Functional deficits are commonly observed in bipolar disorder after symptomatic remission. Social cognition deficits have also been reported, which could contribute to dysfunction in patients with bipolar disorder in remission.
Materials and methodsTwelve bipolar disorder patients in symptomatic remission (7 patients with bipolar disorder type I and 5 with bipolar disorder type II) and 12 healthy controls completed the Reading the Mind in the Eyes Test and the Faux Pas Test to evaluate theory of mind (ToM). Both groups also completed the Functional Assessment Short Test (FAST).
ResultsThe performance of the bipolar patients in the cognitive component of ToM was below normal, although the difference between the control group was not statistically significant (P=.078), with a trend to a worse performance associated with a higher number of depressive episodes (P=.082). There were no statistically significant differences between groups for the emotional component of ToM. Global functionality was significantly lower in bipolar patients compared to the control group (P=.001). Significant differences were also observed between both groups in five of the six dimensions of functionality assessed. No significant correlation was found between functionality and theory of mind.
ConclusionsBipolar patients in symptomatic remission exhibit impairments in several areas of functioning. Cognitive ToM appears more affected than emotional ToM. Deficits in ToM were not related to functional impairment.
Los déficits en la funcionalidad son comunes durante la remisión en el trastorno bipolar (TB). Adicionalmente, existe evidencia de alteraciones en la cognición social en remisión clínica. Estos déficits podrían contribuir a la disfunción observada en estos pacientes.
Material y métodosDoce pacientes bipolares en remisión sintomática (7 bipolares tipo i y 5 de tipo ii) y 12 individuos controles sin patología psiquiátrica completaron el Test de las Miradas y el Test de Faux Pas para evaluar teoría de la mente (ToM), y el Test Breve para la Evaluación de la Funcionalidad (FAST).
ResultadosEl desempeño de los pacientes bipolares en el aspecto cognitivo de la ToM se ubicó por debajo de la línea de corte, sin llegar a presentar diferencias significativas en comparación con el grupo control (p=0,078) y con tendencia a un peor desempeño a mayor número de episodios depresivos (p=0,082). Las puntuaciones medias para el componente emocional de la ToM se encontraron por encima de la puntuación de corte en ambos grupos. La funcionalidad global resultó significativamente inferior en los pacientes bipolares en comparación con la muestra control (p=0,001). A la vez, se observaron diferencias significativas entre ambos grupos en 5 de las 6 dimensiones del funcionamiento evaluadas. No se hallaron correlaciones significativas entre la ToM y la funcionalidad.
ConclusionesLos pacientes con TB presentan, aun en remisión sintomática, disfuncionalidad en un amplio espectro de ámbitos vitales. El aspecto cognitivo de la ToM se encontraría más afectado que la ToM emocional. No se observó una correlación significativa entre alteraciones en la funcionalidad y déficits en ToM.
Bipolar disorder (BP) is a chronic psychiatric disease, characterised by noticeable mood instability with periods of expansive mood that alternate with periods of depressive mood. In addition, neuropsychological deficits and disturbances in functioning have been observed to persist during remission of the clinical symptoms,1,2 and they may continue to aggravate as the disorder continues.3 There is evidence that these disturbances constitute an important obstacle for the social reintegration and rehabilitation of bipolar patients in remission. Therefore, they are receiving increasingly more attention as an object of study.4 There is also interest in investigating the existence of deficits in social cognition and its possible impact on functionality.5
In this context, functionality refers to the capacity to efficiently carry out tasks and activities associated with different life domains. It is a broad concept that includes various skills, including the ability to relate to others socially and romantically, to be autonomous, to work, study and participate in recreational activities.6
There is evidence that the functionality of individuals with BP changes during the remission of clinical symptoms. Tohen et al.7 showed that 97.5% of bipolar patients presented remission of acute clinical symptoms in the 24 months following the start of treatment, but only 37.6% recovered functionality. In addition, Strakowski et al.,8 based on an 8-month follow-up study, reported that at least 1 area of function showed a deficit in the majority of patients during clinical remission. Furthermore, just less than half of the bipolar patients in the sample demonstrated optimal performance in at least 3 of the 4 areas of function evaluated by Strakowsky et al.8
In agreement with these results, Goswami et al.9 reported that 54% of patients in remission showed mild to moderate deficits, 8% a pronounced deficit and 11% a severe functional deficit. In similar studies,6 even higher percentages of severe dysfunction were described among euthymic bipolar patients, ranging from 20% to 30% of the evaluated subjects.
Regarding the areas of functioning affected, Rosa et al.6,10 reported that the functional deficits observed most frequently in BP were disturbances in cognitive, interpersonal and sexual functioning, as well as in use of free time. Dickerson et al.11 reported deficits in proportions similar to the Tsuang et al.12 study, specifically in the areas of social and cognitive functioning. Furthermore, in agreement with Blairy et al.,13 bipolar patients in remission showed adjustment deficits regarding family relationships, marriage, leisure activities and work activity. Coryell et al.14 also described deficits in interpersonal functionality and leisure.
Recently, researchers have begun to study the existence of social cognition deficits in BP during euthymia, as well as the possible relationship between these deficits and patients’ clinical characteristics and functional deficits.5,15 Social cognition includes the neuropsychological processes involved in social interaction between members of the same species. These processes include theory of mind (ToM), which is defined as the ability to attribute third party emotional, epistemic, intentional and motivational states.16 The term ToM was introduced by Premack and Woodruff17 in a publication titled, “Does the chimpanzee possess theory of mind?”, in which the authors examined the possibility of the chimpanzee having the capacity to attribute mental states to other members of its species.16 As for the different aspects of this capability, cognitive ToM refers to the ability to make inferences about other people's beliefs, whereas affective ToM refers to the ability to make inferences with respect to others’ feelings.
There is evidence of ToM deficits in psychiatric disorders such as autism and schizophrenia.18,19 In addition, ToM disturbances have been studied in unipolar depression,20 personality disorders21,22 and in attention deficit disorder,23,24 among other pathologies. With respect to ToM deficits in bipolar disorder, Bora et al.25 reported that disturbances were observed during the affective phases, although the evidence was less conclusive with respect to ToM during remission.
Kerr et al.26 reported alterations in depressive and manic bipolar patients, although these were not observed in patients in remission. Similarly, Ioannidi et al.27 described that the ToM disturbances observed in bipolar patients during affective episodes did not persist after the remission of clinical symptoms, except in the case of cognitive ToM measured by the Faux Pas Recognition Test. Furthermore, in agreement with Martino et al.,28 deficits in ToM abilities did not distinguish patients with BP from controls, once the effects of exposure to medication and of general neuropsychological deficits were controlled.
However, other authors reported subtle deficits during euthymia, which could be observed in tasks that examined ToM at a level of greater complexity.25,29 In agreement with Bora et al.,29 Wolf et al.30 described performance deficits for all ToM measurements in depressive, manic and euthymic bipolar patients.
As for the different aspects of ToM, Shamay-Tsoory et al.31 reported general ToM deficits in euthymic bipolar patients, these deficits being more noticeable in cognitive ToM than in emotional. The authors explained these results by indicating, first, that the neuroanatomical basis (referring to limbic structures such as the amygdala) of affective ToM was largely unknown. These authors then explained that cognitive ToM depended on the functioning of the ventromedial prefrontal cortex, an area in which a function deficit was reported in patients with BP. Montag et al.32 also reported that pronounced cognitive, but not emotional, ToM changes had been found in BP. Olley et al.33 found that patients with BP performed more poorly in ToM tasks with more verbal components, while performance in nonverbal ToM tasks was similar to that of the controls.
There is evidence of a relationship between ToM and functionality in different psychiatric pathologies. ToM deficits are related to deficient social interaction34 and communication difficulties in autism.35,36 Bora et al.37 reported that, in patients with schizophrenia, there was a relationship between functioning and ToM, particularly with the ability to identify third-party emotional mental states, evaluated using the Reading the Mind in the Eyes test. In these patients, a relationship has been found between social exclusion and deficits in the ToM processes involving the ability to register the mental states of others and take them into consideration.38 A relationship has also been found between functioning and ToM in unipolar depression in remission.39
In addition, ToM deficits have been associated with social dysfunction in conduct disorders and borderline personality disorder, as well as disruptive and antisocial conduct.40 However, other cognitive factors influence this relationship.36,41,42
There is little information regarding the relationship between ToM deficits and functionality during euthymia in BP. Olley et al.33 reported that there was no significant relationship between ToM and social and occupational functioning in euthymic bipolar patients. However, research on the relationship between functionality and ToM in BP is still scarce, but there is evidence of a relationship between these variables in other disorders.35–39 For these reasons, in the case of BP, ToM could be relevant for functionality as well.
The main objective of this study was to examine the possible deficits in cognitive and emotional ToM in patients with BP in symptomatic remission. As a secondary objective, the potential relationship between ToM and functionality was also explored in the same group of patients with BP.
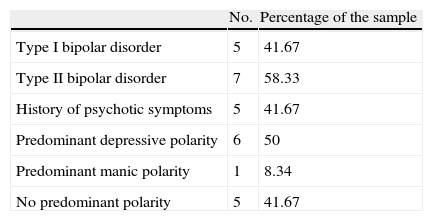
Methods and materialsThe sample consisted of 12 patients diagnosed with bipolar disorder who received treatment in the outpatient department at the Dr. José Tiburcio Borda public psychiatric hospital for men in Buenos Aires, Argentina. Consecutive patients who complied with the predetermined inclusion criteria were recruited. Among the patients evaluated, 7 had a type II BP diagnosis and the other 5, a type IBP diagnosis. All the patients with BP who participated were in symptomatic remission, based on the accepted criteria for remission, defined according to the nomenclature recommended by the International Society for Bipolar Disorders (ISBD).43 None of the patients presented significant medical diseases, neurological disorders, mental deficiency or drug abuse. Furthermore, they were under pharmacological and psychotherapeutic treatment when they were being evaluated. Out of the entire sample, 83.3% received mood stabilisers (lithium carbonate, valproate, lamotrigine and carbamazepine), 50% antipsychotics (aripiprazole, quetiapine, risperidone) and 30% received anxiolytics (clonazepam, diazepam). Table 1 contains the clinical characteristics of the sample of euthymic bipolar patients.
Clinical characteristics of bipolar patients.
| No. | Percentage of the sample | |
| Type I bipolar disorder | 5 | 41.67 |
| Type II bipolar disorder | 7 | 58.33 |
| History of psychotic symptoms | 5 | 41.67 |
| Predominant depressive polarity | 6 | 50 |
| Predominant manic polarity | 1 | 8.34 |
| No predominant polarity | 5 | 41.67 |
| Mean | SD | |
| YMRS score | 2.25 | 2.73 |
| HAMD-17 score | 3.80 | 2.47 |
| No. of manic episodes | 5 | 3.80 |
| No. of depressive episodes | 10.63 | 13.50 |
| Period in remission (months) | 9 | 8.80 |
| Treatment period (months) | 38 | 48.04 |
| No. of hospitalisations | 0.66 | 1.49 |
| Age at onset | 25 | 7.93 |
Regarding demographic variables, the 12 euthymic bipolar patients were male, with a mean age of 48.2 years (SD 11.2). Of the sample, 62% had completed the secondary level of education, 23% the tertiary level and 15% the primary level. The control subjects were 12 male volunteers without present or past psychiatric pathology, evaluated using the MINI Plus interview, which measured the presence of psychiatric symptoms according to DSM-IV and ICD-10 criteria. The mean age of the controls was 46.04 years (SD 12.3). With respect to their educational level, 60% had completed the secondary level (12 years of education), 25% the tertiary level (16 years of education) and 15% the primary level (8 years of education). Statistically significant differences between the sample of bipolar subjects and the control sample were not detected in the age variable (U=53.50, Z=−1.07, P=.29) or the education variable (U=77.00, Z=0.320, P=.80). Both groups were evaluated in sessions of approximately 1h.
All participating patients with BP were in remission, defined by a score lower than the cut-off on both the Young Mania Rating Scale (YMRS)44 and the Hamilton Rating Scale for Depression (HAMD-17).45 The cut-off score was 8 points for the YMRS and 7 points for the HAMD-17. The Reading the Mind in the Eyes test46 and the Faux Pas Recognition Test47 were applied to evaluate ToM, while the Functional Assessment Short Test (FAST)6 was used to evaluate functionality.
The FAST scale measures 6 functional domains: financial, interpersonal, leisure, autonomy, occupational and cognitive functioning. It also evaluates overall functionality, which consists of the sum of the scores obtained for the 6 dimensions.
The Reading the Mind in the Eyes test is made up of 36 photographs of the eye area of different subjects, half of them female and half male. Each of these photographs expresses a certain emotion. The images appear with 4 response options from which the patient can choose the emotion expressed in the photograph. As a control task, the sex of the subject photographed should also be identified to rule out disturbances in facial perception. The cut-off score for this evaluation is 31 out of 36 for the sex identification component. If the score is lower than the sex identification cut-off, the evaluation becomes invalid. The cut-off score is 21 out of 36 for the emotion identification component. Scores lower than the emotion identification cut-off indicate a deficit in the ability to infer emotional states by looking at someone's eyes. This test was developed based on the concept that subjects are able to extract information on emotional mental states from others’ eyes, and this information can consequently be used to evaluate emotional components of ToM.
The Faux Pas Recognition Test is made up of 20 brief stories in which characters interact. In 10 of the stories, a social error is committed, while the other 10 stories are presented as controls. After presenting each story, questions designed to evaluate ToM are asked, along with a control question assessing understanding and capacity to remember the story (with there being a version adapted to Spanish).48 This test can be used to assess both cognitive and emotional components of ToM, although only the questions assessing cognitive ToM were used in the present study. To evaluate performance in this ToM measurement, 1 point was added for every correct answer to the ToM-assessing questions in the stories with social errors, plus 1 point for each correct answer to the control question in the stories without social errors. The gross score obtained by the subject being assessed was then divided by the total possible score, giving the performance measurement. A cut-off score of 0.75 was established for this test. Scores lower than 0.75 indicated a performance deficit.49,50
The data were analysed using the statistical package SPSS, version 20, Spanish language.
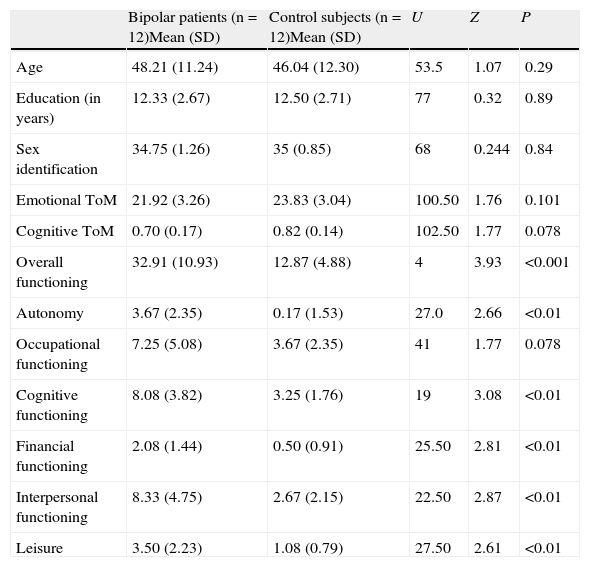
ResultsNo significant differences were found between patients with bipolar disorder in symptomatic remission and healthy control subjects regarding the sex recognition component on the Reading the Mind in the Eyes test (U=68, Z=−0.22, P=.84), as can be observed in Table 2. As for the emotion recognition component, the score obtained by both groups was higher than the cut-off, which indicated normal performance in both control subjects and patients with BP. The difference between the performance of the control subjects and study group patients was not significant in this measurement of emotional ToM (P=.10).
Mann–Whitney U test for cognitive ToM, emotional ToM and functionality.
| Bipolar patients (n=12)Mean (SD) | Control subjects (n=12)Mean (SD) | U | Z | P | |
| Age | 48.21 (11.24) | 46.04 (12.30) | 53.5 | 1.07 | 0.29 |
| Education (in years) | 12.33 (2.67) | 12.50 (2.71) | 77 | 0.32 | 0.89 |
| Sex identification | 34.75 (1.26) | 35 (0.85) | 68 | 0.244 | 0.84 |
| Emotional ToM | 21.92 (3.26) | 23.83 (3.04) | 100.50 | 1.76 | 0.101 |
| Cognitive ToM | 0.70 (0.17) | 0.82 (0.14) | 102.50 | 1.77 | 0.078 |
| Overall functioning | 32.91 (10.93) | 12.87 (4.88) | 4 | 3.93 | <0.001 |
| Autonomy | 3.67 (2.35) | 0.17 (1.53) | 27.0 | 2.66 | <0.01 |
| Occupational functioning | 7.25 (5.08) | 3.67 (2.35) | 41 | 1.77 | 0.078 |
| Cognitive functioning | 8.08 (3.82) | 3.25 (1.76) | 19 | 3.08 | <0.01 |
| Financial functioning | 2.08 (1.44) | 0.50 (0.91) | 25.50 | 2.81 | <0.01 |
| Interpersonal functioning | 8.33 (4.75) | 2.67 (2.15) | 22.50 | 2.87 | <0.01 |
| Leisure | 3.50 (2.23) | 1.08 (0.79) | 27.50 | 2.61 | <0.01 |
The score obtained by the patients with BP was lower than the cut-off on the Faux Pas Recognition Test, indicating a reduction in their functioning. The control subjects’ score fell within normal performance. The difference in performance in this measurement of cognitive ToM between the patients with BP in symptomatic remission and the control subjects was not significant at the level P=.05. However, there was a statistical tendency towards a significant difference (P=.078).
As illustrated in Table 2, overall functionality was significantly lower for patients with BP in comparison to that shown for the control sample (P=.001). There were also significant differences between both groups in 5 out of the 6 functional dimensions that were assessed: autonomy, leisure and cognitive, financial and interpersonal functioning. In the case of occupational functionality, a statistical tendency towards a significant difference was observed (P=.078), although the difference was not significant at the level of P=.05.
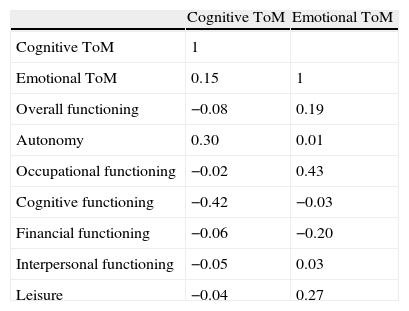
Regarding the correlation between cognitive ToM and functionality, and between emotional ToM and functionality, the results for the group of patients with BP are shown in Table 3. No significant correlations were found between cognitive ToM and the 6 functionality dimensions, or with overall functionality. The results were similar in the case of emotional ToM, as there were no significant correlations found between this variable and overall functionality or the 6 functionality dimensions assessed.
Non-significant Spearman correlation coefficients (ρ) between ToM and functionality.
| Cognitive ToM | Emotional ToM | |
| Cognitive ToM | 1 | |
| Emotional ToM | 0.15 | 1 |
| Overall functioning | −0.08 | 0.19 |
| Autonomy | 0.30 | 0.01 |
| Occupational functioning | −0.02 | 0.43 |
| Cognitive functioning | −0.42 | −0.03 |
| Financial functioning | −0.06 | −0.20 |
| Interpersonal functioning | −0.05 | 0.03 |
| Leisure | −0.04 | 0.27 |
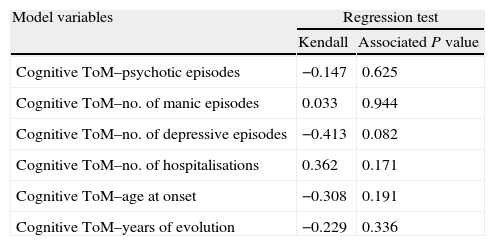
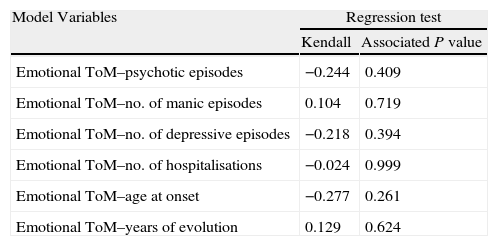
To assess the possible correlation between ToM functioning and each of the different clinical variables of the patients with BP, a multivariate statistical analysis was performed. These variables were not found to influence or to be related to cognitive or emotional ToM (Tables 4 and 5). However, the number of depressive episodes had a statistical tendency (P=.082) to influence cognitive ToM, which should be confirmed or ruled out with a larger sample size in a future study.
Multivariate nonparametric regression analysis to explore cognitive ToM.
| Model variables | Regression test | |
| Kendall | Associated P value | |
| Cognitive ToM–psychotic episodes | −0.147 | 0.625 |
| Cognitive ToM–no. of manic episodes | 0.033 | 0.944 |
| Cognitive ToM–no. of depressive episodes | −0.413 | 0.082 |
| Cognitive ToM–no. of hospitalisations | 0.362 | 0.171 |
| Cognitive ToM–age at onset | −0.308 | 0.191 |
| Cognitive ToM–years of evolution | −0.229 | 0.336 |
Multivariate nonparametric regression model to explore emotional ToM.
| Model Variables | Regression test | |
| Kendall | Associated P value | |
| Emotional ToM–psychotic episodes | −0.244 | 0.409 |
| Emotional ToM–no. of manic episodes | 0.104 | 0.719 |
| Emotional ToM–no. of depressive episodes | −0.218 | 0.394 |
| Emotional ToM–no. of hospitalisations | −0.024 | 0.999 |
| Emotional ToM–age at onset | −0.277 | 0.261 |
| Emotional ToM–years of evolution | 0.129 | 0.624 |
A significant difference was observed between patients with bipolar disorder in symptomatic remission and healthy control subjects regarding overall functionality (P=.001), and in 5 out of the 6 functionality domains assessed by the FAST scale: autonomy, leisure, interpersonal functioning, finances and cognitive functioning.
There is evidence of alterations in different vital function domains in euthymic bipolar patients, as indicated by Rosa et al.6 Among other authors, Blairy et al.13 reported deficits in leisure, work and interpersonal relationships, Dickerson et al.12 described alterations in cognitive and social functionality and Coryel et al.14 deficits in interpersonal functionality and leisure. Likewise, Rosa et al.6 reported alterations in overall functionality, and in autonomy, leisure and interpersonal, cognitive, financial and occupational functionality. The data found regarding functionality in our sample of patients with BP in symptomatic remission were thus congruent with existing publications.
In the case of occupational functioning, the results indicated a statistical tendency towards a significant difference (P=.078). This difference between occupational functionality and the other dimensions might be due to the fact that some questions on the FAST scale used to assess work functionality may not have been appropriate for the cultural and socioeconomic context in which the present study was carried out. For example, some items investigated compensation according to the job, as well as possibilities of insertion in the chosen labour field.
The results obtained by the patients with BP in symptomatic remission fell below the cut-off line for the general population in the case of cognitive ToM, but not in the case of emotional ToM. The difference between scores obtained by our study subjects and the healthy controls was not significant for emotional ToM (P=.101), while there was a statistical tendency towards a significant difference in the case of cognitive ToM (P=.078). Furthermore, cognitive ToM functioning tended to worsen as the number of depressive episodes increased (P=.082). The results, therefore, could suggest the possibility of greater disturbance in cognitive ToM abilities, in comparison to emotional ToM, in patients with BP in symptomatic remission.
The results obtained in the present study consequently agreed with studies indicating that there would be more deficits in cognitive ToM than in emotional ToM in euthymic bipolar patients.29,30,32 Therefore, it could be thought that disturbances in emotional ToM processing would be characteristic of acute affective episodes51 and not of remission periods. However, and in relation to emotional ToM, the data found in this study were contrary to those from Wolf et al.,30 who found alterations in this domain in patients with BP in remission. From the finding of cognitive ToM disturbances in both the acute phase and when the patient's mood is stabilised, it could be suggested that this constitutes a phenotypic characteristic of BP and one that would then need to be studied in greater depth.
No significant correlations were found between any of the ToM and functionality measures (Table 3). These results were similar to those reported by Olley.33 However, a relationship between functionality and ToM has been reported in other mental disorders.35–39 Among the limitations of the study, we should mention the reduced sample size (n=12), which could have resulted in a type II error. The difference observed in cognitive ToM between patients with BP and control subjects might have been significant with a larger sample, given that a statistical tendency in that direction was observed (P=.078). Likewise, the correlations observed between ToM and functionality could possibly have been significant with a greater number of participants. In addition, carrying out this study in a psychiatric hospital of men made it impossible to explore the relationship between ToM and functionality in patients of both sexes. Consequently, comparisons between genders could not be made.
The present study found deficient results in functionality, concordant with the results described in scientific literature, but they were not ToM deficits. Likewise, no correlation was found between ToM deficits and functionality, a relationship found in other pathologies.
It is possible that some techniques used to assess ToM in this clinical population did not detect ToM deficits because the alterations were subtle. Most ToM assessment techniques were developed for clinical populations where the ToM deficit is more severe, such as autistic spectrum disorders or schizophrenia.12,18,23,29 The assessment techniques used in the present study were selected because they can detect deficits at a more subtle level. However, it may be necessary to develop assessments that are more appropriate and specific for this clinical population.
There are few studies on the possibility that ToM disturbances contribute to dysfunction during euthymia.34 Nevertheless, considering that a group of patients with BP in symptomatic remission showed broad functional disturbances compared to healthy controls, ascertaining the underlying factors that alter functionality would be important for designing more specific rehabilitation programmes.
Ethical disclosuresHuman and animal protectionThe authors declare that no experiments were performed with humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their work centre regarding the publication of patient data and that all patients included in the study have received sufficient information and have given their written informed consent to participate in this study.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Barrera Á, et al. Teoría de la mente y funcionalidad en pacientes bipolares en remisión sintomática. Rev Psiquiatr Salud Ment (Barc.). 2013;6:67–74.