To identify the correlation between the psychosocial condition of adolescent women in the postpartum period and mother-infant bonding.
MethodThis study used a cross-sectional design. Using a consecutive sampling method, 103 adolescent women with a 1- to 12-week-old baby were recruited. Participants completed the postpartum bonding questionnaire to identify mother-infant bonding. This questionnaire included four dimensions: the relationship between mother and baby, baby acceptance, readiness to perform maintenance, and delivery of comfort.
ResultsWe identified that 45.6% of the teen mothers in this study were at risk of psychosocial problems and that 67% of them had insufficient mother-infant bonding. There was a statistically significant correlation between the psychosocial condition of adolescent postpartum women and mother-infant bonding (p=0.000; OR=5.143; 95%CI, 0.195 to 135.662).
ConclusionsAdolescent mothers require special attention during the perinatal period. They also require infant care education and preparation to become a successful mother. Maternity nurses play a very important role in providing education for adolescent mothers and the elderly. Maternity nursing services must be expanded to include psychosocial assessments for teen mothers throughout the pregnancy, childbirth, and postpartum periods.
Every human being goes through stages of life that have their own developmental tasks. The developmental tasks of adolescence, for example, are different than those associated with motherhood. Indeed, pregnancy in adolescent is an uncommon phenomenon. Being a mother during one’s adolescent stage may lead to many psychological issues, such as anger, anxiety, and negligence to the baby1. Adolescent mothers tend to experience volatile emotions, irritability, and distress2. Moreover, the egocentric nature of an adolescent may cause an adolescent mother to be less compassionate and empathetic to her baby3. These conditions may make the adolescent mother feel unready to assume the role of motherhood4. This is distressing for the mother but even worse for the baby, who may feel socially isolated, rejected, or sad5.
Maternal and infant bonding is initiated in the first 30-60 minutes after birth and continues with the development of a loving relationship between the mother and baby6. This interaction during the postpartum period is the key process of the individual relationship between the mother and baby, which will last through the future7. Maternal and infant bonding manifests with gentle touches, gazing, and close physical contact, which nourishes the positive emotional state of the baby. This is essential to the baby’s growth and development. Conversely, poor mother-infant bonding negatively impacts the child’s development and trust.
The bonding quality of the mother and baby plays an essential role in their wellness. Positive or negative outcomes of the mother-infant interaction will sustain over time in the baby’s life8. The interpersonal, cognitive, and affective relationships of an adult are rooted in mother-infant bonding during early life. Insufficient mother-infant bonding may have serious long-term impacts on parenting and on the child’s development and psychological condition9. Lack of mother-infant bonding is indicated by the mother’s grumpy attitude and her rejecting of the baby, which may eventually lead to neglect, avoidance, and abuse of the baby10. This study aimed to identify the relations between the psychosocial condition of the postpartum adolescent mother and mother-infant bonding.
MethodThis was a correlational study with a cross-sectional design. A total of 103 respondents were recruited using a consecutive sampling method in the service area of six community health centers in West Java, Indonesia. These six areas have a markedly higher number of adolescent mothers in West Java province. A woman was considered to be eligible as a respondent for this study if she was a postpartum mother aged 14-19 years; in the 1- to 12-week period after birth; had spontaneous vaginal delivery; was married; and could read and write. The exclusion criteria were having current or a history of psychiatric, alcohol consumption, or substance abuse problems.
Data were collated from May to June 2016 after the study permit from the Provincial Health Office was granted. We approached the respondents to fill out the questionnaires during the Integrated Health Service (Pos Pelayanan Terpadu) activity, which is an Indonesian government program for maternal and child public health.
We used a postpartum bonding questionnaire to measure mother-infant bonding. This is a 25-item questionnaire with four dimensions: disturbed bonding, rejection and pathological anger, anxiety about the infant and incipient abuse. The validity and reliability test yielded scores of 0.545-0.922 and a reliability score of 0.971. Hence, the tool is valid and reliable. We also used a postnatal risk questionnaire to assess the psychosocial condition of the postpartum mothers. This questionnaire is a self-report tool consisting of 12 questions regarding perinatal problems, perinatal depression, and anxiety. This tool also assesses the history of mental health problems, physical trauma (i.e., domestic violence), sexual abuse, and emotional abuse. Prior tests showed a validity score of 0.630-0.963 and a reliability score of 0.938.
A univariate analysis was done to describe the psychosocial condition of adolescent mothers during the postpartum period and during mother-infant bonding. Furthermore, we carried out a chi-square analysis to answer the following research hypothesis: is there any relationship between the psychosocial condition of the adolescent postpartum mother and mother-infant bonding? We used SPSS statistical pro-gram version 15 to facilitate the statistical data treatment.
This study was approved by the Ethical Committee of Faculty of Nursing, Universitas Indonesia. All respondents signed the informed consent form after a thorough explanation about the study was given.
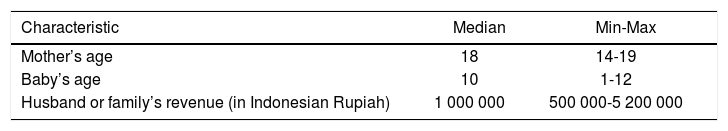
ResultsRespondent characteristics are described in Table 1.
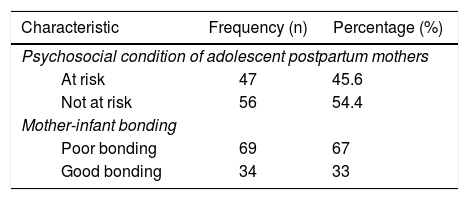
A description of adolescent mothers’ psychosocial conditions during postpartum and mother-infant bonding is summarized in Table 2. Adolescent mothers’ psychosocial conditions during the postpartum period were mostly at risk (45%), with the majority (67%) reporting poor mother-infant bonding.
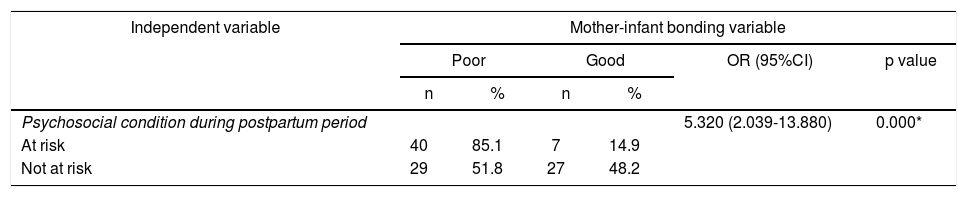
A bivariate analysis to identify the correlation between psychosocial conditions of adolescent mothers during the postpartum period and during mother-infant bonding is presented in Table 3.
Correlation between psychosocial conditions of adolescent mothers during postpartum periods and mother-infant bonding (n=103).
| Independent variable | Mother-infant bonding variable | |||||
|---|---|---|---|---|---|---|
| Poor | Good | OR (95%CI) | p value | |||
| n | % | n | % | |||
| Psychosocial condition during postpartum period | 5.320 (2.039-13.880) | 0.000* | ||||
| At risk | 40 | 85.1 | 7 | 14.9 | ||
| Not at risk | 29 | 51.8 | 27 | 48.2 | ||
As shown in Table 3, there was a statistically significant correlation between the psychosocial conditions of adolescent mothers during postpartum periods and during mother-infant bonding (p=0.000). Adolescent mothers whose psychosocial condition was at risk during the postpartum period were more likely to have poorer mother-infant bonding (5.320 times lower) than those without risk, with a 95% confidence interval between 2.039 and 13.880 (OR=5.320; 95%CI, 2.039-13.880).
DiscussionAdolescence, on the other hand, is the transitional phase to adulthood in which individuals strive for self-identity. Unfulfilled adolescents’ developmental tasks will complicate adolescent mothers’ ability to accept their new role as mothers, resulting in insensitivity towards their babies’ needs. Lacking ability in newborn care leads to insufficient interaction and care, thus loosening the bond between the mother and her baby4.
Results showed that most mother-infant bonding was poor. The majority of mothers at psychosocial risk had poor bonding. Mothers’ psychosocial condition during the post-partum period contributes to changes such as anxiety, fatigue, and physical alterations11. Postpartum mothers are prone to experiencing anxiety12. Other psychosocial conditions include past psychological history, physical trauma, abuse by in-laws and one’s husband, and emotional problems13. These conditions will result in negative consequences that will negatively affect the mother-infant bond14. A negative bond between a mother and her baby may manifest as irritability, hostility, and rejecting the baby, which leads to negligence, avoidance, and abuse10. This will cause emotional disturbances that lead to avoidance and neglect in infants. The number of teenage mothers in Indonesia is high, suggesting a potential increase in the occurrence of infant and child neglect.
Mothers with conditions such as stress, anxiety, and depression are often less active and less responsive and rarely play or communicate with their babies15. Mothers with impaired psychosocial conditions may not feel good when dealing with their babies. Finally, mothers may feel that the presence of a baby is a burden and will experience less confidence in caring for their babies.
The study revealed that adolescent mothers with psychosocial problem experience degraded mother-infant bonding16. Mothers with psychosocial problem such as depression during the 2-3 month postpartum period experience emotional problems in mother-infant bonding17. Similarly, anxiety degrades mother-infant bonding18, and altered psychological conditions may also cause impaired mother-infant interactions. Therefore, mothers with postpartum depression are at a heightened risk for having impaired mother-infant bonding compared to those without such a condition19. Teenage mothers are also at risk of developing an anxiety disorder, especially if they do not receive support from their husbands or families. Family support for a teen mother comes from her husband and her family.
This study on mother-infant bonding in Indonesia showed that there was correlation between mothers with psychosocial problems and mother-infant bonding20. Impaired psychosocial conditions will affect the emotional and physical health of the mother and her baby21 and result in the mother’s hesitancy to care for her baby18. Mothers with psychosocial problems such as depression during the 2-3 month postpartum period will experience emotional problems related to mother-infant bonding17. This is because a disturbed psychosocial condition will affect the emotional and physical aspects of the mother and her baby and will result in the mother’s hesitancy to care for her own baby, thus degrading their bond.
These results are also in line with Kurniawati’s study20, which demonstrated that the psychosocial conditions of a postpartum mother have the greatest correlation to mother-infant bonding. Psychosocial conditions that degrade mother-infant bonding include past psychological history, physical trauma, abuse by in-laws and one’s husband, and emotional problems22. This may contribute to the emotional and behavioral development issues in the baby, leading to the child’s poor sense of self and adaptability23. Infant behavior tends to be fussy, irritable, and sad, for example, and infants tend to struggle to adapt to new environments. Forms of mother-infant bonding, such as mentoring, calm touches, and attentiveness, cultivate positive emotions in the baby and have important implications for growth.
Conflicts of interestThere are no conflicts of interest to declare.
This study was funded by the Direktorat Penelitian dan Pengabdian Masyarakat of Universitas Indonesia.