Kutikov and Uzzo described the R.E.N.A.L. nephrometry score in 2009. It allows the anatomic evaluation of renal tumors in order to compare the technical difficulty during partial nephrectomy according to several characteristics: size, depth of the mass in the renal parenchyma, proximity to the renal collecting system, localization (anterior or posterior and polar). The score is also useful, among others, to predict technical difficulty, define the risk of post-operative complications, define the type of ischemia and standardize dada compilation.
Materials and methodsWe retrospectively reviewed 20 triphasic computed tomography studies from 20 patients that were taken to partial nephrectomy in the Pablo Tobon Uribe Hospital in Medellin between December of 2009 and March of 2014. One urologic oncologist, one radiologist and one urology resident (first year resident) used the nephrometry score to classify the patients. The inter-observer concordance was defined for each of the components by kappa coefficient.
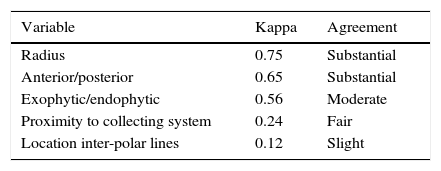
ResultsConcordance for each score component was analyzed separately. The concordance for tumor diameter component was accurate, 0.75 (confidence interval [CI] 95% 0.34–0.98); for the exofitic/endofitic component was adequate 0.56 (CI 95% 0.30–0.81); for proximity to the collecting system was discordant 0.24 (CI 95% −0.08 to 0.56); for anterior/posterior was concordant 0.65 (CI 95% 0.40–0.89) and for location in relation to the interpolar lines was discordant 0.12 (CI 95% −0.14 to 0.38).
ConclusionsWe found in this cohort that the R.E.N.A.L. nephrometry score has a good inter-observer concordance for tumor diameter and anterior/posterior components while it was discordant and acceptable for the proximity to the collecting system and relation to the inter-polar lines respectively. The R.E.N.A.L. nephrometry score is a useful tool to establish the best surgical approach, technical difficulty and type of ischemia during partial nephrectomy.
La escala R.E.N.A.L., que permite evaluar la anatomía de tumores renales, fue propuesta por Kutikov y Uzzo en 2009. Se compone de: R (diámetro tumoral), E (exofítico/endofítico), N (proximidad al sistema colector), A (anterior/posterior) y L (localización en relación con las líneas interpolares). La utilización de sistemas de nefrometría ha servido entre otras cosas para: predicción de la dificultad técnica, riesgo de complicaciones postoperatorias, definir el tiempo de isquemia y estandarizar la forma de reportar los datos.
Materiales y métodosRetrospectivamente se analizaron 20 tomografías de 20 pacientes sometidos a nefrectomía parcial en el Hospital Pablo Tobón Uribe de la ciudad de Medellín, intervenidos entre diciembre de 2009 y marzo de 2014. Un urólogo oncólogo, una radióloga y un residente de urología de primer año clasificaron las masas renales usando el sistema de nefrometría R.E.N.A.L. score. La concordancia interobservador se determinó por separado para cada uno de los componentes del score mediante el estadístico kappa.
ResultadosPara el diámetro tumoral, la concordancia interobservador fue buena: 0,75 (intervalo de confianza [IC] 95%: 0,34-0,98); para el componente exofítico/endofítico fue aceptable: 0,56 (IC95%: 0,30-0,81); para el componente proximidad al sistema colector fue reducida: 0,24 (IC95%: −0,08-0,56); para el componente anterior/posterior fue buena: 0,65 (IC95%: 0,40-0,89), y para el componente de localización con las líneas interpolares fue pobre: 0,12 (IC95%: 0,14-0,38).
ConclusionesEl sistema de puntaje de nefrometría R.E.N.A.L. tiene una buena confiabilidad interobservador para los componentes diámetro del tumor y localización (anterior/posterior), pero una pobre/aceptable confiabilidad interobservador para los componentes proximidad al sistema colector y la localización en relación con las líneas interpolares. Es una herramienta útil para masas renales, define la dificultad técnica y determina el mejor abordaje y el tipo de isquemia en la cirugía.
Nephron sparing surgery is an alternative treatment in patients with small renal masses. Nephrometry systems help to objectively determine the complexity of renal masses in order to define the approach, to predict the time of ischemia and the prognosis of nephron sparing nephrectomy, among other things. The best known systems are: the C-index, PADUA (preoperative aspects and dimensions used for an anatomical) classification, and R.E.N.A.L. nephrometry scale.
The rising incidence of renal masses is partly explained by the increased use of diagnostic imaging to study different symptoms. We should not ignore, however, that the number of renal tumors is also increasing worldwide for reasons still unknown.
Assessing the anatomical characteristics of renal tumors is critical in the preoperative planning of nephron sparing nephrectomy. Tumor characteristics determining the effectiveness and technical difficulty of partial nephrectomy include: size, multifocality, depth, nearness to the collecting system, and renal vascular anatomy. In addition, tumor location (anterior, posterior, polar location) is also important. Some of the previously mentioned characteristics form part of the R.E.N.A.L. nephrometry score, and they are assessed prior to surgery, allowing to determine the complexity of partial nephrectomy by imaging studies, such as triphasic abdominal computed tomography or magnetic resonance imaging of abdomen and pelvis with coronal reconstruction.1
The scoring system for the R.E.N.A.L. nephrometry score was recently proposed by Kutikov and Uzzo,2 with the objective of characterizing renal tumor masses according to the aforementioned characteristics. The study aimed to assess interobserver variability for each of the 5 components of the nephrometry table and for the total score summing up each of the components. It is the most commonly used scale in the US.
In the urologic literature this tool has shown consistent correlation with surgical prognosis and complications. The R.E.N.A.L. nephrometry scale aims to provide quantitative information on renal masses. The total score allows to determine the complexity of partial nephrectomy. Lesions in which the total score of the components is 4–6 are considered renal masses of low complexity; lesions totaling 7–9 are renal masses of moderate complexity; and those totaling 10–12 are considered highly complex lesions. Risk stratification is classified into 3 zones (zones 1, 2, and 3), each corresponding to a score value of 1, 2, and 3, respectively. Tumors are stratified into three levels of complexity. Low-risk renal tumors total 4–6; those of intermediate risk, 7–9; and high-risk tumors total 10–12.3
Materials and methodsIn a medical center in the city of Medellín, the study reviewed triphasic CT scans that were randomly obtained from 20 patients undergoing partial nephrectomy between December 2009 and March 2014. To perform a proper analysis, only patients with available images of axial and coronal sections were taken into account.
A urologic oncologist, a radiologist, and a first-year urology resident reviewed the images and independently assigned the R.E.N.A.L. score to each case, without knowing the total score. The system contains five components: R (radius), E (exophytic/endophytic), N (nearness to collecting system), A (anterior/posterior), and L (location relative to inter-polar lines).
For statistical analysis and to interpret different variables among raters kappa coefficient was used. The kappa range is interpreted as follows: 0–1 (from none to perfect agreement); values <0.20 as indicating slight agreement; 0.21–0.40 as fair agreement; 0.41–0.60 as moderate agreement; 0.61–0.80 as substantial agreement; and 0.81–1 as an almost perfect agreement. The agreement was separately determined for each one of the components of the nephrometry scale.
This study is based on a fixed sample of 20 subjects; nevertheless, 22 is the number of subjects required to detect a statistically significant kappa (0.5), lower than 5%, for a dichotomous variable with 2 raters, with a power of 80%, assuming positive results in 70% and a two-tailed test, according to calculations based on the goodness-of-fit formula developed by Donner and Eliasziw, and summarized in a table by Sim and Wrigth. Similarly, in some situations, it is more practical to increase the number of raters than the number of subjects; and when kappa values greater than 0.4 are expected to be obtained in a dichotomous variable, there is no advantage in using more than three raters by subject.4
ResultsThe interobserver concordance for the radius component (k=0.75; confidence interval [CI], 95% 0.34–0.98) and the anterior/posterior component (k=0.65, CI 95% 0.40–0.89) was substantial; for the exophytic/endophytic component, it was moderate (k=0.56, CI 95% 0.30–0.81); for nearness to collecting system, it was fair (k=0.24, CI 95% 0.08–0.56); and for location in relation to inter-polar lines, it was slight (k=0.12, CI 95% 0.14–0.38). Detection of tumors in contact with the collecting system and renal vasculature had a fair agreement (k=0.25).
Regarding the total score, interobserver concordance for R.E.N.A.L. nephrometry score totaling 4 was slight, because there was variability among the three raters. There was no agreement among the raters when nephrometry scores totaling 5–9 were used (kappa values in these cases were less than 0.20, which is considered a slight agreement). When the three raters qualified renal masses with nephrometry scores totaling 10 and 11, there were fair and moderate agreements, respectively.
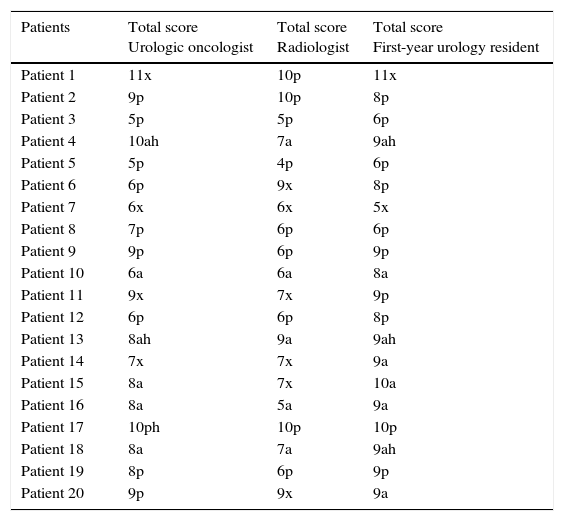
Table 1 shows each of the variables applied by each of the observers (urologic oncologist, radiologist, and urology resident) with their individual component scores and total scores using R.E.N.A.L. nephrometry. Table 2 explains each one of the scale's components with their kappa values and respective agreement.
Variables applied in R.E.N.A.L. nephrometry.
| Patients | Total score Urologic oncologist | Total score Radiologist | Total score First-year urology resident |
|---|---|---|---|
| Patient 1 | 11x | 10p | 11x |
| Patient 2 | 9p | 10p | 8p |
| Patient 3 | 5p | 5p | 6p |
| Patient 4 | 10ah | 7a | 9ah |
| Patient 5 | 5p | 4p | 6p |
| Patient 6 | 6p | 9x | 8p |
| Patient 7 | 6x | 6x | 5x |
| Patient 8 | 7p | 6p | 6p |
| Patient 9 | 9p | 6p | 9p |
| Patient 10 | 6a | 6a | 8a |
| Patient 11 | 9x | 7x | 9p |
| Patient 12 | 6p | 6p | 8p |
| Patient 13 | 8ah | 9a | 9ah |
| Patient 14 | 7x | 7x | 9a |
| Patient 15 | 8a | 7x | 10a |
| Patient 16 | 8a | 5a | 9a |
| Patient 17 | 10ph | 10p | 10p |
| Patient 18 | 8a | 7a | 9ah |
| Patient 19 | 8p | 6p | 9p |
| Patient 20 | 9p | 9x | 9a |
Renal cell carcinoma constitutes approximately 85% of neoplasms of renal origin, with a prevalence between 4.4 and 11/100,000 inhabitants per year. Recent epidemiological data show an increase in the frequency of renal neoplastic disease between 2.3 and 4.3% annual, between 1975 and 1995. Early detection is partly explained by technological advances and an increased realization of non-invasive imaging studies; in many cases, even as an incidental detection.5
In the last two decades, nephron sparing nephrectomy has emerged as an alternative to radical nephrectomy in a significant percentage of localized renal tumors. This procedure has considerably increased for renal masses smaller than 4cm and for selected masses smaller than 7cm.2,6 The benefits of partial nephrectomy include an oncological result in appropriately selected cases and with conservation of renal function. Its use in the past was limited to patients with an anatomical or functional solitary kidney, bilateral renal involvement, and genetic predisposition to renal neoplasm and renal failure in the future; but it has been lately extended to patients with functioning kidneys.
The R.E.N.A.L. score does not predict decrease in glomerular filtration attributable to nephron sparing nephrectomy in patients with solitary kidneys. This scale is safe and effective when applied to this kind of patients and it helps to define the technical difficulty of the surgery, and to predict entrapment time resulting in using the most adequate type of ischemia.7,8
Scales like nephrometry do not only help to determine an appropriate surgical planning, but they are also useful to compare series of partial nephrectomy, given that they provide a standard nomenclature, making, thus, comparisons less subjective. Similarly, it constitutes a common language among different specialties that treat kidney tumors.2,6
Standardized reports of tumor size, location and depth are important characteristics for correct preoperative decision making, allowing to relate the anatomy of a renal mass, the disease, and cancer prognosis.9
The components of the R.E.N.A.L. score have important clinical implications. Tumor size was considered as an indicator for surgical and oncologic prognosis. A study showed that this component of the measurement scale was a risk factor for urinary fistula formation and postoperative renal failure after partial nephrectomy; this has been confirmed by similar studies.10,11
The exophytic component describes the relationship of the mass to the renal surface. This characteristic is thought to impact the complexity of the surgery and associated complications. Some researchers have classified the injuries as exophytic, endophytic, and mesophytic or meso-renal.12 The nearness component (N) describes the distance between the deepest part of the renal mass and the nearest portion of the renal sinus fat or the collecting system; it is known and well described that the depth, and therefore the nearness of the renal mass, is an important variable that affects nephron sparing nephrectomy and related postsurgical complications, including the possibility of fistulas.13 The anterior/posterior/undetermined component considers less problematic the anterior or posterior location for open surgery compared to a complicated laparoscopic partial nephrectomy, as the posterior localization requires extensive mobilization, renal rotation, or a retroperitoneal approach.14 The last component of the measuring scale corresponds to the location of the renal mass in the sagittal plane and coronal plane. Recently, the name of inter-polar lines was proposed for proper localization of these renal masses. It is defined as the most medial portion of the renal parenchyma which is interrupted by the renal sinus fat, the renal hilum, or the collecting system.2 As part of the nomenclature, if renal masses have an intimate contact with the renal hilum, the letter “h” is used to classify them, specifically when the mass touches the artery or main vein.
Radiologists are familiar with the response evaluation criteria in solid tumors (RECIST) for the classification of renal masses, but they know less about the nephrometry scale. Due to the increased use of R.E.N.A.L. nephrometry and nephron sparing nephrectomy, it is important that this group of specialists start to use this system, as it is a simple measurement and once described according to its components it serves for proper surgical planning.15
New methods were recently created for a systematic and quantitative classification of renal tumors, such as the PADUA scale and the C-index system. The R.E.N.A.L. measurement scale and PADUA are similar regarding the description of tumor location, while the C-index system contributes to the description of tumor nearness to the central part of the kidney.2 Another new classification model was recently published and it is known as Zonal NePhRO Scoring System. Its components are: nearness (Ne) to the collecting system (not classified in centimeters but using the architecture of renal parenchyma [renal cortex, renal medulla, collecting system/renal sinus]). The second component is the physical location (Ph) of the kidney tumor in relation to renal architecture. The third component is based on the maximum radius (R) of the renal tumor. The fourth and final component is the organization (O) of the renal mass according to renal parenchymal areas.16 The best renal scale would be the one which includes in its components variables from the previously mentioned measuring scales, since it would provide sufficient information to predict surgical time, ischemia time, and intra- and postoperative complications.2
ConclusionThe R.E.N.A.L. nephrometry scoring system allows to program in advance nephron sparing nephrectomy, and to determine its complexity depending on the size of the mass. It has a substantial interobserver reliability for radius and location (anterior/posterior) components, but fair/moderate interobserver reliability for nearness to the collecting system and location in relation to inter-polar lines. When agreement for the renal nephrometry total score was evaluated, this study observed that the higher the score, the better the concordance (considering that it is a regular and acceptable concordance based on the results of this study). When tumor masses are classified with nephrometry total scores close to 4 (masses of low complexity), interobserver agreement is slight. When the total score is 10 or 11, agreement was fair and moderate, respectively.
This measuring scale does not predict decrease in glomerular filtration attributable to nephron sparing nephrectomy in patients with solitary kidneys, although it is safe and effective when applied to these patients. Several studies have generated criticism of some of the score's components, and others have tried to improve variability. It should be noted, however, that it is a useful and easy-to-use tool when faced with a renal mass. It helps to define technical difficulty, and to determine the best approach and the type of ischemia to be used in surgery. For this reason, it is important that the different specialties involved in the management of renal masses get familiar with this measurement scale.
Ethical disclosuresProtection of people and animalsThe authors declare that there were no experiments performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors declare no conflict of interest.