There is now sufficient evidence to support the importance of interventions in the early stages of psychosis. The delay in the detection and treatment of the first-episode psychosis is related to a lower and slower recovery, as well as a higher risk of relapse. Despite this fact, early intervention units or teams are still not regularly implemented in mental health service settings in Spain. In this opinion article, a review is presented of the main arguments for defending the need to implement these programmes and strategies in order to achieve this aim. There are a number of programmes for early intervention for psychosis currently working in other countries, with a therapeutic programme that includes pharmacological and psychosocial interventions, together with public awareness, information dissemination, and family-professional collaboration activities. Published literature on the experience of these programmes indicates that early intervention is not only effective in terms of the improvement of health status, but is also economically efficient. The main steps and recommendations needed to implement such early intervention programmes in our country are described.
Actualmente existe evidencia suficiente que avala la importancia de las intervenciones en fases tempranas de la psicosis. El retraso en la detección y el tratamiento del primer episodio psicótico se asocia con una recuperación menor y más lenta, así como con un riesgo mayor de recaídas. A pesar de ello, todavía no se han implementado de forma regular programas de intervención temprana en los servicios de salud mental en España. En este artículo de opinión se revisarán los principales argumentos que nos permitan defender la necesidad de la implementación de estos programas y las estrategias a seguir para cumplir con este objetivo. Existen actualmente programas de intervención temprana para la psicosis bien establecidos en otros países que incluyen intervenciones farmacológicas y psicosociales, junto con actividades de sensibilización al público, de colaboración entre familias y profesionales y de difusión de información. Los datos publicados acerca de la experiencia de estos programas ya instaurados indican que esta atención es eficiente no solo en términos de salud, sino también desde el punto de vista económico. Se resumen en este artículo las principales acciones y estrategias para la implementación de servicios de atención temprana en nuestro país.
The lifetime prevalence of psychiatric disorders in the general population is 3%. Usual onset is at the end of adolescence or in early adulthood, which implies major personal, social and healthcare costs.1 Psychoses are broadly defined as a picture of a break with reality, impacting the way the person functions and the presence of psychotic symptoms principally including delirium and hallucinations, and more varied symptoms such as formal thought disorders, mood disorders, and the presence of motor signs.2 The concept of psychosis encompasses multiple combinations of symptoms and this results in classifying patients under several diagnoses that are included in the latest WHO International Classification of Mental and Behavioural Disorders,3 distinguishing between schizophrenia, schizoaffective disorder, persistent delusional thought disorder and bipolar disorder, amongst others.
Over the past two decades, there has been increasing interest in the early phases of psychotic and other psychiatric disorders, since the scientific evidence is that an early diagnosis and intervention can considerably improve therapeutic results4–6 and improve the effectiveness of established treatments.7
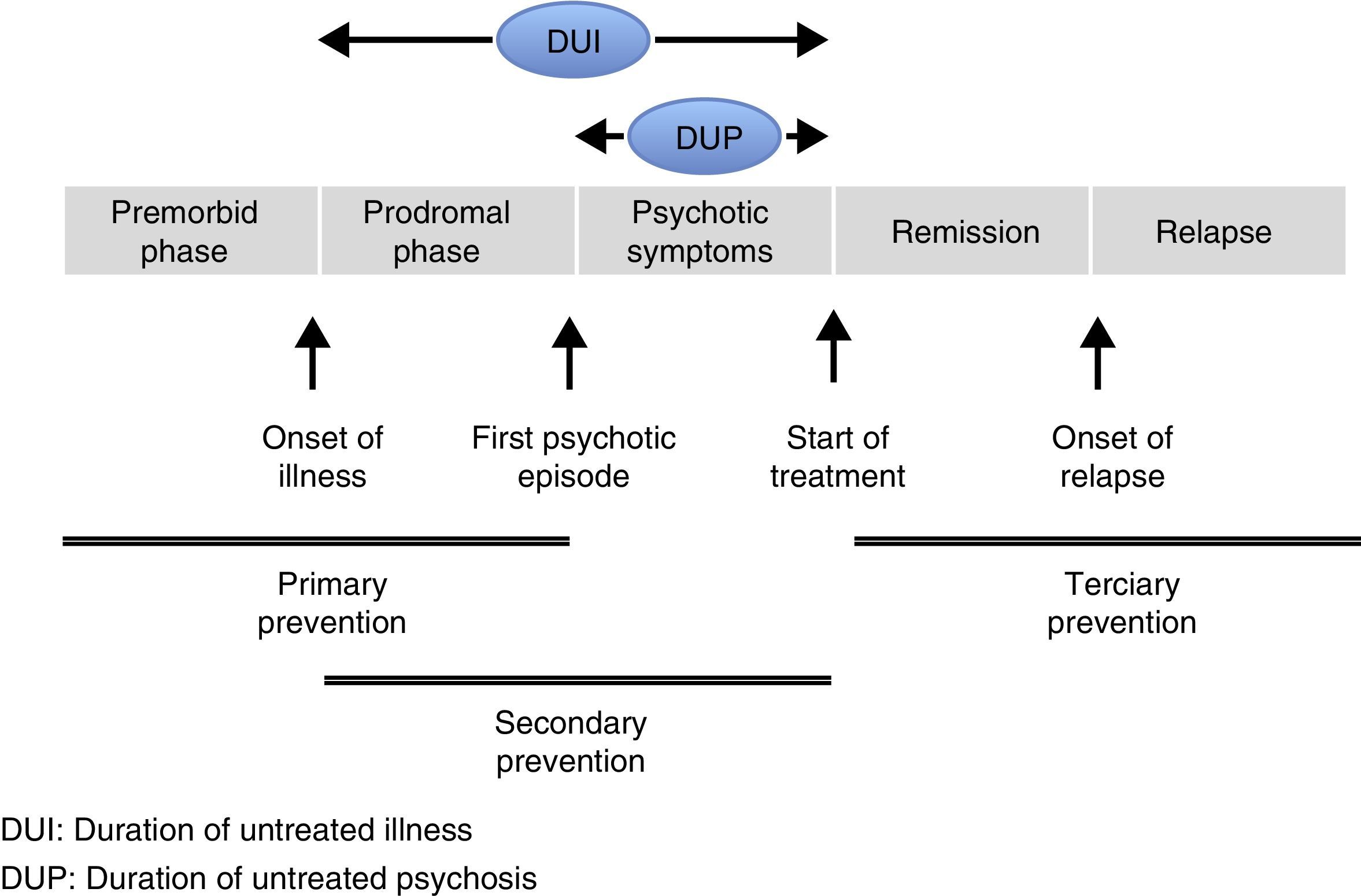
Although the onset of a first psychotic episode (FEP) can be sudden, most people present a prodromal phase that manifests through the slow and gradual development of various signs and symptoms. The premorbid phase is the period prior to the onset of prodromal symptoms (Fig. 1). The prodromal phase of psychotic disorders marks the start of symptoms and precedes an FEP, in other words, the first onset of frank psychotic symptoms.8 The prodromal phase is considered an attenuated form of psychosis that constitutes a risk factor for its development, especially if combined with other risk factors such as a family history of psychosis. In this phase, non-specific mood symptoms and behavioural changes tend to present in addition to attenuated psychotic symptoms. It should be borne in mind that the presence of prodromal symptoms does not always lead on to an FEP. After an FEP, it is considered that the first 2–5 years are crucial in the subsequent evolution of psychotic disorders.9–11 This critical period that affects long-term prognosis, supports optimised intervention in the first stages after an FEP. Intervention in these initial stages should focus not only on symptoms, but also on psychological and psychosocial aspects.12
Several studies that focus on the initial phases of psychosis have demonstrated the importance of the Duration of Untreated Illness (DUI) and the Duration of Untreated Psychosis (DUP). The DUP refers to the period of time between the first evident psychotic symptoms and the start of treatment, whereas the DUI refers to the time between the onset of prodromal symptoms and the start of treatment of psychotic symptoms. These time intervals are decisive in the prognosis and evolution of the illness. This is why strategies have been proposed towards shortening the DUP and encouraging the start of early intervention programmes, detecting prodromal symptoms and evaluating risk factors promptly.13–20 In psychiatry, as in other healthcare areas, there are three distinct traditional levels of prevention.21 Primary prevention is based on reducing the incidence of the illness. This type of prevention can be seen as universal, selective and indicated.22 Universal prevention refers to reducing the incidence of the illness regardless of risk factors. The aim of selective prevention is to focus prevention on populations whose risk of developing mental illness is considerably higher than average due to the concurrence of biological and social factors and the interaction between both. Indicated prevention is aimed at people who show the incipient signs or symptoms of a mental disorder, but who do not yet meet the diagnostic criteria for the illness. In the case of psychotic disorders, primary care includes interventions made prior to the onset of the FPE, either reducing the risk factors or focussing on interventions on people at high risk (these interventions would not be cost-effective in the general population due to the relatively low incidence of psychotic disorders).23–25 Since there are no clear and specific markers as yet to serve as secure indicators of the incipient presence of a psychotic disorder, primary prevention is made all the more difficult. On the other hand, secondary prevention is aimed at the early detection of the disease to prevent its progression or to reduce its severity. As mentioned earlier, there is a window period immediately following an FPE that in many cases determines the prognosis of the illness. The first years of the illness present an extraordinary opportunity to attempt to impede or limit the potential deterioration of the psychosis, via early psychosis intervention programmes (EPI), and increase the possibilities of better recovery. Finally, the aim of tertiary prevention is to reduce disability and prevent relapse, focussing on social rehabilitation and resocialisation. Psychiatry has traditionally placed its major emphasis on tertiary prevention.
To summarise the above points, primary prevention reduces risk factors and identifies the people in the general population with risk factors for the development of psychosis (e.g. a family history, perinatal factors, substance consumption, etc.), while early intervention after an FPE would be a form of secondary prevention. Although identifying attenuated symptoms might be considered a primary prevention measure, we should bear in mind that the symptoms in this prodromal phase easily overlap those of other disorders, such as depression, and if there is no progression to an FPE, most people already have a psychiatric diagnosis of some type. Therefore early detection of these clinical pictures to prevent their progression to an FPE should in most cases be considered secondary prevention.26 EIP is a healthcare model geared towards achieving a recovery from psychosis by early detection and the most effective treatment from the onset of psychotic symptoms. It involves the participation of multidisciplinary mental health teams who assess and treat people with an FPE, and then through the years that follow, until the person achieves a stable recovery. Early intervention services also take into account the negative symptoms of psychosis, such as emotional apathy, lack of motivation, language impoverishment, social withdrawal and self-neglect, and everybody with these symptoms should have ensured access to them. Following National Institute for Health and Care Excellence (NICE) guidelines, early treatment of these patients should include all interventions and evaluations summarised within a total of seven quality standards: psychological therapy, family interventions, education and employment support programmes, physical health assessments, wellbeing and education support.27 Furthermore, according to NICE, people suffering an FPE should be immediately referred to the early intervention services, in order for treatment to start within a period not exceeding 2 weeks.27
In sum, the main objectives of EIP are the early detection of the illness and the use of specific treatment for the FPE.28–30 The goal is thus to achieve recovery from symptoms and maximum functional recovery. Functional recovery involves appropriate psychosocial functioning, cognitive functioning and quality of life, although functional recovery has also been posited as freedom from psychotic symptoms, being able to undertake productive daily activities, live independently and maintain social relationships.31 EIP also aims to reduce the incidence of relapse and subsequent hospitalisation, suicide prevention, avoid stigmatisation and address social, educational and employment needs.
EIP programmes have already been implemented in other countries that demonstrate the efficacy and efficiency of early care, resulting in long-term cost saving.27,32–36 In fact, early detection and intervention are highly-developed strategies in the area of medicine that have led to major advances in reducing disease morbidity and mortality. In this opinion article we detail the arguments in favour of this type of intervention and argue that these care devices should be established in our country. Similarly, we propose a series of strategies and action plans to implement these EIP programmes in Spain, in the same way as in other European countries, America and Australia.
The need to create early intervention in psychosis programmes in SpainLongitudinal studies of patients who have had a first episode enable an examination of the factors associated with prognosis, monitoring response to therapeutic intervention and outcomes.37 The various studies that have been undertaken demonstrate that although prognosis is influenced by premorbid factors,38 early identification and appropriate treatment of the FPE lead to better long-term prognosis. A longer DUP results, for example, in a poorer response to treatment in various areas of clinical symptoms.13,14,39 Other consequences of delaying the treatment of patients in the initial stages of psychotic disorders include slower recovery, poorer prognosis, functional and cognitive impairment in attention and memory, worse general functioning, interrupted psychological and social development, interrupted studies or employment, substance abuse, loss of self-esteem and confidence.15–20,40 In addition, a relationship between DUI and DUP and morphological changes has been demonstrated on MRI imaging, specifically an inverse correlation between the duration of these periods and grey matter density.41–44 Just as delayed treatment has a negative effect on the outcomes of patients with psychosis, the advantages of appropriate45 and early anti-psychotic treatment in terms of disease prognosis have also been demonstrated.46 In addition, other longitudinal studies have established recovery predictors in follow-ups of up to 10 years, demonstrating that early identification of psychosis in young adults and starting treatment promptly, specifically geared at the negative symptoms, has long term benefits for these patients.47
Not only have factors associated with the duration of DUP and DUI been studied, but also the so-called delay in intensive psychosocial treatment (DIPT) has been taken into account, defined as the first contact with the psychiatrist in relation to the first episode and the time of admission for specialist consultation. Longer DUP and DIPT have been associated with poorer outcomes for negative symptoms.48 A longer DUP has been associated with a greater number of relapses, whereas a greater DIPT has been linked with longer hospital stays.48
Finally, but no less important, there are studies that demonstrate that EIP is cost-effective compared to standard treatment, resulting in savings in costs associated with the illness both short and long term.34–36,49,50 For example, McCrone et al.36 estimated a saving of £4814 per patient for children and adolescents treated over 6 months by the early care services, compared to standard treatment. The saving in costs was principally due to shorter hospital stays. Another long-term study calculated a saving of £2087 per person over 3 years, with better employment rates for patients who received EIP. In addition, the reduction in suicides in this group of patients resulted in an annual saving of £957.35 Thus EIP results in a saving for the healthcare system at least mid and long term. Although most studies come from the early care services provided in England, other early care programmes implemented in Australia have also proved highly cost-effective.51
Not only should treatment be offered early, but this should be inclusive, as indicated by the systematic review of healthcare technology evaluation undertaken by OSTEBA in collaboration with the Ministry of Health.52 According to the results of the OPUS programme, implemented in Denmark, inclusive multidisciplinary intervention (assertive treatment, psychoeducational and social skills) over the first 2 years following an FPE enables better symptomatic and functional recovery, and reduced family burden.53 Furthermore, after 5 years of inclusive treatment the patients presented greater autonomy and fewer hospitalisations.54
In addition to the existing studies that support early intervention, we should bear in mind that the physical health of these patients is compromised from the initial phases of the illness. Interventions that focus on physical health to avoid smoking, inactivity and obesity and that introduce healthy life habits can have a favourable effect on global health parameters, minimise the adverse effects of treatment and help to prevent subsequent common comorbidities in patients with psychotic disorders.55 A high proportion of the population with serious mental illness have comorbidities with physical health problems,56 and comorbidities between different mental illnesses are very common in chronic mental health patients (around 50%).
Based on the above, we deduce that the relationship between the duration of untreated psychosis and the clinical, social and financial consequences mean that there is a need to implement early intervention immediately after the onset of psychotic symptoms, and this can be achieved through EIP programmes.
There are currently international guidelines and agreements regarding early intervention in schizophrenia and other psychotic disorders. According to the International Early Psychosis Association (IEPA) and the World Health Organisation (WHO) in their Ministerial Conference (Helsinki, 2005), an early and preventive approach is recommended to target the populations at high risk of psychosis (ARMS) or those who have had an FPE.
Obstacles and situation of early intervention in psychosis in SpainDespite the aforementioned benefits, early care measures that are already in operation in other countries and that work are still not common in Spain. Our services are based above all (and devote more time) to the care of chronic disease and longstanding mental disorders. Prevention activity is low and the professionals most in contact with the population at risk of schizophrenia and other psychoses lack the tools and support to enable early detection. Before an FPE occurs it is common for there to have been signs of it in the context of primary care (PC), education, and/or the social services, but it is probable that these signs will not be appropriately evaluated and/or addressed. In this regard, apart from the odd exception,57 sufficient coordination and a link are lacking between mental health specialists, PC professionals and the social and education services in terms of generally established and implemented care strategies. In some of the autonomous regions there are incipient early detection programmes that are implemented unequally. Even so, even in the regions that are better developed with better ratios in mental health, many of the elements that should be included in EIP programmes are lacking.
Furthermore, the mental health treatment modalities offered take little account of the features of the initial phases of the disease and the context in which they occur, i.e., young people who are very reluctant to seek help, prejudiced against psychiatry, with high consumption of toxic substances, insufficient psychological care and information on how to receive help. The services do not meet the needs for appropriate outcomes and care. For example, the reorganisation of resources is not appropriate and there are long waiting lists and long times between visits. Furthermore, they only take health resources into account, and not psychosocial resources. There is also a tendency to minimise the seriousness of mental disorders in the adolescent population, about which there is major ignorance and stigma in the general population. EIP should address vocational and employment aspects.58 This does not occur in part because of the poor coordination between the healthcare services and the social services in the different autonomous regions. And neither is the necessary integral intervention offered, apart from rare exceptions, nor is continuity of care ensured: treatments are fragmented into services (care services, hospitalisation, substance abuse, psychosocial, etc.). Physical spaces should be adapted for young people, preventing them from becoming stigmatised, and should be integrated into a modern medical system that meets the needs of this population. Finally, the services do not contemplate the use of software-based tools for mobile phones or social network platforms which are nowadays essential access ports for this population.59
The primary objective of the acute admission units that frequently attend patients with FPE (occasionally under a section), is to rapidly reduce the most acute symptoms. On occasion it is not easy to rectify the traumatic event and this might involve admission to hospital, which increases the difficulty of the continuity of care needed, including therapeutic adherence. The most prompt transition possible or treatment from the start in specific programmes for psychosis adapted to the young population and their needs and preferences constitutes an added advantage in continuity of care and in reducing discontinuation of treatment.
Given the transfers of healthcare organisation, available conditions and resources vary greatly between the different autonomous regions and hospitals of our country, and even within the districts of the same city. This further impedes the implementation of EIP programmes. There is often also a lack of knowledge of the benefits of these programmes amongst mental health practitioners, possibly due in part to the lack of information on the results of the studies discussed in this article, showing that early intervention can significantly help patients with incipient psychosis. The unresolved problem is thus accentuated as to how much time patients should attend these first episode programmes. There needs to be excellent coordination between these programmes and mental health centres of the area at the time the patients are transferred. Added to all of this is the lack of political commitment and interest in preventive measures whose benefits are seen over periods of time that exceed terms of government, and there is no healthcare policy that takes decisions based on scientific evidence to enable knowledge from research to be used to improve the health of the population.
Stigma associated with mental illness remains very entrenched in Spain and can constitute another major barrier to people attending the mental health services promptly, and can trigger discriminatory situations in various areas of their daily lives which affect their social integration and quality of life.56,60
Proposal for early intervention programmes and basic strategies for their implementationThere can be no doubt that procedures that improve treatment and outcomes of the illness should be incorporated into healthcare systems. Therefore it is necessary to create programmes for the early detection and intervention of psychosis, reducing the untreated duration of the illness and offering inclusive and intensive multidisciplinary intervention programmes in the first years.
We believe that the necessary adaptations or incorporations to increase EIP and to reduce the wait time until receiving treatment (currently the time between the onset of symptoms and the first therapeutic contact can be in excess of 2 years for patients with schizophrenia)61 can result in a saving for our current healthcare system. Therefore, we should take as our reference aspects such as a specialist evaluation of the problem, establishing the appropriate therapeutic alliance, designing and starting to implement an integrated approach plan.
Against this background, we suggest a series of strategies and proposals directed at EIP to guarantee that EIP and evidence-based treatment can be made public and available to everyone up to the age of 60 who have suffered an FPE, regardless of the duration of untreated psychosis.
To meet this objective, we consider that a series of actions are required along the following lines, amongst which we highlight: (1) the creation of pressure groups and awareness-raising strategies, and (2) the participation of patients as well as their families in the early intervention services.
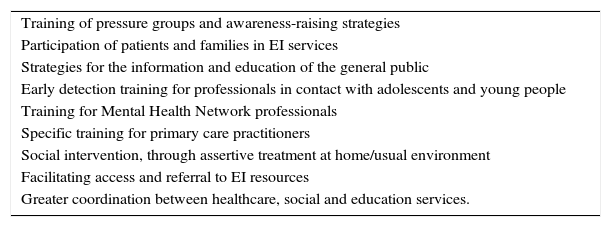
We also consider that other actions are important to improve and implement EIP programmes in our system (Table 1).
Actions and strategies for implementing early care services.
| Training of pressure groups and awareness-raising strategies |
| Participation of patients and families in EI services |
| Strategies for the information and education of the general public |
| Early detection training for professionals in contact with adolescents and young people |
| Training for Mental Health Network professionals |
| Specific training for primary care practitioners |
| Social intervention, through assertive treatment at home/usual environment |
| Facilitating access and referral to EI resources |
| Greater coordination between healthcare, social and education services. |
We must stress that all interventions should include individual, group, vocational and family approaches.
Current models of early psychosis intervention programmesIn European countries, America and Australia, EPI programmes are being implemented following the recommendations of international guidelines and organisations.32,49,62 The experience that these countries bring in launching these programmes can enable their implementation in other countries, like Spain, where EPI services are as yet not well established. Some of the most relevant, amongst many others, are: Early Intervention in Psychosis (TIPS) in Norway and Denmark,63–66 Initiative to Reduce the Impact of Schizophrenia (IRIS) in Great Britain, and Early Psychosis Prevention and Intervention Centre (EPPIC) in Australia.67 All make interventions at both a social and clinical level. The interventions aim to reduce the stigma associated with psychotic disorders and to educate the population about the correct use of services. Educational programmes are also included and training of groups that are in direct contact with the at-risk population who might detect and refer, such as PC doctors, teachers and other professionals. Once a case is detected, EPI programmes offer appropriate care at a clinical level.
Some of the most relevant common components of EPI programmes are outlined below:
- -
Education of the general public about the signs that might precede psychosis and specific training for teachers and general practitioners.
- -
Clinical teams dedicated principally to the early detection of people with untreated FPE. The treatment teams are interdisciplinary, comprising psychiatrists, psychologists, nurses, social workers and occupational therapists. The EPPIC and OPUS programmes also include a specialist in their teams to implement the early intervention model (Individual Placement and support Specialist [IPS]).
- -
Integrated treatment, with the participation of the entire therapeutic team, with periodic meetings to discuss the treatment plan.
- -
The practitioner: patient ratio is 10:15 case:practitioner.
- -
Family intervention, with psychoeducational workshops, individual family therapy and family support groups. The family is also included in discussions regarding treatment.
- -
Domiciliary care, considering the structure and functioning of the family environment, and patient's symptomatic and psychosocial severity level.
- -
Unrestrictive view of the concept of FPE, which is occasionally erroneously considered a symptom of schizophrenia, when in reality it could be applied to all disorders and illnesses that start with a psychotic episode.68
- -
Attitude and training of practitioners to relate with patients in situations of incipient psychosis. On the one hand not focussing on a diagnosis (at a time of great clinical variability) but on the symptoms and their functional repercussions. And on the other, having the ability to adapt care to needs (type of support, timetables, care spaces, etc.).
Finally, we should highlight the importance of not-for-profit associations, driven by patients and families, such as the European Federation of Associations of Families of People with Mental Illness (EUFAMI). These bodies are a tool for welcoming, supporting and representing people with mental disorders and their families, and for training volunteers and raising awareness about mental health. One of their founding members the Confederación Salud Mental España, (Spanish Mental Health Confederation) was launched in 1983 and currently includes 19 regional federations and uniprovincial associations, bringing together around 300 associations with more than 44,000 members nationwide. Without doubt, these associations should play a major role on a daily basis in healthcare in this country: they also encourage healthcare practitioners to inform patients and their families about them once an FPE has occurred.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsDr. Arango was a consultant, and has received fees or grants from Abbot, AMGEN, AstraZeneca, Bristol-Myers Squibb, Caja Navarra, CIBERSAM, Fundación Alicia Koplowitz, Forum, Instituto de Salud CarlosIII, Janssen Cilag, Lundbeck, Merck, Ministerio de Ciencia e Innovación, Ministerio de Sanidad, Ministerio de Economía y Competitividad, Mutua Madrileña, Otsuka, Pfizer, Roche, Servier, Shire, Schering Plough and Takeda.
Dr. Bernardo was a consultant and has received research grants and/or has participated as a speaker and/or advisor for AB-Biotics, Adamed, Boehringer, Eli Lilly, Ferrer, Forum Pharmaceuticals, Janssen-Cilag, Lundbeck, Otsuka, Pfizer, Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación, Ministerio de Educación, Cultura y Deporte, Ministerio de Economía y Competitividad, CIBERSAM, Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement (2014SGR441), Foundation European Group for Research In Schizophrenia (EGRIS) and 7th Framework Programme of the European Union.
Mrs. Ana Cabrera has received fees or grants from Janssen Cilag, the Otsuka-Lundbeck Alliance and CIBERSAM.
Prof. Benedicto Crespo-Facorro has received fees for consultancy or advice services and lecture fees from Janssen Johnson & Johnson, Lundbeck and Otsuka Pharmaceuticals. He has received research funds from the Instituto de Salud Carlos III, MINECO, The Government of Cantabria, Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM) (Spanish network of Biomedical Research Centres in Mental Health), from the 7th Framework Programme of the European Union and Lundbeck.
Dr. Vieta has received funding for research projects and/or fees as a consultant or speaker from the following companies and institutions: AB-Biotics, Allergan, AstraZeneca, Bristol-Myers Squibb, Dainippon Sumitomo, Elan, Eli Lilly, Ferrer, Forest Research Institute, Gedeon Richter, Glaxo-Smith-Kline, Janssen, Lundbeck, Otsuka, Pfizer, Roche, Sanofi-Aventis, Servier, Shire, Solvay, Sunovion, Takeda, Instituto de Salud CarlosIII, the Seventh Framework Programme (ENBREC), the Brain and Behaviour Foundation (NARSAD) and the Stanley Medical Research Institute.
Please cite this article as: Arango C, Bernardo M, Bonet P, Cabrera A, Crespo-Facorro B, Cuesta MJ, et al. Cuando la asistencia no sigue a la evidencia: el caso de la falta de programas de intervención temprana en psicosis en España. Rev Psiquiatr Salud Ment (Barc.). 2017;10:78–86