The flu represents a major public health issue. The flu vaccination rate among healthcare professionals has traditionally been lower than recommended by national health authorities, and there is also regional heterogeneity. The objective of the Gripetool project was to identify the most effective initiatives to promote influenza vaccination in Spain among healthcare workers.
Material and methodsInformation was obtained through an online survey conducted among members of the Spanish Society of Primary Care Physicians (SEMERGEN) between July and November 2020, which had been previously validated by a committee of experts. A multiple linear regression analysis was performed to analyse the possible relationship between the vaccination coverage of health professionals and the different promotion measures reported in the survey.
ResultsAccording to respondents (n = 385), the publication of vaccination recommendations (18.6%), the use of media and social networks (14.4%), and the active recruitment through email/letters (10.6%) are the most effective measures to increase vaccination rates. According to the statistical analysis, there are 10 measures that have a positive impact on the vaccination rate, the most relevant include the distribution of posters in health centres (17 percentage points increase, pp), the publication of vaccination recommendations (14 pp), and the development of protocols and guidelines (13 pp).
ConclusionsThe most effective strategies to increase influenza vaccination comprehend actions at macro-, meso-, and micro levels to promote vaccination and communicate its benefits, exploiting the potential of new technologies.
La gripe representa un importante problema de salud pública. La cobertura de vacunación antigripal entre profesionales sanitarios ha sido tradicionalmente inferior a la recomendada por las autoridades sanitarias nacionales, con heterogeneidad regional. El proyecto Gripetool pretende identificar las iniciativas más efectivas para fomentar la vacunación antigripal en España en este colectivo.
Material y métodosSe recabó información a través de una encuesta online realizada a los socios de la Sociedad Española de Médicos de Atención Primaria (SEMERGEN) entre julio y noviembre de 2020, previamente validada por un comité de expertos. Se realizó un análisis de regresión lineal múltiple para analizar la posible relación entre la vacunación en gripe de los profesionales sanitarios y las distintas medidas de fomento reportadas en la encuesta.
ResultadosSegún los encuestados (n = 385), la publicación de recomendaciones de vacunación (18,6%), el uso de medios de comunicación y redes sociales (14,4%) y la captación activa a través de email /cartas (10,6%) son las medidas más eficaces para aumentar la cobertura vacunal. Según el análisis estadístico, son diez las medidas con impacto positivo en la tasa vacunal, siendo las más relevantes la distribución de carteles en los centros sanitarios (aumento de 17 puntos porcentuales, pp), la publicación de recomendaciones de vacunación (14 pp) y la elaboración de protocolos y guías (13 pp).
ConclusionesLas medidas más efectivas para aumentar la vacunación antigripal en profesionales sanitarios pasarían por acciones a nivel macro, meso y micro para promover la vacunación y comunicar sus beneficios, explotando el potencial de las nuevas tecnologías.
Seasonal flu is a major public health problem that affects from 5% to 20% of the population every year.1 Although this disease is usually mild, in some cases it may lead to complications that require hospitalisation or even cause death. Worldwide, it is calculated that flu causes from 3 to 5 million severe cases per year, and from 290 000 to 650 000 deaths.2 Only in Spain it may cause up to 15 000 deaths per year.3 In socio-economic terms, the costs associated with flu may exceed 1200 million euros per year in our country.4
Vaccination is the most effective way to prevent seasonal flu and its consequences,5 so that every year different campaigns are used to encourage this. The World Health Organisation recommends annual vaccination in high risk populations, including those over the age of 65 years, pregnant women, children under the age of 5 years, chronic patients, and medical personnel.6
It is important to vaccinate medical personnel for several reasons; on the one hand, it is a measure of self-protection, given that medical staff are highly exposed to infectious agents and therefore are at higher risk of transmission than the general population. On the other hand, this also has an ethical basis, to prevent them from becoming a preventable risk of infection for their colleagues and patients. Finally, being vaccinated is also a sign of professionalism and shows how important it is. Raising the awareness of medical personnel about the advantages of vaccination leads to greater impact when recommendations about it are communicated to the population.7 Together with all of the above considerations, it is also important to keep maintain the level of the workforce in the healthcare system during flu epidemics or outbreaks.8 It is well-known that with vaccination against flu, the number of days off work among vaccinated personnel may be 28%–40% fewer than they are among those who had not been vaccinated.9
In 2020, the Covid-19 pandemic has substantially changed the situation with the disease of flu. There is now higher awareness of its severity and an unprecedented increase has occurred in the uptake of flu vaccination (from 39% to 74% among professionals10) with lower circulation of flu viruses.11 In spite of these advances, flu vaccination among personnel is still lower than is recommended, as the new target of the Ministry is to reach 75%,12 and there are notable differences between the Autonomous Communities in this respect.13.
The aim of the Gripetool project was to identify the most effective initiatives to increase the vaccination rate against flue among medical personnel in Spain, and to estimate the effect of each measure on the said rate.
Material and methodsDesignAn observational cross-sectional study was performed based on the data gathered in an online survey without sampling of all of the members of the Spanish Society of Primary Care Doctors (SEMERGEN) from July to October 2020. As it was anonymous, no informed consent was required. The draft questionnaire had previously been outlined and validated in a pilot study with 8 experts who were primary care doctors (the Gripetool Group of Experts), who discussed its length, difficulty, comprehensibility, interpretability, and structure. The specific questionnaire used figure in the supplementary material of this paper, and it is divided into 3 blocks.
InformationThe survey contained questions on sex, age group, and Autonomous Community where the interviewee worked, as well as whether they had been vaccinated this year and if they had received flu training. Information was also recorded on 15 potential strategies to increase the proportion of vaccinated medical personnel, grouped into 3 areas: “Documentation or institutional recommendations”; “Campaign publicity activities”; and “Activities to encourage the involvement of professionals in vaccination”. Questions were also asked on the validity of measures to encourage vaccination, interviewees' opinions of the types of initiatives being used in their place of work or health region to increase vaccination coverage among medical personnel, and the level of excellence and impact attained (with a maximum possible score of 10 points). A question was also asked about the level of vaccination among the medical professionals in their place of work.
Statistical analysisAfter the descriptive analysis of the survey results, a multiple lineal regression analysis was performed to determine the possible relationship between vaccination coverage in medical personnel and the different measures contained in the survey. The dependent variable in the models was the rate of vaccination coverage among medical personnel in the interviewee's place of work during the 2019–2020 flu campaign, with values from 2.5 to 97.5 (class mark for the 20 intervals of vaccination coverage from 0% to 100% set in the survey). Each one of the different measures used to encourage vaccination were the independent variables included in the regressions (one in each regression). Moreover, the control variables included were the sex and age group of the interviewee and whether or not they had been vaccinated against flu in this or the previous campaign. A statistical significance of 90% was considered. The models were created using the Stata 14.0 program.
Results385 individuals responded to the survey, of whom 40.5% were men and 59.5% were women. 37% of the interviewees were professionals aged ≥60 years, and 12.7% were professionals aged from 40 to 49 years (Table 1).
Basal characteristics of the respondents.
| Variable | Category | Total replies (n = 385) | Vaccinated (n = 319) | Not vaccinated (n = 66) | |||
|---|---|---|---|---|---|---|---|
| % | Sample size | %⁎ | Sample size | %⁎ | Sample size | ||
| Sex | Men | 40.52% | 156 | 82.05% | 128 | 17.95% | 28 |
| Women | 59.48% | 229 | 83.41% | 191 | 16.59% | 38 | |
| Total | 100% | 385 | 82.86% | 319 | 17.14% | 66 | |
| Age group | <40 years | 29.35% | 113 | 82.30% | 93 | 17.70% | 20 |
| 40–49 years | 12.73% | 49 | 87.76% | 43 | 12.24% | 6 | |
| 50–59 years | 20.78% | 80 | 81.25% | 65 | 18.75% | 15 | |
| 60 years or more | 37.14% | 143 | 82.52% | 118 | 17.48% | 25 | |
| Total | 100% | 385 | 82.86% | 319 | 17.14% | 66 | |
Of the Autonomous Communities, Andalusia had the highest proportion of interviewees (12.5%), followed by the Canary Islands (11.7%). The Autonomous Communities with the fewest replies were the Balearic Islands (0.52%) and La Rioja (0.78%). Based on the proportion of medical professionals in 2020, the most over-represented regions in the survey (with the greatest relative difference between the sample proportion and the proportion of medical professionals in comparison with the national total) would be the Canary Islands (11.7 vs. 4.5%) and Extremadura (5.5 vs. 2.2%). The most under-represented would be Madrid (11.2 vs. 21.1%) and Catalonia (5.7 vs. 9.6%) (Table 2).
Distribution according to Autonomous Community of the number of interviewees versus the actual population of medical professionals and the proportion vaccinated against flu reported in the survey versus the official Ministry of Health figure for the 2019–2020 campaign.
| Autonomous Communities (AC) | Distribution | Vaccination coverage of professionals | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total replies to survey (n = 385) | Complete replies to survey (n = 160) | Population of medical professionals | Ministry | Survey | Diff. (p) | Sample size | |||
| % | Sample size | % | Sample size | % | |||||
| Andalusia | 12.47% | 48 | 10.00% | 16 | 15.20% | 36.10% | 47.20% | 11.1 | 16 |
| Aragón | 4.42% | 17 | 3.75% | 6 | 4.40% | 20.80% | 50.70% | 29.9 | 6 |
| Asturias | 5.45% | 21 | 4.38% | 7 | 2.60% | 50.5%a | 58.20% | 7.7 | 7 |
| Balearic Islands | 0.52% | 2 | 0.63% | 1 | 0.70% | 24.30% | 62.50% | 38.2 | 1 |
| Canary Islands | 11.69% | 45 | 13.13% | 21 | 4.50% | 27.5%a | 53.70% | 26.2 | 21 |
| Cantabria | 3.90% | 15 | 2.50% | 4 | 1.50% | 41.00% | 40.00% | − 1 | 4 |
| Castile y León | 9.09% | 35 | 8.13% | 13 | 6.20% | 37.90% | 44.40% | 6.5 | 13 |
| Castile-La Mancha | 5.19% | 20 | 5.00% | 8 | 5.70% | 43.50% | 52.50% | 9 | 8 |
| Catalonia | 5.71% | 22 | 5.00% | 8 | 9.60% | 30.20% | 48.80% | 18.6 | 8 |
| C. Valenciana | 11.17% | 43 | 14.38% | 23 | 11.30% | 65.50% | 52.30% | − 13.2 | 23 |
| Extremadura | 5.45% | 21 | 7.50% | 12 | 2.30% | 40.40% | 47.50% | 7.1 | 12 |
| Galicia | 5.45% | 21 | 6.25% | 10 | 3.70% | 50.90% | 43.00% | − 7.9 | 10 |
| La Rioja | 0.78% | 3 | 0.63% | 1 | 0.80% | 29.80% | 47.50% | 17.7 | 1 |
| Madrid | 11.17% | 43 | 13.13% | 21 | 21.10% | 36.60% | 60.80% | 24.2 | 21 |
| Murcia | 2.34% | 9 | 1.25% | 2 | 3.40% | 31.00% | 47.50% | 16.5 | 2 |
| Navarre | 1.30% | 5 | 1.25% | 2 | 2.00% | 28.50% | 42.50% | 14 | 2 |
| Basque Country | 2.86% | 11 | 2.50% | 4 | 4.70% | 37.40% | 45.00% | 7.6 | 4 |
| Ceuta / Melilla | 1.04% | 4 | 0.63% | 1 | 0.30% | 37.2%b | 32.50% | −4.7 | 1 |
| Total | 100% | 385 | 100% | 160 | 100% | 39.40% | 50.80% | 11.4 | 160 |
Source: prepared by the authors based on the survey and Ministry of Health data (2021).
82.9% of the respondents had been vaccinated in 1 of the 3 most recent flu vaccination campaigns. The proportion of vaccinated individuals was higher in the subgroup aged 40–49 years (87.76%) than it was in the other age groups (in which it was under 83%) (P > .05) (Table 1). 88.1% of the respondents had been vaccinated to protect other people, while 77.4% had done so to protect themselves and 33.5% had done so to give an example to their patients and those around them. On the other hand, the reasons given by the 66 unvaccinated doctors included the adverse effects of the vaccine (33%), the belief that they were at low risk of infection (26%), and the lack of efficacy of the vaccine (14%). They also gave other reasons, such as lack of availability or a fear of needles (29%).
Respecting vaccination coverage in professionals for the 2019–2020 campaign, 18.8% of the respondents reported a vaccination rate higher than 75%. 34.4% reported a rate between 50% and 75%; 31.3% reported a coverage of from 25% to 50%, and only 15.6% reported a rate lower than 25%. The AC with the highest vaccination rates among professionals were the Balearic Islands (62.5%; n = 1) and the Community of Madrid (60.8%; n = 21), while the respondents who reported lower vaccination rates were Ceuta/Melilla (32.5%; n = 1) and Cantabria (40%; n = 4) (Table 2).
Descriptive analysis of the proposed measuresThe most frequently used measures to increase and/or maintain vaccination rates in medical professionals (Table 3) were the distribution of posters in medical centres (in 89.8% of centres) and the preparation and publication of protocols and technical guides (84.9%). On the contrary, the least used were incentives for professionals such as payment for variable productivity or attending congresses (which was only applied in 11.3% of centres) and invitations to professionals to take part in the design and implementation of new strategies to increase coverage (20.1%).
Levels of use of the measures to increase vaccination coverage among medical personnel in the 2019–2020 campaign.
| Area | Measure | Not applied | Applied | No. of replies obtained | |||
|---|---|---|---|---|---|---|---|
| New | 1–4 years | ≥5 years | Total | ||||
| Documentation or institutional recommendations | Publication of recommendations to vaccinate | 16.0% | 2.7% | 17.6% | 63.8% | 84.0% | 188 |
| Preparation and publication of protocols and technical guides | 15.1% | 2.5% | 18.2% | 64.2% | 84.9% | 159 | |
| Inclusion of new strategies in the services portfolio | 28.1% | 5.8% | 20.1% | 46.0% | 71.9% | 139 | |
| Campaign publicity | Distribution of posters in medical centres | 10.2% | 1.0% | 14.6% | 74.1% | 89.8% | 205 |
| Audio and/or video publications | 47.1% | 3.2% | 17.8% | 31.8% | 52.9% | 157 | |
| Activity in the media and/or social networks | 17.6% | 4.3% | 21.4% | 56.7% | 82.4% | 187 | |
| Specific web page or section on flu and/or vaccination | 15.1% | 3.0% | 22.9% | 59.0% | 84.9% | 166 | |
| Sending emails and/or personalised letters | 62.7% | 2.7% | 12.0% | 22.7% | 37.3% | 150 | |
| Activities to encourage the involvement of professionals in vaccination | Incentives | 88.7% | 0.5% | 2.1% | 8.7% | 11.3% | 195 |
| Informing professionals of new strategies | 55.3% | 4.1% | 17.1% | 23.5% | 44.7% | 170 | |
| Participating in the design and implementation of new strategies | 79.9% | 2.4% | 7.3% | 10.4% | 20.1% | 164 | |
| Training and updating about flu and vaccination against it | 59.7% | 3.2% | 15.1% | 22.0% | 40.3% | 186 | |
| Computerised reminder of coverage registry | 42.9% | 3.6% | 13.7% | 39.9% | 57.1% | 168 | |
| Report on specific data in their workplace | 49.1% | 2.5% | 16.0% | 32.5% | 50.9% | 163 | |
| Meetings to raise awareness of the need for vaccination | 62.1% | 2.7% | 8.8% | 26.4% | 38.1% | 181 | |
Taking into account the time during which the 15 measures included in the survey were applied, the most common actions are also the ones which were applied for the longest periods of time. Posters had been distributed for ≥5 years in 74.1% of the centres, and protocols and guides were prepared in 64.2% of the centres (Table 3). In turn, the new measures implemented the most widely in the last campaign were the inclusion of new strategies in the portfolio of services (implemented for the first time in 5.8% of the centres), activities in the media and/or social networks (4.3%), and informing professionals of new strategies (4.1%).
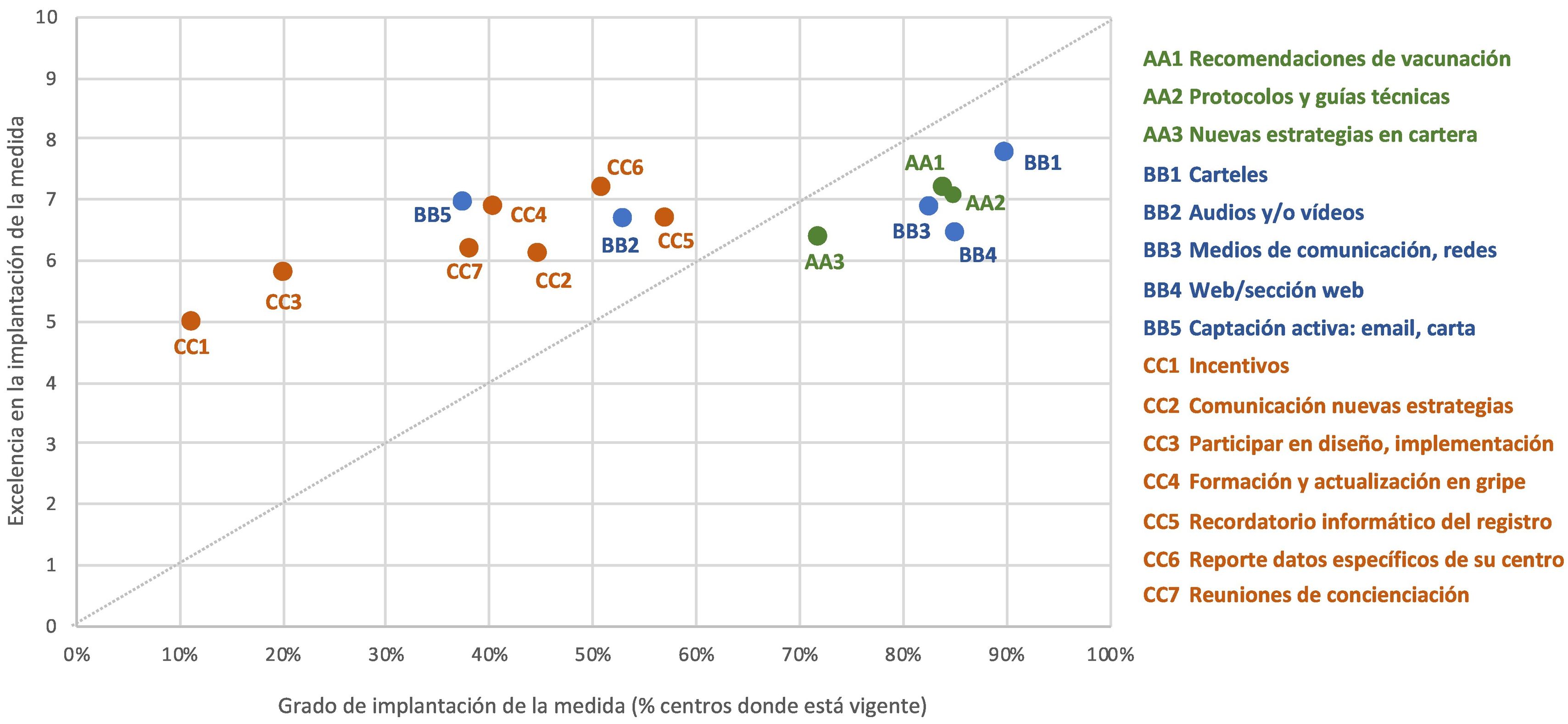
The next step was to ask about the quality of the implementation of the measures used. According to the respondents, the 3 measures that were best implemented were the distribution of posters in medical centres (with an average score of 7.8/10; SD: 2.0), informing professionals of the specific data in their place of work (7.2/10; SD:1.9) and publishing recommendations for vaccination (7.2/10; SD: 1.8), each one of which corresponded to a different area. On the contrary, the respondents considered that the measures which were implemented the poorest were vaccination incentives for professionals and invitations to take part in the design and implementation of new strategies to increase coverage (with average scores of 5.0/10 and 5.8/10, respectively). Both of these measures are also the ones that were implemented the least. Fig. 1 shows the relationship between the level of implementation or application of each measure to encourage vaccination among professionals and the degree of perceived quality in how it was implemented.
Measures to encourage vaccination according to the level of implementation in 2019–2020 and the quality of implementation.
Note: the level of implementation refers to the percentage of centres where the measure is currently being applied, regardless of how long this has been so. The quality of the implementation of the measure refers to the average score awarded by the respondents for how optimum its actual application was (where 10 is the maximum possible score). The colours of the figure correspond to the 3 blocks of areas identified in the survey, while the codes (letters and numbers) correspond to the 15 measures covered by the survey.
When the respondents were asked about which 2 measures in each block, they considered to be the most effective or able to increase the vaccination rate among medical professionals (n = 178), the highest scoring measures were, in this order: publishing recommendations to vaccinate (87.1% of votes), using the media and social networks (78.1%) and preparing and publishing protocols and technical guides (60.7%). At the opposite extreme, the measures considered to be the least effective were communicating new strategies and informing professionals of the data in their own workplace, with only 14% and 17% of votes, respectively.
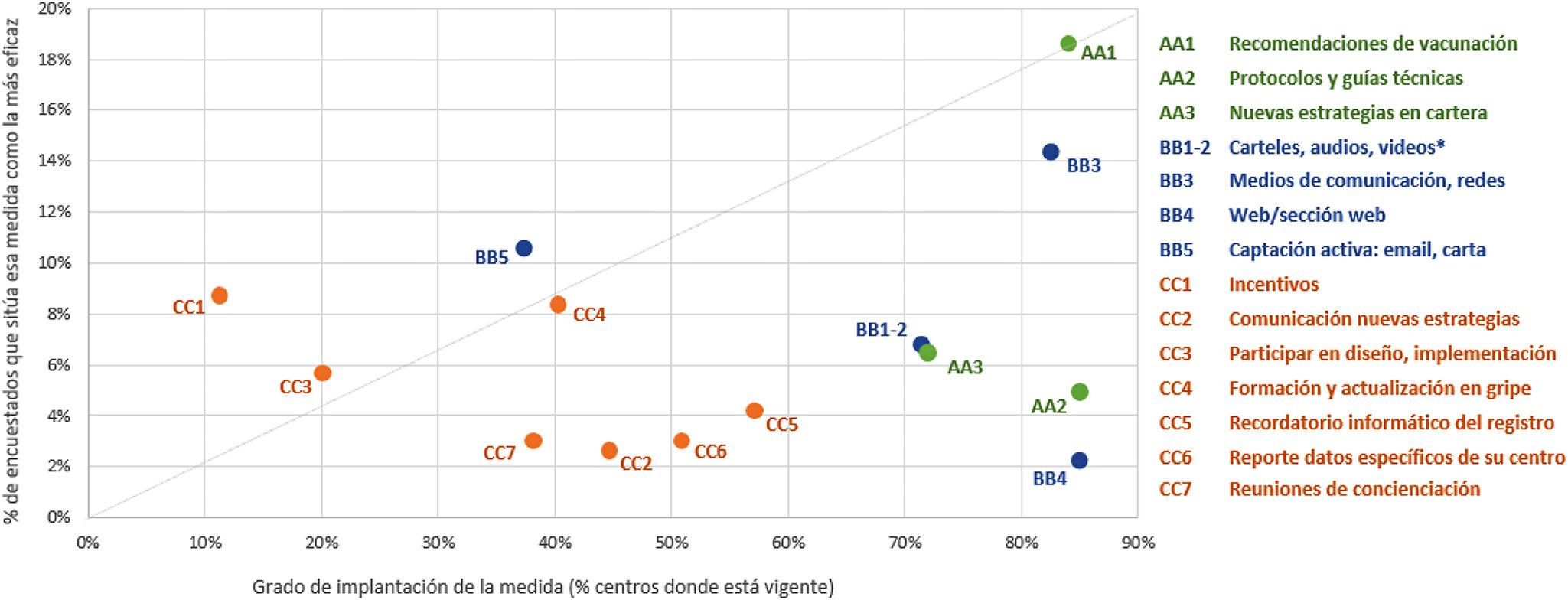
Finally, the respondents were asked to rank the 2 measures they had considered to be the most effective in each block. They chose the 3 which they considered to be the most effective in general, ranking them from more to less effective. They selected publishing recommendations to vaccinate in first place as the strongest action, with 18.6% of votes, followed by the use of the media and social networks (14.4%) and active recruitment by sending personalised emails and/or letters to professionals (10.6%) (Fig. 2).
Measures to encourage vaccination according to level of implementation in 2019–2020 and the efficacy of the measure.
⁎These measures were condensed in the question about efficacy, so that for the figure the average level of implementation or application is used.
Note: level of implementation refers to the percentage of centres where the measure is currently applied, regardless of how long this has been so. The quality of the implementation of the measure refers to the average score awarded by the respondents for how optimum its actual application was (where 10 is the maximum possible score). The colours of the figure correspond to the 3 blocks of areas identified in the survey, while the codes (letters and numbers) correspond to the 15 measures covered by the survey.
In the multivariate regression models, 10 measures to encourage vaccination were found to have a statistically significant effect on the vaccination of medical professionals in the 2019–2020 campaign (n = 160) (Table 4). The 3 measures with the greatest impact on vaccination coverage in this group were the distribution of posters in medical centres (with an increase of 17 percentage points in vaccination coverage, ceteris paribus the other measures), publishing recommendations for vaccination (14 pp) and preparing protocols and guides (13 pp). Meetings to raise awareness of the importance of vaccination would also be relevant, as would informing medical personnel of vaccination data, including new strategies in the services portfolio, computerised reminders, and personalised letters or emails.
Coefficients obtained in the regression models for measures to encourage vaccination among medical personnel.
| Measure | Coefficient | % corresponding to this measurea | |
|---|---|---|---|
| A | AA1. Publishing recommendations for vaccination | 14.05b | 86% |
| AA2. Protocols and technical guides | 13.24b | 87% | |
| AA3. New strategies in services portfolio | 10.22a | 73% | |
| B | BB1. Distributing posters in medical centres | 17.23b | 92% |
| BB2. Publishing audios and/or videos | – | 54% | |
| BB3. The media, social networks | – | 84% | |
| BB4. Specific web page/section | – | 86% | |
| BB5. Sending personalised emails, letters | 9.23b | 37% | |
| C | CC1. Incentives | – | 10% |
| CC2. Communicating new strategies | 7.68a | 46% | |
| CC3. Participating in strategy design / implementation | 8.83a | 22% | |
| CC4. Training and updating in flu and vaccines | – | 39% | |
| CC5. Computerised reminder of registry | 9.51b | 57% | |
| CC6. Report of specific data for their centre | 10.60b | 52% | |
| CC7. Meetings to raise awareness | 11.90b | 40% |
A: Block of measures “Documentation or institutional recommendations”. B: Block of measures “Campaign publicity activities”. C: Block of measures “Activities to encourage the involvement of professionals in vaccination”. The codes (letters and numbers) correspond to the 15 measures identified in the survey. a) Percentage of valid respondents (who supplied data on vaccine coverage in medical personnel during 2020) for whom this measure is applied. Models controlled according to sex, age group, flu vaccination, and flu training.
The Gripetool project made it possible to know which measures have been implemented in the regions and medical centres to encourage flu vaccination among medical personnel. For the first time in Spain, it compared the impact perceived by personnel of the different measures with the actual affect of the same using multivariate regression statistical analysis.
The results showed that half of the measures which models showed to be effective in increasing vaccination coverage were also considered to be relevant by the personnel surveyed. These were the recommendation to vaccinate, the preparation of protocols and technical guides, the distribution of posters, audios, and videos, the inclusion of new strategies in the portfolio of services, and the active recruitment of professionals to be vaccinated by personalised emails or letters. However, other actions which the models found to be effective were not supported so strongly by the personnel. These included meetings to raise awareness, informing personnel of the data, computerised reminders of the registration of coverage, professionals taking part in the design of new vaccination strategies, and informing personnel of the new strategies. In turn, certain of the initiatives which the respondents had said were effective lacked impact in theory. The most representative of these were publicity in the media and social networks, together with incentives.
If we combine the level of implementation or application of each measure and its perceived degree of effectiveness, then emphasis should be placed on the following measures, as they seem to be highly effective but are hardly used: incentives for medical personnel, active recruitment, and training about flu. On the other hand, it would also be necessary to emphasise or at least study measures which have a statistically significant impact but which are currently used less. These include meetings to raise awareness or computerised reminders.
However, it must also be borne in mind that this study was undertaken prior to the Covid-19 pandemic, so that the association between the measures applied then and vaccination coverage achieved in the 2019–2020 campaign are very different from the situation during the pandemic.10 In any case, once the economic, medical, and social crises causes by the pandemic have been overcome, there will be a risk of returning to the original situation, with vaccination rates that are below desirable levels and which differ from region to region, so that this study will be relevant as an analysis of the possible levers that could be used for anti-flu vaccination.
The vaccination of medical personnel against flu is a controversial subject in the literature, and many different approaches to this have been used.14,15 The desire to be vaccinated is associated with the perceived severity of the disease and the expected costs and benefits (clinical as well as social) of vaccination.16,17 Moreover, it should be remembered that vaccinating medical staff is not only cost-effective,18 as it may also have a positive association with the vaccination of other groups at risk.19 Medical personnel are also at higher risk of multiple morbidities, as more than half of them are over the age of 50 years,20 and that 40% of them have a higher risk of having 2 or more chronic diseases.21 Due to all of the above considerations, medical personnel should be made aware of the importance of vaccination against flu, raising their knowledge, and increasing their positive attitude to vaccination.22–24
According to some authors, the most effective intervention to encourage vaccination by medical personnel would be to demand that they be vaccinated, imposing fines, or other negative consequences if they are not, such as prohibiting any contact with patients, or making it obligatory to use a mask.14,25 Some studies link obligatory vaccination to an increase of more than 90% in vaccination coverage.26,27 Nevertheless, “tough” regulations may also give rise to drawbacks in practice when implemented, as they are associated with ethical problems and doctors' reluctance. Thus in spite of their high level of efficacy, alternative options are often chosen.
Of the “soft” forms of vaccination policy, rejection documents have been proven to be effective as a mild form of pressure, so that hesitant or indifferent workers come to accept vaccination, although it is recommended that this should not be the priority measure. Other interventions, such as easier access (free vaccination in the workplace, vaccination by colleagues, etc.), measure to raise awareness (posters, pamphlets, letters, reminders, informative pages about myths, etc.) or incentives (for individuals or groups) are less effective if they are applied alone. Nevertheless, if they are applied in combination their cumulative effect may be similar to that of the declarations of rejection.25 Other authors have also noted that combined strategies seem to be more effective than isolated measures,28 or that the centres which achieve the greatest success in vaccinating their personnel against flu use a wider variety of measures in terms of strategy, organisation, logistics, and staff in comparison with centres that achieve less coverage.29 There is also evidence that the means of getting the attention of the target population and directly connecting with their personal experiences are very important factors.30
This study has certain limitations. On the one hand, the number of replies to the survey was relatively low, restricting the degree to which the results may be representative and preventing detailed sub-analyses. The low rate of participation (a response rate of 3.2% of the 12 000 members of SEMERGEN) may be due to doctors' heavy workload during the pandemic and the type of information - technical - which was requested. On the one hand, the sample may be biased in favour of the most committed or participatory professionals. On the other hand, the regression analyses show the estimated of the measures when each one is applied alone, i.e., ceteris paribus regarding all of the other variables considered but not in combination or grouped. They should therefore be taken only as indicative values of what may happen if a centre that does not use one measure commences to do so. In any case, to the best of our knowledge, this is the first study in Spain which has attempted to quantify the actual impact of each measure on vaccination coverage, while also making it possible to compare the said effect with the opinions of the doctors.
To conclude, the Gripetool project has helped to strengthen the available evidence, suggesting that the most effective strategies to increase flu vaccinations among medical personnel could be those that include a range of actions at macro-, meso- and micro levels. These actions would connect with making it easy to access vaccines while also informing about their benefits, using the potential of the new technologies. It would be desirable in the future to continue with this line of work in greater depth, to determine which strategies may be the most relevant in each context to increase vaccination coverage. Finally, it would also be advisable to analyse the degree to which the pandemic may have affected vaccination against seasonal flu and the management of this, together with whether the new scenario will be static or dynamic over time.
FinancingThe Gripetool collaboration project received financial support from Sanofi Pasteur.
Juan Luis López-Belmonte, Elena Jurío and Georgina Drago are Sanofi employees and may hold company shares and/or share options. Néboa Zozaya, Javier Villaseca and Álvaro Hidalgo-Vega are Weber employees, a consultancy that received financing from Sanofi to undertake this project.
Conflict of InterestsThe Gripetool collaboration project received financial support from Sanofi Pasteur.
JLL-B, EJ and GD are Sanofi employees and may hold company shares and/or share options. NZ, JV and ÁH are Weber employees, a consultancy that received financing from Sanofi to undertake this project.
Grupo de expertos Gripetool: María del Carmen Azcárate Bang, Agustina Cano Espín, Cèlia Cols Sagarra, José Luis Díaz-Maroto Muñoz, Leovigildo Ginel Mendoza, Vicente Martín Sánchez, Gregorio Mediavilla Tris y Mercedes Ricote Belinchón.
Please cite this article as: Redondo Esther, Zozaya Néboa, Martín Vicente, Villaseca Javier, López-Belmonte Juan Luis, Drago Georgina, et al. Análisis de las mejores estrategias para el fomento de las coberturas de vacunación antigripal entre los profesionales sanitarios. Vacunas. 2022. https://doi.org/10.1016/j.vacun.2021.11.004