjects.
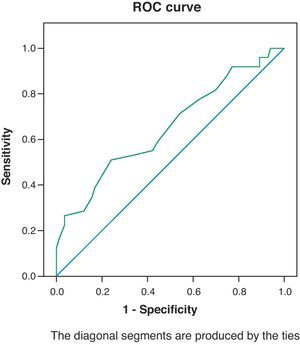
Discriminative capacity of the scale was analysed for bipolar disorder by ROC curve (Fig. 1). Discriminative capacity for the HCL-32 scale was assessed with the ROC curve, using the positive diagnosis of manic and hypomanic episodes–according to the MINI scale–as a reference or the gold standard. The ROC curve found allowed us to identify the sensitivity and specificity values for each decision level or each cut-off point on the HCL-32 scale. The cut-off point established a level of reference on the HCL-32 scale for screening hypomania. The area under the curve was 0.65 CI 95% (0.55–0.75), which indicates a low-moderate discriminative capacity.29
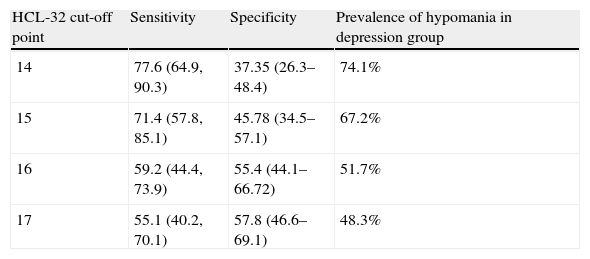
Table 3 shows the sensitivity and specificity results for each cut-off point and the hypomanic prevalence results among patients in the depression group.
Prevalence of hypomania in depression group.
| HCL-32 cut-off point | Sensitivity | Specificity | Prevalence of hypomania in depression group |
| 14 | 77.6 (64.9, 90.3) | 37.35 (26.3–48.4) | 74.1% |
| 15 | 71.4 (57.8, 85.1) | 45.78 (34.5–57.1) | 67.2% |
| 16 | 59.2 (44.4, 73.9) | 55.4 (44.1–66.72) | 51.7% |
| 17 | 55.1 (40.2, 70.1) | 57.8 (46.6–69.1) | 48.3% |
The best cut-off point was 15, with sensitivity and specificity values of 71.43 and 45.78%, respectively, and positive and negative predictive values of 43.75 and 73.08%, respectively. With this cut-off point, a hypomania prevalence of 67.2% was obtained among patients with an MD diagnosis.
The possible relationship between scores on the HCL-32 scale and the IPDE was analysed by means of Spearman's rank correlation coefficient. No statistically significant differences were found in the IPDE scale results between the different groups. The results obtained did not show correlation between the HCL-32 values and abnormal personality traits.
DiscussionIn our sample, the area under the ROC curve is low-moderate, considering the confidence intervals previously cited.29 This means that the HCL-32 scale did not seem to have adequate psychometric properties for the diagnosis of hypomanic episodes in patients with a previous diagnosis of depression. Nevertheless, the HCL-32 is an instrument for screening hypomania in patients with a previous diagnosis of unipolar depression, thus requiring high sensitivity values. The data obtained for each cut-off point, according to what is shown in Table 3, correspond to a position in the area under the curve (AUC) between 0.58 and 0.82, which means a low-moderate discriminative capacity.29 If we compare the previous studies (Table 3), we find AUC values close to those obtained in the studies from Angst et al.28 and Rybakowski et al. (2009), with an AUC of 0.75. In turn, the Vieta et al. (2006) and Forty et al. (2007) studies obtained superior AUC levels (AUC 0.82). Considering these data, as well as the low specificity and positive predictive values, we believe the HCL-32 to be an applicable instrument in screening for hypomania. However, to reduce the percentage of false positives and obtain an appropriate diagnosis, it would be necessary to complement the evaluation with a more specific instrument. The cut-off point of 15 possesses the best psychometric properties for this objective, with a sensitivity of 71.48% and a specificity of 45.78%. The corresponding PPV to the cut-off point at 15 is 43.75% with a 95% CI (32.25–55.25) and the NPV is 73.08% with a 95% CI (60.06–86.09).
If we use this cut-off point, 67.2% of the total sample score 16 or more points, meaning that more than half of the patients in the study have had or are having a hypomanic episode. This is in agreement with the results of previous studies stating that the prevalence of BP increases to 40% among psychiatric patients.31
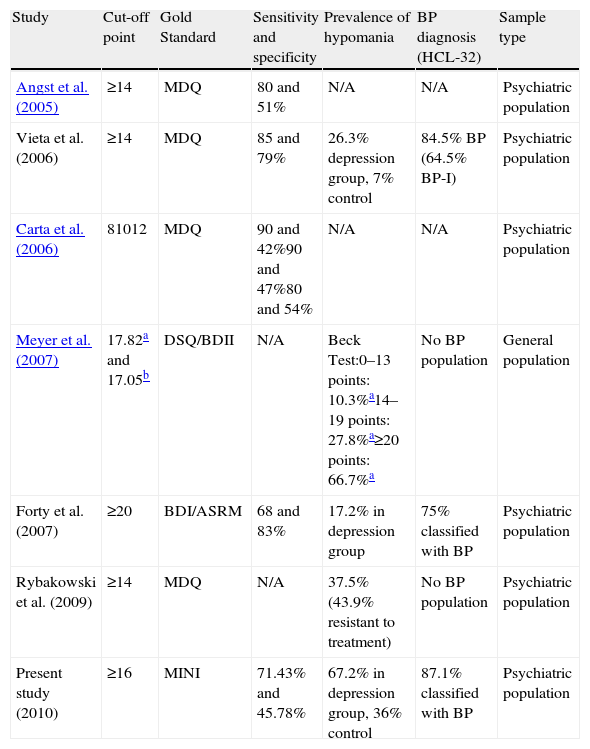
In Table 4, the results of our study were compared to the main articles published with the application of the HCL-32. Most of the studies established a cut-off point at 14,14,24,28 although Forty et al. (2007)30 placed it higher (20 points) in theirs.
Results of main published studies performed with HCL-32.
| Study | Cut-off point | Gold Standard | Sensitivity and specificity | Prevalence of hypomania | BP diagnosis (HCL-32) | Sample type |
| Angst et al. (2005) | ≥14 | MDQ | 80 and 51% | N/A | N/A | Psychiatric population |
| Vieta et al. (2006) | ≥14 | MDQ | 85 and 79% | 26.3% depression group, 7% control | 84.5% BP (64.5% BP-I) | Psychiatric population |
| Carta et al. (2006) | 81012 | MDQ | 90 and 42%90 and 47%80 and 54% | N/A | N/A | Psychiatric population |
| Meyer et al. (2007) | 17.82a and 17.05b | DSQ/BDII | N/A | Beck Test:0–13 points: 10.3%a14–19 points: 27.8%a≥20 points: 66.7%a | No BP population | General population |
| Forty et al. (2007) | ≥20 | BDI/ASRM | 68 and 83% | 17.2% in depression group | 75% classified with BP | Psychiatric population |
| Rybakowski et al. (2009) | ≥14 | MDQ | N/A | 37.5% (43.9% resistant to treatment) | No BP population | Psychiatric population |
| Present study (2010) | ≥16 | MINI | 71.43% and 45.78% | 67.2% in depression group, 36% control | 87.1% classified with BP | Psychiatric population |
In the Meyer et al.32 study, the possible history of hypomania in 2 populations (German and Swedish) was examined. The authors reflected that 11.4% of the German sample and 4.7% of the Swedish sample fulfilled criteria for “bipolarity.” The mean score on the HCL-32 for subjects who probably had hypomanic episodes in the past was 17.82 in the German population and 17.05 in the Swedish population.
Upon analysing the results of all the studies, the sensitivity value for our cut-off point (71.43%) was lower than in the Angst et al.,28 Vieta et al.,14 and Carta et al.31 studies, but slightly higher than in the Forty et al. (2007)30 study. Regarding specificity, our figure (45.78%) was similar to that in the Angst et al.28 and Carta et al.31 studies, but it did not reach the high figures reflected in the Vieta14 and Forty (2006)30 studies.
Nevertheless, the cut-off point chosen (15) had good capacity for screening patients previously diagnosed with both types of BP, given that the percentage of subjects with more positive diagnoses of hypomania, according to the HCL-32, occurs in the BP-I group (87.1%).
In reference to this, it should be pointed out that our study had an even better capacity to confirm the BP diagnosis than previous studies.14,30The group with the second-highest prevalence of hypomania was the MD group, in which 67.2% of them scored 16 points or more, a considerably higher figure than in previous studies.14,24,30 Nevertheless, high rates of BP prevalence have been described (between 30 and 61%) in diagnoses that were initially MD.7,16,19–25
Likewise, the prevalence closest to that found in our study was in the Meyer et al.32 study. The authors divided the German sample into 3 groups according to levels of intensity by using the Beck Depression Inventory: low level (0–13 points), medium level (14–19 points) and moderate level (≥20 points). According to the results obtained, hypomania was detected in 66.7% of the subjects from the most severe group.32
Another important fact in our study was the prevalence found of hypomanic episodes in the AD (26.7%) and control (36%) groups, which had percentages higher than those from a study with similar methodology.14 Nevertheless, literature shows that in the primary healthcare population, between 20 and 30% of the patients who present anxious or depressive symptoms may have BP.33
The disparity between the results obtained, regarding some of the previously mentioned studies could be explained by methodological differences.
Firstly, in previous studies, the population was homogenous and psychopathologically stable. With the exception of the Meyer et al.32 study, which was carried out in the general population, the rest of the studies involved a population in a psychiatric environment.14,24,28,30,32 Specifically, in the Vieta et al.14 study, the entire population came from mental health centres, there were no changes in treatment during the months previous to inclusion in the study and the scores on the YMRS and HRSD scales were lower than in our study. Our population was at a severe and unstable psychopathological level and came from different environments. In the groups from the emergency and in-hospital units, the scores on the HCL-32 were, overall, higher. The prevalence figures increased from those found in other studies, thus being more similar to the studies where the HCL-32 was used with a more severe psychiatric population.32 Although Angst et al.28 concluded that the scale could be used as a screening instrument even in patients with active affective symptomatology, it seems that this circumstance would limit generalisation of the results.
Secondly, several studies used the Structured Clinical Interview for DSM-IV Axis I disorders (SCID-IV) as a diagnostic interview.14,28,32 Instead, we applied the MINI. Despite having demonstrated moderate validity in comparison to the SCID in multiple languages,34–36 the MINI is a diagnostic instrument designed for application in primary healthcare and other non-psychiatric environments. Using different diagnostic interviews might have caused differences between the results that we obtained and those described in previous studies.
Thirdly, most previous studies used the MDQ scale14,24,28,32 as a reference test, a questionnaire specifically for mood disorders. Instead, we used a general diagnostic interview in our study: the MINI. This action may have made the specificity values lower than those in previous studies.
It should be emphasised that our study was carried out by resident physicians and physicians specialised in psychiatry, with training in the application of different scales. Likewise, the population used was divided not only by diagnosis but also by different environments, which contributed to a better interpretation of the data obtained. Given that the HCL-32 scale is a self-administered instrument and contains questions of a retrospective nature, we believe that the clinical state of the patients could have conditioned their perception of their own state of health.
Our study had limitations as well. The most relevant was the use of DSM-IV criteria for clinical diagnosis. As is known, recent studies suggest that the DSM-IV diagnostic criteria for BP-II are highly specific but not very sensitive22; this problem extends to diagnostic instruments developed after the release of DSM-IV. On the other hand, symptoms of hypomania and cyclothymia tend to be more difficult to diagnose than those of mania. Consequently, many patients on the bipolar spectrum receive a diagnosis of depression.37,39 This way, in the BP group, only type II patients could be recruited according to DSM-IV criteria. In reality, however, according to the HCL-32 results, 67.2% of the patients diagnosed with MD could really have been diagnosed with BP-II. Therefore, the true number of BP-II patients is much higher than that diagnosed by clinicians, which justifies both this study and the use of the HCL-32 in clinical practice.
The issue of correctly diagnosing BP-II is important because many studies show that treatment for type II bipolar disorder is not initiated until 10 years after the onset of the illness.17 This delay is largely due to the depressive episodes that appear at the onset of the illness, which are typically diagnosed as unipolar depression. In addition, patients with bipolar disorder often do not seek treatment during hypomanic episodes, given that this state is rarely perceived as pathological and is typically associated with functional improvement.8,16,38 The results of the 2000 survey carried out in the U.S. by the National Depressive and Manic-Depressive Association40 revealed that 69% of those with bipolar disorder were initially misdiagnosed (60% with major depressive disorder).
As we have previously commented, the data obtained by the AUC reflect a low-moderate discriminative capacity.29 Although the studies have demonstrated that the HCL-32 is a tool designed to detect hypomanic symptoms in patients diagnosed with MD, it is not an appropriate scale for distinguishing between type I and type II bipolar disorder.14,28 Most patients diagnosed with BP-I are going to achieve high scores on the scale because it assesses their hypomanic symptomatology as well as the repercussions of this symptomatology on different areas of patient life. On the other hand, BP-I is easier to detect than type II given that it is clinically more severe and also because it may present hypomanic episodes. In conclusion, the purpose of the scale is its usefulness in discriminating between BP and unipolar depression, limiting the under-diagnosis of BP-II.
Given the results obtained, we can highlight 2 conclusive aspects:
The HCL-32 is a detection instrument that is very sensitive but not very specific.
The HCL-32 is preferably applicable to patients with mood disorders that are psychopathologically stable and not severe at the moment of completing the scale.
For these reasons, future research needs to develop more specific measuring instruments for hypomanic symptoms with the objective of detecting, with more validity, those subjects who have experienced hypomanic episodes throughout their lives.
Ethical disclosuresProtection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestsThis study was made possible by the grants awarded to 1 of the authors, Dr. Santiago Ovejero: the first grant between February 2005 and January 2006 from the General Foundation of the Autonomous University of Madrid and the second, between February 2006 and January 2007 from the Foundation for Biomedical Research of the Puerta de Hierro University Hospital, with ties to the project titled “Implementation of the Research and Clinical Unit for Bipolar Disorder.”
The authors of this document wish to thank the selfless collaboration of Isabel Millán and Fernando García from the departments of biostatistics and epidemiology, respectively, at the Puerta de Hierro University Hospital in Majadahonda, the participants from the psychiatry department at the Puerta de Hierro University Hospital in Majadahonda and the evaluators and coordinators.
Please cite this article as: García-Castillo I, et al. Detección precoz de episodios de hipomanía en pacientes con trastorno afectivo. Rev Psiquiatr Salud Ment (Barc). 2012;5:89–97.