A high prevalence of obsessive–compulsive symptoms (OCSs) in anxiety-depressive disorders ranging from 30 to 67% has been described.
ObjectiveThis study aims to assess the presence and persistence of OCSs in an outpatient sample of subjects with anxiety and depressive disorders, as well as its relationship with recent life events (RLEs) and/or traumatic experiences (TEs).
MethodWe conducted a prospective, observational, analytical study of 200 subjects with DSM-5 diagnoses of anxiety and/or depression. Participants were included by consecutive sampling and were evaluated at baseline and after 6–12 months (mean 8.5 months) of follow-up. The severity of the symptoms was assessed through the Hamilton Anxiety Scale (HARS) and Hamilton Scale for the evaluation of depression (HRSD-17), and comorbidity was assessed through the International Neuropsychiatric Interview (MINI). The Revised Inventory of Obsessions and Compulsions (OCI-R), the Recent Vital Changes Questionnaire (CVSV), and the Diagnostic Scale for Post-Traumatic Stress (PDS) were also administered.
Results54% of the sample presented OCSs, and 30.5% presented one or more TEs throughout life. At the baseline visit, the presence of OCSs was associated with the severity of depressive symptoms (p=0.028), the presence of TEs (p<0.01), symptoms of post-traumatic stress disorder (p<0.01) and the number of RLEs (p<0.01). Response rate at follow-up was 38%, and persistence of OCSs was found in 60.5% of patients, independent of depressive or anxious symptoms, but was associated with the number of RLEs (p<0.01).
ConclusionThe presence of OCSs in patients with anxiety and depressive disorders is frequent and persistent. Anxious-depressive patients with a history of TEs and RLEs had higher OCS levels. These findings highlight the importance of early detection and the use of therapeutic strategies focused on resilience to stress and trauma.
Se ha descrito una alta prevalencia de síntomas obsesivo-compulsivos (SOC) en los trastornos de ansiedad-depresivos que van desde el 30 al 67%.
ObjetivoEste estudio tiene como objetivo evaluar la presencia y persistencia de SOC en una muestra ambulatoria de sujetos con trastornos de ansiedad y depresión, así como su relación con eventos de la vida recientes (EVR) y/o experiencias traumáticas (ET).
MétodoSe llevó a cabo un estudio prospectivo, observacional y analítico de 200 sujetos con diagnósticos de ansiedad y/o depresión, según el manual diagnóstico y estadístico de los trastornos mentales, quinta edición (DSM-5). Los participantes fueron incluidos mediante muestreo consecutivo y evaluados al inicio del estudio y después de seis a 12 meses (media 8,5 meses) de seguimiento. La gravedad de los síntomas se evaluó mediante la escala Hamilton anxiety rating scale (HARS) y Hamilton depression rating scale (HRSD-17), y la comorbilidad a través del mini international neuropsychiatric interview (MINI). También, se administró el inventario revisado de obsesiones y compulsiones (OCI-R), el cuestionario de cambios vitales recientes (CVSV) y la escala de diagnóstico de estrés postraumático (PDS).
ResultadosEl 54% de la muestra presentó SOC y el 30,5% mostró uno o más ET a lo largo de la vida. En la visita basal, la presencia de SOC se asoció con la gravedad de los síntomas depresivos (p = 0,028), la presencia de ET (p < 0,01), los síntomas de trastorno de estrés postraumático (p < 0,01) y el número de EVR (p < 0,01). La tasa de respuesta en el seguimiento fue del 38% y la persistencia de los SOC se encontró en el 60,5% de los pacientes, independientemente de los síntomas depresivos o ansiosos, aunque asociada al número de EVR (p < 0,01).
ConclusionesLa presencia de SOC en pacientes con trastornos de ansiedad y depresión es frecuente y persistente. Las personas ansioso-depresivas con antecedentes de eventos traumáticos y recientes eventos de la vida tenían niveles más altos de SOC. Estos hallazgos resaltan la importancia de la detección temprana y el uso de estrategias terapéuticas enfocadas en la resiliencia al estrés y al trauma.
The transdiagnostic approach arises from the need to provide a basis for understanding, classifying, and integrating the different symptoms and diagnoses from common processes and factors. Its purpose is to find underlying mechanisms that are relevant to a set of disorders in order to find therapeutic strategies aimed at these processes, regardless of the specific diagnosis.1–4
For all anxiety-depressive disorders, a high prevalence of obsessive–compulsive symptoms (OCSs) has been described, with rates ranging from 30 to 67%,5–8 differences that, in part, depend on the great variability methodological when assessing this symptomatology. Baer et al. (2015)8 evaluated the proportion of OCSs in a sample of 3984 subjects diagnosed with major depressive disorder, within the Sequenced Treatment Alternatives to Relief Depression (STAR*D) study, and found a prevalence of 67% through the use of the Psychiatric Diagnostic Screening Questionnaire (PDSQ). More recently, Hofmeijer-Sevink et al. (2017)7 reported, in a cohort of 2981 subjects included in the Netherlands Study of Depression and Anxiety (NESDA), a prevalence of OCSs of 36.1% for those patients with a depressive disorder, of 35.9% for those with an anxiety disorder, and of 66.5% for anxiety-depressive comorbidity, using the 8-item YASR-OCS (The Young Adult Self-Report Scale for obsessive compulsive symptoms) scale.
On the other hand, several studies have pointed out the association between stressful and/or traumatic experiences (TEs) and the development of OCSs.9–15 In relation to this association between trauma and OCSs, the prevalence of obsessive–compulsive disorder (OCD) after a TE (whether or not it involves the presence of post-traumatic stress disorder) varies from 30 to 82% depending on the population, dimensions, and criteria used.16,17 Classically, the performance of compulsions has been explained as an anxiolytic mechanism to cope with post-traumatic stress symptoms.15 Furthermore, there is an important line of research on the presence of recent life events (RLEs) at the onset and course of different mental disorders.18–21 Pioneering studies in this regard were those of Khanna et al. (1988),20 who found an excess of life events in the preceding 6 months of the onset of OCD. The experience of such events had a negative impact in the clinical course of the disorder and was described as having a high uncontrollability. More recently, other authors have found that 37.4%22 and 60.8%23 of the patients with OCD reported at least one stressful event that could be related to the onset of the disorder. In a recent cross-sectional study involving 1001 patients, RLEs have been found to be relevant triggers of the onset or exacerbation of obsessive–compulsive symptoms.24
This study aims to assess the presence and persistence of OCSs in a sample of patients with anxiety and depression disorders. It also aims to analyze the relationship between the presence of OCSs with the existence of RLEs and/or TEs.
MethodsDesignThis observational analytical study had two phases: (a) an extensive clinical assessment of a consecutive sample of patients with anxiety and depression disorders. The objective of this phase was to assess the presence of OCSs in the sample and its relationship with RLE and/or TE; (b) a follow-up in the next 6–12 months, with a second clinical assessment. The objective of this phase was to analyze the persistence of OCSs and its association with the severity of depressive and anxious symptoms.
Selection of participantsWe initially selected 248 subjects who attended a first psychiatric evaluation in the Alcalá de Henares district, referred from their primary care physician. The main inclusion criterion was the presence of an anxiety or depressive disorder (always in subjects over 18 years of age). These disorders included the following: major depressive disorder (296.21; 296.22; 296.23; 296.31; 296.32; 296.33), persistent depressive disorder (300.4), and anxiety disorders such as panic disorder (300.01), agoraphobia (300.22), social phobia (300.23), generalized anxiety disorder (300.02), or an adaptive disorder with either symptoms of anxiety (309.22), depression (309.0), or mixed anxious-depressive symptoms (309.28), according to DSM-5 diagnostic criteria. Exclusion criteria were as follows: any psychiatric diagnosis that did not meet DSM5 criteria for the aforementioned disorders, personal history of psychotic disorder, intellectual disability, suffering from a neurological disease other than tics, history of traumatic brain injury and/or serious medical illness, functional illiteracy, psychoactive substance abuse, and refusal to participate. Forty-eight subjects from the initial set were excluded from the study. 32 patients did not fulfill criteria of anxiety or depressive disorder, 6 refused to participate in the study, 7 had psychiatric comorbidity and 3 psychoactive substance abuse.
The study was carried out under the approval of the Research Ethics Committee of the Príncipe de Asturias University Hospital. After reviewing a brief description of the study, the participants gave their written informed consent.
AssessmentsSubjects were included by consecutive sampling, based on the established inclusion criteria. The subjects were assessed during a first psychiatric evaluation (basal evaluation, hereafter), and 6–12 months after the first visit (follow-up evaluation, hereafter). The same battery of tests was applied at both times. We controlled sociodemographic variables, including age, sex, marital status, number of children, level of education, and employment status. Additionally, the presence of perinatal complications and the use of psychoactive substances were recorded.
To establish the severity of the anxiety-depressive symptoms, the following tests were administered:
- •
The Hamilton Anxiety Scale (HARS): a 14-item hetero-applied scale that assesses the degree of anxiety. The Spanish version presents good psychometric properties similar to those of the original scale. The following cutoff points were used in this study: from 0 to 5 points (nonanxiety), from 6 to 13 points (subclinical anxiety), and 14 or more (clinical anxiety).25
- •
The Hamilton Scale for the evaluation of depression (HRSD, 17 items): a hetero-applied scale for the evaluation of depression. The total score ranges from 0 to 54 points. The following cutoff points were made for this study: from 0 to 7 (nondepression), from 8 to 13 (subclinical depression), and equal to or greater than 14 points (clinical depression).26
The presence of associated comorbidity was assessed through the International Neuropsychiatric Interview (MINI), which explores the main psychiatric disorders. MINI consists of a short structured diagnostic interview, which takes about 15min (on average) to be completed. The MINI is considered to have an acceptably high validity and reliability.27
For the evaluation of OCSs, the Revised Obsessive–Compulsive Inventory (OCI-R) was used: a self-applied questionnaire consisting of 18 items. The score ranges from 0 to 72 points, and its structure provides measures of 6 subscales: cleanliness, obsession, accumulation, order, checking, and neutralization. Various studies indicate that the OCI-R has adequate internal consistency, test–retest reliability, and convergent-divergent and discriminant validity, both in clinical and nonclinical samples.28
The evaluation of RLEs (those that occurred during the last 12 months) was carried out using the Recent Life Changes Questionnaire (CVSV): a self-applied questionnaire that presents a list of 61 vital events in different spheres.29 The events described are not necessarily negative; the scale tries to assess the degree of social adjustment that the person must carry out in each situation. TEs were assessed using the Posttraumatic Stress Diagnostic Scale (PDS)30: a self-applied scale that assesses the number of TEs as well as the intensity of post-traumatic stress disorder (PTSD) symptoms.
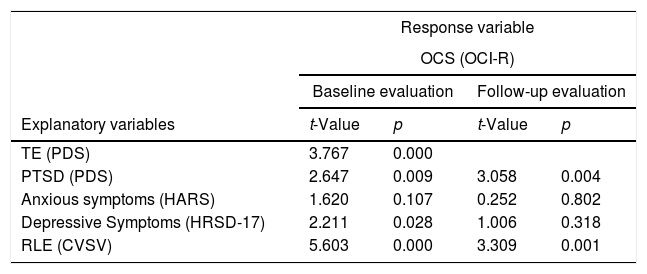
Statistical analysisWe first evaluated the effects of anxiety-depressive syndrome (HARS, HRSD-17), PTSD, and the number of TEs and RLEs on the severity of obsessive–compulsive symptomatology, by fitting Generalized Linear Mixed Models (GLMMs). GLMMs provide a flexible way to model traits that do not satisfy the assumptions of standard linear modeling, allowing the distinction between fixed and random factors in the model.31 We assumed a Poisson error distribution (with a log link function) for the response variable obsessive–compulsive symptomatology, which was consistent with the distribution of the data and is commonly used when modeling count-data32 and OCD-related variables.33 We carried out models for the basal and the follow-up groups separately. The explanatory variables fitted in the model included HARS, HRSD-17, PTSD, RLEs, and TEs, considered as fixed factors (the variable TE was only included in the basal group, since it was only evaluated at the beginning of the study). We accounted for the potential individual variation in OCSs by including the factor “Patient” as a random factor in the model. GLMMs were performed using the function glmm.PQL of the MASS package of R (v.3.2.1; https://www.r-project.org).
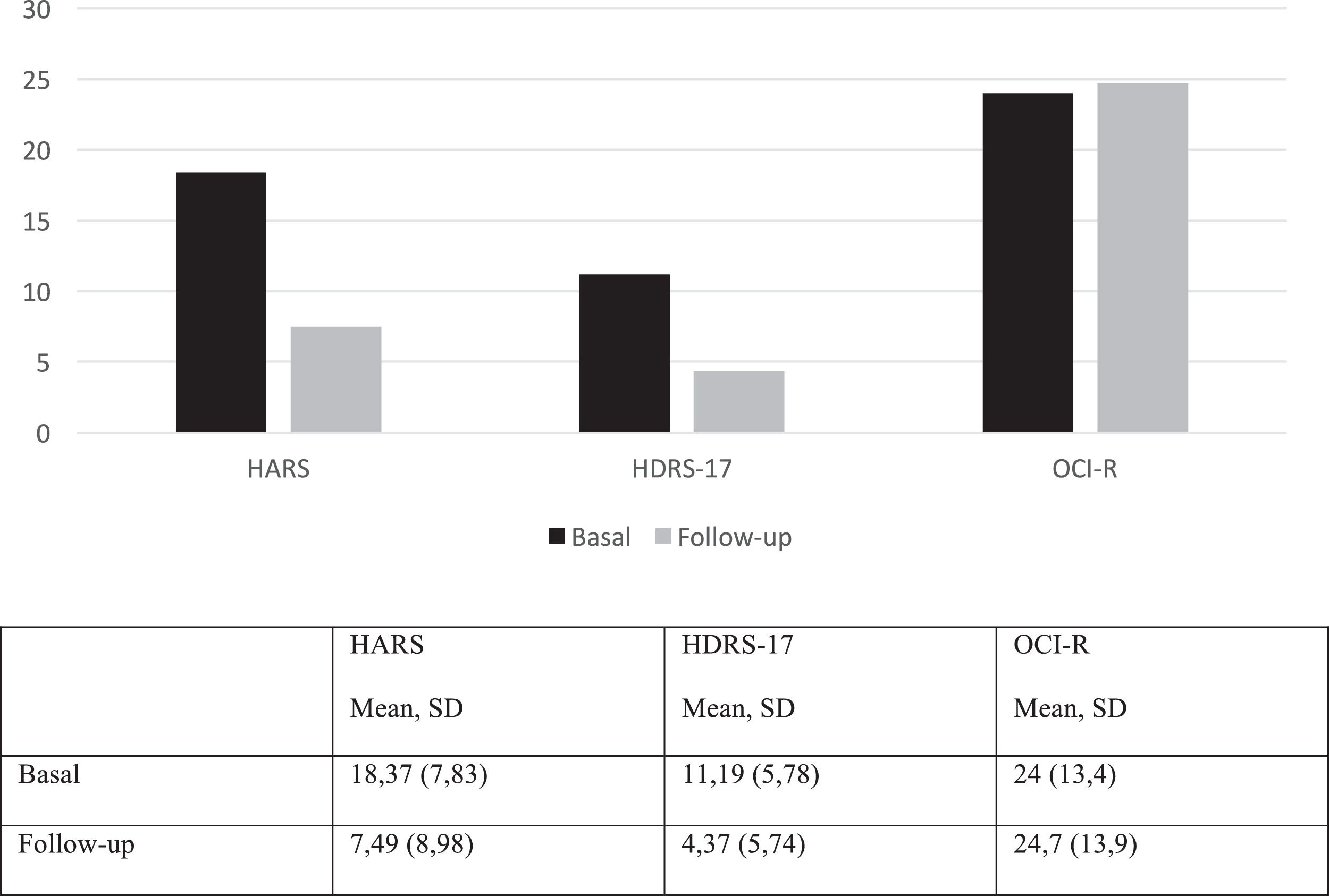
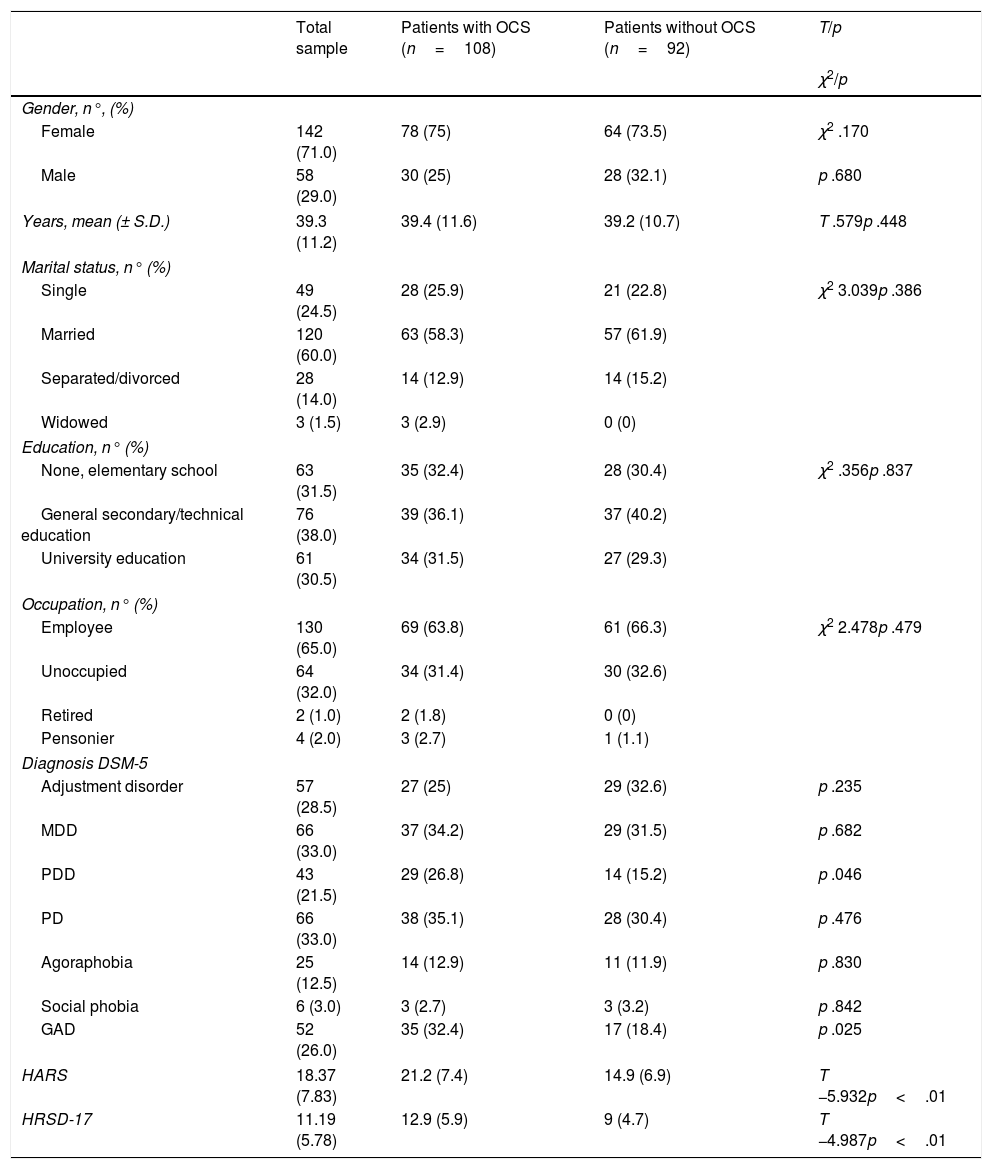
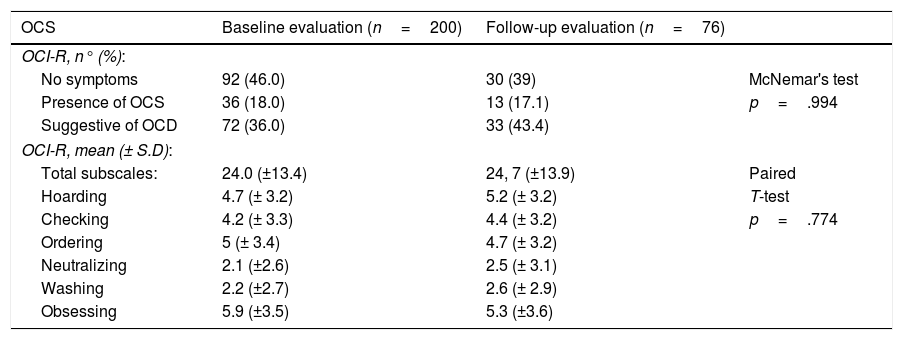
ResultsTable 1 summarizes the clinical and sociodemographic characteristics of the sample at baseline evaluation. Fifty-four per cent of the anxious-depressive outpatients sample endorsed OCSs (OCI-R≥21 points). Of these, 18% presented OCSs in isolation, and 36% met criteria for a probable OCD (OCI-R≥28 points) (Table 2). Regarding the dimensions evaluated in the OCI-R, at baseline evaluation, obsession obtained the highest mean, followed by ordering, accumulation, checking, washing, and neutralization. Likewise, in the follow-up, obsessiveness remained in first place followed by accumulation, order, checking, washing, and neutralization. Patients with OCSs did not show significant differences in sociodemographic characteristics, but they show higher severity in depressive and anxious symptoms and a higher proportion of patients with persistent depressive disorder and generalized anxiety disorder (Table 1). A total of 76 subjects (38% of the initial sample) completed the 6–12 months of follow-up (mean=8.5 months, SD 2.23). A significant decrease was observed in anxious-depressive symptomatology: for the anxiety symptoms, the mean HARS scores were 18.37 (±7.83) at baseline and 7.49 (±8.98) at follow up. For depressive symptoms, the mean HDRS-17 scores were 11.19 (±5.78) at baseline and 4.37 (±5.74) at follow-up (Fig. 1). Among subjects that completed the follow-up, the remission rate for depression was 75.4% (HDRS17≤7).
Sociodemographic and clinical characteristics of the baseline sample (n=200).
| Total sample | Patients with OCS (n=108) | Patients without OCS (n=92) | T/p | |
|---|---|---|---|---|
| χ2/p | ||||
| Gender, n°, (%) | ||||
| Female | 142 (71.0) | 78 (75) | 64 (73.5) | χ2 .170 |
| Male | 58 (29.0) | 30 (25) | 28 (32.1) | p .680 |
| Years, mean (± S.D.) | 39.3 (11.2) | 39.4 (11.6) | 39.2 (10.7) | T .579p .448 |
| Marital status, n° (%) | ||||
| Single | 49 (24.5) | 28 (25.9) | 21 (22.8) | χ2 3.039p .386 |
| Married | 120 (60.0) | 63 (58.3) | 57 (61.9) | |
| Separated/divorced | 28 (14.0) | 14 (12.9) | 14 (15.2) | |
| Widowed | 3 (1.5) | 3 (2.9) | 0 (0) | |
| Education, n° (%) | ||||
| None, elementary school | 63 (31.5) | 35 (32.4) | 28 (30.4) | χ2 .356p .837 |
| General secondary/technical education | 76 (38.0) | 39 (36.1) | 37 (40.2) | |
| University education | 61 (30.5) | 34 (31.5) | 27 (29.3) | |
| Occupation, n° (%) | ||||
| Employee | 130 (65.0) | 69 (63.8) | 61 (66.3) | χ2 2.478p .479 |
| Unoccupied | 64 (32.0) | 34 (31.4) | 30 (32.6) | |
| Retired | 2 (1.0) | 2 (1.8) | 0 (0) | |
| Pensonier | 4 (2.0) | 3 (2.7) | 1 (1.1) | |
| Diagnosis DSM-5 | ||||
| Adjustment disorder | 57 (28.5) | 27 (25) | 29 (32.6) | p .235 |
| MDD | 66 (33.0) | 37 (34.2) | 29 (31.5) | p .682 |
| PDD | 43 (21.5) | 29 (26.8) | 14 (15.2) | p .046 |
| PD | 66 (33.0) | 38 (35.1) | 28 (30.4) | p .476 |
| Agoraphobia | 25 (12.5) | 14 (12.9) | 11 (11.9) | p .830 |
| Social phobia | 6 (3.0) | 3 (2.7) | 3 (3.2) | p .842 |
| GAD | 52 (26.0) | 35 (32.4) | 17 (18.4) | p .025 |
| HARS | 18.37 (7.83) | 21.2 (7.4) | 14.9 (6.9) | T −5.932p<.01 |
| HRSD-17 | 11.19 (5.78) | 12.9 (5.9) | 9 (4.7) | T −4.987p<.01 |
Abbreviations: Major Depressive Disorder (MDD). Panic Disorder (PD). Persistent Depressive Disorder (PDD). Generalized Anxiety Disorder (GAD). Hamilton Anxiety Rating Scale (HARS). Hamilton Depression Rating Scale 17 items (HRSD-17 items).
Persistence of OCS, n° (%), mean (± S.D.) at baseline and follow-up evaluation.
| OCS | Baseline evaluation (n=200) | Follow-up evaluation (n=76) | |
|---|---|---|---|
| OCI-R, n° (%): | |||
| No symptoms | 92 (46.0) | 30 (39) | McNemar's test |
| Presence of OCS | 36 (18.0) | 13 (17.1) | p=.994 |
| Suggestive of OCD | 72 (36.0) | 33 (43.4) | |
| OCI-R, mean (± S.D): | |||
| Total subscales: | 24.0 (±13.4) | 24, 7 (±13.9) | Paired |
| Hoarding | 4.7 (± 3.2) | 5.2 (± 3.2) | T-test |
| Checking | 4.2 (± 3.3) | 4.4 (± 3.2) | p=.774 |
| Ordering | 5 (± 3.4) | 4.7 (± 3.2) | |
| Neutralizing | 2.1 (±2.6) | 2.5 (± 3.1) | |
| Washing | 2.2 (±2.7) | 2.6 (± 2.9) | |
| Obsessing | 5.9 (±3.5) | 5.3 (±3.6) | |
Abbreviations: Obsessive–Compulsive Symptoms (OCS). Obsessive–Compulsive Disorder (OCD). Obsessive–Compulsive Inventory Revised (OCI-R).
Mean (± S.D.) HARS, HDRS-17 and OCI-R scores (mean, SD) at baseline and follow-up evaluation. Abbreviations: Hamilton Anxiety Rating Scale (HARS). Hamilton Depression Rating Scale 17 items (HRSD-17); Revised Inventory of Obsessions and Compulsions (OCI-R); 1 (Baseline evaluation). 2 (Follow-up Evaluation).
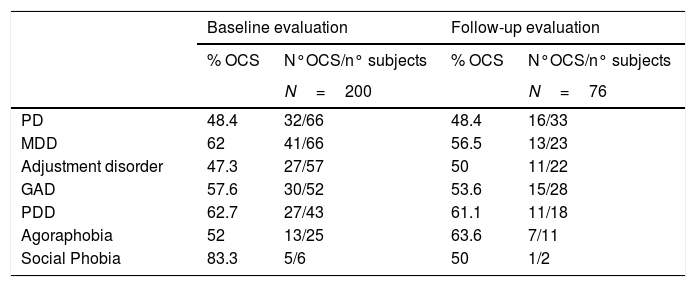
Table 3 shows the percentage of OCSs in the different disorders included in the study at baseline and at follow-up, respectively. The severity of depressive symptoms, measured through HDRS-17, had a statistically significant association (p=0.028) with OCSs. 67% of subjects with subclinical depression (HDRS-17 between 8 and 13) presented OCSs. Anxious symptoms (HARS) were not significantly associated (p=0.107) with the presence of OCS. During follow-up, persistence of OCSs was found in 60.5% of subjects, independently of depressive (p=0.318) and anxious (p=0.802) symptoms.
Prevalence of OCS in the different disorders included in the sample, n° (%), mean (± S.D.) at baseline and follow-up evaluation.
| Baseline evaluation | Follow-up evaluation | |||
|---|---|---|---|---|
| % OCS | N°OCS/n° subjects | % OCS | N°OCS/n° subjects | |
| N=200 | N=76 | |||
| PD | 48.4 | 32/66 | 48.4 | 16/33 |
| MDD | 62 | 41/66 | 56.5 | 13/23 |
| Adjustment disorder | 47.3 | 27/57 | 50 | 11/22 |
| GAD | 57.6 | 30/52 | 53.6 | 15/28 |
| PDD | 62.7 | 27/43 | 61.1 | 11/18 |
| Agoraphobia | 52 | 13/25 | 63.6 | 7/11 |
| Social Phobia | 83.3 | 5/6 | 50 | 1/2 |
Abbreviations: Obsessive Compulsive Symptoms (OCS). Panic Disorder (PD). Major Depressive Disorder (MDD). Generalized Anxiety Disorder (GAD). Persistent Depressive Disorder (PDD). Number of subjects in each diagnostic category (n° subjects) McNemar's test: n.s.
On the other hand, 30.5% of the total sample reported having suffered one or more TEs in their lifetime. The most reported types of TEs were the following: accident (16.5%), nonsexual assault by stranger (11%), sexual assault by family member (9%), nonsexual assault by family member (8%), sexual contact before 18 years (9%), fatal disease (4%), and natural disaster (2.5%). 37% reported “other TE,” including the death of relatives, the breakup of a partner, psychological abuse, and the illness of the children. According to the cut-off scores of the PDS scale, 51.5% of the sample presented some type of PTSD symptomatology: 9% mild, 14% moderate, 18% moderate-severe, and 10.5% severe. The post-traumatic stress symptomatology more frequently reported was avoidance, followed by hyperalertness and re-experimentation, both at baseline assessment and at follow-up. The mean PTSD symptomatology on the PDS scale score was 22.4 (±12.9) at baseline and 17.0 (±13.1) at follow-up. The mean stressful life events (SLEs) was 7.7 during the baseline evaluation and 6.4 at follow-up, respectively. Changes in sleep rhythm and diet were by far the most registered SLE in both evaluations.
During the baseline evaluation, the presence of OCSs (OCI-R≥21) was associated with the following: presence of depressive symptoms (p=0.028), having suffered one or more TE throughout life (p=0.000), and PTSD symptoms (p=0.009), as well as the number of registered SLEs (p=0.000). During follow-up, the persistence of OCSs, independently of depressive symptoms (p=0.318), maintained a strong association with the number of SLEs (p=0.0001). Table 4 shows the results of the multivariate analysis using a GLMM.
Generalized Linear Mixed Models of explanatory variables over the OCSs (response variable).
| Response variable | ||||
|---|---|---|---|---|
| OCS (OCI-R) | ||||
| Baseline evaluation | Follow-up evaluation | |||
| Explanatory variables | t-Value | p | t-Value | p |
| TE (PDS) | 3.767 | 0.000 | ||
| PTSD (PDS) | 2.647 | 0.009 | 3.058 | 0.004 |
| Anxious symptoms (HARS) | 1.620 | 0.107 | 0.252 | 0.802 |
| Depressive Symptoms (HRSD-17) | 2.211 | 0.028 | 1.006 | 0.318 |
| RLE (CVSV) | 5.603 | 0.000 | 3.309 | 0.001 |
Abbreviations: Obsessive–Compulsive Symptoms (OCS). Obsessive–Compulsive Inventory Revised (OCI-R). Traumatic Events (TE). Posttraumatic Stress Diagnostic Scale (PDS). Posttraumatic Stress Disorder (PTSD). Hamilton Anxiety Rating Scale (HARS). Hamilton Depressive Rating Scale 17 items (HRSD-17). Recent Life Events (RLE). Recent Life Changes Questionnaire (CVSV).
Finally, the clinical and sociodemographic characteristics of the patients who completed the follow-up (n=78) were compared with those who only performed the baseline evaluation (n=122), without finding any statistically significant difference. The mean score in HARS in the group that completed the follow-up was 18 (±7.8) and in the group that did not complete it was 18.9 (±7.9) (T=−0.75; p=0.456). The mean HDRS17 scores were 11.3 (±6) and 11.1 (±5.5), respectively (T=0.20; p=0.842). Finally, mean OCI-R scores were 24.9 (±13.2) and 23.9 (±13.2), respectively (T=0.00; p=0.996). There were no differences in the proportion of patients with depression (χ2 1.010; p=.315), adjustment disorder (χ2 1.845; p=.174), dysthymia (χ2 .390; p=.532), agoraphobia (χ2 2.030; p=.154) and generalized anxiety (χ2 .323; p=.570) between both groups. A higher proportion of patients diagnosed with panic disorder (χ2 5.010; p=.025) and social phobia (χ2 5.110; p=.024) was observed in the group that completed the follow-up.
DiscussionThe present study has attempted to assess the prevalence of OCSs in a sample of patients with a set of anxiety-depressive disorders, and to analyze its association with RLEs and TEs. It was found that 54% of the sample of 200 patients with anxious-depressive symptoms had OCSs, with 18% presenting some type of OCS and 36% patients suggesting probable OCD. At the baseline visit, the presence of OCSs is associated with the severity of depressive symptoms, the presence of TEs, the symptoms of post-traumatic stress, and the number of RLEs. At follow-up at 6–12 months, a high persistence of OCSs was found (present in 60.5% of patients), independent of the severity of anxiety-depressive symptoms, but associated with the number of RLEs.
Our findings on the prevalence of OCSs in anxiety/depression are comparable to previous studies,7,8 taking into account the differences in the sample size and methodology. In the previous literature, the presence of OCSs in depressive disorders has been more recognized,34,35 but to a lesser extent in anxiety disorders.36–41 Previous research has focused mainly on panic disorder36,37 and its relationship with hypochondriasis and anticipatory anxiety.38 Our results also show a high presence of OCSs in adaptive disorders (47.3%) or generalized anxiety (57.6%). A characteristic of our transdiagnostic sample of anxious-depressive patients is that it included a high percentage of subclinical depression (33.5%), which almost equaled that of clinical depression (34.5%), with a similar presence of OCSs being found in both entities. This shows that the strong association between depressive symptoms and OCSs is also present when the former appears subclinically. It has been previously described that low mood is associated with the frequency and intensity of intrusive thoughts, so that encoding negative thoughts would lead to the elaboration of rituals to reduce the level of stress.10 Regarding the content of the obsessions, the OCI-R suggests that these are “thoughts that are difficult to control, unpleasant, filthy, or horrible that are not easy to get rid of,” whose description could correspond to any of the cognitive processes (thoughts negatives, worries, obsessions) commonly present in the anxious-depressive population.
In our sample, the most present dimension of the OCI-R was obsession, followed by ordering, accumulation, checking, washing, and neutralization. Likewise, in the follow-up at 6–12 months, obsessiveness remained first. In summary, maladaptive cognitive processes such as rumination, worries, and intrusive memories take place in anxiety-depressive disorders, which share common characteristics with obsessions, such as intrusiveness or the degree of discomfort generated by their content.42–44 Given the frequency with which they usually occur interchangeably in these disorders, it has been proposed that these maladaptive cognitive processes be considered transdiagnostic variables.42,44
At follow-up at 6–12 months, patients presented a significant improvement in anxiety-depressive symptoms with pharmacological treatment. This is congruent with the fact that patients were consecutively recruited through clinical referrals from Primary Care and showed a mild-moderate severity. Most of them began treatment at the time of the assessment or some weeks before, and 28.5% of the sample had the diagnosis of Adaptive Disorder. In contrast with this good outcome in anxiety and depression, we found that OCSs persisted in up to 60.5%. This persistence of OCSs alerts us to the existence of residual symptoms that can be disabling and annoying, and that do not respond adequately to the usual treatment for anxious-depressive symptoms. Authors like Sugarman et al. (2018) expose that OCSs respond, generally speaking, worse to placebo and antidepressants.45 They usually debut before other psychiatric disorders, establishing more rigid and permanent behaviors and, therefore, being more resistant to change.45,46 OCD with comorbid anxiety and depression disorders is associated with a worse prognosis and greater probability of chronicity and disability, an aspect that could be transferred to OCS.46,47 When addressing the presence of TEs, it is noteworthy that 30.5% of the sample reported having suffered one or more TEs throughout their lives. Overall, most of the TEs collected were nonsexual and intentional in nature. In general, interpersonal trauma (e.g., sexual abuse, physical violence) seems to contribute more to the development of psychological symptoms compared to non-interpersonal ones.9
In our study, there was a significant relationship between having presented one or more TEs throughout life and the presence of OCSs. Our results are consistent with previous studies that have indicated the relationship between trauma, whether or not it involves the development of PTSD, and the appearance of OCSs.9–17 The concurrence of OCSs and post-traumatic stress symptoms could be related to the fact that they share formal characteristics such as intrusiveness, unwanted character, repetitiveness, and uncontrollability.17 This strong association between previous OCSs and TEs in anxious-depressive patients would have clinical implications, suggesting the recommendation to systematically ask about TEs and develop transdiagnostic therapeutic strategies focused on resilience to stress and trauma. As a guide, some authors have suggested that therapies based on stress inoculation and prolonged exposure to trauma-related memories are effective in patients with OCD associated with PTSD.17
The presence of OCSs was associated, both in baseline evaluation and in follow-up, with the presence of RLEs. Specifically, the most significant contributing factor to the persistence of OCS is the presence of stressful life events. This underscores the importance of therapeutic strategies based on coping with stress in anxious-depressive patients. However, changes in sleep rhythm and diet were the most registered RLEs. These items correlate excessively with psychopathology, and it is difficult to discriminate to what extent they are environmental risk factors or psychiatric symptoms when applied to clinical populations.48,49 In this study, only the total number of RLEs was taken into account as it was less correlated with the rest of the clinical variables than the degree of adjustment. In the literature reviewed in other fields of study, the number of events that the subject experiences has a decisive influence, as well as its threatening quality and its undesirability.50,51
The main strength of the study is the representativeness of the sample, which was relatively broad and was obtained through consecutive recruitment. The symptomatic evaluation of different nosological entities has allowed us to offer a transdiagnostic view of psychopathology and to explore the relationships between various symptoms.52 The main limitation is the loss of 63% of the sample in the follow-up at 6–12 months, which may have led to an information bias. However, the comparison between the patients who completed the study with the losses to follow-up did not find any sociodemographic or clinical difference.
In conclusion, our findings on the high prevalence and persistence of OCSs in patients with anxiety-depressive disorders, and its association with recent and/or traumatic life events, suggest the realization of new studies on this transdiagnostic psychopathological approach, addressing its nature, diagnosis, clinical relevance, and effective therapeutic strategies.
Funding sourceNo official funding was provided to conduct this study.
Conflict of interestsDr. Cardoner declares that he has received honoraria as consultant, advisor or CME speaker from Janssen, Lundbeck, Pfizer, Exeltis and MSD. Dr. Lahera has been a consultant to or has received honoraria or grants from Janssen-Cilag, Otsuka-Lundbeck, Lilly, Astra-Zeneca, CIBERSAM and Instituto de Salud Carlos III. The rest of authors declare no conflict of interests.