A 29-yr-old male Melicopter co-pilot with high flight hours in air transport missions of the patients with COVID-19 tested positive for his RT-PCR due to clinical suspicion. With the diagnosis of SARS-CoV-2, he was treated based on the national protocol and stayed in the home quarantine for two weeks. Having been released for flying, he faced nausea, vomiting, facial cold sweat and pallor, dizziness, and imbalance that eventually caused flying avoidance during the three first flights. He has never had a similar problem or any predisposing factors during his pilot's training and afterwards. All the probable reasons ruled out after a complete assessment. Following the diagnosis of moderate airsickness, he was abstained from flying and treated with different prevention and rehabilitation techniques. None of them had enough clinical efficacies, applying the United States Air Force Preventive Airsickness Protocol as the last choice. Despite the three separate consecutive therapeutic courses, no significant clinical improvement was observed, and could not return to fly, yet. That is the first reported case of intractable airsickness in a flight crew that may be associated with SARS-CoV-2 infection.
Un varón de 29 años de edad, copiloto de helicóptero médico, con gran número de horas de vuelo en misiones de transporte aéreo de los pacientes de COVID-19, dio positivo en las pruebas rápidas de PCR, debido a sospecha clínica. Diagnosticándose SARS-CoV-2, fue tratado sobre la base del protocolo nacional, permaneciendo en cuarentena domiciliaria durante dos semanas. Habiendo sido eximido de volar, padeció náuseas, vómitos, sudores fríos y palidez facial, mareos y falta de equilibrio, que le abstuvieron de volar durante las primeras tres semanas. No había tenido nunca un problema similar ni factores predisponentes durante su formación como piloto, ni después de esta. Tras un reconocimiento completo se descartaron todas las causas probables. Al diagnosticarse mareo moderado al volar, se le recomendó que se abstuviera de viajar en avión, tratándosele con diferentes técnicas de prevención y rehabilitación. Ninguna de ellas tuvo eficacia clínica suficiente, aplicándose el protocolo para la prevención de mareo al volar de las Fuerzas Aéreas de los Estados Unidos como última elección. A pesar de realizar los tres cursos terapéuticos separados consecutivos no se observó una mejora clínica significativa, y no pudo volver a volar. Se trata del primer caso reportado de mareo al volar irresoluble en una tripulación de vuelo, que puede estar asociado a la infección por SARS-CoV-2.
A year have passed since the severe acute respiratory syndrome Coronavirus 2 (SARS-Cov-2) caused the COVID-19 outbreak in Wuhan, China. The full-blown COVID-19 pandemic thus emerged a century after the Spanish influenza. The World Health Organization (WHO) records 66,855,949 confirmed cases and 1,534,553 fatalities globally as of 6 December 2020.1,2 Neurological manifestations are not common but reported during the acute phase and treatment period.3 Being a neurotrophic, neuroinvasive, and neuroinflammatory virus,4 Li et al. recently described the neuroinvasive potential of COVID-19 and related clinical manifestations.
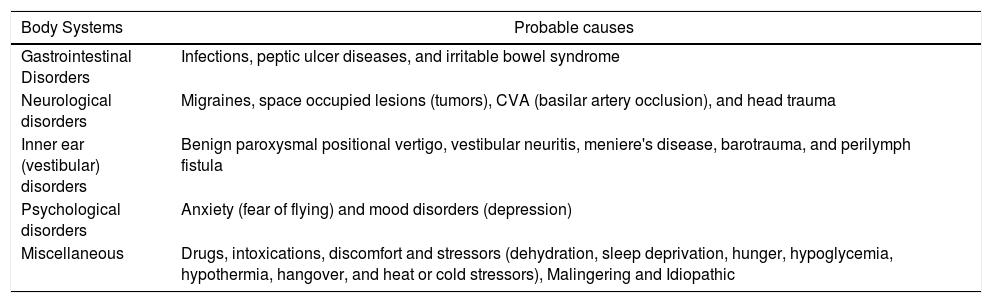
Case reportA 29-yr-old male Medicopter (Mil, Mi-17) co-pilot with high flight hours in air transport missions of the patients with COVID-19 tested positive for his nasopharyngeal specimen RT-PCR due to clinical suspicion. With positive test for COVID-19 he was treated based on the national protocol and recommended for rest and staying in quarantine for two weeks at home. Three weeks later, in the follow-up session with the aeromedical examiner, he was in good clinical condition except for mild malaise and then released for flying. During the first three flights, he faced several irritating features as nausea, vomiting, facial cold sweat and pallor, dizziness, and imbalance that eventually caused flying avoidance. He has never had a similar problem or any predisposing factors during his pilot's training and afterwards. Before the airsickness diagnosis, during a full and exact clinical and paraclinical (electronystagmography and brain MRI) assessment, all the probable reasons which may have been the cause of these features must be ruled out as differential diagnosis (Table 1).
Probable causes that must be ruled out before the airsickness diagnosis.
| Body Systems | Probable causes |
|---|---|
| Gastrointestinal Disorders | Infections, peptic ulcer diseases, and irritable bowel syndrome |
| Neurological disorders | Migraines, space occupied lesions (tumors), CVA (basilar artery occlusion), and head trauma |
| Inner ear (vestibular) disorders | Benign paroxysmal positional vertigo, vestibular neuritis, meniere's disease, barotrauma, and perilymph fistula |
| Psychological disorders | Anxiety (fear of flying) and mood disorders (depression) |
| Miscellaneous | Drugs, intoxications, discomfort and stressors (dehydration, sleep deprivation, hunger, hypoglycemia, hypothermia, hangover, and heat or cold stressors), Malingering and Idiopathic |
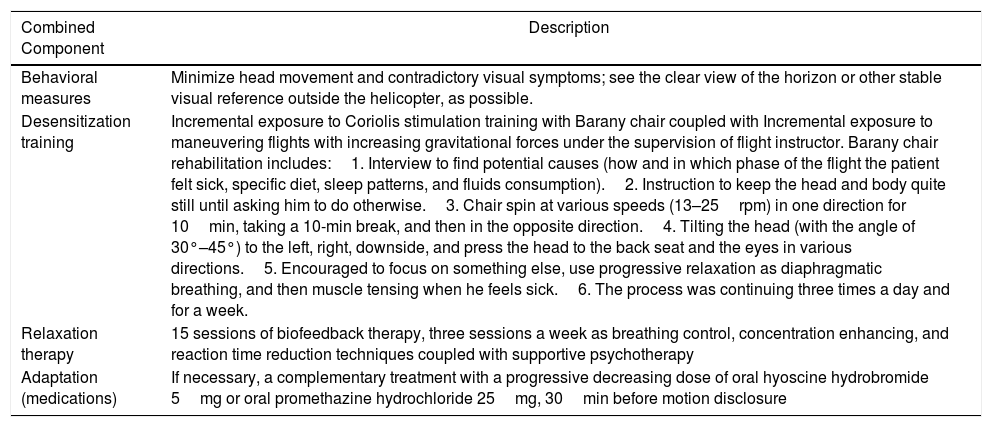
Then, with the diagnosis of moderate airsickness, base on the airsickness severity scoring, he was suspended from flying and treated with a wide range of preventative methods as adaptation, desensitization training, relaxation therapy, behavioral therapy, and medication modalities, but after a month, there was no significant improvement. In the last attempt to recover and return to flying, the United States Air Force (USAF) preventive airsickness protocol was conducted, as the most effective and acceptable combined method (Table 2).
USAF preventive airsickness protocol.
| Combined Component | Description |
|---|---|
| Behavioral measures | Minimize head movement and contradictory visual symptoms; see the clear view of the horizon or other stable visual reference outside the helicopter, as possible. |
| Desensitization training | Incremental exposure to Coriolis stimulation training with Barany chair coupled with Incremental exposure to maneuvering flights with increasing gravitational forces under the supervision of flight instructor. Barany chair rehabilitation includes:1. Interview to find potential causes (how and in which phase of the flight the patient felt sick, specific diet, sleep patterns, and fluids consumption).2. Instruction to keep the head and body quite still until asking him to do otherwise.3. Chair spin at various speeds (13–25rpm) in one direction for 10min, taking a 10-min break, and then in the opposite direction.4. Tilting the head (with the angle of 30°–45°) to the left, right, downside, and press the head to the back seat and the eyes in various directions.5. Encouraged to focus on something else, use progressive relaxation as diaphragmatic breathing, and then muscle tensing when he feels sick.6. The process was continuing three times a day and for a week. |
| Relaxation therapy | 15 sessions of biofeedback therapy, three sessions a week as breathing control, concentration enhancing, and reaction time reduction techniques coupled with supportive psychotherapy |
| Adaptation (medications) | If necessary, a complementary treatment with a progressive decreasing dose of oral hyoscine hydrobromide 5mg or oral promethazine hydrochloride 25mg, 30min before motion disclosure |
Despite the three separate consecutive treatment courses, no significant clinical improvement was observed. His airsickness control depends on taking sedative agents (hyoscine and promethazine), according to the international aeromedical regulations, any sedative agent usage for flight crew is forbidden, and could not return to fly, yet.
DiscussionAirsickness is a common and complex syndrome that could be an inappropriate response to an abnormal real or perceived motion stimulus. Although the exact neurobiological mechanism is unclear, the widely accepted “Sensory Conflict or Neural Mismatch” hypothesis proposes that the motion stimulus has to be abnormal in such a way as to generate illegitimate combinations of motion sensation either within the components of the vestibular system or between visual and vestibular evidence of motion. This theory has been very successful in explaining the features of those types of motion that provoke sickness, but it does not address the question as to why nausea, or for that matter, any symptoms, should be associated with these types of motion. Such signals are at variance with the internal model of the pattern of motion signals that the central nervous system expects to receive. It is proposed that the resulting mismatch signal evokes the sequence of neural responses that constitute the motion sickness syndrome. An additional feature of this hypothesis is that a sustained mismatch signal brings about a rearrangement of the internal model to accommodate the changed pattern of motion stimuli. This leads to a reduction in sensory conflict and a lessening of symptoms that allows the individual to function more effectively in the novel motion environment.8,9
Airsickness presentation can be diverse, varied from nausea facial cold sweating, pallor, dizziness, imbalance, yawning, and increased salivation that may lead to flying avoidance. So, it is a debilitating condition that harms flight crew performance and is quite unable to perform its allotted duties. There is considerable individual variability in susceptibility and a variety of techniques that are available for assessing an individual's vulnerability.5–9
Airsickness is also one of the most common causes of flying avoidance during flight training and eventually may leads to early and permanent medical disqualification, especially in military cadets.10
These days, behavioral therapy, especially a combination of biofeedback, progressive exposure, and autogenic training, is more common and acceptable. Yet, the USAF preventive airsickness protocol is the most effective and reliable combined method, and 85 percent of the aircrews were taken back to flying. That is a combination therapy that by learning to control the autonomic responses and allay anxiety evoked by motion stimuli, susceptibility to motion sickness will be decreased and the rate at which protective adaptation acquired will be enhanced.9 This mysterious respiratory virus is also able to produce different extra respiratory multi-systemic (particularly neurological) involvement as an immune-mediated complexes.3,4
In conclusion, this is the first reported case of intractable airsickness associated with COVID-19 infection. Considering the probable pathophysiology of airsickness and the possibility of multi-systemic involvement in COVID-19, the authors believe that these features, in this case, maybe due to vestibular, visual, or neural systems involvement. More research and investigations should be done by expert colleagues to clarify the definitive causes in the future.
Conflict of interestsThe authors declare no conflict of interests.