There is a growing interest in mobile Health interventions (m-Health) in patients with psychosis. The aim of this study is to conduct a systematic review in order to analyse the current state of research in this area. The search of articles was carried out following the PRISMA criteria, focusing on those studies that used mobile technologies in patients with psychosis during the period from 1990 to 2016. A total of 20 articles were selected from the 431 studies found. Three types of studies are distinguished: (1) Analysis of quality and usability, (2) Improving treatment adherence and reducing hospital admissions, and (3) Analysis of patient symptoms. Conclusions: m-Health interventions are feasible, and are easy to use for patients with psychosis. They evaluate the evolution of psychotic symptoms more efficiently, and improve adherence to treatment, as well as symptoms and hospital admissions. However, a particular strategy does not stand out over the rest, because differences in methodology make them difficult to compare.
Hay un creciente interés en las intervenciones mobile Health (m-Health) en pacientes con psicosis. El objetivo de este estudio es realizar una revisión sistemática para analizar el estado actual de la investigación en este ámbito. La búsqueda de publicaciones se llevó a cabo siguiendo los criterios PRISMA, centrándose en aquellos estudios que utilizan tecnologías móviles en pacientes con psicosis durante el periodo de 1990 a 2016. Se seleccionó un total de 20 artículos de los 431 estudios que se encontraron. Se diferencian 3 tipos de intervenciones: 1) análisis de calidad y usabilidad; 2) mejora de la adherencia, síntomas y reducción de hospitalizaciones, y 3) análisis de la sintomatología del paciente. Conclusión: Las intervenciones m-Health son viables y resultan fáciles de utilizar para los pacientes con psicosis. Evalúan de forma más eficiente la evolución de los síntomas psicóticos y mejoran la adherencia al tratamiento, los síntomas y las hospitalizaciones. No se puede destacar una estrategia sobre las demás debido a que las diferencias en la metodología las hace difícilmente comparables.
In recent years information and communication technology (ICT) applied to health have evolved extremely quickly. This has led to a change in the patient-doctor relationship, as now the “empowered patient” has emerged. This refers to individuals who are knowledgeable and have information about their disease, who are involved in their treatment and able and interested in contributing and deciding about it (equipped, enabled, empowered and engaged).1
Electronic Health (e-Health) technologies combine the use of electronic communications and ICT have clinical, educational, ethical and administrative uses, with the aim of improving the healthcare system, promoting health and increasing the access of the whole population to healthcare. One of its components is mobile Health or m-Health, defined by the World Health Observatory as “the medical or public healthcare practice supported by mobile devices, patient monitoring devices, personal digital assistants (PDA) and other wireless devices”.2
These technologies have been used in the treatment of a wide range of physical and mental pathologies.3,4 Of these, psychosis is an interesting field due chiefly to the low level of adherence of these patients, as 70% will have abandoned their antipsychotic treatment 18 months after commencing it.5 The use of m-Health interventions which enables continuous, direct and personalised evaluation, gives the patient a greater role in his treatment and may improve this situation.
A growing number of studies have been undertaken during the past 20 years with the aim of increasing psychosis patient adherence through the use of mobile applications. However, it is hard to extract conclusions from these studies due to the differences between them in terms of sample selection, study procedure or the technique used.
The aim of this study is to carry out a systematic review of the literature to obtain an overview of the state of research into the use of mobile applications in patients with psychosis to improve adherence to treatment.
MethodologySome of the recommendation and criteria of the PRISMA6 declaration were followed in undertaking this review. Studies were selected that centre on the analysis of the acceptability, viability, use and possibilities of therapy using mobile devices in the treatment of psychotic patients. The following inclusion/exclusion criteria were applied:
- 1)
We considered mobile device (PDA, mobile telephone and/or smartphone) based interventions to be those which use SMS (short message service) and/or mobile applications (apps). This therefore exclude mobile interventions that only use services based on telephone calls.
- 2)
Studies were selected that covered patients diagnosed with psychotic disorder according to the definition and classification of the fourth and fifth editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV, DSM-IVR and DSM-5), including: schizophrenia, schizoaffective disorders, bipolar disorder and other psychoses. Studies were included with hospitalised patients as well as follow-ups in outpatient departments.
- 3)
Articles published in the English language from 1990 to 2016.
The data bases PsycINFO, PubMed, Scopus, Medline, ISI Web of Knowledge and the bibliographical data of the CSIC IME were used to search for publications. The following terms or key words were used: “Cell phone AND schizophrenia”, “Cell phone therapy AND mental health”, “Mobile assessment AND treatment schizophrenia”, “Mobile phone applications (apps) AND mental health”, “Smartphone AND schizophrenia adherence”, “The use of smartphones in antipsychotic adherence”, “The use of smartphones in psychosis”, “Cell phone AND psychosis” and “SMS AND psychosis”.
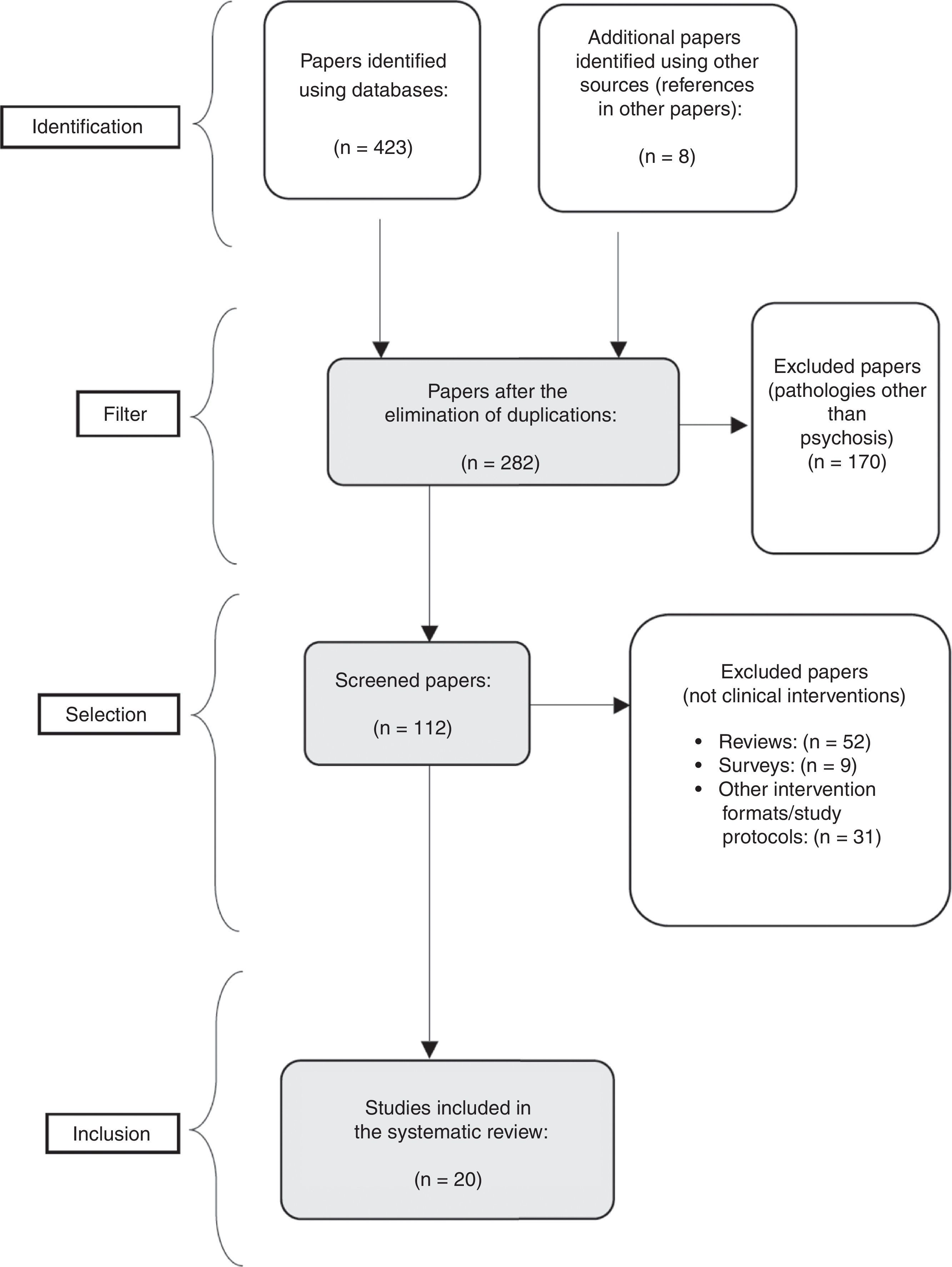
The publications were first screened by reading their titles and summaries of their results contained in the databases, checking to see whether they fitted the above criteria. In a second phase the papers that had not been excluded were read completely, to evaluate whether they fitted our search criteria. Their references were also studied to find new publications that would complete our registry (Fig. 1).
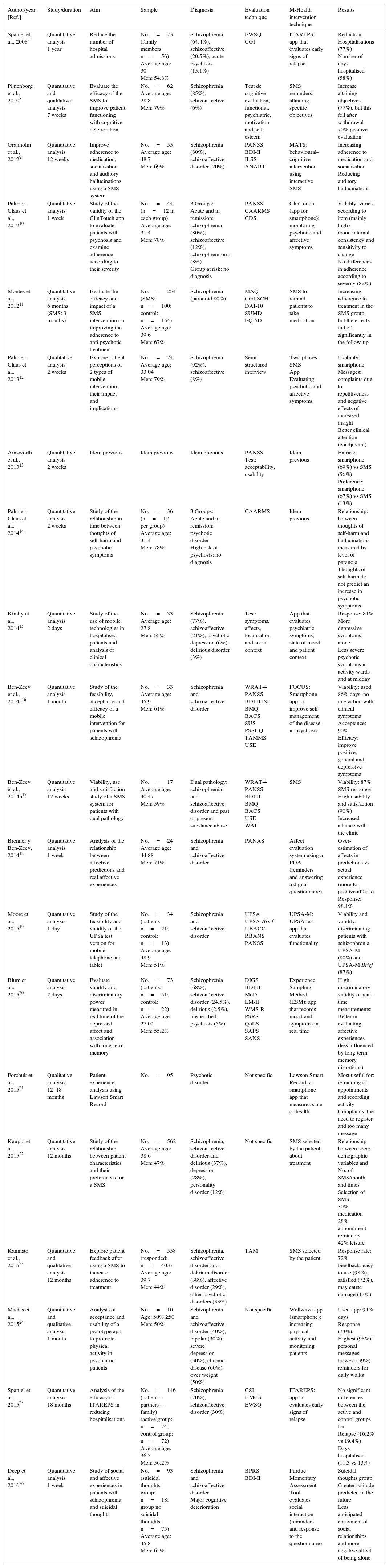
The papers finally selected were evaluated to check: their date of publication, type of study, duration, objective, sample size, patient epidemiological data (age and sex), evaluation method (scales), m-Health intervention method, mobile device used and the results obtained. These data are shown in Table 1.
Papers included on the use of mobile applications in psychosis.
| Author/year [Ref.] | Study/duration | Aim | Sample | Diagnosis | Evaluation technique | M-Health intervention technique | Results |
|---|---|---|---|---|---|---|---|
| Spaniel et al., 20087 | Quantitative analysis 1 year | Reduce the number of hospital admissions | No.=73 (family members n=56) Average age: 30 Men: 54.8% | Schizophrenia (64.4%), schizoaffective (20.5%), acute psychosis (15.1%) | EWSQ CGI | ITAREPS: app that evaluates early signs of relapse | Reduction: Hospitalisations (77%) Number of days hospitalised (58%) |
| Pijnenborg et al., 20108 | Quantitative and qualitative analysis 7 weeks | Evaluate the efficacy of the SMS to improve patient functioning with cognitive deterioration | No.=62 Average age: 28.8 Men: 79% | Schizophrenia (85%), schizoaffective (6%) | Test de cognitive evaluation, functional, psychiatric, motivation and self-esteem | SMS reminders: attaining specific objectives | Increase attaining objectives (77%), but this fell after withdrawal 70% positive evaluation |
| Granholm et al., 20129 | Quantitative analysis 12 weeks | Improve adherence to medication, socialisation and auditory hallucinations using a SMS system | No.=55 Average age: 48.7 Men: 69% | Schizophrenia (80%), schizoaffective disorder (20%) | PANSS BDI-II ILSS ANART | MATS: behavioural–cognitive intervention using interactive SMS | Increasing adherence to medication and socialisation Reducing auditory hallucinations |
| Palmier-Claus et al., 201210 | Quantitative analysis 1 week | Study of the validity of the ClinTouch app to evaluate patients with psychosis and examine adherence according to their severity | No.=44 (n=12 in each group) Average age: 31.4 Men: 78% | 3 Groups: Acute and in remission: schizophrenia (80%), schizoaffective (12%), schizophreniform (8%) Group at risk: no diagnosis | PANSS CAARMS CDS | ClinTouch (app for smartphone): monitoring psychotic and affective symptoms | Validity: varies according to item (mainly high) Good internal consistency and sensitivity to change No differences in adherence according to severity (82%) |
| Montes et al., 201211 | Quantitative analysis 6 months (SMS: 3 months) | Evaluate the efficacy and impact of a SMS intervention on improving the adherence to anti-psychotic treatment | No.=254 (SMS: n=100; control: n=154) Average age: 39.6 Men: 67% | Schizophrenia (paranoid 80%) | MAQ CGI-SCH DAI-10 SUMD EQ-5D | SMS to remind patients to take medication | Increasing adherence to treatment in the SMS group, but the effects fall off significantly in the follow-up |
| Palmier-Claus et al., 201312 | Qualitative analysis 2 weeks | Explore patient perceptions of 2 types of mobile intervention, their impact and implications | No.=24 Average age: 33.04 Men: 79% | Schizophrenia (92%), schizoaffective (8%) | Semi-structured interview | Two phases: SMS App Evaluating psychotic and affective symptoms | Usability: smartphone Messages: complaints due to repetitiveness and negative effects of increased insight Better clinical attention (coadjuvant) |
| Ainsworth et al., 201313 | Quantitative analysis 2 weeks | Idem previous | Idem previous | Idem previous | PANSS Test: acceptability, usability | Idem previous | Entries: smartphone (69%) vs SMS (56%) Preference: smartphone (67%) vs SMS (13%) |
| Palmier-Claus et al., 201414 | Quantitative analysis 2 weeks | Study of the relationship in time between thoughts of self-harm and psychotic symptoms | No.=36 (n=12 per group) Average age: 31.4 Men: 78% | 3 Groups: Acute and in remission: psychotic disorder High risk of psychosis: no diagnosis | CAARMS | Idem previous | Relationship: between thoughts of self-harm and hallucinations measured by level of paranoia Thoughts of self-harm do not predict an increase in psychotic symptoms |
| Kimhy et al., 201415 | Quantitative analysis 2 days | Study of the use of mobile technologies in hospitalised patients and analysis of clinical characteristics | No.=33 Average age: 27.8 Men: 55% | Schizophrenia (77%), schizoaffective (21%), psychotic depression (6%), delirious disorder (3%) | Test: symptoms, affects, localisation and social context | App that evaluates psychiatric symptoms, state of mood and patient context | Response: 81% More depressive symptoms alone Less severe psychotic symptoms in activity wards and at midday |
| Ben-Zeev et al., 2014a16 | Quantitative analysis 1 month | Study of the feasibility, acceptance and efficacy of a mobile intervention for patients with schizophrenia | No.=33 Average age: 45.9 Men: 61% | Schizophrenia and schizoaffective disorder | WRAT-4 PANSS BDI-II ISI BMQ BACS SUS PSSUQ TAMMS USE | FOCUS: Smartphone app to improve self-management of the disease in psychosis | Viability: used 86% days, no interaction with clinical symptoms Acceptance: 90% Efficacy: improve positive, general and depressive symptoms |
| Ben-Zeev et al., 2014b17 | Quantitative analysis 12 weeks | Viability, use and satisfaction study of a SMS system for patients with dual pathology | No.=17 Average age: 40.47 Men: 59% | Dual pathology: schizophrenia and schizoaffective disorder and past or present substance abuse | WRAT-4 PANSS BDI-II BMQ BACS USE WAI | SMS | Viability: 87% SMS response High usability and satisfaction (90%) Increased alliance with the clinic |
| Brenner y Ben-Zeev, 201418 | Quantitative analysis 1 week | Analysis of the relationship between affective predictions and real affective experiences | No.=24 Average age: 44.88 Men: 71% | Schizophrenia and schizoaffective disorder | PANAS | Affect evaluation system using a PDA (reminders and answering a digital questionnaire) | Over-estimation of affects in predictions vs actual experience (more for positive affects) Response: 98.1% |
| Moore et al., 201519 | Quantitative analysis 1 day | Study of the feasibility and validity of the UPSa test version for mobile telephone and tablet | No.=34 (patients n=21; control: n=13) Average age: 48.9 Men: 51% | Schizophrenia and schizoaffective disorder | UPSA UPSA-Brief UBACC RBANS PANSS | UPSA-M: UPSA test app that evaluates functionality | Viability and validity: discriminating patients with schizophrenia, UPSA-M (80%) and UPSA-M Brief (87%) |
| Blum et al., 201520 | Quantitative analysis 2 days | Evaluate validity and discriminatory power measured in real time of the depressed affect and association with long-term memory | No.=73 (patients: n=51; control: n=22) Average age: 27.02 Men: 55.2% | Schizophrenia (68%), schizoaffective disorder (24.5%), delirious (2.5%), unspecified psychosis (5%) | DIGS BDI-II MoD LM-II WMS-R PSRS QoLS SAPS SANS | Experience Sampling Method (ESM): app that records mood and symptoms in real time | High discriminatory validity of real-time measurements: Better in evaluating affective experiences (less influenced by long-term memory distortions) |
| Forchuk et al., 201521 | Qualitative analysis 12–18 months | Patient experience analysis using Lawson Smart Record | No.=95 | Psychotic disorder | Not specific | Lawson Smart Record: a smartphone app that measures state of health | Most useful for: reminding of appointments and recording activity Complaints: the need to register and too many message |
| Kauppi et al., 201522 | Quantitative analysis 12 months | Study of the relationship between patient characteristics and their preferences for a SMS | No.=562 Average age: 38.6 Men: 47% | Schizophrenia, schizoaffective disorder and delirious (37%), depression (28%), personality disorder (12%) | Not specific | SMS selected by the patient about treatment | Relationship between socio-demographic variables and No. of SMS/month and times Selection of SMS: 30% medication 28% appointment reminders 42% leisure |
| Kannisto et al., 201523 | Quantitative and qualitative analysis 12 months | Explore patient feedback after using a SMS to increase adherence to treatment | No.=558 (responded: n=403) Average age: 39.7 Men: 44% | Schizophrenia, schizoaffective disorder and delirium disorder (38%), affective disorder (29%), other psychotic disorders (33%) | TAM | SMS selected by the patient | Response rate: 72% Feedback: easy to use (98%), satisfied (72%), may cause damage (13%) |
| Macias et al., 201524 | Quantitative and qualitative analysis 1 month | Analysis of acceptance and usability of a prototype app to promote physical activity in psychiatric patients | No.=10 Age: 50% ≥50 Men: 50% | Schizophrenia and schizoaffective disorder (40%), bipolar (30%), severe depression (30%), chronic disease (60%), over weight (50%) | Not specific | Wellwave app (smartphone): increasing physical activity and monitoring patients | Used app: 94% days Response (73%): Highest (98%): personal messages Lowest (39%): reminders for daily walks |
| Spaniel et al., 201525 | Quantitative analysis 18 months | Analysis of the efficacy of ITAREPS in reducing hospitalisations | No.=146 (patient – partners – family) (active group: n=74; control group: n=72) Average age: 36.5 Men: 56.2% | Schizophrenia (70%), schizoaffective disorder (30%) | CSI HMCS EWSQ | ITAREPS: app tat evaluates early signs of relapse | No significant differences between the active and control groups for: Relapse (16.2% vs 19.4%) Days hospitalised (11.3 vs 13.4) |
| Deep et al., 201626 | Quantitative analysis 1 week | Study of social and affective experiences in patients with schizophrenia and suicidal thoughts | No.=93 (suicidal thoughts group: n=18; group no suicidal thoughts: n=75) Average age: 45.8 Men: 62% | Schizophrenia and schizoaffective disorder Major cognitive deterioration | BPRS BDI-II | Purdue Momentary Assessment Tool: evaluates social interaction (reminders and response to the questionnaire) | Suicidal thoughts group: Greater solitude predicted in the future Less anticipated enjoyment of social relationships and more negative affect of being alone |
ANART: American National Adult Reading Test; BACS: Brief Assessment of Cognition in Schizophrenia; BDI-II: Beck Depression Inventory-2 Edition; BMQ: Brief Medication Questionnaire; BPRS: Brief Psychotic Rating Scale; CAARMS: Comprehensive Assessment of At Risk Mental State; CDS: Calgary Depression Scale; CGI: Clinical Global Impression; CGI-SCH: Clinical Global Impression-Schizophrenia scale; CSI: Clinical Global Impression Scale; DAI-10: 10 – item Drug Attitude Inventory; EQ-5D: Health Quality of life assessed using the second part of the Spanish version of the EuroQol; EWSQ: Early Warning Sings Questionnaire; HMCS: Hayward Medication Compliance Scale Score; ILSS: Independent Living Skills Survey; ISI: Insomnia Severity Index; ITAREPS: Information Technology Aided Relapse Prevention Programme in Schizophrenia; LM-II: Logical Memory II; MAQ: Morisky Green Adherence Questionnaire; MATS: Mobile Assessment and Treatment for Schizophrenia; MoD: Experience Sampling Method with Mobile Devices; PANAS: Positive and Negative Affect Schedule; PANSS: Positive and Negative Syndrome Scale; PDA: personal digital assistants; PSRS: Provision of Social Relations Scale; PSSUQ: Post Study System Usability Questionnaire; QoLQ: Quality of Life Questionnaire; RBANS: Repeatable Battery for the Assessment of Neuropsychological Status; SANS: Scale for the Assessment of Negative Symptoms; SAPS: Scale for the Assessment of Positive Symptoms; SMS: short message service; SUMD: Scale to Assess Unawareness of Mental Disorder; SUS: System Usability Scale; TAM: Technology Acceptance Model; TAMMS: Technology Assessment Model Measurement Scales; UBACC: UCSD-Brief Assessment of Capacity to Consent; UPSA: University of California San Diego (UCSD) Performance Skills Assessment; USE: Usability and User Experience; WAI: Working Alliance Inventory; WMS-R: Wechsler Memory Scale-Revised; WRAT-4: Wide Range Achievement Test (reading subsection)-Fourth Edition.
As Fig. 1 shows, at first a total of 431 papers were identified. These were reduced to 112 after the elimination of duplications and publications that were not about patients with psychotic disorders. After this, 92 publications were excluded as they did not refer to clinical interventions but were rather systematic reviews (57%), surveys (10%) and study protocols or other intervention formats (33%). Finally a sample of 20 papers was selected, of which 17 were independent interventions.7–26
Of these interventions, 35% were published from 2008 to 2014 and 65% were published from 2014 to 2016. 75% analysed data quantitatively, 10% were qualitative and 15% used both types of analysis. The duration of these studies runs from transversal studies of a single day's intervention to follow-up studies lasting for 18 months.
The average total number of participants per study is 113. However, if the outlying values of 2 studies with samples of 562 and 558 subjects are eliminated, this average falls to 63 participants per study. The total average age of the participants is 37.3 years old. In 90% of the interventions the percentage of men is higher than that of women. The main diagnosis of the participants is schizophrenia, followed by schizoaffective disorder.
The most common evaluation methods use standardised scales, although their own scales were designed in 15% of studies. 3 types of interventions were differentiated: interventions using PDA (10%), SMS services (25%) and smartphone apps (50%). The remaining 15% used SMS and app interventions simultaneously.
The objectives may be divided into 3 major sets of interventions:
- 1)
Analysis of the quality and usability of mobile interventions: 11 interventions have the aim of analysing the validity, feasibility, usability and utility of interventions using mobile devices.10,12,13,16,17,19–24
Four studies analysed the usability and viability of their interventions; among these, Ainsworth et al.13 offered the possibility of choosing between an app or SMS, and they found that patients used the app service 13% more than they did the SMS. Ben-Zeev et al.16 observed that the FOCUS app for improving self-management of the disease was used on 86% of days, with a 90% acceptance rate, while in his second study,17 90% of the patients used a text messaging service and were satisfied with it. Finally, in the study by Macias et al.24 the Wellwave app, which encourages walking every day, was used on 94% of days, although only 39% of answers were confirmations to the daily reminders to take a walk that this activity had been undertaken.
Three studies analysed the discriminatory validity of the devices. The study by Moore et al.19 shows the validity of a mobile application that implements the UCSD Performance-Based Skills Assessment (UPSA). This evaluates its functionality in discriminating patients with schizophrenia (80%). The study by Blum et al.20 confirmed the discriminatory validity of momentary measurements to evaluate depressive state of mood, and the one by Palmier-Claus et al.10 concluded the validity, internal consistency and sensitivity of the switch to the ClinTouch app, which monitors psychotic and affective symptoms.
Finally, 4 studies analysed patient perceptions and opinions after they had used different types of mobile interventions. In the study by Palmier-Claus et al.12 the participants would prefer to use a mobile app rather than a SMS, and they complained about the repetitive nature of messages and the negative effects of constantly focussing their attention on their symptoms. In the study by Forchuk et al.21 the participants stated that the most useful functions of the Lawson Smart Record app were the appointment reminder, while their complaint referred to the excessive number of messages and the laborious nature of using the system. In the study by Kauppi et al.22 the patients expressed their preference for reminders associated with leisure (42%) and medication (30%). And to finish, in the study by Kannisto et al.,23 98% of the patients considered that SMS is easy to use, while 13% considered that they may be harmful.
- 2)
Improving adherence, symptoms and reducing hospitalisations: 5 interventions aim to increase adherence to antipsychotic treatments, improve symptoms and reduce hospitalisations.7–9,11,25
Two studies used the SMS to improve adherence to medication: the study by Granholm et al.9 increased adherence to medication and improved other symptoms of schizophrenia (socialisation and auditory hallucinations) by means of a mobile cognitive-behavioural intervention. The study by Montes et al.11 used the SMS to remind patients to take their medication and increased adherence, although the results were not maintained following the end of this service. Two studies seek to reduce the number of admissions to hospital by using the ITAREPS application: in the first study by Spaniel et al.7 in 2008, a fall of 77% was found, while in the 201525 study no significant differences were observed between those participants who used this app and those who did not. Finally, the intervention by Pijnenborg et al.8 used the SMS to increase the functionality of psychotic patients, obtaining a 77% improvement in the attainment of objectives.
- 3)
The analysis of patient symptoms: 4 interventions used mobile devices to measure clinical variables associated with patient emotions and thoughts.14,15,18,26
Two studies analysed thoughts of self-harm: the study by Palmier-Claus et al.14 found a relationship between the worsening of auditory hallucinations and thoughts of self-harm, measured by degree of paranoia. Deep et al.26 observed that patients with symptoms of self-harm presented greater negative affect when they were alone, predicting increased solitude in the future. Two studies analyse patient affects: the study by Kimhy et al.15 found by using an app that patients experience more depressive and psychotic symptoms when they are alone, while the study by Brenner and Ben-Zeev18 observed by using a PDA that patients over-estimate predictions and their affects, chiefly the positive ones.
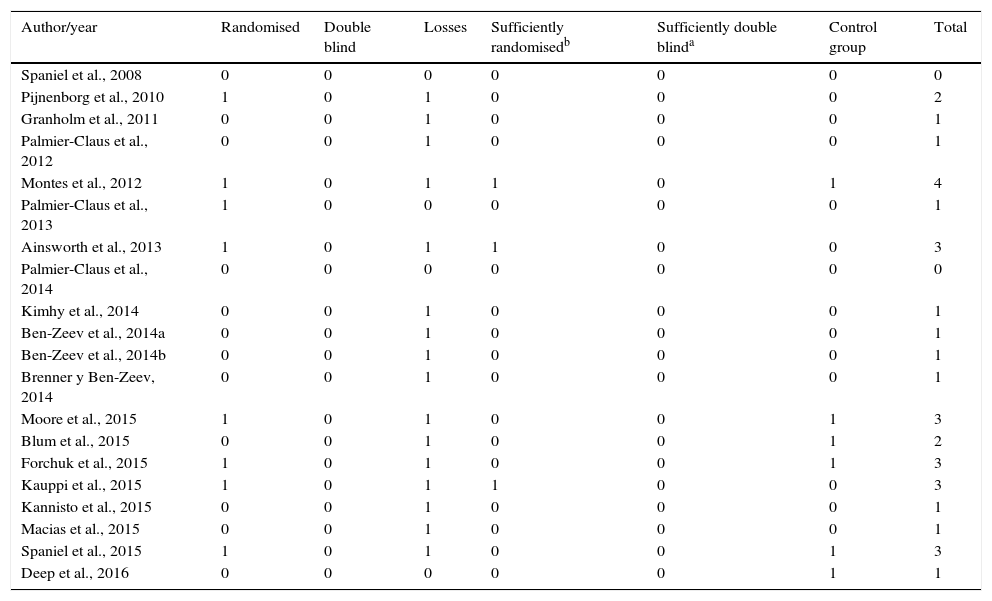
Finally, the methodological quality of the interventions was analysed using a Jadad scale that includes: randomisation, masking/double blind and a description of losses during follow-up.27 The variable of the existence or not of a “control group” was added to the said scale. We considered scales to be of poor quality when they scored less than 3 points, and they were considered to be of maximum quality at 5 and 6 points. These data are shown in Table 2.
The methodological quality of the studies analysed.
| Author/year | Randomised | Double blind | Losses | Sufficiently randomisedb | Sufficiently double blinda | Control group | Total |
|---|---|---|---|---|---|---|---|
| Spaniel et al., 2008 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pijnenborg et al., 2010 | 1 | 0 | 1 | 0 | 0 | 0 | 2 |
| Granholm et al., 2011 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Palmier-Claus et al., 2012 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Montes et al., 2012 | 1 | 0 | 1 | 1 | 0 | 1 | 4 |
| Palmier-Claus et al., 2013 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| Ainsworth et al., 2013 | 1 | 0 | 1 | 1 | 0 | 0 | 3 |
| Palmier-Claus et al., 2014 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Kimhy et al., 2014 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Ben-Zeev et al., 2014a | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Ben-Zeev et al., 2014b | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Brenner y Ben-Zeev, 2014 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Moore et al., 2015 | 1 | 0 | 1 | 0 | 0 | 1 | 3 |
| Blum et al., 2015 | 0 | 0 | 1 | 0 | 0 | 1 | 2 |
| Forchuk et al., 2015 | 1 | 0 | 1 | 0 | 0 | 1 | 3 |
| Kauppi et al., 2015 | 1 | 0 | 1 | 1 | 0 | 0 | 3 |
| Kannisto et al., 2015 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Macias et al., 2015 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Spaniel et al., 2015 | 1 | 0 | 1 | 0 | 0 | 1 | 3 |
| Deep et al., 2016 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
0=no; 1=yes.
No study attained the highest score for methodology, as the lack of masking was their main limitation. The study by Montes et al.11 scored the highest for methodological quality, at 4 on the Jadad scale, followed by the studies by Ainsworth et al.,13 Moore et al.,19 Forchuk et al.,21 Kauppi et al.22 and Spaniel et al.,25 which all scored 3.
DiscussionAll of the 20 studies analysed in this systematic review confirm the growing clinical interest in interventions using mobile devices for psychotic patients, given that 65% of the articles found that were written in the past 26 years were published from 2014 to 2016. This is reasonable, given that smartphone use had only spread to 21% of the population in Western Europe in 2013.
Mobile interventions were shown throughout the studies analysed to be a viable strategy for psychotic patients. Patient response to communications using devices is above 70% in the studies that analyse this variable.9,10,13,15–18,24,25 Additionally, when patients responses are studied, the majority express their satisfaction with these interventions, finding them useful, beneficial and easy to use.8,9,12,13,16,17,23,24 No relationship was found between patient symptoms16 and their severity10 when responding to reminders. All of this suggests that these interventions are suitable and well-accepted by patients.
Nevertheless, and in spite of the generally positive results of these interventions, small percentages of patients (10–12%) said they encountered difficulties in using these devices16 and consider that too many communications per day may be found intrusive and tedious.12,21 In turn, in 2 studies a minority of the sample thought that the continuous recording of symptoms increased their worries and thoughts about the disease.12,23 Nevertheless, these were isolated cases which never brought about a worsening in the health of the patients, so that these problems are not significant or widespread.
The real-time evaluation of patient symptoms, cognitions, emotions and behaviour using mobile applications has been shown to achieve good validity and correlation with traditional psycho-pathological evaluation scales.12,14,15,18–20,25 Regarding the benefits of these interventions in improving adherence to treatment, reducing hospitalisation and improving psychiatric symptoms, the results are promising.7–9,11,16 All of the studies which gather data on the symptoms have an alarm system to urgently respond to the patient if they have suicidal ideas or symptoms that indicate a psychotic relapse. These benefits increase the more a device is used and are reduced if a device is withdrawn, while improved attitudes to medication, social relationships and symptoms are maintained over time.9,11
These studies contain multiple limitations that have to be taken into account. Firstly, the methodological quality of the studies analysed is quite low. This is due to the nature of the psycho-social interventions, which prevents the use of masking, together with the lack of randomisation in the sample selection of some studies. Secondly, the short duration of some of these studies and the small size of some of their samples render them insufficient to obtain results that are conclusive and which can be extrapolated. Thirdly, 25% of these publications include a qualitative analysis of the data which, although it may increase internal validity, is more liable to distortion by the patients and hinders the external validity of the conclusions. When scales are used to measure the acceptability and usability of devices, these scales are not validated for mental health or schizophrenia in particular. Fourthly, as Ben-Zeev et al.17 underline, patients respond to device communications without any supervision by medical staff, so that it is impossible to directly check the quality and emotional context of their answers.
This review has shown that mobile interventions are potentially viable, usable, acceptable, valid and beneficial for patients’ mental health in improving the self-management and treatment of psychotic disorders. These devices make real-time recording possible, not only of patient symptoms but also of their associated ecosystem. They are more reliable than the retrospective records obtained when patients visit, above all if they present cognitive deterioration.20 They are therefore able to help to improve the quality of clinical decisions, and to aid patients in giving a more accurate description of their experiences.18 They also make it possible to reduce the distance between research and clinical practice and between patients and healthcare staff.17 Nevertheless, one problem with these studies are the ethical and practical questions about confidentiality and data use. In the studies that collect clinical data, these will only be accessible to the research personnel using a specific password. Although this resolves the problem of confidentiality, it does not clarify how to translate research data into clinical practice. Finally, the early detection of symptoms using real-time recording systems and reducing the number of visits by patients to the surgery may lead to an economic saving for healthcare services (above all in preventing admissions to hospital). However, we are not aware of any economic study that proves the efficiency (a good cost/effectiveness ratio) of these devices.
Higher methodological quality research is needed in the future to analyse the reliability of these interventions and to make it possible to extrapolate the above-mentioned benefits. Nor has the long-term effect of these interventions been studied, or whether the results and patient involvement are maintained over time. Finally, in reply to the complaints expressed by patients, it is indispensible to develop devices that are simple and easy to use, in direct collaboration with the patients themselves. The core objectives of these devices must be firstly to achieve a suitable degree of application integration in patients’ everyday lives, without interfering in them, and secondly to tailor them to their specific needs and interests.22,23
FundingA “Prometeo” support grant from the Conselleria de Sanidad de la Comunidad Valenciana.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Bonet L, Izquierdo C, Escartí MJ, Sancho JV, Arce D, Blanquer I, et al. Utilización de tecnologías móviles en pacientes con psicosis: una revisión sistemática. Rev Psiquiatr Salud Ment (Barc.). 2017;10:168–178.