Help-seeking for mental disorders is a complex process, which includes different temporary stages, and in which the motivational variables play an especially relevant role. However, there is a lack of instruments to evaluate in depth both the temporary and motivational variables involved in the help-seeking process. This study aims to analyse in detail these two sets of variables, using a specific instrument designed for the purpose, to gain a better understanding of the process of treatment seeking.
Material and methodsA total of 152 patients seeking treatment in mental health outpatient clinics of the NHS were individually interviewed: 71 had Obsessive-Compulsive Disorder, 21 had Agoraphobia, 18 had Major Depressive Disorder), 20 had Anorexia Nervosa, and 22 had Cocaine Dependence. The patients completed a structured interview assessing the help-seeking process. Disorder severity and quality of life was also assessed.
ResultsThe patients with agoraphobia and with major depression took significantly less time in recognising their mental health symptoms. Similarly, patients with major depression were faster in seeking professional help. Motivational variables were grouped in 3 sets: motivators for seeking treatment, related to the negative impact of symptoms on mood and to loss of control over symptoms; motivators for delaying treatment, related to minimisation of the disorder; and stigma-associated variables.
ConclusionsThe results support the importance of considering the different motivational variables involved in the several stages of the help-seeking process. The interview designed to that end has shown its usefulness in this endeavour.
La búsqueda de ayuda profesional por enfermedad mental es un proceso complejo, con etapas y momentos temporales diferentes, en el que desempeñan un papel especialmente relevante los aspectos motivacionales. Sin embargo, no hay instrumentos de evaluación que permitan valorar tanto las variables temporales como las motivacionales. El objetivo de este estudio es ofrecer información detallada sobre ambos conjuntos de variables, mediante un instrumento específicamente diseñado para ello, de tal manera que se pueda comprender mejor el proceso de búsqueda de tratamiento.
Material y métodosParticiparon 152 pacientes ambulatorios que habían solicitado ayuda profesional en una unidad de salud mental del SNS. Los diagnósticos principales fueron: trastorno obsesivo-compulsivo (n=71), agorafobia (n=21), trastorno depresivo mayor (n=18), anorexia nerviosa (n=20) y dependencia a cocaína (n=22). Los pacientes fueron evaluados mediante una entrevista estructurada, específicamente diseñada para el estudio. Asimismo, se obtuvieron datos sobre gravedad y calidad de vida.
ResultadosLos pacientes con agorafobia y depresión mayor tardaron menos en reconocer los síntomas que los pacientes de los otros grupos. Asimismo, los pacientes con depresión mayor demoraron menos en solicitar ayuda profesional. Las variables motivacionales se agruparon en 3 conjuntos: motivos de consulta, relacionados con el malestar y la falta de control; motivos de demora de la consulta, relacionados con la minimización del problema; y motivos asociados al estigma.
ConclusionesLos resultados indican la necesidad de valorar las distintas variables motivacionales implicadas en las diferentes etapas del proceso de búsqueda de ayuda profesional. La entrevista que presentamos ha mostrado ser útil para ello.
People who suffer from a mental disorder, and often those close them, face complex decisions as to how to approach their distressing condition and this may or may not lead them to seek professional help. The “path” providing access for patients to specialist healthcare professionals is not always direct and immediate, because it is very dependent on the extent of activation and direction when the process is started, and on how persistently it is followed. In this regard, it is very probable that the type of distress and its severity play a major role in motivating the search for help. Other elements ranging from sociodemographic aspects to attitudes, beliefs and values regarding mental disorders and illnesses and their treatment, held by both the sufferer and the people close to them, will determine where this search will be directed.
The difficulty in deciding to seek professional help is reflected in the low percentage of people with a mental disorder that seek treatment, despite great distress and impaired quality of life,1 even though they are aware that they need help. Published studies indicate that this percentage varies between 23.3% and 41%,2–7 and that it increases to 55%–65% if there is comorbidity and/or moderate and/or severe interference.2–4
Motivational variables play a fundamentally relevant role in the process of help-seeking. The specialist literature has particularly focussed on analysing the motivators for professional help-seeking. From this perspective, very diverse motivators have been demonstrated, from those that are specifically disorder-related, to the distress felt in appraising the disorder, concern about stigma, fear of the opinion of third parties, fear that the symptoms will worsen and even a determination to self-manage the problem. Another group of motivators are belief-related: from those that question the utility and/or efficacy of treatment, to beliefs that the symptoms will pass without treatment, or will be resolved with the support of family and friends, or that the disorder is not serious enough to warrant specialist treatment. The third group of motivators includes very diverse variables, generally associated with factors that are outside the problem itself: lack of time, financial difficulties, accessibility of appropriate therapists and/or centres, waiting lists and even a lack of knowledge about the healthcare resources.8–12
From the opposite perspective, i.e., from an analysis of the motivators that encourage help-seeking, there are fewer published studies. Noteworthy among the motivators suggested is the interference caused by mental illness, the sensation (real or otherwise) that symptoms are out of control, the persistence of symptoms despite efforts to manage them, deteriorating or worsening13–15 symptoms and the influence of the social and family environment.15–18
Bearing in mind the importance of both time and motivational factors in the analysis and understanding of the process by which a person with a mental disorder decides to seek the help of a mental health professional, the scarcity of studies in our context on these aspects, and the few standardised assessment tools on help-seeking,19 we decided to undertake a study with the following objectives: first, to obtain information about the time that patients with various mental disorders take to (a) recognise that they have a problem (disorder awareness), (b) disclose the problem and/or the difficulties in managing the problem to a third party and (c) seek specialist professional help. We then decided to analyse the motivators underlying each of the time periods mentioned, those that encouraged or helped towards appraisal of the problem, those that contributed to the delay in help-seeking and those that prompted actively seeking treatment.
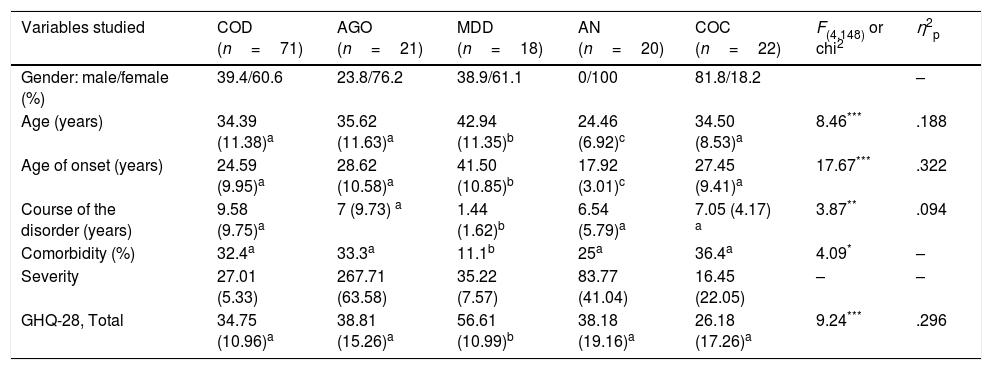
Material and methodsParticipantsOne hundred and fifty-two adult ambulant patients with the following main diagnoses participated (axis 1, DSM-IV-TR20): compulsive obsessive disorder (COD, 71 patients), agoraphobia (AGO, 21 patients), major depressive disorder (MDD, 18 patients), anorexia nervosa (AN, 20 patients) and cocaine dependence (COC, 22 patients). Table 1 shows the sociodemographic and clinical features of each group. As can be observed, the 5 groups differed in all the sociodemographic variables, with effect sizes between medium and large. The post hoc analyses (Bonferroni) showed that while there were only women in the AN group, men predominated in the COC group. The patients with MDD were older than those in the other 4 groups, both at the time of the study and at onset of the first symptoms. In contrast, the patients with AN were younger than the other clinical groups and therefore, also developed the disorder at an earlier age. With regard to the clinical variables, the patients with MDD had had the disorder for less time and had fewer comorbidities than the other clinical groups. All the groups scored highly in the severity measurements, because these were different for each disorder they were not compared (the various tools are described below). The patients with MDD (Goldberg General Health Questionnaire-28 [GGHQ-28]21) had the poorest quality of life, with a large effect size. There were no differences between the rest of the clinical groups in this variable.
Sociodemographic and clinical features of the sample and differences between the 5 groups of patients (ANOVA).
| Variables studied | COD (n=71) | AGO (n=21) | MDD (n=18) | AN (n=20) | COC (n=22) | F(4,148) or chi2 | η2p |
|---|---|---|---|---|---|---|---|
| Gender: male/female (%) | 39.4/60.6 | 23.8/76.2 | 38.9/61.1 | 0/100 | 81.8/18.2 | – | |
| Age (years) | 34.39 (11.38)a | 35.62 (11.63)a | 42.94 (11.35)b | 24.46 (6.92)c | 34.50 (8.53)a | 8.46*** | .188 |
| Age of onset (years) | 24.59 (9.95)a | 28.62 (10.58)a | 41.50 (10.85)b | 17.92 (3.01)c | 27.45 (9.41)a | 17.67*** | .322 |
| Course of the disorder (years) | 9.58 (9.75)a | 7 (9.73) a | 1.44 (1.62)b | 6.54 (5.79)a | 7.05 (4.17) a | 3.87** | .094 |
| Comorbidity (%) | 32.4a | 33.3a | 11.1b | 25a | 36.4a | 4.09* | – |
| Severity | 27.01 (5.33) | 267.71 (63.58) | 35.22 (7.57) | 83.77 (41.04) | 16.45 (22.05) | – | – |
| GHQ-28, Total | 34.75 (10.96)a | 38.81 (15.26)a | 56.61 (10.99)b | 38.18 (19.16)a | 26.18 (17.26)a | 9.24*** | .296 |
AGO: agoraphobia; AN: anorexia nervosa; COC: cocaine dependence; GHQ-28: Goldberg General Health Questionnaire-28; MDD: major depressive disorder; COD: compulsive obsessive disorder.
The data are expressed in means (SD).
The superscripts a, b, c indicate the intergroup differences (same superscript, no differences; Bonferroni).
Severity was assessed using a specific tool for each disorder. Severity of COD was measured using the structured interview of the Yale-Brown Obsessive-Compulsive Scale (YBOCS).22,23 Severity of AGO was assessed using the Agoraphobia Inventory,24 a self-report scale with 69 items (response scale from 0 to 5), grouped into 3 subscales: avoidance behaviours, physical symptoms and cognitive symptoms. The clinical cut-off point was at 176. Internal consistency in this study was α=.747. The severity of MDD was assessed using the Spanish version of the Beck Depression Inventory.25 AN was evaluated using the Spanish version of the Eating Disorder Inventory-II.26 Internal consistency in this study varied between α=.695 and α=.944 for the 11 subscales. The severity of COC was assessed using the semi-structured Cocaine Selective Severity Assessment,27 which evaluates the presence and intensity of cocaine abstinence symptoms over the last 24h (internal consistency: α=.913).
Quality of life was evaluated with the Spanish version of the GGHQ-28,21 a self-report scale comprising 4 subscales. The internal consistency of the tool's total score in the clinical groups ranged between α=.855 (COD) and α=.956 (AN group).
The Interview on Motivators for Help-seeking (EMBA) was developed by the authors based on the interview about the delay in seeking professional help for COD.13 This is a structured interview given by the clinician in the normal diagnostic assessment process. The interview was designed to assess seeking professional help as a process of 3 stages: appraisal of the problem, disclosure of the problem, and formal request for treatment. Help-seeking was defined as the first voluntary contact with a healthcare or social health professional (doctor of any speciality, psychiatrist, clinical psychologist or social worker). The first 4 questions refer to time determinations: when the problem for which professional help was sought started, first appraisal of their problem, when they talked to somebody about their problem for the first time, when they first requested the help of a health professional. After these initial questions, the patient was asked to answer 3 blocks of questions: (a) motivators for appraisal of the problem, (b) motivators for delaying requesting treatment (i.e., barriers to help-seeking) and (c) motivators for requesting professional help (i.e., help-seeking facilitators). Each of the 3 blocks was presented with an open question “How did you come to realise that what was happening to you was not normal?”, “Why did you delay seeking professional help?” and “Why did you seek professional help?”. After each question the patient was shown a list of possible responses and was asked to indicate all the responses that could apply to them. The first question was followed by 7 possible responses, the second by 18 and the third by 15 possible responses. In addition, at the end of each block, they were offered the option of adding other reasons not covered on the list. Reasons for delay that were beyond the patient's control were excluded from the analysis of the study results (e.g., waiting lists, difficulties at work, difficulty in accessing the health centre, personal commitments, etc.). The interview took approximately 15min. Attached as complementary material.
ProcedureThe sample was gathered consecutively over a period of one year in 3 mental health units of the public health network and the university. The patients were referred to the authors in the mental health unit following each unit's usual procedure. In the case of the university department, the majority of the patients were referred by other professionals (psychiatrists or clinical psychologists) from the mental health network, and a smaller proportion self-referred. The inclusion criteria were: main diagnosis of COD, AGO, MDD, AN and COC; aged between 18 and 65 years; absence of organic mental disorder or intellectual disability; and not having started psychological treatment in order to avoid biasing the assessment of clinical severity at the time of the study. In addition, the patients under psychopharmacological treatment had to have been stable for at least 3 weeks before starting the assessment protocol. The severity of the disorder, time of onset, comorbidity with other mental disorders, or concurrent psychopharmacological treatment were not considered exclusion criteria.
All the patients who met the criteria for participating in the study were assessed by one of the study authors, all of whom are clinical psychology specialist practitioners at doctorate level. The patients were informed beforehand of the assessment reasons and procedure and, if they agreed to take part, signed their informed consent. The initial assessment consisted of a diagnostic interview using the Anxiety Disorders Interview Schedule of the DSM-IV (ADIS-IV-L).28 Information was also gathered on sociodemographic data, whether they had any medical diseases and whether they had received or were receiving psychological and/or pharmacological treatment at the time of the study. They then answered the EMBA. After this assessment session, each patient was given a booklet with the abovementioned self-report questionnaires. For the COD patients, the assessor also completed the YBOCS to assess severity. The study was approved by the ethical committees of the university and the hospitals with mental health resources.
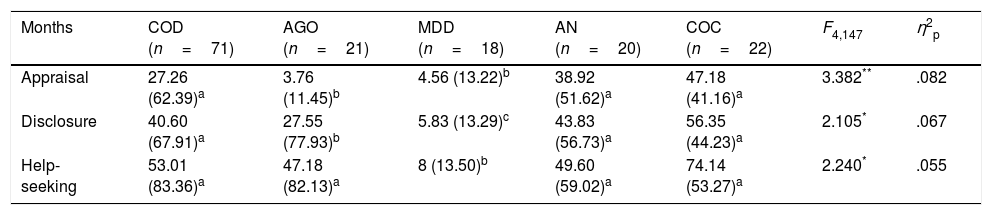
ResultsThe time taken by patients to appraise, disclose and seek help for their symptomsThe 5 groups showed differences in the 3 time periods assessed, with medium effect sizes (see Table 2). The mean time that the patient took to appraise their problem varied between a little more than 3 months in the AGO group and nearly 4 years in the COC group. The post hoc comparisons (Bonferroni) showed that the patients with AGO and MDD took significantly less time to recognise their symptoms than the other groups, which did not differ from each other. Similar results were obtained with regard to the time that the patients took to talk about their problem for the first time (disclosure), although in this case the patients with MDD took less than the AGO group. By contrast, the COD, AN and COC patients took longer to disclose their problem with no significant differences between them. Finally, the MDD patients also took less time to seek professional help, whereas there were no differences between the rest of the clinical groups. However, the wide variability in the 3 time periods is worth noting, which indicated differences between the patients in all the clinical groups due to the influence of the different variables in the help-seeking process.
Intergroup differences in time of appraisal, disclosure and help-seeking about symptoms.
| Months | COD (n=71) | AGO (n=21) | MDD (n=18) | AN (n=20) | COC (n=22) | F4,147 | η2p |
|---|---|---|---|---|---|---|---|
| Appraisal | 27.26 (62.39)a | 3.76 (11.45)b | 4.56 (13.22)b | 38.92 (51.62)a | 47.18 (41.16)a | 3.382** | .082 |
| Disclosure | 40.60 (67.91)a | 27.55 (77.93)b | 5.83 (13.29)c | 43.83 (56.73)a | 56.35 (44.23)a | 2.105* | .067 |
| Help-seeking | 53.01 (83.36)a | 47.18 (82.13)a | 8 (13.50)b | 49.60 (59.02)a | 74.14 (53.27)a | 2.240* | .055 |
AGO: agoraphobia; AN: anorexia nervosa; COC: cocaine dependence; MDD: major depressive disorder; COD: compulsive obsessive disorder.
The data are expressed in means (SD).
The superscripts a, b, c indicate the intergroup differences (same superscript, no differences; Bonferroni).
In order to examine whether the structure of the interview corresponded with the initial theoretical design of 3 sets of motivators (those that encourage appraisal, those that contribute towards delay and those that encourage help-seeking), we performed an exploratory factor analysis (principal components) with the 40 items. KMO analysis gave a value of .553 and the Bartlett's sphericity test result was significant (χ2(780)=1342.145; p=.0001), which indicates appropriate data distribution for the tests. Firstly, Oblimin rotation was applied which showed Independence between the factors, and therefore a second Varimax rotation was performed. In both cases, the Scree test was applied to extract the optimal number of factors. The 3-factor structure was the most satisfactory, at 29.06% total variance. The content of the 3 factors did not fit the 3 theoretical blocks of motivators for help-seeking that were initially designed, since the items of each block were distributed into each of the 3 factors obtained. The first factor (13.91% of explained variance, EV; 17 items) fundamentally comprised motivators that led the patient to seek help for their problem, and therefore, adjusted well to the initial theoretical block of reasons for seeking help. These reasons basically included those related to a feeling of loss of control, in addition to items associated with the patient's own appraisal of the problem. The second factor (EV=7.61%; 10 items) included positive evaluations on the disorder and a lack of perception of its negative impact, which indicates minimisation of the problem and delay in help-seeking. The third factor (EV=7.54%; 9 items) included items about stigma and its influence on delay.
It is worth highlighting that 4 items (delay due to mistrust of professional help, delay because the problem had occurred seldom, seeking help on the recommendation of another person and delay due to fear of the treatment) did not saturate in any specific factor because their saturation was <.30 and distributed between the 3 factors.
In sum, the analysis revealed 3 well-differentiated sets of factors, which in turn reflect the motivators that encourage patients to seek help or otherwise: firstly (factor 1), there are the “personal” motivators to consult a professional for a mental health problem, experiencing emotional symptoms (anxiety, sadness, etc.) and loss of control over the problem. Secondly (factor 2), there are the reasons that impede appraisal of the problem and therefore, result in delayed help-seeking. These reasons include positive sensations, minimising symptoms and/or their consequences, etc. And in third place (factor 3), there is a group of reasons other than the previous reasons that also result in delayed help-seeking, since they are linked to fear of social rejection and therefore refer to the stigma associated with mental illness.
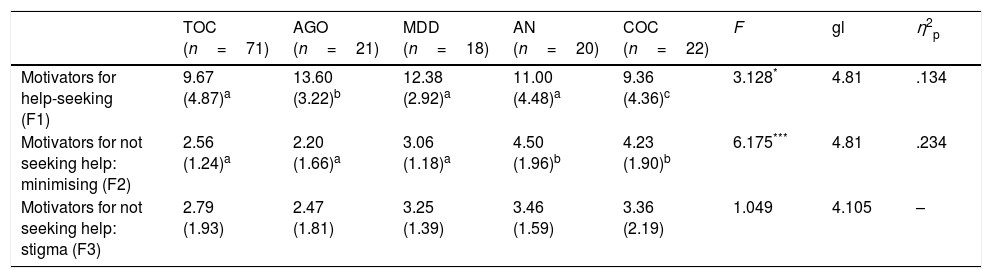
Differences between groups of patients in the factors–subscales of the Interview on Motivators for Help-seekingThe differences were studied between the groups (ANOVA, with post hoc Bonferroni tests) in the 3 factors or subscales of the interview (Table 3). The results showed significant differences in the 2 first factors, with large effect sizes. The post hoc tests showed that the patients in the COC group stated that they had fewer motivators to consult than the AGO patients, while the other 3 groups were placed in an intermediate point between the 2 groups mentioned. With regard to the differences in factor 2, the patients of the AN and COC groups had lower scores, i.e., they identified more motivators for not seeking help and, therefore, tended to minimise the problem more than the other groups. Finally, none of the groups differed in factor 3 (i.e. motivators for not seeking help: fear and stigma), which indicates that there is a similar level of personal stigma and fear of social rejection, irrespective of the disease suffered.
Differences between the 5 groups of patients in ANOVA in the factors of the Interview on Motivators for Help-seeking.
| TOC (n=71) | AGO (n=21) | MDD (n=18) | AN (n=20) | COC (n=22) | F | gl | η2p | |
|---|---|---|---|---|---|---|---|---|
| Motivators for help-seeking (F1) | 9.67 (4.87)a | 13.60 (3.22)b | 12.38 (2.92)a | 11.00 (4.48)a | 9.36 (4.36)c | 3.128* | 4.81 | .134 |
| Motivators for not seeking help: minimising (F2) | 2.56 (1.24)a | 2.20 (1.66)a | 3.06 (1.18)a | 4.50 (1.96)b | 4.23 (1.90)b | 6.175*** | 4.81 | .234 |
| Motivators for not seeking help: stigma (F3) | 2.79 (1.93) | 2.47 (1.81) | 3.25 (1.39) | 3.46 (1.59) | 3.36 (2.19) | 1.049 | 4.105 | – |
AGO: agoraphobia; AN: anorexia nervosa; COC: cocaine dependence; MDD: major depressive disorder; COD: compulsive obsessive disorder.
The data are expressed in means (SD).
The superscripts a, b, c indicate the intergroup differences (same superscript, no differences; Bonferroni).
There are different stages in the process of seeking help for mental diseases, in which time and motivational aspects are intertwined, and in which the patient and their environment participate. Therefore a reliable assessment tool is needed to capture the set of variables that form this process. The EMBA was constructed for this purpose. The fact that it was designed as an interview enables detailed information to be gathered that combine quantitative and qualitative information. Furthermore, the structure that shapes the interview gathers what is essential from the process. Compared to more specific tools that focus on a stage of the process, such as appraisal of the problem,29 motivators for delaying helpseeking,8,30–32 or the resources of those receiving help,4,33–36 the interview developed for this study attempts to combine the maximum information in a single tool, and to that end marks appraisal, disclosure of the problem and professional care-seeking in stages of time, capturing the motivators that encourage appraisal of the disorder, those that hinder the search for professional help, and the reasons for requesting treatment.
With regard to the time aspects of the process, the results of this study reflect the high delay in the different stages of help-seeking, which varies between 3.76 and 47.18 months in the appraisal stage, between 5.83 and 56.35 months in the disclosure stage, and between 8 and 74.14 months in the requesting treatment stage.
The interview groups the motivational aspects into 3 blocks that reflect the influence of emotional symptoms and the experience of loss of control over requesting professional help, the influence of positive feelings and the consequent minimisation of symptoms and/or their consequences on the delay in recognising the problem and in seeking professional help, and the negative impact of stigma on the decision to seek treatment. These results correspond with those of other studies, that indicate that the people most likely to seek help are those who recognise greater interference by the symptoms in their daily lives.2 Increased awareness of the disease is without doubt one of the most important variables that motivate patients to seek help. In this study, this was particularly significant in the group of AGO patients. At the polar opposite is the negative influence of minimising symptoms on appraisal of the problem, in other words, on awareness of disease, which is in line with Saunders’ approach37 indicating that recognising that one has a problem that is beyond one's own capacities to control is one of the most difficult stages in the help-seeking process. This is clearly seen in the COC patients and the AN patients, who overestimate the “benefits” of their symptoms from consumption in the COC group and associated with restricting food intake in the AN group, while they underestimate the disadvantages, which results in delayed appraisal of the problem and also in seeking treatment. Minimising the problem, which occurred in all the clinical groups of the study, might reflect the influence of the lack of education on mental health in our environment and the consequent negative effect that the stigma associated with mental illness continues to bear. The negative influence of stigma coincides with other studies as a major constraint to seeking professional help.9,10,15,38–40
Of the 3 factors that shape the interview structure, the most emphasis was placed on the factor relating to the motivators for help-seeking, in turn related to increased, or established, awareness of illness. This indicates that this set of variables is the most important in determining when a person will seek professional help, irrespective of their disorder, as has been confirmed in other studies.10,15
This study has some limitations. On the one hand, its retrospective and cross-sectional design means that it might be subject to some memory bias in the patients’ assessment. And on the other hand, the limited size of the AGO, MDD, AN and COC groups makes it difficult to generalise the results. Despite these limitations, we believe that the data enable a better understanding of the help-seeking process for people with a mental disorder and of the role of the motivating variables in shortening or lengthening the time they take to appraise their problem, discuss it and seek treatment. The availability of this type of information could contribute to improving the dissemination of appropriate information about mental illness and access to effective treatments in our environment. This is essential in improving the quality of life of these patients and reducing the personal and social cost associated with mental illness.41
Conflict of interestThe authors have no conflict of interest to declare.
This study was carried out with the help of MINECO (PSI2013-44733-R) and the Conselleria d’Educació, Cultura i Esport (Department of Education, Culture and Sport) of the region of Valencia (PROMETEO/2013/066).
Please cite this article as: del Valle del Valle G, Carrió C, Belloch A. Fases temporales y variables motivacionales: dos perspectivas complementarias en el proceso de búsqueda de ayuda por enfermedad mental. Rev Psiquiatr Salud Ment (Barc.). 2018;11:176–183.