Joint hypermobility syndrome (JHS) has been found to be associated with anxiety disorders in clinical and nonclinical populations, but to date no studies have evaluated this association in children. The main goal of this study is to evaluate JHS along with anxiety, somatic and behavioral measures in children to clarify if JHS is associated with any of these variables in this age range.
MethodsA sample of 160 children (74 girls and 86 boys) ranging from 5 to 17 o were recruited from a Child-Adolescent Mental Health clinic to participate in the study. All children underwent a diagnostic interview using the Mini International Neuropsychiatric Interview for Children and Adolescents. Instruments used include the Child Behavior Checklist (CBCL), the Screening Questionnaire to detect Hypermobility (SQ-CH) and the Children Manifested Anxiety Scale (CMAS-R).
ResultsThe prevalence of JHS in this sample was 22%, and this was significantly higher in girls (31%) than in boys (14%) (χ2=6.83; p=.001). The JHS group scored significantly higher in the CMAS-R total anxiety (F=4.51; p=.035), CMAS-R Physiological anxiety (F=7.19; p=.008) and the CBCL somatic complaints (F=8.46; 0.004) and regression analyses showed that these 3 variables were predictors of JHS (χ2=36.77; p<.001; r2=0.22). The JHS group also scored higher in some behavioral measures.
ConclusionChildren with JHS have higher frequency of anxiety disorders and higher intensity of physiological anxiety, somatic complaints, and therefore, JHS might be used as marker for this anxiety phenotype in youngsters.
Se ha encontrado que el síndrome de hiperlaxitud articular (SHLA) está asociado a trastornos de ansiedad en poblaciones clínicas y no clínicas, aunque hasta la fecha ningún estudio ha evaluado esta asociación en niños. El objetivo principal de este estudio es evaluar el SHLA junto con la ansiedad, las medidas somáticas y conductuales en niños, para clarificar si el SHLA está asociado a cualquiera de estas variables en este rango de edad.
MétodosSe reclutó una muestra de 160 niños (74 chicas y 86 chicos) con edades comprendidas entre los 5 y los 17 años, procedentes de una clínica de salud mental de niños/adolescentes, para participar en el estudio. A todos los niños se les realizó una entrevista diagnóstica utilizando Mini International Neuropsychiatric Interview for Children and Adolescents. Los instrumentos utilizados incluyeron Child Behavior Checklist (CBCL), Screening Questionnaire to detect Hypermobility (SQ-CH) y Children Manifested Anxiety Scale (CMAS-R).
ResultadosLa prevalencia de SHLA en esta muestra fue del 22%, siendo significativamente alta en chicas (31%) en comparación con los chicos (14%) (χ2=6,83; p=0,001). El grupo SHLA obtuvo una puntuación considerablemente superior en la escala de ansiedad total CMAS-R (F=4,51; p=0,035), ansiedad fisiológica CMAS-R (F=7,19; p=0,008) y quejas somáticas CBCL (F=8,46; 0,004), y los análisis de regresión reflejaron que estas 3 variables eran factores predictivos de SHLA (χ2=36,77; p<0,001; r2=0,22). El grupo SHLA obtuvo también puntuaciones superiores en determinadas medidas conductuales.
ConclusiónLos niños con SHLA tienen mayor frecuencia de trastornos de ansiedad y mayor intensidad de ansiedad fisiológica, quejas somáticas y, por tanto, podría utilizarse el SHLA como marcador para este fenotipo de ansiedad en los jóvenes.
Anxiety disorders (ADs) are the most prevalent psychiatric disorders affecting children as shown by epidemiological studies.1 In early life they are associated with considerable developmental, psychosocial, and psychopathological complications.2 The prevalent rates in children vary substantially between studies,3–6 with estimated life prevalence's ranging from 15%2 to 31.9%.3 Some community samples have estimated that separation anxiety is the most common individual anxiety disorder in childhood with prevalence's ranging between 2.8 and 8%7 followed by specific phobia 10% and social phobia 7%.2 Moreover, some studies suggest that there is a considerable comorbidity among anxiety disorders in this age range.8
Literature describes higher rates of anxiety in girls across all ages although no significant gender differences are found in the average age at onset of anxiety.2,6,9 Besides this, ADs in youth are associated with increased risk of depression, substance abuse and other disorders occurring later in life.10–12 However, ADs remain mostly underdiagnosed and untreated, which represent an economic burden to society.13,14 In the recent years, a growing interest has developed to understand different aspects of anxiety and its related psychopathology in order to ameliorate this burden.
Parental psychopathology, behaviorally inhibited temperament, or early life adversity, have been identified as potential risk factors for ADs although several authors highlighted that more work is needed to identify the most powerful predictors and biomarkers.2,9 One of the limitations of the study of anxiety in children is the use categorical approaches, and there is emerging research supporting the implementation of the dimensional approach to differentiate degrees of symptom expression in terms of duration, severity, and illness stages.15,16 The dimensional approach may provide more fine-grained information about anxiety severity, which may guide novel therapeutic approaches and help with the diagnostic delay. Nonetheless, dimensional approaches carry less specificity and require more biological strengths. Another limitation is the fact that current nosology of ADs mainly considers the psychological and cognitive aspects of anxiety17 and neglects other important symptoms such as the somatic and physical manifestations of the illness.
In this sense, the joint hypermobility syndrome (JHS) has been associated with anxiety in clinical, nonclinical, adult and elderly populations.18–22 In children, only one study explored this association and the authors found that JHS was associated with greater anxiety severity.23 The JHS is a highly heritable collagen condition is characterized by and increased distensibility of the joints in passive movements as well as hypermobility in active movement in the absence of any rheumatologic disease.24 The JHS is more frequent in females (3:1) and has an estimated prevalence of 10–15% in the general population,24,25 and by age groups, is more common in youngsters.26
The association between anxiety and JHS was first described by Bulbena et al. in 1988 in a letter to the Lancet.18 Specifically, the JHS has been associated with higher frequency and intensity of fears and greater severity of anxiety, higher somatic complaints and higher frequency of the so-called endogenous anxiety disorders (panic, agoraphobia and social phobia). The literature confirms a strong association between these two variables,22,26,27 and there is also limited but growing evidence that this “anxiety/joint hypermobility” entity constitutes a unique phenotype that is seen across different areas of the psychopathology.21 The underlying mechanisms behind this association include genetic risks,28 autonomic nervous system dysfunction, increased exteroceptive and interoceptive mechanisms and decreased proprioception,29–31 and higher affective reactivity.32
Since JHS has been barely studied in relation to anxiety in this age range, it would be of great interest to clarify if JHS is also associated to anxiety in youth. The main aim of this study is to evaluate if JHS in children is associated with a subtype of anxiety to facilitate the earlier identification of the disorder. We hypothesize that JHS will be strongly associated with anxiety disorders in children, and also that JHS could be used as a predictor of anxiety in this age.
MethodsThis is a cross sectional study that was carried out in Barcelona, Spain. A total of 180 children and adolescents that were consecutively referred for a mental health evaluation to the Outpatient Child and Adolescence Mental Health Service (CAMHS) from October 2007 to February 2013 were selected as eligible subjects for the study. All participants had a full diagnostic interview using the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-Kid)33 as part of the systematic structured intake to assess the primary psychiatric diagnoses. Diagnoses were stablished by a multidisciplinary team of psychologists and psychiatrists after reviewing all available information, including data from medical records, the structured interviews, and clinical evaluations with the parents and child, school observations and behavioral checklists. All subjects with a clinical diagnosis were invited to participate in the study. Exclusion criteria included intellectual disabilities, autism and psychotic spectrum disorders, absence of a defined clinical diagnosis and failure to answer all the battery of questions.
The final sample included 160 children ranging from 5 to 17 years old; 12 subjects did not have a primary psychiatric diagnosis and 8 refused to participate. The participation of the study was voluntary with no monetary reward and the informed consent was obtained from all parents after the study procedures were fully explained. The study was reviewed and approved by the Ethics Committee of Clinical Investigation (CEIC) of the facility.
Instruments- -
The Mini international Neuropsychiatric Interview for Children and Adolescents (MINI-Kid33: it is a structured clinical diagnostic interview designed to assessed the presence of current DSM-IV and ICD-10 psychiatric disorders in children and adolescents aged 6–17 years and provides reliable and valid psychiatric diagnoses for this age range.34 The interview was administered to the child/adolescent together with the parents in most cases, although it can be administered to adolescents without a parent present.
- -
The Child Behavior Checklist (CBCL): this is a widely used caregiver checklist with 120 items that evaluate emotional, behavioral, and social problems based on the Achenbach system, in this study we used the version for schooled-age children (6–18 y/o). The Internalizing problems scale includes the “Anxious-depressed”, “Withdrawn-depressed”, and “Somatic complaints” subscales. There is also an externalizing problem scale that includes the “Rule-Breaking behavior” and “Aggressive Behavior” and the total problems scale that includes the “Social problems”, “Thought problems”, “Attention problems”, subscales.35
- -
The Screening Questionnaire to detect Hypermobility (SQ-CH): this is a 7-item questionnaire that was developed by Bulbena et al.36,37 It combines the Beighton and the Hospital del Mar and therefore evaluated not only the articular, but the extra-articular features associated with joint hypermobility and has been recently validated for children.23 Cut off points to determine the presence of JHS in children were stablished at scoring 4 or greater.
- -
The Children Manifested Anxiety Scale (CMAS-R): This is a 37-item self-report inventory used to measure anxiety in children.38 The total anxiety score is based on 28 items that include 3 subscales (Physiological Anxiety, Worry and Social Anxiety) and the Lie scale, which is a 9-item subscale designed to detect acquiescence, social desirability or faking of response. The results of the CMAS-R scale are reported as direct results (Pd) and the adjusted scalar or percentile scoring controlling for age (Pc).
Continuous variables were reported as means and standard deviations (SD) and categorical variables were reported as % (n). The ANOVA was used when comparing means of continuous data and the Chi Square test (χ2) for categorical data. Statistical significance was determined by two-tailed p<0.05. All statistical analyses were made using the SPSS – IBM version 22 for Macintosh. Multiple regression analyses were carried out to identify the group of variables significantly attached to the dependent variable of the model, in this case, belonging to the anxiety and JHS groups.
ResultsAnxiety vs. non-anxiety groupsThe final sample included 160 subjects, 74 females (46.2%) and 86 males (53.8%). The sample was initially divided into two groups in basis of the presence of anxiety as primary diagnosis (anxiety vs. non-anxiety group). Eighty subjects (50%) met Mini-Kid criteria for any anxiety disorder (separation anxiety disorder 2.5%, social anxiety disorder 3.75%, specific phobia 6.25%, generalized anxiety disorder 20%, obsessive–compulsive disorder 1.25%, and anxiety disorder not otherwise specified 16.25%). The other 50% of the sample met criteria for other diagnoses including mood/affective disorders 9.87%, Adjustment disorders 8.57%, eating disorders 3.66%, developmental disorders 5.56%, Hyperkinetic disorders 8.86%, Conduct disorders 6.41%, other emotional/behavioral disorders 5.70% and others 1.28%.
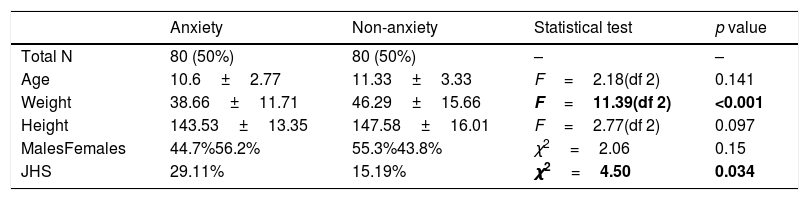
The anxiety group had significantly higher rates of JHS (29.11% vs. 15.19%; χ2=4.5; p=0.034) and lower body weights compared to the non-anxiety group (39.6kg vs. 46.29kg; F=11.39; p=<0.001), refer to Table 1 for details. No significant differences between groups were found in age, height, or sex distribution.
Sociodemographic differences between the anxiety and the non-anxiety group.
| Anxiety | Non-anxiety | Statistical test | p value | |
|---|---|---|---|---|
| Total N | 80 (50%) | 80 (50%) | – | – |
| Age | 10.6±2.77 | 11.33±3.33 | F=2.18(df 2) | 0.141 |
| Weight | 38.66±11.71 | 46.29±15.66 | F=11.39(df 2) | <0.001 |
| Height | 143.53±13.35 | 147.58±16.01 | F=2.77(df 2) | 0.097 |
| MalesFemales | 44.7%56.2% | 55.3%43.8% | χ2=2.06 | 0.15 |
| JHS | 29.11% | 15.19% | χ2=4.50 | 0.034 |
JHS: joint hypermobility syndrome.
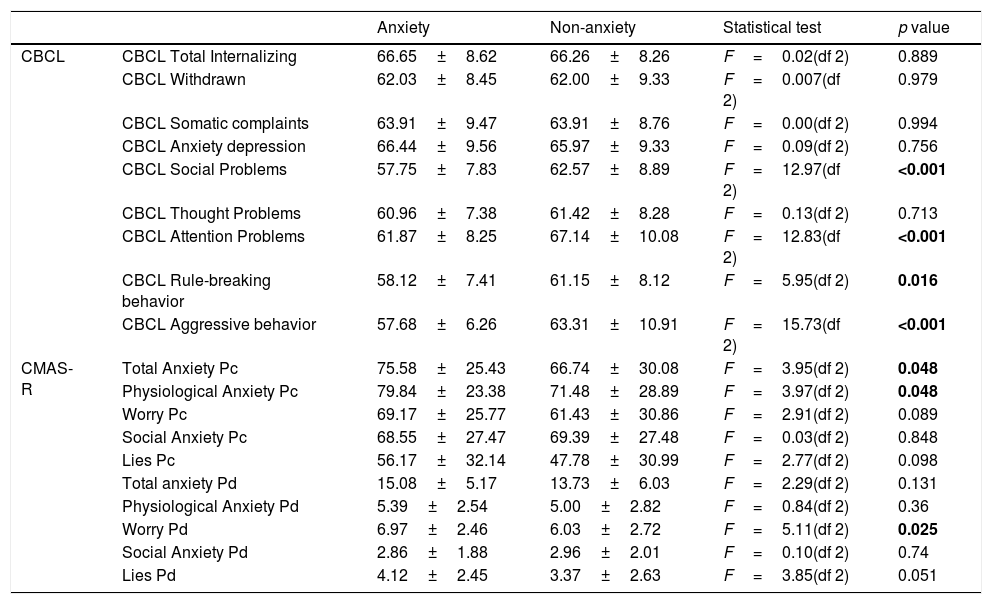
The anxiety group had significantly lower scores in the CBCL social problems (F=12.97(df 2); p=0.0004), the CBCL Attention Problems (F=12.83(df 2); p<0.001), the CBCL Rule-breaking behavior (F=5.95(df 2); p=0.016) and the CBCL Aggressive behavior subscales (F=15.73(df 2); p<0.001). No significant differences between groups were found on the other CBCL subscales, see Table 2 for details. The anxiety group had significantly higher scores in the CMAS-R Total Anxiety Pc (F=3.95(df 2); p=0.048), the CMAS-R Physiological anxiety Pc (F=3.97(df 2); p=0.048) and the CMAS-R Worry Pd subscales (F=5.11(df 2); p=0.025). No significant differences were found in the other subscales including the CMAS-R Worry Pc (p=0.089), the CMAS-R social anxiety Pc (p=0.848) and Pd (p=0.74), the CMAS-R lies Pc (p=0.098) and Pd (p=0.051), the Physiological anxiety Pd (p=0.36) and the Total anxiety scale Pd (p=0.131) subscales, full details in Table 2.
Scoring differences between the anxiety and the non-anxiety group.
| Anxiety | Non-anxiety | Statistical test | p value | ||
|---|---|---|---|---|---|
| CBCL | CBCL Total Internalizing | 66.65±8.62 | 66.26±8.26 | F=0.02(df 2) | 0.889 |
| CBCL Withdrawn | 62.03±8.45 | 62.00±9.33 | F=0.007(df 2) | 0.979 | |
| CBCL Somatic complaints | 63.91±9.47 | 63.91±8.76 | F=0.00(df 2) | 0.994 | |
| CBCL Anxiety depression | 66.44±9.56 | 65.97±9.33 | F=0.09(df 2) | 0.756 | |
| CBCL Social Problems | 57.75±7.83 | 62.57±8.89 | F=12.97(df 2) | <0.001 | |
| CBCL Thought Problems | 60.96±7.38 | 61.42±8.28 | F=0.13(df 2) | 0.713 | |
| CBCL Attention Problems | 61.87±8.25 | 67.14±10.08 | F=12.83(df 2) | <0.001 | |
| CBCL Rule-breaking behavior | 58.12±7.41 | 61.15±8.12 | F=5.95(df 2) | 0.016 | |
| CBCL Aggressive behavior | 57.68±6.26 | 63.31±10.91 | F=15.73(df 2) | <0.001 | |
| CMAS-R | Total Anxiety Pc | 75.58±25.43 | 66.74±30.08 | F=3.95(df 2) | 0.048 |
| Physiological Anxiety Pc | 79.84±23.38 | 71.48±28.89 | F=3.97(df 2) | 0.048 | |
| Worry Pc | 69.17±25.77 | 61.43±30.86 | F=2.91(df 2) | 0.089 | |
| Social Anxiety Pc | 68.55±27.47 | 69.39±27.48 | F=0.03(df 2) | 0.848 | |
| Lies Pc | 56.17±32.14 | 47.78±30.99 | F=2.77(df 2) | 0.098 | |
| Total anxiety Pd | 15.08±5.17 | 13.73±6.03 | F=2.29(df 2) | 0.131 | |
| Physiological Anxiety Pd | 5.39±2.54 | 5.00±2.82 | F=0.84(df 2) | 0.36 | |
| Worry Pd | 6.97±2.46 | 6.03±2.72 | F=5.11(df 2) | 0.025 | |
| Social Anxiety Pd | 2.86±1.88 | 2.96±2.01 | F=0.10(df 2) | 0.74 | |
| Lies Pd | 4.12±2.45 | 3.37±2.63 | F=3.85(df 2) | 0.051 |
CBCL: Child Behavior Checklist; CMAS-R: Children Manifested Anxiety Scale; Pc: percentile scoring; Pd: direct results.
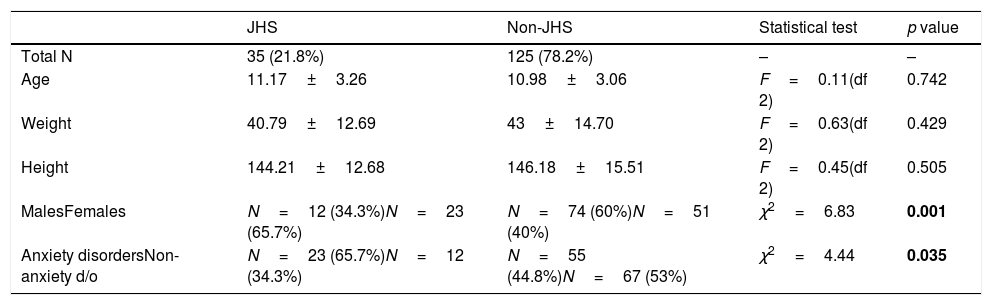
Approximately, 22% the subjects in the sample met criteria for JHS following the SQ-CH criteria. Taking into account these results, the sample was divided into 2 groups (JHS (n=35) vs. non JHS (n=125)) to further study the anxiety, somatic, and behavioral profiles in both groups. Girls were more hypermobile compared to boys (31% vs. 14%; χ2=6.83; p=0.001) but no significant differences in age (p=0.742), weight (p=0.43), height (p=0.505) were found between the JHS and the non-JHS group. However, when comparing the frequencies of anxiety disorders in both groups, the JHS group had significantly higher rates of anxiety disorders (χ2=4.41; p=0.035), see all details in Table 3 for details.
Differences between JHS and non JHS group.
| JHS | Non-JHS | Statistical test | p value | |
|---|---|---|---|---|
| Total N | 35 (21.8%) | 125 (78.2%) | – | – |
| Age | 11.17±3.26 | 10.98±3.06 | F=0.11(df 2) | 0.742 |
| Weight | 40.79±12.69 | 43±14.70 | F=0.63(df 2) | 0.429 |
| Height | 144.21±12.68 | 146.18±15.51 | F=0.45(df 2) | 0.505 |
| MalesFemales | N=12 (34.3%)N=23 (65.7%) | N=74 (60%)N=51 (40%) | χ2=6.83 | 0.001 |
| Anxiety disordersNon-anxiety d/o | N=23 (65.7%)N=12 (34.3%) | N=55 (44.8%)N=67 (53%) | χ2=4.44 | 0.035 |
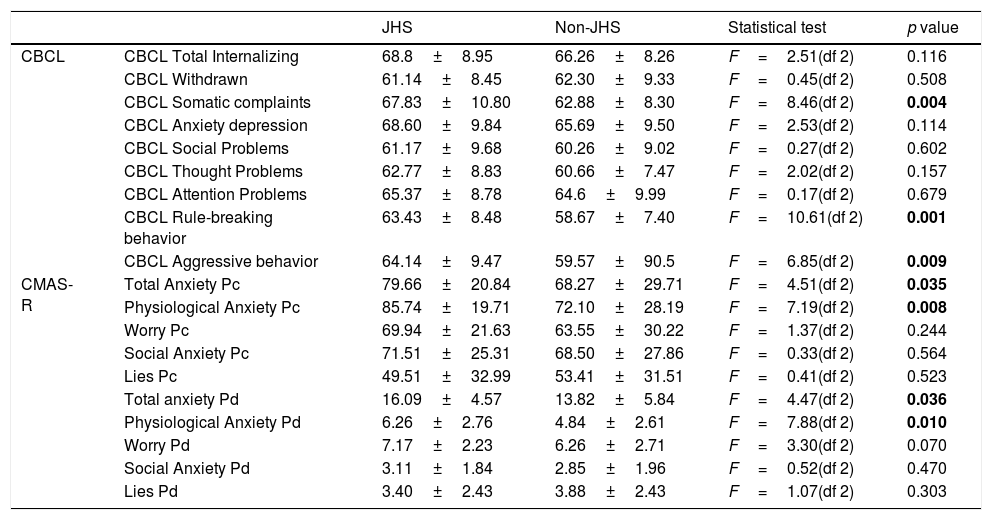
The JHS group scored significantly higher in the CBCL somatic complaints subscale (F=8.46(df 2); p=0.004) and despite they also scored higher in the CBCL Anxiety depression subscale, the differences between groups were not statistically significant, refer to Table 4 for details. No significant differences between groups were found in the CBCL Social Problems (p=0.602), CBCL Thought Problems (p=0.157) and CBCL Attention Problems (p=0.679) subscales. Interestingly, the JHS group had significantly higher scores in the CBCL Rule breaking behavior subscale (F=10.61(df 2); p=0.001) and the CBCL Aggressive behavior subscale (F=6.85(df 2); p=0.009). When evaluating the scoring differences between groups in the CMAS-R scale, it was noted that the JHS had significantly higher scores on the Total anxiety scale (Pd scores F=4.47(df 2); p=0.036) and the physiological anxiety subscale (Pd scores F=7.88(df 2); p=0.010). Despite the JHS scored higher on the CMAS-R worry subscales, the difference did not reach statistical significance (p=0.07). No significant differences were found between groups in the other subscales, see all details in Table 4.
Scoring differences between JHS and non JHS group.
| JHS | Non-JHS | Statistical test | p value | ||
|---|---|---|---|---|---|
| CBCL | CBCL Total Internalizing | 68.8±8.95 | 66.26±8.26 | F=2.51(df 2) | 0.116 |
| CBCL Withdrawn | 61.14±8.45 | 62.30±9.33 | F=0.45(df 2) | 0.508 | |
| CBCL Somatic complaints | 67.83±10.80 | 62.88±8.30 | F=8.46(df 2) | 0.004 | |
| CBCL Anxiety depression | 68.60±9.84 | 65.69±9.50 | F=2.53(df 2) | 0.114 | |
| CBCL Social Problems | 61.17±9.68 | 60.26±9.02 | F=0.27(df 2) | 0.602 | |
| CBCL Thought Problems | 62.77±8.83 | 60.66±7.47 | F=2.02(df 2) | 0.157 | |
| CBCL Attention Problems | 65.37±8.78 | 64.6±9.99 | F=0.17(df 2) | 0.679 | |
| CBCL Rule-breaking behavior | 63.43±8.48 | 58.67±7.40 | F=10.61(df 2) | 0.001 | |
| CBCL Aggressive behavior | 64.14±9.47 | 59.57±90.5 | F=6.85(df 2) | 0.009 | |
| CMAS-R | Total Anxiety Pc | 79.66±20.84 | 68.27±29.71 | F=4.51(df 2) | 0.035 |
| Physiological Anxiety Pc | 85.74±19.71 | 72.10±28.19 | F=7.19(df 2) | 0.008 | |
| Worry Pc | 69.94±21.63 | 63.55±30.22 | F=1.37(df 2) | 0.244 | |
| Social Anxiety Pc | 71.51±25.31 | 68.50±27.86 | F=0.33(df 2) | 0.564 | |
| Lies Pc | 49.51±32.99 | 53.41±31.51 | F=0.41(df 2) | 0.523 | |
| Total anxiety Pd | 16.09±4.57 | 13.82±5.84 | F=4.47(df 2) | 0.036 | |
| Physiological Anxiety Pd | 6.26±2.76 | 4.84±2.61 | F=7.88(df 2) | 0.010 | |
| Worry Pd | 7.17±2.23 | 6.26±2.71 | F=3.30(df 2) | 0.070 | |
| Social Anxiety Pd | 3.11±1.84 | 2.85±1.96 | F=0.52(df 2) | 0.470 | |
| Lies Pd | 3.40±2.43 | 3.88±2.43 | F=1.07(df 2) | 0.303 |
CBCL: Child Behavior Checklist; CMAS-R: Children Manifested Anxiety Scale; Pc: percentile scoring; Pd: direct results.
Multiple regression analyses were carried out to identify the group of variables significantly attached to the belonging to the Anxiety and the JHs groups.
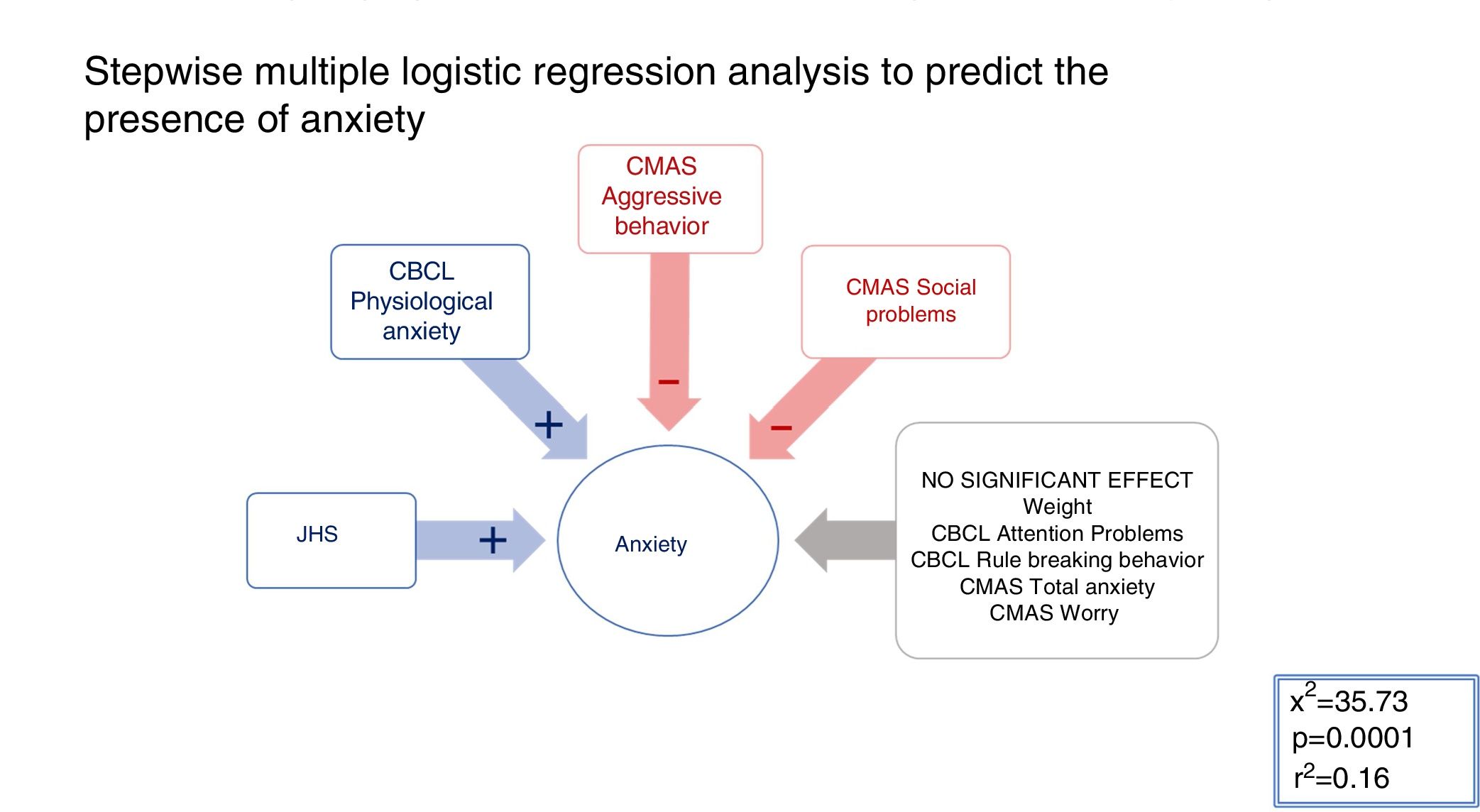
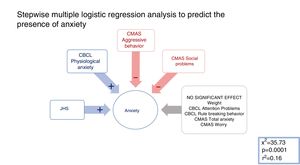
AnxietyAll significant variables in the comparison between the anxiety vs. the non-anxiety groups (refer to Tables 1 and 2 for details) were included in a mixed stepwise model, with a 0.25 p threshold to enter or remove variables (χ2=35.73; p<0.001; r2=0.16). The presence of JHS (χ2=7.10; p=0.008) and the CMAS-R Physiological anxiety scores (χ2=4.45; p=0.035) had a positive beta sign, which means a positive association with the dependent variable. On the contrary, the CBCL Aggressive behaviour (χ2=11.23; p<0.001) and CBCL Social problems (χ2=4.38; p=0.036) were selected with a negative beta sign, which means a negative association with the dependent variable (see Fig. 1 for details). Therefore, the presence of Joint hypermobility, physiological anxiety and the absence of aggressive behavior and social conflicts predicted significantly the belonging to the anxiety group in this sample.
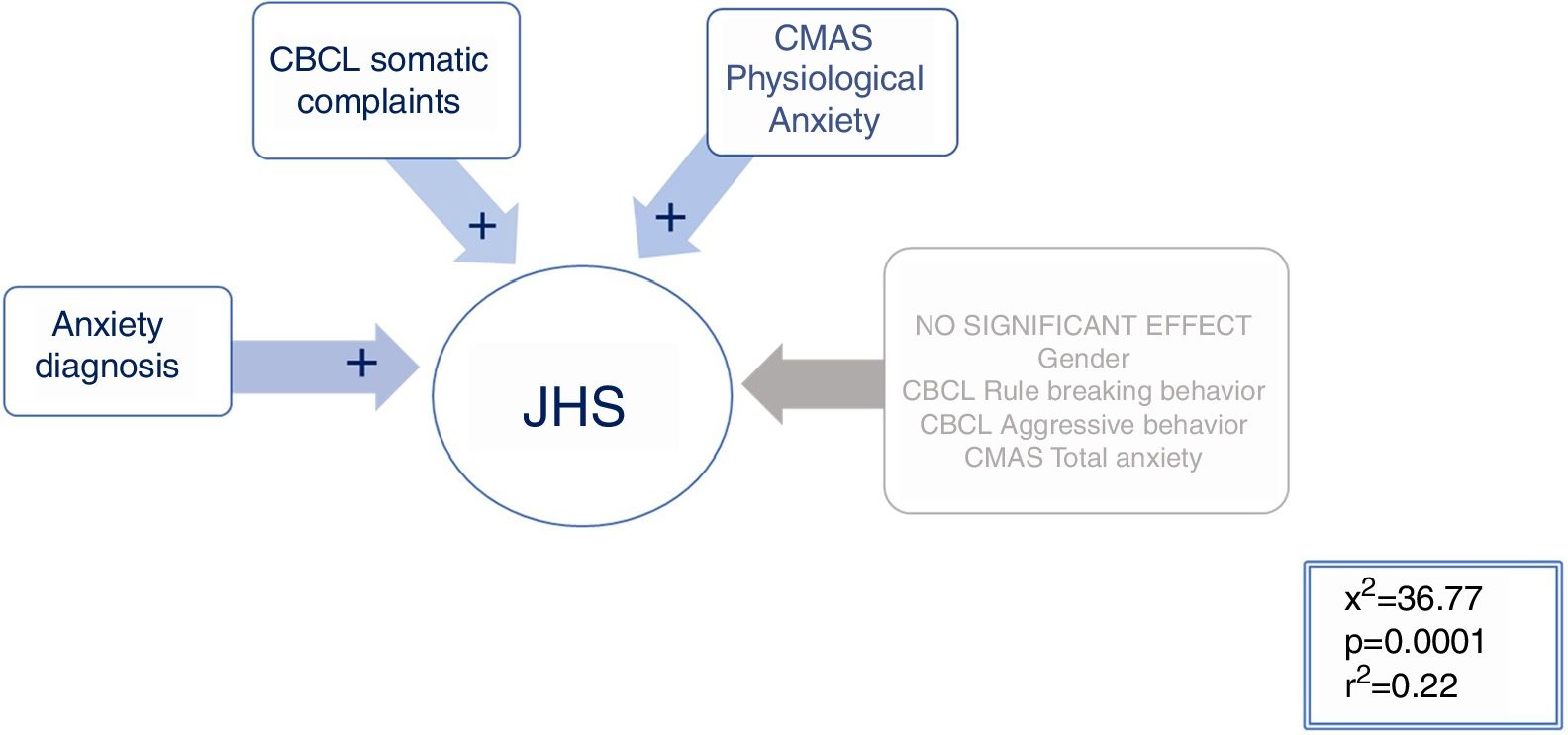
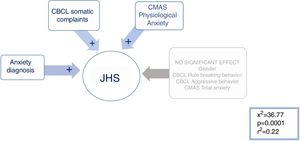
JHSAll significant variables in the comparison between the hypermobile vs. the non-hypermobile groups (refer to Tables 3 and 4 for details) were included in a mixed stepwise model, with a 0.25 p threshold to enter or remove variables. The resulting equation (χ2=36.77; p<0.001; r2=0.22) selected the following variables with positive beta sign: Anxiety diagnosis (χ2=8.77; p=0.0031), the CBCL Somatic Complaints (χ2=5.50; p=0.019) and the CMAS-R Physiological anxiety Pd (χ2=4.86; p=0.0275), see Fig. 2 for details. Therefore, having an anxiety diagnosis, the presence of somatic complaints and physiological signs of anxiety predicted significantly being in the Joint hypermobility syndrome group.
Stepwise multiple logistic regression analysis to predict the presence of JHS. Multiple regression model in which group membership is predicted with the syndrome of joint hypermobility. Having a diagnosis of anxiety, somatic complaints and physiological signs of anxiety are predictive of SHA.
In this paper, we studied anxiety and somatic symptoms along with behavioral problems in relation to JHS in a pediatric sample to see if JHS can be used as a marker of anxiety in this age range. We used both categorical and dimensional instruments to capture sub-threshold anxiety, somatic and behavioral symptoms.
Hypermobile spectrum disorders are common in pediatric populations, ranging from 3 to 30%39-41 which is similar to our findings. This spectrum includes a variety disorders in which hypermobility is understood as a continuum from asymptomatic hypermobility (i.e. joint hypermobility) to hypermobile Elher–Dalnos syndromes, with intermediate phenotypes such as JHS. One of the most commonly used measure to evaluate joint hypermobility in children is the Beighton score,42 but this scale only evaluates the laxity of the joints but neglects the extra-articular symptoms of the JHS. Some of these extra-articular symptoms in adults include dysautonomia, hernias and organ prolapses, chronic pain, easy bruising and tendency toward keloid scarring to name a few.25 Numerous extra-articular manifestations of JHS have been similarly reported in children, including but not limited to chronic constipation and encopresis, enuresis and urinary tract infections (UTI), higher skin extensibility, lower systemic blood pressure, lower bone quantitative ultrasound measurements, chronic fatigue syndrome, temporomandibular joint disease, fibromyalgia, and gross motor developmental delay.43 In the present study, we evaluated JHS, the multi-systemic condition with the SQ-CH, a validated self-assessment instrument that includes some extra-articular symptoms and has good reliability and validity.36,37 The JHS in adults is diagnosed with scores greater than 3, but in this study, the cut off scores were adapted (≥4) to consider the higher joint hyperlaxity in younger populations. Therefore, to ensure the proper assessment of the JHS, as opposed to JH only, would recommend that subsequent studies use this instrument. The extra-articular symptoms of the JHS are a paramount part of the disorder and should be always evaluated.
Categorically, the anxiety group had significantly higher rates of JHS and on the other hand; the JHS had significantly higher rates of anxiety disorders. Literature shows that JHS is associated with a heightened expression of anxiety symptoms26,44,45 and represents a risk factor trait for developing anxiety disorders as shown in a 15 follow up prospective study.46 While the CBCL profiles of the anxiety group and the JHS were different, it is interesting to notice that they both had higher scores in the CMAS-R total anxiety and physiological anxiety which highlights the importance of the bodily symptoms in both anxiety and JHS. The scores of the anxiety and the JHS group were not significantly higher in other anxiety subscales such as CBCL anxiety depression and the CMAS-R social anxiety subscales. However, the JHS group had a tendency toward more somatic complaints as evidenced by their significantly higher scores in the CBCL somatic complaints. The regression analyses showed the predictors of being in the JHS group included being diagnosed with an anxiety disorder, having somatic complaints and physiological anxiety reinforcing the hypothesis that subjects with JHS have a tendency toward anxiety with higher bodily symptoms and somatic complaints. One possible hypothesis for these findings is the fact that people with JHS have increased body perception and autonomic abnormalities, and as a result, suffer from stress-sensitive and somatic illnesses and complaints.30 Another possible explanation is that people with JHS have greater fragility of the structural tissues which translates into greater tendency toward trauma and multisystem complaints. Eccles et al. found that JHS subjects have larger amygdala volumes compared to non JHS subjects47 and in that study, the JHS subjects scored higher on body awareness, reinforcing the theory that body perception plays a role in the interaction between JHS and amygdala volumes. While no specific treatment studies have been done for this specific phenotype, future lines of research should explore interventions that address not only the psychological symptoms but the physical and somatic complaints including integrated approaches and innovative psychotherapies coupled with modern physiotherapy.
When comparing the JHS and the non JHS group, there were no body weight or height differences between groups but prior studies point toward a relationship between the ectomorph somatotype (linear, thin, and usually tall) and JHS.21 Adult JHS subjects have higher rates of restrictive or compensatory eating disorders such as anorexia or bulimia.22 In this sense, Baeza Velasco proposed a model of eating disorders in JHS that hypothesized that both articular (i.e. temporomandibular joint dysfunction) and extra-articular features (i.e. gastrointestinal problems, food intolerances) play a role in developing and maintain these eating patterns.48 However, all those studies were done in adult populations and therefore based on our findings; these data may not be applicable to younger populations. On the other hand, the anxiety group had significantly lower body weights compared to the non-anxiety group. A review of the literature shows that while anxiety can be associated with higher weight status in children and adolescents,49 it has also been associated with eating disorders.49-52 In this study, we did not assess eating patterns or behaviors and therefore we cannot draw conclusions on the influence of anxiety on eating disorders and weight. Subsequent studies should better characterize the influence of anxiety in the development and maintenance of eating disorders and assess if JHS plays a role in this association in this age range.
Contrary to prior findings, the JHS group did not display greater attention problems as evidenced by the similar scores between groups in the CBCL Attention Problems. Several studies found that individuals with JHS have a higher frequency of ADHD/ADD and anxiety compared to the non JHS in children53-55 and adults.56,57 One possible explanation for the negative findings could be the fact that we measured attention with a behavioral checklist instead of using a structured interview or specific scales that measure dimensional features of attention. Additionally, the anxiety group scored lower on some of the behavioral measures such as attention, rule breaking or aggressive behavior. In fact, the regression analysis showed that the absence of aggressive behavior and the social problems predicted being in the anxiety group. These findings reinforce the hypothesis that JHS is a marker for a homogeneous type of anxiety only, and subsequent studies should clarify the role of behavior in the JHS phenotype in children. As stated above, it is important to move toward a dimensional approach of illness to characterize the different forms of anxiety in order to study and define the pathophysiology behind those associations.
In summary, children with JHS have higher frequency of anxiety disorders and tend to suffer from a homogeneous type of anxiety characterized by higher physiological anxiety (bodily symptoms) and somatic complaints. Based on these findings, JHS could be used as a marker for this anxiety phenotype in this age range. This is in line with other studies that showed that JHS can also be used as a marker for a subtype of anxiety in adults and in the elderly populations. Further studies are required to clarify the role of JHS in the relationship between anxiety disorders and behavioral disturbances in children. These results may be a step toward a better understanding of the association between joint hypermobility and anxiety but new studies are required to further explore this association.
FundingThis study has not received any funding.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Bulbena-Cabre A, Duñó L, Almeda S, Batlle S, Camprodon-Rosanas E, Martín-Lopez LM, et al. La hiperlaxitud articular como marcador de ansiedad en niños. Rev Psiquiatr Salud Ment (Barc.). 2019;12:68–76.