Functional impairment in schizophrenia is one of the main features of the disorder and implies a great impact on the patient's quality of life. The Brief Functioning Assessment Scale (FAST), originally validated in bipolar disorder, has also been validated for its application in other mental disorders. However, we only found one study on the reliability and validity of the Brazilian version in schizophrenia. The purpose of this study was to analyze the psychometric properties of the Spanish version of the FAST in patients diagnosed with schizophrenia.
Material and methodsA total of 226 patients with a diagnosis of schizophrenia were evaluated by mean the FAST, the GAF and the self-care requirements scale (ERA). Scale properties were analyzed in terms of internal consistency, inter-observer agreement and test-retest reliability. Convergent validity with the GAF and ERA scales was also analyzed, as well as construct validity by means of a Confirmatory Factor Analysis (CFA).
ResultsFor the total scale, the results showed high internal consistency (Cronbach's Alpha of, 87), as well as good inter-observer (ICC=,86) and test-retest (ICC=,77) agreement. Concurrent validity with the GAF scale was discrete (r=−,32; P<,001) and with the ERA scale was moderate (r=,50; P<,001). CFA showed an internal structure that matched the six factors proposed by the original scale, with a good level of item saturation for each factor.
ConclusionsThe FAST scale showed good psychometric properties in terms of reliability and validity in its Spanish version for its application in patients with schizophrenia. It can be considered as a good tool to assess different areas of functional impairment in clinical practice and research.
El deterioro funcional es una de las principales características del curso de la esquizofrenia e implica un gran impacto en la calidad de vida del paciente. La escala de funcionamiento breve (FAST) validada originalmente en trastorno bipolar también ha sido validada para su aplicación en otros trastornos mentales, aunque solo encontramos un estudio sobre la fiabilidad y validez de la versión brasileña en esquizofrenia. El propósito de este estudio fue analizar las propiedades psicométricas de la versión española de la FAST en pacientes diagnosticados de esquizofrenia.
Material y métodosUn total de 226 pacientes con diagnóstico de esquizofrenia fueron evaluados, cumplimentando la FAST, la GAF y la escala de requisitos de autocuidado (ERA). Se analizaron las propiedades de la escala en términos de consistencia interna, concordancia inter-observador y fiabilidad test-retest. Se analizó también la validez convergente con las escalas GAF y ERA, y la validez de constructo mediante un Análisis Factorial Confirmatorio (AFC).
ResultadosPara el total del cuestionario, los resultados mostraron una elevada consistencia interna (Cronbach’s Alpha de, 87), así como una buena concordancia inter-observador (CCI=,86) y test-retest (CCI=,77). La validez concurrente con la escala GAF fue discreta (r=−,32; P<,001) y con la escala ERA moderada (r=,50; P<,001). El AFC mostró una estructura interna que se ajustaba a los seis factores de la escala original, con un buen nivel de saturación de los ítems para cada factor.
ConclusionesLa escala FAST mostró buenas propiedades psicométricas en términos de fiabilidad y validez en su versión española para su aplicación en pacientes con esquizofrenia. Se puede considerar una buena herramienta para evaluar diferentes áreas del deterioro funcional en la práctica clínica y en investigación.
Schizophrenia is characterised by profound cognitive and emotional impairment, affecting a number of areas of daily functioning, including deficits in social, occupational, or autonomous functioning (paying bills, taking the bus…), even during periods when psychotic symptomatology is in remission,1 leading to a major impact on quality of life.2 At least 2/3 of these patients are unable to achieve major life milestones such as getting a job, and more than half of them have difficulty maintaining stable relationships.3 As a result, 80%–90% of all people with schizophrenia exhibit significant functional (social or occupational) impairment compared to what might be expected based on their premorbid level of functioning or family level.4 These deficits in different areas of functioning cause schizophrenia to be considered one of the most disabling conditions in adults, with a prevalence of 24 million people worldwide.5
To assess the impact of rehabilitative therapeutic measures, and to improve the understanding of the course of the illness, the functioning of individuals with schizophrenia must be quantified.6 This is also necessary in order to adjust health system planning, given that diagnosis alone does not predict the need for services, days of hospitalisation, work performance, etc.7 What clearly impacts the health care costs associated with schizophrenia is symptomatic severity and impaired functioning on a day-to-day basis.8 Nevertheless, functioning is a complex construct that encompasses many different domains from personal, occupational, or recreational contexts,9 thereby making it challenging to obtain a comprehensive measure that captures all areas of functioning and reflects the patient's true status.
The tools most commonly used in clinical practice to assess functioning are global assessment scales; these scales focus on evaluating functioning as a single dimension, rather than appraising each of its component dimensions. Such is the case of the Global Assessment of Functioning Scale (GAF). These kinds of scales are limited with regard to their use in psychiatry; they do not distinguish well between clinical and functional recovery,10 and, by not including all areas of functioning, they are also limited in providing complete information about the patient's level of decline and recovery.
On the other hand, we have found an instrument designed in Spanish to measure self-care requirements, specifically designed for patients with schizophrenia, the Escala de Requisitos de Autocuidado (ERA). This scale was designed to enable nursing professionals to design a care plan by assessing patients' ability to care for themselves, an ability that has to do with global functioning.11 However, there is shortage of tools adapted to the Spanish population to assess daily functioning in people with severe mental disorders, especially schizophrenia, as highlighted in a recent review by Gil-Palmero et al.12 This review also highlights shortcomings in the adaptation process, related to translation, confusion of concepts, or the metric properties of the instruments reviewed. The authors concluded that the conceptualisation and assessment of functioning in this field continues to be a complex and controversial issue. Among the instruments reviewed in this paper are: Life Skills Profile,13Basic Everyday Living Schedule,14Independent Living Skills Survey,15,16The WHO Disability Assessment Schedule,17Personal and Social Performance,18 the Spanish version of the Performance-Based Skills Assessment,19 and the Function Assessment Short Test (FAST).20
FAST is a brief interview designed to be administered by a trained clinician, with a brief user manual to rate each item. The assessment refers to the period of the previous 15 days and takes into consideration both the patient's response and information provided by people from their surroundings. This scale examines six areas of functioning: occupational, autonomy, cognitive, financial, interpersonal relationships, and leisure time. Originally designed in Spanish to gauge functioning in people with mental illness, it exhibits good psychometric properties in people with bipolar disorder.20 It has subsequently been adapted to different languages21–26 and validated in patients suffering from first psychotic episodes,27 attention deficit hyperactivity disorder,28 and autism spectrum disorders.29 In the case of patients with schizophrenia, we found a single study that addressed the psychometric properties of the Portuguese version of FAST, which included a group of 107 outpatients. In this study, FAST demonstrated high internal consistency (Cronbach’s alpha 0.89) and excellent test-retest reliability (ICC=0.93).30 At present, FAST is widely used in illnesses bordering on schizophrenia, such as bipolar disorder31–33 and first psychotic episodes,34–36 and is even beginning to be used without validation in schizophrenic patients,37,38 meaning that the validation of the Spanish version among people with schizophrenia would mark a step forward in the methodological improvement of studies that explore the functioning of patients with schizophrenia.
Therefore, taking into account the brevity and ease of use of FAST, the multidimensional measure it provides of patient functioning, and the good psychometric properties it has in versions in other languages and for other diagnoses, the purpose of the present study was to analyse the psychometric properties of the Spanish version of FAST for use in the population diagnosed with schizophrenia.
Material and methodsParticipantsThe study sample consisted of 226 participants with a diagnosis of paranoid schizophrenia, undifferentiated schizophrenia, residual schizophrenia, and disorganized schizophrenia according to DSM-IV (classification system in use at the recruitment centre during the period of the study). Recruitment was carried out between the months of January 2017 and December 2019 at the Adult Mental Health Centre of Granollers (Barcelona) by each patient’s reference psychiatrist or nurse. For this purpose, each psychiatrist and nurse offered all the patients they cared for during the recruitment period and who met the inclusion criteria the opportunity to participate in the study. Fifteen percent of the sample was recruited from psychiatry and 85% from nursing. Inclusion criteria to select the participants included: having a diagnosis of paranoid, undifferentiated, residual, or disorganized schizophrenia and being clinically stable; therefore, having a link to or follow-up by a psychiatrist working at the centre for at least six months was also regarded as an inclusion criterion. Exclusion criteria included: being in the acute phase of the disease or having been discharged from the acute care unit in the previous month, as well as presenting comorbidity with intellectual disability or developmental disorders.
The study was approved by the Ethics Committee of the Benito Menni Mental Health Care Complex (Reference PR 2017-2018). The study was conducted in accordance with the guidelines of the Helsinki Declaration.39 All participants gave their voluntary consent to participate in the study.
InstrumentsAll participants were interviewed individually by means of an initial semi-structured interview that covered sociodemographic data (age, gender, marital status, who they live with, level of education, employment status, and degree of disability) as well as clinical variables (type of treatment: oral and/or parenteral; years of evolution of the disease, and diagnoses), in addition to the following scales and questionnaires:
- -
Brief Functioning Scale (FAST). The scale consists of 24 items with Likert-type response format with 4 response options (“no difficulty”, “average difficulty”, “moderate difficulty” and “great difficulty”) scored from 0 (“no difficulty”) to 3 (“great difficulty”). The total score is obtained by adding the score on each item, so that the scale ranges from 0 to 72, with higher scores indicating greater difficulty in functioning. The 24 items are grouped into 6 factors or dimensions of functioning: 1) autonomy: referring to the ability to do things alone and make one's own decisions; 2) occupational functioning: concerning the ability to hold a paid job, efficiency in performing work activities, that the job should be related to the area in which the person had been trained and receive a salary commensurate with the job; 3) cognitive functioning: regarding the ability to concentrate, perform simple mental calculations, solve problems, learn new information, and remember learned information; 4) financial issues: involving the ability to manage finances and spend in a balanced way; 5) interpersonal relationships: encompassing relationships with friends and family, engaging in social activities, sexual relationships, and the ability to defend ideas and opinions, and 6) leisure time: referring to the ability to engage in physical activities (sports, exercise) and enjoy hobbies. The psychometric properties of the FAST in Spain in patients with bipolar disorder40 revealed high internal consistency, with a Cronbach’s alpha coefficient of 0.909, high concurrent validity with the GAF (r=−0.903; P<.001), and high test-retest reliability (ICC=0.98; P<.001). In patients with schizophrenia, in Brazil30 the FAST has presented good internal consistency with a Cronbach’s alpha of 0.89, high concurrent validity with the GAF (r=−0.71; P<.001), and high test-retest reliability (ICC=0.93; P<.005).
- -
GAF.41 This scale assesses the patient's global functioning along a hypothetical health-illness continuum. It consists of a single item that assigns an overall level of patient activity at the time of assessment or over a predefined period of time. It is scored using a scale ranging from 0 to 100, with the following benchmarks: 0 inadequate information; 20 some danger of causing injury to others or self, occasionally failing to maintain minimal personal hygiene, or displaying significant communication impairment; 50 severe symptoms or any severe impairment of social, occupational, or educational activity; 80 existence of symptoms that are temporary and represent reactions that are to be expected to psychosocial stressors and mild impairment of social, occupational, or educational activity, and 100 satisfactory activity across a wide range of activities.
- -
ERA.11 Measures self-care requirements in individuals with schizophrenia by means of an interview. It consists of 35 items with 5 possible specific responses ranging from 1 (no impairment) to 5 (total impairment), assessing self-care impairment, and six dimensions corresponding to the eight self-care requirements of Orem42: maintenance of sufficient intake of air, water, and food; provision of care associated with elimination process; maintenance of balance between activity and rest; maintenance of balance between solitude and social interaction; anticipation of dangers to the well-being of human life, and promotion of human functioning. It has evidenced good internal consistency in its Spanish version validated in patients with schizophrenia (Chronbach’s Alpha of 0.87).11
Between the months of January 2017 and December 2019, all patients with a diagnosis of paranoid schizophrenia, undifferentiated schizophrenia, residual schizophrenia, or disorganized schizophrenia at the Adult Mental Health Centre of Granollers (Barcelona) were included by each patient's psychiatrist or nurse of reference. For this purpose, all the psychiatrists and nurses who were attending during those months were asked to explain the study to all the patients who met the inclusion criteria to participate in it and to offer them the chance to take part in it. All those who accepted were individually scheduled for evaluation. After signing the informed consent form, the scales were administered in the following order: FAST, GAF, and ERA. The evaluations were carried out by two researchers previously trained in the application of all three scales.
With the aim of analysing test-retest reliability, a total of 74 patients were randomly selected from the total number of patients evaluated and were scheduled for a second appointment, after a period of 1–2 weeks from the first evaluation; the FAST scale was administered at this second appointment. In addition, to gauge interobserver agreement, 50 patients were randomly selected from the total sample to be evaluated by another rater blinded to the first evaluation, who administered the FAST scale again.
Statistical analysesTo determine whether any of the sociodemographic variables were related to the FAST scores, Pearson's correlation statistic and ANOVA group comparison analysis were used.
To determine FAST reliability, internal consistency was evaluated using Cronbach's alpha reliability coefficient for the total scale and for each of its six factors. Secondly, interobserver agreement was probed by means of the intraclass correlation coefficient (ICC) for the total scale and for each of the factors in a sample of 50 patients. Test-retest reliability was assessed in a sample of 74 patients using the ICC.
Convergent validity was determined with the score on the GAF scale and on the ERA scale by means of the ICC. Additionally, the relationship between the cut-off points for GAF and FAST severity grading (no, minimal, mild, moderate, and severe impairment) proposed by Amoretti43 was studied in patients with first psychotic episodes, using a Chi-square analysis and the Gamma coefficient to determine the degree of association.44
Finally, to analyse construct validity, a confirmatory factor analysis was performed to verify the original 6-factor internal structure. Parameter estimation was carried out using the least squares method. The Root Mean Square Error of Approximation (RMSEA) and Root Mean Standard Error (RMSE) and the Comparative Fit Index (CFI) and Goodness-of-Fit Index (GFI) were used to appraise the fit of the confirmatory factor analysis models and their stability to the data. In addition, different incremental indices were calculated: the Adjusted Goodness-of-fit Index (AGFI) and the Bentler Bonnet Normed Fit Index (BBNFI) and Bentler Bonnet Non-Normed Fit Index (BBNNFI). Finally, with respect to the parsimony index, the standardized Chi-square was used, defined as the ratio between the Chi-square value and the number of degrees of freedom.
Data analysis was performed using the SPSS version 25.0 statistical package (IBM® Statistical Package for the Social Sciences, SPSS) and the EQS structural equations program (EQS 6.1 for Windows, Multivariate Software, Inc., Encino, CA, USA).
ResultsSociodemographic characteristicsOf an initial sample of 279 patients, 38 declined to participate in the study or dropped out and 15 were excluded because they were in the decompensated phase or had a developmental disorder. The final sample, consisting of 226 patients, had a mean age of 44.39 years (SD 11.42), the majority of whom were male, 69%. The marital status with the highest percentage was single in 76.5%; 15.5% lived alone, and 53.1% lived with their family of origin. Eighty-seven point six percent had primary and/or secondary education and only 10.2% were actively employed. A total of 80.5% had some degree of disability. Of the total sample, 87.6% were diagnosed with paranoid schizophrenia, 46.9% of whom had been suffering from the disease for more than 15 years. Some 52.2% were receiving oral treatment. Of the 52%, 32.5% are being treated with clozapine, followed by 23.1% with olanzapine. All sociodemographic and clinical variables, as well as FAST scores in each of the subgroups according to these variables are shown in Table 1.
Sociodemographic and clinical variables.
| N | % | Mean FAST score | SD | F | P | |
|---|---|---|---|---|---|---|
| Age | 44.39 years (SD 11.42) | r=–.03 | .58 | |||
| Sex | ||||||
| Male | 158 | 69.9 | 35.67 | 10.88 | .008 | .93 |
| Female | 68 | 30.1 | 35.82 | 11.92 | ||
| Marital status | ||||||
| Single | 173 | 76.5 | 36.51 | 10.78 | 1.60 | .18 |
| Married or partnered | 24 | 11.2 | 35.86 | 12.31 | ||
| Separated-divorced | 24 | 10.6 | 30.75 | 11.74 | ||
| Widowed | 5 | 2.2 | 31.60 | 14.32 | ||
| Lives with | ||||||
| Alone | 35 | 15.5 | 35.40 | 11.63 | .15 | .93 |
| With their own family | 32 | 14.2 | 35.43 | 11.46 | ||
| Family of origin | 120 | 53.1 | 35.52 | 11.38 | ||
| Others | 39 | 17.3 | 36.82 | 10.20 | ||
| Level of studies | ||||||
| Primary studies | 148 | 65.5 | 35.02 | 11.17 | .71 | .55 |
| Secondary studies | 50 | 22.1 | 36.56 | 11.43 | ||
| University studies | 12 | 5.3 | 39.08 | 11.97 | ||
| No studies | 16 | 7.1 | 36.93 | 10.08 | ||
| Employment status | ||||||
| Pensioner | 168 | 74.3 | 35.18 | 11.22 | .74 | .48 |
| Actively employed | 23 | 10.2 | 37.30 | 10.92 | ||
| Unemployed | 35 | 15.5 | 31.27 | 10.66 | ||
| Degree of disability | ||||||
| Yes | 182 | 80.5 | 35.77 | 10.81 | .03 | .87 |
| No | 44 | 19.5 | 35.47 | 12.73 | ||
| Diagnosis of schizophrenia | ||||||
| Paranoid | 198 | 87.6 | 35.41 | 11.04 | 2.02 | .11 |
| Undifferentiated, disorganized, or residual | 28 | 13.4 | 37.8 | 12.1 | ||
| Type of treatment | ||||||
| Oral | 118 | 52.2 | 35.88 | 11.82 | 1.61 | .20 |
| Parenteral | 28 | 12.4 | 32.35 | 12.98 | ||
| Oral and parenteral | 79 | 35.0 | 36.73 | 9.31 | ||
| No treatment | 1 | 0.4 | ||||
| Years of evolution | ||||||
| Less than 5 years | 16 | 7.1 | 33.06 | 12.77 | .53 | .66 |
| Between 5 and 10 years | 53 | 23.5 | 34.88 | 8.94 | ||
| Between 10 and 15 years | 51 | 22.6 | 36.11 | 11.41 | ||
| More than 15 years | 106 | 46.9 | 36.33 | 11.87 | ||
SD: Standard Deviation.
The total sample presented a mean FAST score of 35.72 (SD=11.18). No significant relationship was found between age and FAST scores, nor were there any intergroup differences for any of the sociodemographic or clinical variables.
ReliabilityCronbach’s alpha coefficient of internal consistency for the total scale was 0.87, indicating homogeneity of the items. Additionally, the internal consistency of each of the factors was tested, obtaining values exceeding 0.70 (factor 1: 0.79; factor 2: 0.95; factor 3: 0.74; factor 4: 0.78), except for factors 5 (interpersonal relationships) with a value of 0.61 and 6 (leisure) with a value of 0.66.
The ICC for the total scale was 0.86 (P<.001), indicating good interobserver agreement. For all factors of the scale the ICC was greater than 0.70 (factor 1: 0.80; factor 2: 0.93; factor 3: 0.74; factor 4: 0.79; factor 5: 0.74; and factor 6: 0.78).
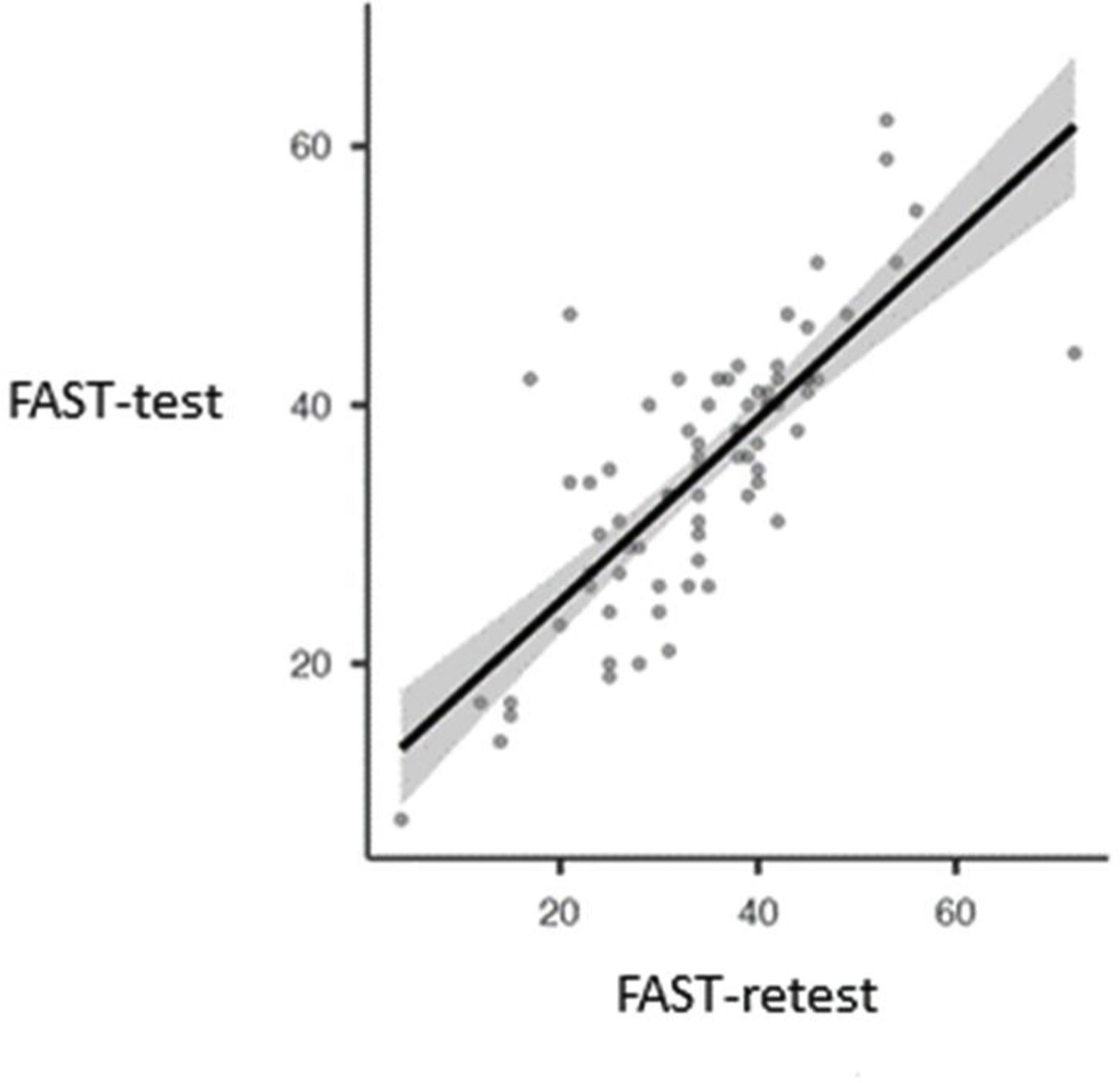
As regards test-retest reliability, the mean test score was 34.95 (SD=10.35) and retest score 34.37 (SD=11.33) (Fig. 1). The ICC was 0.77 (P<.001) indicating good test-retest agreement.
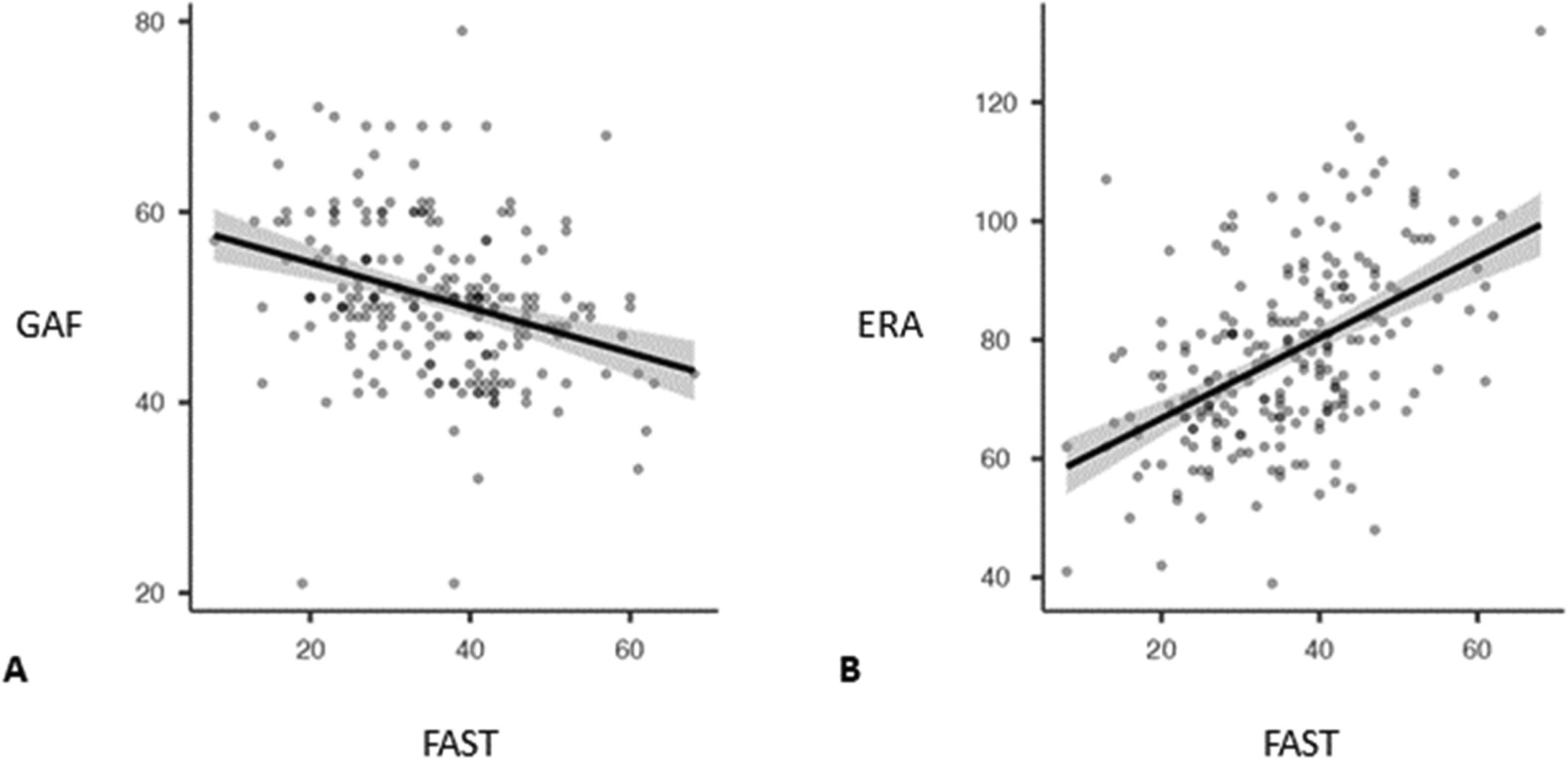
Convergent validityConvergent validity with the GAF scale exhibited a small, negative, significant correlation (r=−0.324; P<.001). Patients with higher FAST scores had lower GAF scores (Fig. 2A). With the ERA scale, FAST had a moderate, positive correlation (r=0.50; P<.001). Subjects with higher FAST scores also presented higher scores on the ERA scale, indicating a moderate convergent validity (Fig. 2B).
The 5×5 cross-tabulation resulted in a significant association of FAST and GAF severity categories (Chi-square=47.3; gl=16; P<.001). Patient classification according to FAST cut-off points was as follows: 0.9% of the sample with no impairment, 5.3% of the sample with minimal impairment, 37.6% with mild impairment, 38.9% with moderate impairment, and 17.3% with severe impairment (Table 2). The Gamma coefficient demonstrated a positive, moderate level of association, with a value of 0.50.
Contingency table between severity levels according to GAF and FAST.
| GAF | ||||||
|---|---|---|---|---|---|---|
| FAST | Severe (0−51) | Moderate (52−58) | Mild (59−68) | Minimal (69−74) | None (75−100) | Total |
| Severe (44−72) | 33 | 4 | 2 | 0 | 0 | 39 |
| Moderate (33−45) | 64 | 14 | 7 | 2 | 1 | 88 |
| Mild (34-18) | 43 | 17 | 20 | 5 | 0 | 85 |
| Minimal (19-8) | 4 | 1 | 6 | 1 | 0 | 12 |
| None (9-0) | 0 | 1 | 0 | 1 | 0 | 2 |
| Total | 144 | 37 | 35 | 9 | 1 | 226 |
ERA: Self-care Requirement Scale. Categorization based on cut offs proposed by Amoretti et al.43; FAST: Functioning Assessment Short Test; GAF: Global Assessment of Functioning.
The analysis of the internal structure of the FAST scale reveals an acceptable fit to the original model, as reflected by the CFI (0.931) and GFI (0.971) indices. The rest of the incremental indices indicate good fit of the data to the original model (RMSE=0.048; AGFI=0.964; BBNFI=0.858; BBNNFI=0.919), with a significant Chi-square (Chi-square=425.399; gl=237; P<.001) with a fit ratio of 1.79.
Factor 2 (items 5, 6, 8 and 9) and factor 4 (items 16 and 17) have the highest factor loadings or saturations, while factor 5 (items 19, 20 and 21) appears to be the worst reflected by its indicators. All the saturations are statistically significant, as illustrated in Table 3.
Factor loadings derived from LS (least squares) estimation of confirmatory factor analysis (λij).
The aim of this study was to analyse the psychometric properties of the Spanish version of the FAST test for use in the population diagnosed with schizophrenia. The results yielded good psychometric properties in terms of reliability and construct validity for its application in Spanish in patients with schizophrenia.
The internal consistency coefficient was excellent, both for the six components and for the complete scale, indicating the homogeneity of the items. Concurrent validity with the GAF scale exhibited a significant, but low negative correlation. High scores on the GAF scale are indicative of less impairment in functioning, whereas high FAST scores reflect worse functioning; therefore, this result points to the fact that well-functioning patients assessed by FAST had higher scores on the GAF scale. On the other hand, convergent validity with the ERA scale demonstrated a significant and moderate positive correlation. The test-retest analysis evidenced a high intraclass correlation, with an interval between measurements of between 7 and 15 days, which proves good reliability. The interobserver agreement analysis also showed a high intraclass correlation. Finally, the internal structure of the scale revealed a satisfactory adjustment to the factor structure of the original version.20 The factor loadings of the components were largely consistent with the a priori structure of the instrument, except for factor 5 (interpersonal relationships), which was shown to be the worst represented by its indicators.
In patients with schizophrenia, we found only one validation study of the Brazilian version of the FAST test, in which reliability and validity were assessed in a sample of 107 patients in comparison with a group of healthy controls. The results of the internal consistency analysis yielded a Cronbach's alpha similar to that of the Spanish version, while the ICC, measured in a sample of 19 patients at an interval of 6–8 months, indicated a high level of test-retest reliability, somewhat higher than that found in the Spanish version. These data confirm that the scale offers satisfactory reliability for use in individuals with schizophrenia. In this study, interobserver reliability was not investigated, which exhibits a high intraclass correlation index in our study. However, unlike the Spanish version, which presents discrete convergent validity with the GAF, a higher correlation was found in the Brazilian version. This difference may be due to the difficulty of measuring psychosocial functioning,45 together with the fact that both scales are subject to rater bias. In fact, it has been shown that the variation in GAF scores can account for more than 50% of the dispersion of scores, and deviations can be 20 points or more.46 Furthermore, it is worth mentioning that when using the categorization proposed by Amoretti,43 the “severe” category included 63.7% of patients according to the GAF and 17.3% according to FAST. This lack of agreement between the FAST and GAF in this category could be attributed to the variability of the GAF, or to the fact that the scores in the “severe” category cover a wider range, which increases the probability of patients being classified in this category.
On the other hand, to assess convergent validity, this study also used the ERA scale, designed to measure self-care requirements in schizophrenia, a construct closely related to functionality, although it does not consider dimensions such as work or cognitive functioning.11 The results demonstrated an intermediate level of correlation, which indicates that the FAST has good convergent validity, taking into account the dimensions that are common to both scales. With regard to construct validity, the confirmatory factor analysis exhibited a good fit to the model proposed in the original 6-factor scale.20 All items displayed statistically significant, high factor loadings, except for items 19 (having a good relationship with close people), 20 (living with one's own family), and 21 (having satisfactory sexual relations), belonging to factor 5 (interpersonal relationships), for which loading was less than 0.5. Therefore, further studies will be needed to determine how relevant these items are to assess the dimension of interpersonal relationships in people with schizophrenia.
This study has several limitations. First, the patient sample was comprised largely of participants with more than 15 years of disease progression, with a DSM-IV diagnosis of schizophrenia, and with at least 6 months of connection to the mental health centre; therefore, further studies are needed to analyse the psychometric properties of the scale in cases with a shorter history of the disease and with a diagnosis based on more recent diagnostic classification criteria. Furthermore, although the type of medication used was recorded, it was not included in the analyses to determine its effect on patient functionality. Second, the relationship with GAF was poor, in contrast to previous studies. Considering the GAF scores, we might consider that there is some bias towards the “severe” impairment range, so further studies will be necessary to determine the relationship between both scales. Finally, a control group was not included, and hence, we do not have data with which to analyse divergent validity.
In conclusion, the FAST scale demonstrated good psychometric properties in its Spanish version in the present sample of patients with schizophrenia. It can be regarded as a reliable and valid instrument. The FAST scale is straightforward and both quick and easy to administer, making it a good tool for assessing different areas of functional impairment in clinical and research practice in schizophrenia. Its use is spreading internationally and in Spanish-speaking countries, which makes this validation all the more pressing and relevant. However, future larger studies are needed to determine the factorial structure of the scale, and longer follow-up studies to replicate and apply the proposed cut-off points for use in clinical practice and to better characterize functionality in individuals with schizophrenia and its variability throughout the course of the illness.
FundingThe present work has been funded by the Spanish Association of Mental Health Nursing (AEESME) (XVI AEESME Research Grant Award).
Conflict of interestsNone.