The purpose of this study was to obtain an overview on nurses’ opinions and perceptions related to pain assessment and other problems experienced in evaluating pain in cancer patients.
MethodThis descriptive qualitative study was part of a series of studies to develop a pain assessment tool for cancer patients in Indonesia. Data were collected by semi-structured interviews from 16 oncology nurses. A cross-case comparison of the interview responses was used to analyze the data from verbatim interview transcripts.
ResultsSix themes were identified: pain as the main complaint reported by cancer patients; pain assessment using a pain scale; an awareness of the absence of nurses’ role in pain management; a lack of understanding of pain conditions; acknowledgement that a pain assessment tool should be practical and user friendly; and the need to develop a pain assessment tool. We also explored the knowledge of nurses in pain management and achieved an in-depth understanding of the nurses’ desire to seek additional knowledge related to pain assessment.
ConclusionsA pain assessment tool should be developed to assist nurses to independently interpret data about pain and allow them to select or modify interventions consistent with the patients’ needs. Pain management for cancer patients is one of the essential nurses’ responsibilities in providing comprehensive meaningful nursing care.
Pain is one of the main complaints of most cancer patients1. The pain is caused by tumor infiltration into pain-sensitive anatomical structures, such as bone, soft tissue, muscles, nerves, viscera, and blood. Some pain arises from medical treatments, including surgery, chemotherapy or radiotherapy. Approximately 15% of cancer patients who require a neurological assessment suffer from disturbing symptoms and neurological complications. Among them, pain is the most frequently reported complaint2.
Cancer patients usually have several different types of pain, including nociceptive and neuropathic pain3. Neuropathic cancer pain can result from nerve injury associated with neoplasm or anti-neoplasm therapy, such as a nerve or plexus that may be depressed or infiltrated by the tumor or damaged during surgery. Chemotherapy can cause axonal injury or changes in the axoplasm, and radiation injuries may lead to gliosis, fibrosis, and vascular disorders2.
Pain has been reported as the main reason many patients seek medical help, including those with cancer. The pain management needs of cancer patients should be considered by nurses when providing comprehensive nursing care4–9. However, nursing care in Indonesia does not include pain assessment practices that are appropriate to the culture and needs of Indonesian patients. Ideally, any pain assessment must be supported by an instrument that can measure all dimensions of pain.
Aspects that should be covered in a pain assessment instrument are pain intensity, the pattern of pain, treatment or mitigating factors, location, interference, quality, effect, duration, patient beliefs (attitude/coping strategies), and pain history10–13. Several instruments have been previously developed and have met the criteria of a good instrument. However, the experience of pain is not only physical but also psychological, socio-cultural, and environmental; therefore, it is necessary to use an instrument appropriate for the Indonesian context.
Various inventories that have been developed allow nurses to choose or modify them according to their needs. However, the ability of nurses and the characteristics of patients should be considered during the development of these instruments. Therefore, a study to develop a pain assessment instrument that involves nurses with considering the nurses and patient background should be conducted so that nursing professionals can easily use the instrument to assess pain and integrate the assessment in their nursing care. This study aimed to explore the different reflections of nurses who work in cancer or oncology care units. The reflections were associated with nurses’ opinions and perceptions of pain assessment as well as other problems experienced by the nurses when performing pain assessments.
MethodThis descriptive qualitative study incorporated four phases of analysis: bracketing (ethical inquiry); analyzing (empirical examination); intuiting (personal insight), and describing (esthetics)14. The investigators set aside any preconceived ideas that might influence the data collection in the bracketing phase.
The investigation included 16 nurses who worked at the Cancer Hospital in Jakarta, Indonesia, and they were selected using a purposive sampling method. The study was approved by the Ethical Committee of the Faculty of Medicine at the Universitas Indonesia. All participants met the inclusion and exclusion criteria. A close relationship between the participants and the investigators was established. The participants received a detailed explanation about the study and provided written consent for their participation, including permission to record their statements. Next, the participants were asked to determine the time and place to conduct the interviews according to their wishes so that they would feel comfortable describing their experiences associated with the pain assessment. A cross-case comparison of the interview responses was applied to analyze the obtained data. The investigators later transcribed all interviews into verbatim transcripts. Each participant approved his or her own verbatim transcript to ensure data accuracy. The data analysis was then followed by a four-step procedure using Giorgi's method as follows: the transcriptions were read and re-read to gain a sense of the whole meaning; meaningful units were isolated from the text of the interview; the data were then individually placed on index cards; and the investigators devised a coding system including categories, subcategories, and themes, which were extracted to create a structure15.
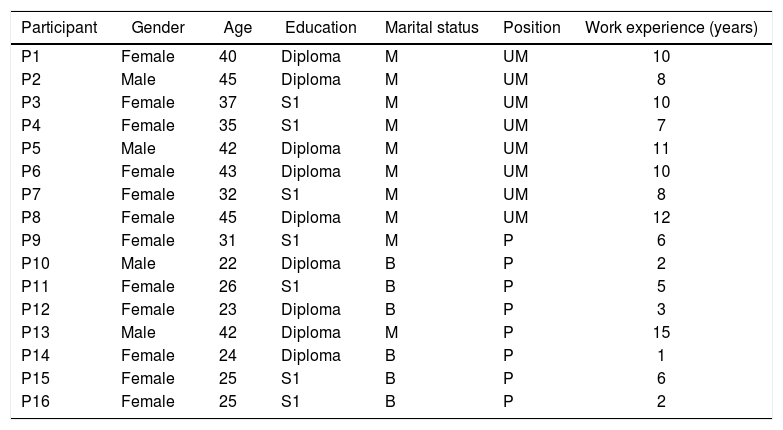
ResultsThe age of participants varied from 22-45 years old, and their amount of work experience at a cancer hospital ranged between 2-15 years. Their educational backgrounds included a mixture of nursing diplomas and bachelor's degrees. Table 1 describes the characteristics of the participants in detail.
Characteristics of the participants.
| Participant | Gender | Age | Education | Marital status | Position | Work experience (years) |
|---|---|---|---|---|---|---|
| P1 | Female | 40 | Diploma | M | UM | 10 |
| P2 | Male | 45 | Diploma | M | UM | 8 |
| P3 | Female | 37 | S1 | M | UM | 10 |
| P4 | Female | 35 | S1 | M | UM | 7 |
| P5 | Male | 42 | Diploma | M | UM | 11 |
| P6 | Female | 43 | Diploma | M | UM | 10 |
| P7 | Female | 32 | S1 | M | UM | 8 |
| P8 | Female | 45 | Diploma | M | UM | 12 |
| P9 | Female | 31 | S1 | M | P | 6 |
| P10 | Male | 22 | Diploma | B | P | 2 |
| P11 | Female | 26 | S1 | B | P | 5 |
| P12 | Female | 23 | Diploma | B | P | 3 |
| P13 | Male | 42 | Diploma | M | P | 15 |
| P14 | Female | 24 | Diploma | B | P | 1 |
| P15 | Female | 25 | S1 | B | P | 6 |
| P16 | Female | 25 | S1 | B | P | 2 |
B: unmarried; M: married; P: practitioner; UM: unit manager.
Six themes were generated from a variety of the participants’ reflections, which included pain as the main complaint reported by cancer patients; pain assessment using a pain scale; an awareness of the absence of nurses’ role in pain management; a lack of understanding of pain conditions; the realization that a pain assessment tool should be practical and user friendly; and the need to develop an appropriate pain assessment tool. However, these themes were interconnected with each other to provide an essential meaning of the nurses’ reflection related to their experiences in pain assessment and the need to use a pain assessment instrument. Detailed explanations of the description of the themes are as follows:
1. Pain as the main complaint reported by cancer patients. All nurses stated that a pain assessment should be routinely performed and become one of their regular duties. The assessment should be carried out early when the patients are admitted to the hospital for the very first time. The nurses also said that there is a need to change their nursing practice, especially with regard to pain management, because pain is the main complaint reported by cancer patients. Here is one of the participants’ statements: “Ever since I’ve worked here, I have never found any patient who doesn’t have a pain complaint... Well, most of them (the patients) have pain complaints, and in my opinion, the pain is a day-to-day experience. In general, I can say that pain is the primary complaint of cancer patients...” (P1).
2. Pain assessment using a pain scale. Some nurses said that to assess pain, they only used a pain scale. The patient's pain was classified using the numbers listed on that scale. However, some nurses assessed patient pain by measuring vital signs, observing body movements, and evaluating the anxiety experienced by the patients. “We usually use a pain scale to identify how patients can feel pain... The patient just points to the numbers listed on the scale...” (P4). “We also can assess pain using vital sign measurements... or body movement whenever the pain comes and the patient is experiencing it... sometimes (we can know) from their anxious behavior... if (they are) highly anxious, it means that they have severe pain...” (P16).
3. An awareness of the absence of nurses’ role in pain management. Currently, the role of nurses in pain management is more likely to be a collaborative role rather than an independent role. The nurses stated that recognition of their roles in pain management should be a priority, especially in the management of cancer patients. However, the healthcare service system in the cancer unit still predominantly uses a medical approach, which may make nurses’ role in pain management less optimal. “Until now, we feel that patient's complaint of pain is very medical... (we are) too quick to provide pain medications, and some (patients) even develop an addiction... the dose ride continues... I think... so, our role to provide nursing intervention is very limited... (it is) no more than teaching about deep breathing...” (P8).
4. A lack of understanding of the problems experienced in a pain assessment.
Most nurses do not understand how the diagnosis of pain is formulated, as they generate their knowledge of patient pain based only on the result of a pain assessment. They reported that they were given only limited time to learn to understand pain conditions. The nurses stated that their current understanding of pain conditions was minimal. They did not understand the entire concept of the pain phenomenon. “We frankly do not know much about the concept of pain, maybe even the very basic facts that we should know about pain; it is reasonable that we are still performing the assessment only on superficial ground... (smile)...” (P9).
Pain assessments should be performed to allow interventions to be given to alleviate patient pain. Nurses have historically not performed a comprehensive pain assessment because pain is usually treated with medical or pharmacological interventions. Most interventions to ease pain have traditionally been performed by physicians. “Yes, we seek a reason for our hesitation in performing the pain assessment because... Well, you know... we are told that pain management in this unit is very medical (pharmacological)... it is difficult for us (who are not physicians) to do a pain assessment...” (P10).
5. A pain assessment tool should be practical and user friendly. The participants had been using a general format form to identify pain; however, they preferred a specific instrument for pain assessment that was more beneficial for treatment, as the instrument may focus more on pain assessment. The form they currently used often caused the nurses to fail to formulate a nursing diagnosis, as pharmacological agents were the only intervention they had to relieve the pain: “So far, we are only using general forms, like this (she showed the forms) [...] yeah, it is not as specific as you mentioned... and we actually need a specific one... one that is more appropriate when formulating a diagnosis related to pain...” (P12).
6. The need to develop an appropriate pain assessment tool. This study revealed that nurses need to develop a pain instrument. They mentioned the ability to develop its format to allow for nursing interventions related to pain. The instruments they will need should be specific to pain and should not be combined with other assessments. “We really need to have our own form for this... so far, we still use a common, general assessment, which is a part of other assessments... So, yes, we just need a little aspect of assessment on pain...” (P11).
Throughout the interviews, the nurses mentioned that pain is the main complaint reported by patients with cancer. Generally, our major finding was the need for an instrument to assess pain that can also identify the causes of pain, understand its impact, identify pain relief strategies, and evaluate their effectiveness11. Our study also revealed that pain complaints experienced by cancer patients should be a major concern and pain should be considered one of the major physical complaints that may cause acute and severe distress and affect the long-term survival of patients with cancer16,17.
Nurses have attempted to assess patient complaints and behavior related to pain in different ways. They have identified the characteristics and intensity of pain using the Visual Analog Scale, observing the patients’ behavior or body language during pain, or assessing their anxiety level. Increased blood pressure, pulse, and respiration rates may also become their major concern. Similar findings have also been revealed by previous studies18,19. However, the assessments made by the nurses in our study are more likely to be based on intuitive calls, and they were not well organized.
As health providers, oncology nurses have an important role in the assessment and management of pain20,21. It is important to enhance the knowledge and skills related to pain assessment among healthcare providers, especially nurses, to improve their performance in pain management22,23.
When performing pain assessments, nurses first must have the competency to do so. A deep understanding of the pain concept itself is required so that the nurses may communicate effectively and assist patients in alleviating their pain24. Some studies have reported that healthcare providers, including nurses, are not optimal for performing pain management, particularly for the management of pain in cancer patients4–9. A similar issue has also been suggested by our findings. All nurses have agreed that they do not completely understand the pain conditions experienced by their patients, as the method of pain management they currently perform only focuses on pharmacological treatment.
Furthermore, the nurses indicated their eagerness for greater knowledge related to pain assessment. They also will require an appropriate tool for pain assessment to allow them to independently obtain more accurate data on pain management. The instrument for pain assessment may assist nurses in selecting or modifying pain interventions according to their patient's needs. To provide comprehensive nursing care, nurses are responsible for offering cancer patients adequate pain relief.