The aim of this study was to gather sources of validity evidence of the Mood Disorder Questionnaire (MDQ) in young adults for its use as a screening tool for bipolar spectrum disorders. The sample was composed of 1002 participants, 268 men (26.7%). The mean age of participants was 21.1 years (SD=3.9). The results showed that between 3 and 59% of the sample reported some hypomanic experience. Gender differences were found in the total score of the MDQ. The analysis of the internal structure by exploratory factor analysis yielded 2 factors, called Energy-Activity and Disinhibition-Attention. This dimensional structure was replicated in the exploratory structural equation modelling (ESEM), and also had factorial equivalence by gender. Participants who met the cut-off points of the MDQ reported a worse perceived mental health status and more consummatory and anticipatory pleasure, compared to the low scores group. These findings indicate that the MDQ has adequate psychometric properties in non-clinical samples, and could be useful as a screening tool in psychopathology, with the possibility of optimising strategies for early identification and prevention in individuals at high risk for bipolar disorders. Future studies should further explore the role of subclinical bipolar phenotype and conduct longitudinal studies in samples of the general population.
El objetivo de este trabajo fue obtener evidencias de validez del Mood Disorder Questionnaire (MDQ) en adolescentes y adultos jóvenes en su uso como instrumento de detección del riesgo para trastornos del espectro bipolar. La muestra la conformaron 1.002 participantes, 268 varones (26,7%). La media de edad de los participantes fue 21,1 años (DT=3,9). Los resultados mostraron que entre un 3 y un 59% de la muestra informó de alguna experiencia hipomaníaca. Se encontraron diferencias en función del género en la puntuación total del MDQ. El análisis de la estructura interna, mediante análisis factorial exploratorio, reveló la presencia de 2 factores, denominados Energía-Actividad y Desinhibición-Atención. Esta estructura factorial fue replicada en el modelo exploratorio de ecuaciones estructurales y se mostró invariante en función del género. Los participantes que cumplieron el punto de corte del MDQ informaron de un peor estado de salud mental percibida y una mayor experiencia de placer anticipatorio y consumatorio que el grupo de comparación. Estos hallazgos indican que el MDQ presenta una adecuada calidad psicométrica y que podría ser útil como herramienta de cribado psicopatológico, con la posibilidad de optimizar las estrategias de identificación y prevención temprana en participantes de riesgo de padecer trastornos del espectro bipolar. Futuros estudios deberían seguir analizando el papel del fenotipo bipolar subclínico, así como llevando a cabo seguimientos longitudinales en muestras de población general.
Bipolar spectrum disorders are a set of incapacitating mental disorders that cause a high burden in terms of morbidity, associated disability and economic costs for society.1–5 These disorders have a prevalence of 2.4%, and the symptoms usually begin in late adolescence and early adulthood.1 Most cases are preceded by a prodromal period (for example, sleep alterations, irritability, anxiety, signs and symptoms of depression and mania), which lasts from 1.8 to 7.3 years on average.6–8 Longitudinal studies carried out with individuals in the general population show that the presence of persistent hypomanic experiences increases the long-term likelihood of developing a clinical condition.9–11 Untreated bipolar disorder normally lasts an average of some 6 years.12 This delay in identifying the clinical picture is associated with, among other aspects, greater depressive symptomatology and suicide attempts, as well as worse long-term progression.12 Likewise, early intervention in patients with bipolar disorder is linked to better functional results,13–15 as well as better response to psychiatric mood stabilising drugs.16
These results demonstrate that identification and early intervention for (hypo)manic symptoms and experiences in the general population or in high-risk groups, as well as in health care and clinical settings, would be a relevant task.8,17 Helping health care professionals to detect this set of experiences early, both at the clinical and subthreshold levels, is a highly interesting goal with clear practical implications.3,18 Likewise, if identifying individuals at risk of being affected by bipolar spectrum disorders is possible, it might allow us to analyse different markers of risk and protection, as well as the underlying etiopathogenic mechanisms. This would improve understanding of the disorder, design of therapeutic targets and resource management. To this end, it is necessary to provide detection tools that let the professional make valid, well-founded decisions based on the score on them. Logically, assessment tools have to be adapted and validated for a specific context and population, and their psychometric properties have to back their administration and use. The goal of such tools is no other than that of studying, analysing, identifying, diagnosing and following up bipolar spectrum disorder symptoms at both clinical and subclinical levels. Various different measurement instruments have been developed for the study, identification and diagnosis of the symptoms of bipolar spectrum disorders.17,19 The Mood Disorder Questionnaire (MDQ),20 the Bipolar Spectrum Diagnostic Scale21 and the 32-Hypomania Check-List22 are clear examples.
Specifically, the MDQ20 is a tool designed to assess hypomanic symptomatology based on the DSM-IV criteria for bipolar disorder. It consists of 13 items in all to do so, plus 2 others that assess concurrence in time of various symptoms and the seriousness of the problems. The MDQ has been widely used in clinical contexts (including primary care) and in the general population.17,19,23,24 Its psychometric properties have been analysed in clinical samples, with its sensitivity and specificity values being of special interest. It is also being used currently as an epidemiological and screening tool for hypomanic experiences and symptoms in samples from the general population.25–28 Previous psychometric studies with non-clinical samples revealed appropriate levels of internal consistency and test-retest. In addition, these studies reflected a 2-dimensional factor structure, materialised in the factors energised-activity and irritability-racing thoughts, or energy and acceleration.25,28 Other studies have replicated this underlying 2-factor structure using confirmatory factor analyses.29 This structure is convergent with that found in diagnosed patients.30,31 Another matter is that some authors have questioned the validity of the MDQ as a screening instrument because of the low levels and sensitivity and/or specificity found in non-clinical samples.25 Specifically in Spain, the MDQ has been validated in patient samples,31,32 where adequate psychometric properties referring to reliability and evidence of validity. The questionnaire has also been used as a screening measure in primary care.33
As can be seen, there are currently few studies that analyse the psychometric quality of MDQ scores in non-clinical samples of adolescents and young adults.19 Likewise, there are specific aspects about measurement that have not yet been studied in detail. Examples of this are the incorporation of the exploratory structural equation model (ESEM),34 the analysis of measurement invariance35 or response item theory. As Sanchez-Moreno et al.31 indicate, it would be interesting to carry out new studies that make it possible to assess in detail the metric quality of this measurement instrument as a screening tool during adolescence and early adulthood, periods of special risk for presenting various psychopathological symptoms.36–38 Likewise, it would be interesting to analyse the phenotype expression of hypomanic experiences in this segment of the population as a possible phenotypic marker indicating bipolar spectrum disorder risk.
Within this research context, the purpose of our study was to obtain evidence of MDQ validity in a non-clinical sample of Spanish adolescents and young adults. To this end, the rates of positively screened patient-reported experiences were analysed, the internal structure of the instrument and its measurement invariance by sex were examined, and score reliability and measurement accuracy were estimated. Likewise, the obtained evidence of validity in relation to other variables was obtained. This objective allowed us to examine the psychometric quality of the MDQ more in depth in its validation in Spanish, with an eye to the possibility of it being used as a screening method for severe mental disorders graves, specifically bipolar spectrum ones. Our hypothesis was that MDQ scores would present adequate psychometric behaviour for this task. Likewise, based on previous studies, we hypothesised that we would find a 2-dimensional structure and that this underlying structure would be invariant by sex. Finally, we hypothesised that MDQ scores would be related to the perceived mental health state and with consummatory and anticipatory pleasure.
MethodParticipantsAn incidental sample of adolescents and young adults was used in this study. The sample consisted of a total of 1002 participants, 268 males (26.7%) studying at the Universidad de La Rioja (Spain) in the fields of Elementary and Secondary Teaching, Information Technology, Mathematics, Social Work, Economics or University Teaching. The mean participant was 21.11 years (Standard Deviation [SD]=3.9); the participants ranged from 17 to 35 years old. In the sample, 44.9% had an age equal to or less than 19 years. Mean number of years of education was 16.8 (SD=2.3). From the total, 1.1% of the sample reported that a first-degree relative had been diagnosed with a psychotic disorder, while 9.5% indicated that some first-degree relative had a history of some type of mental disorder. As for marital status, 57.6% of the sample were single, 36.9% lived in an intimate partner relationship, 2.9% were married, 0.2% were divorced, and 1.7% gave no information about their marital status. With respect to employment, 86.6% of the participants were unemployed, 12.6% were employed, and 1.2% did not report their employment status. To perform the crossed validation study, the sample was randomly divided into 2 subsamples (n=501). The first subsample had a mean age of 21.08 years (SD=3.87) (129 males); the mean age in the second subsample was 21.33 years (SD=3.98) (139 males). No statistically significant differences were found by sex (χ2=0.509, P=.475), years of education (t(1.000)=−0.640, P=.522) and age (t(1.000)=−0.217, P=.828) between the 2 subsamples.
InstrumentsMood Disorder Questionnaire (MDQ).20 The MDQ consists of 13 yes/no items based on the DSM-IV criteria for bipolar disorder. A result was considered positive if the participant replied affirmatively to 7 or more items of the 13 proposed and if, in addition, the symptoms described occurred during the same time period (Criterion 2) and represented moderate or severe problems (Criterion 3). Some authors also consider a result positive when 7 or more items receive an affirmative answer, which is given concurrently in time (Criterion 2). In this screening system, the presence of severity of problems, because that is not considered a diagnostic criterion within the DSM-IV and a few previous studies find better levels of sensitivity and specificity. In our study, we used the version adapted to Spanish and validated in patients and in primary care.31–33
General Health Questionnaire-12 (GHQ-12).39 This questionnaire is a screening tool designed to detect individuals that may be diagnosed with a mental disorder. It is also used as a measure of perceived mental health state. The GHQ-12 consists of a total of 12 items that assess the severity of the mental health problems over the preceding 4 weeks. The items are in the format of 4-point Likert answers. The correction system used in our study was 0–1–2–3. The Spanish version of the GHQ-12 presents appropriate levels of internal consistency as well as several measures of evidence of validity.40,41
Temporal Experience of Pleasure Scale (TEPS).42 The TEPS is an instrument designed to assess anticipatory and consummatory components of pleasure. It has also been used as an indirect measure of anhedonia.43 It consists of 18 items divided into 2 subscales that assess anticipatory pleasure (10 items) and consummatory pleasure (8 items). The TEPS answer format is a 6-point Likert scale ranging from 1 (very false for me) to 6 (completely true for me). The TEPS has been used widely and its properties have been analysed in both clinical and non-clinical samples.44–46 In this study, we used the version adapted to and validated for Spanish following international standards.47
ProcedureThe measurement instruments were administered collectively, in groups of 10–45 students, during the normal educational schedule and in a room adapted for this purpose. The study was presented to the participants as research on various features of personality, guaranteeing the confidentiality of their answers and indicating that participation was voluntary. Informed consent was obtained for participants that were minors. The self-reports were administered under the researchers’ supervision at all times. This study lies within the framework of 2 wider lines of investigation related to early detection of severe psychological disorders in adolescents and young adults in the general population. The Ethics Committee at the Universidad de La Rioja approved the study.
Data analysisFirst of all, the descriptive statistics for the MDQ items were calculated, along with the percentage of positives based on the point cut-offs recommended in the literature.
Secondly, to examine the internal structure48 of the MDQ, a crossed validation study was performed, dividing the total sample randomly into 2 subsamples. In the first subsample, an exploratory factor analysis was carried out using the minimum rank factor analysis method with posterior Promax rotation. Given the dichotomous character of the answer options, factor loads were estimated from the tetrachoric correlation matrix. To determine the number of dimensions, the procedure used was the optimal implementation of the parallel analysis.49
Next, various confirmatory factor analyses were performed in the second subsample. Different dimensional models were tested. The first model considered the presence of a single general dimension general that could explain all the underlying symptomatology. The second model proposed the 2 general dimensions, resulting from the exploratory factor analysis. The third model postulated a 2-dimensional ESEM. The ESEM model makes it possible to solve some of the problems associated with confirmatory factor analysis, such as cases in which no satisfactory goodness-of-fit indexes are found or that modify the hypothesised models (for example, correlating error terms), to improve goodness-of-fit indexes.34 All the factor loads are estimated in the ESEM model, while specific restrictions are imposed on the parameters in confirmatory factor analysis. Likewise, adjusting ESEM models to the data are evaluated with the goodness indexes of the usual ajustments.34 Our method of estimation for the confirmatory models was the weighted least squares mean and variance adjusted statistics. We used the polychoric correlation matrix. In the case of the ESEM model, the rotation method was Geomin.
The goodness-of-fit indexes used were the comparative fit index (CFI), the Tucker-Lewis index, the root mean square error of approximation and la weighted root mean square residual. For a good fit of the data to the model, the CFI values and Tucker-Lewis index should be above 0.95, and the values of the root mean square error of approximation should be lower than 0.08 for a reasonable fit and lower than 0.05 for good fit.50 For the weighted root mean square residual, adequate values are considered to be those lower than 1.0. In our next step, a study on measurement invariance by sex was carried out with the factor model that showed the best goodness-of-fit indexes. To do so, we followed the steps of successive restriction of parameters.35 Measurement invariance, or factor equivalence, tests whether the factor structure of the measurement instrument is equivalent based on the groups to be compared.51
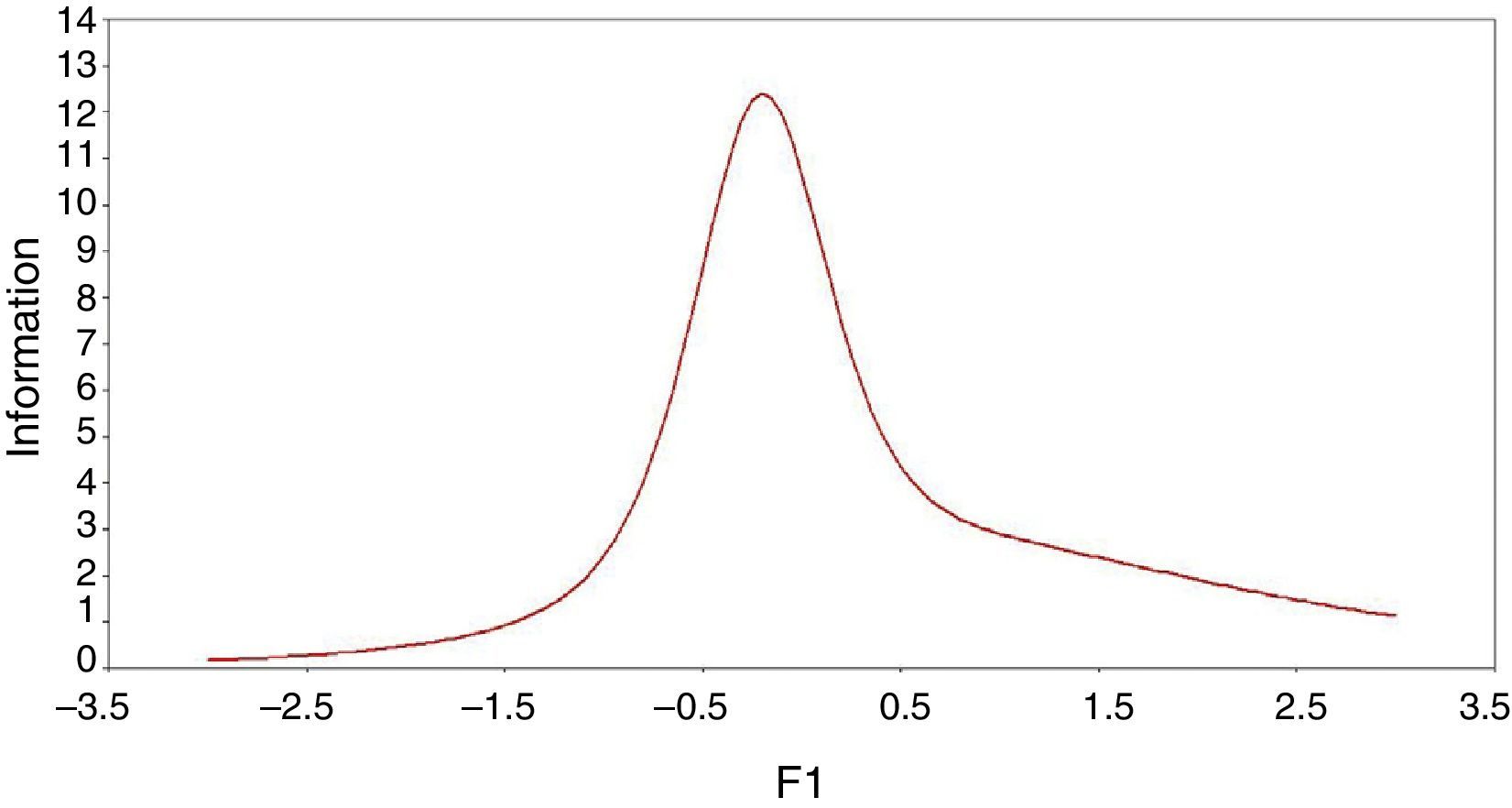
The fourth step was estimating the ordinal alpha that would permit adequate estimation when the item scores were ordinal or dichotomous in nature.52 As an indicator of accuracy of the measurement instrument, the information function was also calculated from the viewpoint of the item response theory.53 The information function makes it possible to analyse the accuracy with which the construct is measured based on the individual's position (score) in the latent variable (for example, risk of bipolar disorder).
Next, to obtain evidence of validity in relation to other variables, the relationship between the MDQ and the GHQ-12 and the TEPS was examined. To do so, we chose 2 extreme groups, participants with scores below the 10th percentile and with a positive screening (Criterion 2).
For the data analysis, we used the SPSS 15.0,54 FACTOR 9.155 and Mplus 7.056 programmes.
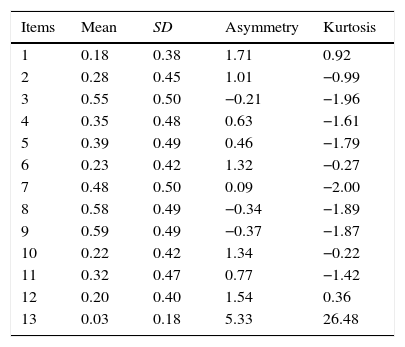
ResultsDescriptive statistics and prevalenceTable 1 shows the descriptive statistics for the MDQ items referring to the mean, SD, asymmetry and kurtosis in the total sample. As reflected in Table 1, the percentage of participants that responded affirmatively to a MDQ item ranged from 3% to 59% of the sample. For dichotomous items, the value of the item mean multiplied by 100 corresponds to the percentage of participants that responded affirmatively to that item. The percentage of participants that responded to 7 or more MDQ items affirmatively was 23.9%; if the criterion of time concurrence of the 2 symptoms was added, the percentage was 19.2%, while if the criterion of moderate or severe problems was added, the figure dropped to 3.4%.
Descriptive statistics for the Mood Disorder Questionnaire items for the sample total (n=1002).
| Items | Mean | SD | Asymmetry | Kurtosis |
|---|---|---|---|---|
| 1 | 0.18 | 0.38 | 1.71 | 0.92 |
| 2 | 0.28 | 0.45 | 1.01 | −0.99 |
| 3 | 0.55 | 0.50 | −0.21 | −1.96 |
| 4 | 0.35 | 0.48 | 0.63 | −1.61 |
| 5 | 0.39 | 0.49 | 0.46 | −1.79 |
| 6 | 0.23 | 0.42 | 1.32 | −0.27 |
| 7 | 0.48 | 0.50 | 0.09 | −2.00 |
| 8 | 0.58 | 0.49 | −0.34 | −1.89 |
| 9 | 0.59 | 0.49 | −0.37 | −1.87 |
| 10 | 0.22 | 0.42 | 1.34 | −0.22 |
| 11 | 0.32 | 0.47 | 0.77 | −1.42 |
| 12 | 0.20 | 0.40 | 1.54 | 0.36 |
| 13 | 0.03 | 0.18 | 5.33 | 26.48 |
SD, standard deviation.
No statistically significant sex-based differences were found among the participants that fulfilled the 3 criteria (χ2=2.371; P=.124). However, significant sex-based differences were indeed found when the criterion was either a score equal to or greater than 7 (χ2=7.248; P=.007), or 7 or more items plus symptom time concurrence (χ2=4.461; P=.037). In these 2 cases, there were more males than females that exceeded the recommended cut-off criteria. From a dimensional point of view, the males also presented greater mean total MDQ scores than the women did (Mmale=4.73, DTmale=3.10; Mfemale=4.28, DTfemale=2.85); these differences were statistically significant (t(1.000)=2,286; P=.022).
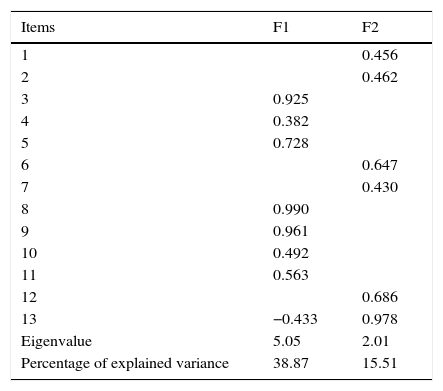
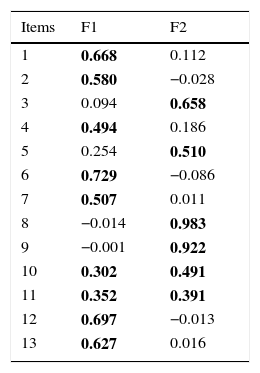
Evidence of internal MDQ structure: exploratory and confirmatory factor analysisIn the first subsample, an exploratory factor analysis was carried out with the 13 MDQ items. The index for Bartlett's test of sphericity was 1172.7 (P<.001), and the Kaiser–Meyer–Olkin value was 0.80. The optimal implementation of the parallel analysis advised extracting 2 factors that explained 54.37% of the total variance. The first factor was called Energy-Activity, while the second was Disinhibition-Attention. The correlation between the 2 factors was 0.47 (P<.05). The root mean square residual was 0.07. The estimated factor loads for the 2-dimensional solution, as well as the values greater than 1 and the variance percentage explained for each factor are shown in Table 2.
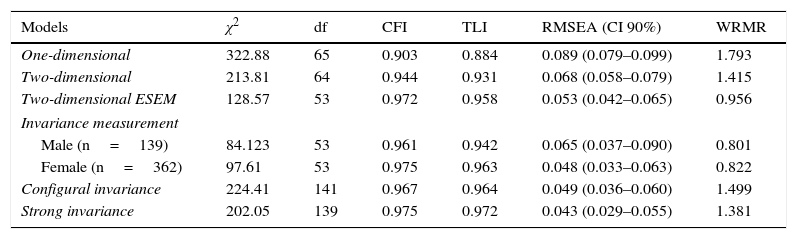
In the second subsample, we performed various confirmatory factor analyses, in which we tested 3 dimensional models. Table 3 shows the goodness-of-fit indexes for the hypothetical models put to test. As can be seen, the dimensional model that presented the best goodness-of-fit indexes was the ESEM 2-factor model. The distribution and weight of the factor loads for the ESEM model were close to those found in the exploratory factor analysis. The resulting standard factor loads are shown in Table 4. They were all statistically significant (P<.01). That most of the estimated factor loads were greater than 0.30 is worth noting. Two items had factor loads above 0.30 in the 2 factors. The Pearson correlation between the 2 dimensions was, likewise, sadistically significant (r=0.45; P<.01).
Goodness-of-fit indexes from the confirmatory factor analysis of the Mood Disorder Questionnaire and measurement invariance by sex for the second subsample (n=501).
| Models | χ2 | df | CFI | TLI | RMSEA (CI 90%) | WRMR |
|---|---|---|---|---|---|---|
| One-dimensional | 322.88 | 65 | 0.903 | 0.884 | 0.089 (0.079–0.099) | 1.793 |
| Two-dimensional | 213.81 | 64 | 0.944 | 0.931 | 0.068 (0.058–0.079) | 1.415 |
| Two-dimensional ESEM | 128.57 | 53 | 0.972 | 0.958 | 0.053 (0.042–0.065) | 0.956 |
| Invariance measurement | ||||||
| Male (n=139) | 84.123 | 53 | 0.961 | 0.942 | 0.065 (0.037–0.090) | 0.801 |
| Female (n=362) | 97.61 | 53 | 0.975 | 0.963 | 0.048 (0.033–0.063) | 0.822 |
| Configural invariance | 224.41 | 141 | 0.967 | 0.964 | 0.049 (0.036–0.060) | 1.499 |
| Strong invariance | 202.05 | 139 | 0.975 | 0.972 | 0.043 (0.029–0.055) | 1.381 |
CFI, comparative fit index; CI, confidence interval; df, degrees of freedom; ESEM, exploratory structural equation model; RMSEA, root mean square error of approximation; TLI, Tucker-Lewis index; WRMR, weighted root mean square residual; χ2, Chi squared.
Standard factorial loads from the ESEM model for the second subsample (n=501).
| Items | F1 | F2 |
|---|---|---|
| 1 | 0.668 | 0.112 |
| 2 | 0.580 | −0.028 |
| 3 | 0.094 | 0.658 |
| 4 | 0.494 | 0.186 |
| 5 | 0.254 | 0.510 |
| 6 | 0.729 | −0.086 |
| 7 | 0.507 | 0.011 |
| 8 | −0.014 | 0.983 |
| 9 | −0.001 | 0.922 |
| 10 | 0.302 | 0.491 |
| 11 | 0.352 | 0.391 |
| 12 | 0.697 | −0.013 |
| 13 | 0.627 | 0.016 |
Factorial loads higher than 0.30 are shown in bold type.
We next tested the measurement invariance hypothesis based on sex for the 2-dimensional ESEM model. As shown in Table 3, the resulting goodness-of-fit indexes for both males and females were appropriate. These results indicated that the data fit the model in the 2 groups and, consequently, that performing the analysis of factor equivalence is possible. The model of configural measurement invariance presented adequate goodness-of-fit indexes. This model is considered the baseline against which the case of strong measurement invariance (more restrictive) is considered. Likewise, the strong measurement invariance model in which the parameters were restricted was also adequate. The ΔCFI was less than 0.01, which led us to accept the strong measurement invariance hypothesis for the 2-dimensional ESEM model of the MDQ by sex.
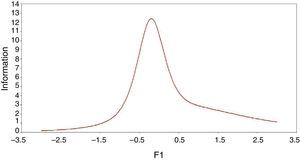
Estimation of the internal consistency of the MDQ scoresIn the first subsample, the ordinal alpha for the first dimension was 0.94 and it was 0.89 for the second. In the second subsample, the figures were 0.93 and 0.86, respectively. Fig. 1 reflects the information function for the total MDQ score from the TRI. As can be seen, measurement instrument evaluates with mayor precision the mean values of the latent variable more accurately.
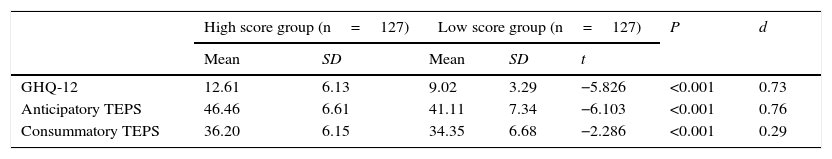
Evidence of validity in relation to external variablesTable 5 shows the mean scores on the GHQ-12 and the TEMPS for the participants that exceeded the 2 MDQ criteria and for those with scores lower than the 10th percentile. The participants that exceeded the MDQ cut-off point showed a worse state of perceived mental health, as well as greater mean scores in the capacity to experience anticipatory and consummatory pleasure, compared with the low-scoring group.
Comparison of means on the General Health Questionnaire-12 and on the temporal experience of pleasure scale of the participants having high and low scores on the Mood Disorder Questionnaire.
| High score group (n=127) | Low score group (n=127) | P | d | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | |||
| GHQ-12 | 12.61 | 6.13 | 9.02 | 3.29 | −5.826 | <0.001 | 0.73 |
| Anticipatory TEPS | 46.46 | 6.61 | 41.11 | 7.34 | −6.103 | <0.001 | 0.76 |
| Consummatory TEPS | 36.20 | 6.15 | 34.35 | 6.68 | −2.286 | <0.001 | 0.29 |
d, Cohen's d; GHQ-12, General Health Questionnaire-12; SD, standard deviation; TEPS, Temporal Experience of Pleasure Scale.
One of the most promising lines in the health field is the prevention of mental disorders based on early detection and early intervention. Accurately and validly identifying the risk for bipolar spectrum disorders becomes a major line of action. The main objective of our study was to obtain new evidence of MDQ validity in a non-clinical sample of adolescents and young adults. To this end, we analysed the rates of subclinical experiences of the bipolar phenotype, examined the internal structure, estimated score reliability and accuracy and obtained various cases of evidence of validity with external variables. All of this makes it possible to know the psychometric properties of the MDQ in non-clinical samples for its possible use as a screening instrument for an age group at special risk of developing severe mental disorders. Along the same lines, this study provides new empirical evidence on the distribution and phenotypic expression of this symptomatology at the subclinical level. It also provides such evidence of the links with other clinical and personality variables. The results seem to indicate that the MDQ scores presented adequate psychometric behaviour in this sample and demonstrate that the MDQ could be used as a short, simple screening tool to evaluate hypomanic experiences in the non-clinical adolescent and young adult population.
The prevalence of hypomanic experiences ranged between 3% and 59%, with the percentage of participants reaching the cut-off point of 2 criteria being 19.2%, and that of 3 criteria, 3.4%. Likewise, the males presented greater mean total MDQ scores than the females. Epidemiological studies carried out using general population samples (depending on the cut-off point used) found similar prevalence rates.26,27,29 For example, Hirschfeld et al.,26 in a national United States study, found prevalence ranging from 7.3% to 36% for this type of experiences. In another Hirschfeld et al. study27 positive screening prevalence of 3.7% was found. In Spain, specifically with a sample of primary care patients, the ratio of 11.9% was found, with the percentage of participants having positive screening being greater for the males.33 In non-clinical samples, it seems that this type of experiences are fairly common and are usually transitory. Previous studies have indicated that the subclinical or attenuated forms of the bipolar phenotype precede the development of bipolar spectrum disorders,9,57 which opens the door to early detection and early intervention.
The analysis of the internal structure of the MDQ revealed the presence of 2 factors called Energy-Activity and Disinhibition-Attention. With certain nuances, this 2-dimensional structure was replicated in the ESEM model and, in addition, revealed its sex-based factor equivalence. It is worth noting that until now few studies had examined MDQ scores from ESEM models or paying attention to measurement invariance. Previous studies carried out on non-clinical population samples have found factor structures with 229 and 328 factors. For example, Carta et al.,29 performing an exploratory and confirmatory factor analysis, found a 2-factor structure similar to the one reported in this study. This 2-factor structure has also been found in diagnosed patients diagnosticados.30,31,58,59 This indicates a certain phenotypic parallelism between the structures found at clinical and subclinical levels. For example, Sanchez-Moreno et al.,31 in a study using Spanish patients, found a 2-factor structure quite close to the one found in our research. Pending new factor studies, our results seem to indicate that the structure underlying the MDQ scores is explained by 2 related dimensions.
Our reliability values, estimated using alpha for ordinal data, were appropriate, above 0.86. Likewise, the information function showed that the latent variable (bipolar phenotype or risk of bipolar disorder) was measured with greater accuracy in the mean values. This demonstrates that the MDQ accurately measures the sample participants that obtain scores in the middle values of the dimensional continuum. Previous studies using general population samples have found levels of internal consistency for the total MDQ score above 0.75.25–28 Equivalent results have been found when levels of internal consistency examining samples of patients with bipolar disorder.30,31,59,60 Nevertheless, as far as we know, no previous study had examined the reliability of the MDQ scores using the alpha for ordinal data or from the perspective of the TRI. Incorporating new forms of measuring MDQ reliability is of interest. It also makes it possible to improve the gathering of evidence of validity to a certain extent, as well as making decisions (such as selecting participants at risk). For example, the analysis of the test information function permits ascertaining the levels at which the latent variable is measured with greatest accuracy and consequently allows us to chose participants based on their position in that continuum.
Another point is that the participants with high MDQ scores reported worse levels of perceived mental health and well-being, and showed greater scores in their capacity to experience anticipatory and consummatory pleasure. These results indicate that, at the subclinical level, there is an impact on the perceived mental health of the young people that self-reported greater bipolar phenotype symptomatology. It should be mentioned that at present there are few studies that have examined the relationship between MDQ scores and different clinical variables in general population samples. For example, studies carried out in Spain in the context of primary care indicate that participants with a positive MDQ screen presented worse quality of life, evidenced social, work and family dysfunction and had greater levels of perceived stress.33 Likewise, and considering that the study of early detection of bipolar spectrum disorders is in its initial phases,3 it is possible that some of the participants with a positive MDQ screen may have greater latent vulnerability (at a theoretical level) to developing this type of clinical picture, and that the combination with other environmental factors (such as substance use, stress, trauma or uncontrolled urban development), along with the presence of associated discomfort, worry or disability, causes such experiences to last longer and brings about a mental state at risk; these factors might then lead the participants to clinical symptomatology and the need for treatment.8,9 This type of attenuated experiences could be used in conjunction with other risk markers to improve our understanding of the underlying etiopathogenic mechanisms and help to predict bipolar spectrum disorders.
Our study results should be interpreted in the light of several limitations. In the first place, the sample characteristics make it impossible to generalise the results to other populations of interest. The sample used consisted of technical institute/university students, with a high ratio of females, an aspect that somewhat limits the generalisation of our findings. It would certainly be worthwhile to carry out our studies using other samples and populations of interest. Another limitation is the issue inherent in applying any type of self-report. Consequently, it would have been interesting to use external informants (for example, hetero-reports) or laboratory measures (such as psycho-physiological ones). A third limitation is that nothing was done to control social desirability or random response patterns, aspects that might affect the results found. In fourth place, this type of self-report and studies for detecting the risk of severe mental disorders may generate a certain stigma, an aspect that should be remembered when interpreting and generalising the results found.
Future studies should carry out longitudinal follow-ups and determine the predictive value of this set of experiences and symptoms in samples representative of the general population. Likewise, it would be of interest to analyse the relationship between different markers of risk and endophenotypes and the subclinical phenotypic expression of bipolar spectrum symptoms.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
FundingThis research was funded by the Spanish Ministry of Science of Innovation (MICINN), the Carlos III Institute and Biomedical Research Networking Centre for Mental Health (CIBERSAM). Project references: PSI 2011-28638 and PSI 2011-23818.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Fonseca-Pedrero E, Ortuño-Sierra J, Paino M, Muñiz J. Detección del riesgo para los trastornos del espectro bipolar: evidencias de validez del Mood Disorder Questionnaire en adolescentes y adultos jóvenes. Rev Psiquiatr Salud Ment (Barc.). 2016;9:4–12.