Over the last decade, family medicine has been progressively rejected by medical students as a career choice in many Western countries. Our objective is to contribute to a better understanding of this phenomenon by examining the reputation of and identification processes with family medicine by medical students.
DesignA qualitative case study.
MethodsFocus groups and document analysis were used for generating empirical material. Focus groups (n=6) were conducted (2008–2009). Thematic analysis was adopted as the technique for analyzing data gathered.
SettingA faculty of medicine of a Spanish university.
ParticipantsSecond and sixth year undergraduate medical students (N=48).
ResultsFamily medicine appears to be largely devalued as a professional activity, among medical students, being viewed as a monotonous and non-technological medical practice with no intellectual challenge. Such a negative view, which already appears in early stages of medical training, leads to a lack of identification with this medical practice by students.
ConclusionMisconceptions about the practice of family medicine, created and reproduced in health care system and societal contexts, encourage the practice of specialized medicine. In addition, the academic environment appears to promote organ- and disease-based medical knowledge, which goes against the holistic and patient-centered approach characteristic of the practice of family medicine. In order to improve the reputation of family medicine and for it to be considered as an attractive career path by medical students, it is recommended that family medicine is developed as an academic medical field, and that improvements are made in the conditions and status of this medical practice within the health care system.
En la última década, los estudiantes de medicina han ido descartando progresivamente la medicina de familia como opción de carrera en muchos países occidentales. El objetivo de este artículo es contribuir a comprender mejor este fenómeno mediante el examen de la reputación y los procesos de identificación de los estudiantes de medicina con la medicina de familia.
DiseñoEstudio de caso cualitativo.
MétodoGrupos focales y análisis documental fueron los métodos utilizados para generar datos. Se desarrollaron seis grupos focales (2008–2009). El análisis temático fue la técnica de análisis del material recogido.
EmplazamientoUna facultad de medicina española.
Participantes48 estudiantes de 2.o y 6.o año.
ResultadosLa medicina de familia aparece devaluada como actividad profesional entre los estudiantes, siendo su práctica considerada como monótona, no tecnológica y sin desafío intelectual. Esta visión negativa, que ya aparece en primeras etapas de la formación, estimula la falta de identificación con esta especialidad.
ConclusiónLos conceptos erróneos sobre la práctica de la medicina de familia se crean y reproducen tanto en el sistema de salud como en otros contextos sociales, donde se prima la práctica de medicina especializada. Así mismo, el contexto académico promueve el conocimiento médico basado en el órgano y la enfermedad, en claro contraste con la visión holística característica de la medicina de familia. Para mejorar la reputación de esta especialidad y su consideración como opción profesional atractiva, se sugiere estimular su desarrollo como disciplina académica así como mejorar las condiciones de su práctica en el sistema sanitario.
Over the last decade, medical students from a number of Western countries have shown a common declining interest in family medicine as a career choice.1–5 Thus far, a number of factors have been identified as possible explanations for this trend, e.g. a significant gap between specialty and family medicine incomes, the increasing number of clinical conditions requiring medical specialty interventions, due to medical technological advancements, and professional status.6–9 As part of a larger international investigation1 aimed at understanding the social construction of professional identity of family physicians in different academic centres, the purpose of the present study has been to explore the reputation of and professional identification processes with family medicine practice among students enrolled in a modern Spanish faculty of medicine.
A profession is an occupation characterised by both the possession of a specialised body of knowledge and a commitment to service.10Identification involves a process of differentiation by which individuals attach value to a particular group membership and a separation from other social groups that are not only ‘different,’ but also usually ‘less valuable’.11–13 From this, it follows that reputation, i.e. what outside observers believe or say about the uniqueness of ‘something’ (e.g. an organization, a company, a profession) appears to be a critical concept to better understand professional identity construction.14
Professional identity construction starts in educational institutions where trainees internalise the norms, values and power relations that characterise the collective identity of the profession to which they aspire to belong.15 Two recent papers examine identity issues during the family medicine residency period.16,17 However, processes of family medicine professional identity construction throughout undergraduate medical studies remain little explored. Due to the fact that medical students are ‘physicians-to-be’, it would appear premature to explore family physician professional identity per se. However, the examination of contributing identity-linked processes of reputation of and identification (or lack thereof) with family medicine practice among medical students appears to be not only reasonable but also suitable to better explain the observable phenomenon of waning interest in family medicine as a career choice. Accordingly, the research questions that have guided the present investigation have been stated as follows: (1) What do medical students think about family medicine practice? (2) What are the reasons why medical students take up or avoid family medicine as a career choice?
MethodsResearch designAs mentioned previously, this investigation is part of a larger international project, led by the third author, in which a qualitative case-based research strategy has been adopted.18 Our four cases are international medical academic centres in Canada, France, Spain, and the United Kingdom. Appropriate approvals by the Institutional Review Boards of the faculties of medicine involved in the study were obtained.
The cases were chosen purposefully and respond to both theoretical and practical concerns. The cases offer a variety of situational, organizational and societal contexts (maximum variation sampling18) regarding the topic under investigation. Practical concerns relate to the leader of the international research team, who holds a faculty position at a Canadian Department of Family Medicine, is of Spanish origin, and has established professional relationships with a number of family medicine researchers from the UK and France. In this paper, we report the results of the Spanish individual case of our international investigation.18
The Spanish Medical and Family Medicine Training ProgramThe Faculty of Medicine of this Spanish university graduates about 100 medical students every year, after 6 years of undergraduate medical training. By law, 80% of the curriculum content is shared with the rest of Spanish medical schools. Clerkships (rotations) start at the end of the 3rd academic year and take place in university hospitals. In contrast to Canada and France and similarly to UK, the Spanish Health Ministry is responsible for specialized training in medical residency programs. All graduate students must pass an annual national exam, i.e. Medical Internal Resident (MIR). According to their scores, graduate students will be able to choose their medical specialty. Family medicine offers the greatest number of residency positions – about 33–35% on average – and, in general, is a career path chosen by candidates with lower MIR scores. Indeed, family medicine comprises 4 years of residency, and training takes place in acute care hospitals, long-term care facilities, and community health centres.
Data gathering and analysisThe main method used for gathering appropriate data for the study was focus group interviewing. This technique is intended to obtain information regarding the attitudes, opinions, and behaviors of the participants around a particular topic of interest.19 Our intention was to engage medical students in in-depth discussions about their thoughts on the family medicine specialty (i.e. reputation) and the pros and cons of pursuing a career as a family physician (i.e. identification). In order to capture differences in thoughts, opinions, and attitudes related to the number of years of exposure to medical education centre discourses, focus groups were carried out with both 2nd and 6th year medical students. Their involvement in the study was requested through the Dean of the Faculty, who contacted student representatives and informed them about the study. The project was then publicised on the faculty students’ intranet. In addition, the first two authors introduced the project personally to students during lectures. Participation was on a voluntary basis. A total of 6 focus groups (i.e. 3 meetings per group of students) were conducted in May 2008 and May 2009. Focus groups consisted of 6–9 students. In total, 48 students participated in the discussions over the period, 27 out of a total of about 120 2nd year medical students and 21 out of a total of about 100 6th year medical students. Focus groups took place in university classrooms and lasted 2h on average. The first and second authors acted alternatively as group coordinator in all, and the third author participated in the last focus group. Notes about the discussion process and content were systematically written down by the authors during the sessions. Students signed a consent form prior to participation and, with their permission, all the focus groups were recorded and transcribed verbatim by research staff.
Data from focus groups were complemented by documentary analysis of a variety of documents pertinent to the purpose of the investigation, such as academic material, health ministry reports, and documents about family medicine residency.
Focus groups verbatim were subjected to discursive thematic analysis.20 First, researchers carefully read the corpus verbatim. Then, initial inductive coding, using the software package N-Vivo 7.0, was performed separately by the two first authors. The initial list of codes was discussed among the three authors and was followed by successive iterations until a definitive set of themes was created. These resulting themes, in combination with documentary analysis and field notes, supported further discussions among the three members of the research team, which ended up with the elaboration of interpretations on processes under examination.
We finally note that, in order to ensure maximum qualitative reliability and validity, a number of verification strategies21 were adopted while conducting the investigation. Thus, we first consider the congruence between the research question and our methodological decisions (methodological coherence). Then we carefully selected participants who could provide the best possible information regarding the topic of the study. Also data collection and analysis were iterative processes, emerging ideas being systematically confirmed with new data. Finally, the research team worked closely in developing the interpretations and concepts that best facilitate the understanding of the phenomenon under investigation.
ResultsWe have identified four main themes that refer to the reputation of and identification processes with family medicine as a career choice. These interrelated themes are family medicine ‘practice’, ‘knowledge and skills’, ‘prestige’, and ‘attitudes,’ and are interpreted in connection with four different contexts, namely individual, medical academic environment, health care system, and society as a whole (see also Tables 1–4).
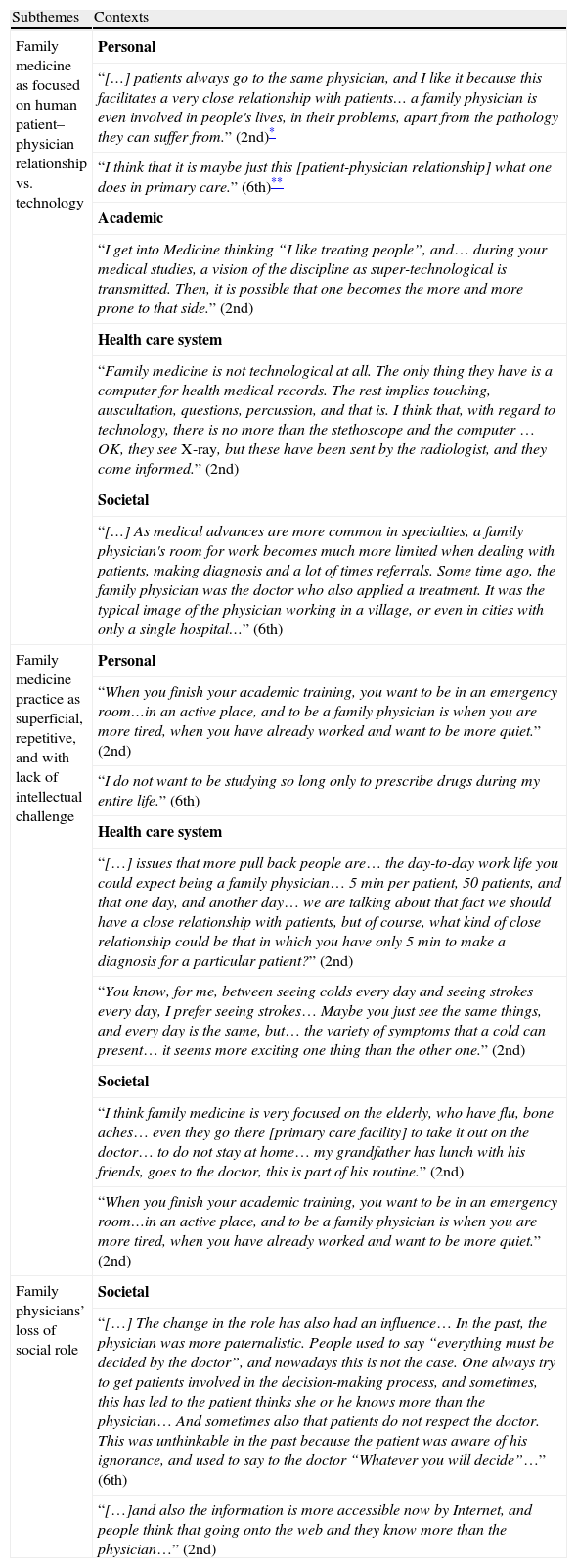
The practice of family medicine
| Subthemes | Contexts |
| Family medicine as focused on human patient–physician relationship vs. technology | Personal |
| “[…] patients always go to the same physician, and I like it because this facilitates a very close relationship with patients… a family physician is even involved in people's lives, in their problems, apart from the pathology they can suffer from.” (2nd)* | |
| “I think that it is maybe just this [patient-physician relationship] what one does in primary care.” (6th)** | |
| Academic | |
| “I get into Medicine thinking “I like treating people”, and… during your medical studies, a vision of the discipline as super-technological is transmitted. Then, it is possible that one becomes the more and more prone to that side.” (2nd) | |
| Health care system | |
| “Family medicine is not technological at all. The only thing they have is a computer for health medical records. The rest implies touching, auscultation, questions, percussion, and that is. I think that, with regard to technology, there is no more than the stethoscope and the computer … OK, they see X-ray, but these have been sent by the radiologist, and they come informed.” (2nd) | |
| Societal | |
| “[…] As medical advances are more common in specialties, a family physician's room for work becomes much more limited when dealing with patients, making diagnosis and a lot of times referrals. Some time ago, the family physician was the doctor who also applied a treatment. It was the typical image of the physician working in a village, or even in cities with only a single hospital…” (6th) | |
| Family medicine practice as superficial, repetitive, and with lack of intellectual challenge | Personal |
| “When you finish your academic training, you want to be in an emergency room…in an active place, and to be a family physician is when you are more tired, when you have already worked and want to be more quiet.” (2nd) | |
| “I do not want to be studying so long only to prescribe drugs during my entire life.” (6th) | |
| Health care system | |
| “[…] issues that more pull back people are… the day-to-day work life you could expect being a family physician… 5min per patient, 50 patients, and that one day, and another day… we are talking about that fact we should have a close relationship with patients, but of course, what kind of close relationship could be that in which you have only 5min to make a diagnosis for a particular patient?” (2nd) | |
| “You know, for me, between seeing colds every day and seeing strokes every day, I prefer seeing strokes… Maybe you just see the same things, and every day is the same, but… the variety of symptoms that a cold can present… it seems more exciting one thing than the other one.” (2nd) | |
| Societal | |
| “I think family medicine is very focused on the elderly, who have flu, bone aches… even they go there [primary care facility] to take it out on the doctor… to do not stay at home… my grandfather has lunch with his friends, goes to the doctor, this is part of his routine.” (2nd) | |
| “When you finish your academic training, you want to be in an emergency room…in an active place, and to be a family physician is when you are more tired, when you have already worked and want to be more quiet.” (2nd) | |
| Family physicians’ loss of social role | Societal |
| “[…] The change in the role has also had an influence… In the past, the physician was more paternalistic. People used to say “everything must be decided by the doctor”, and nowadays this is not the case. One always try to get patients involved in the decision-making process, and sometimes, this has led to the patient thinks she or he knows more than the physician… And sometimes also that patients do not respect the doctor. This was unthinkable in the past because the patient was aware of his ignorance, and used to say to the doctor “Whatever you will decide”…” (6th) | |
| “[…]and also the information is more accessible now by Internet, and people think that going onto the web and they know more than the physician…” (2nd) |
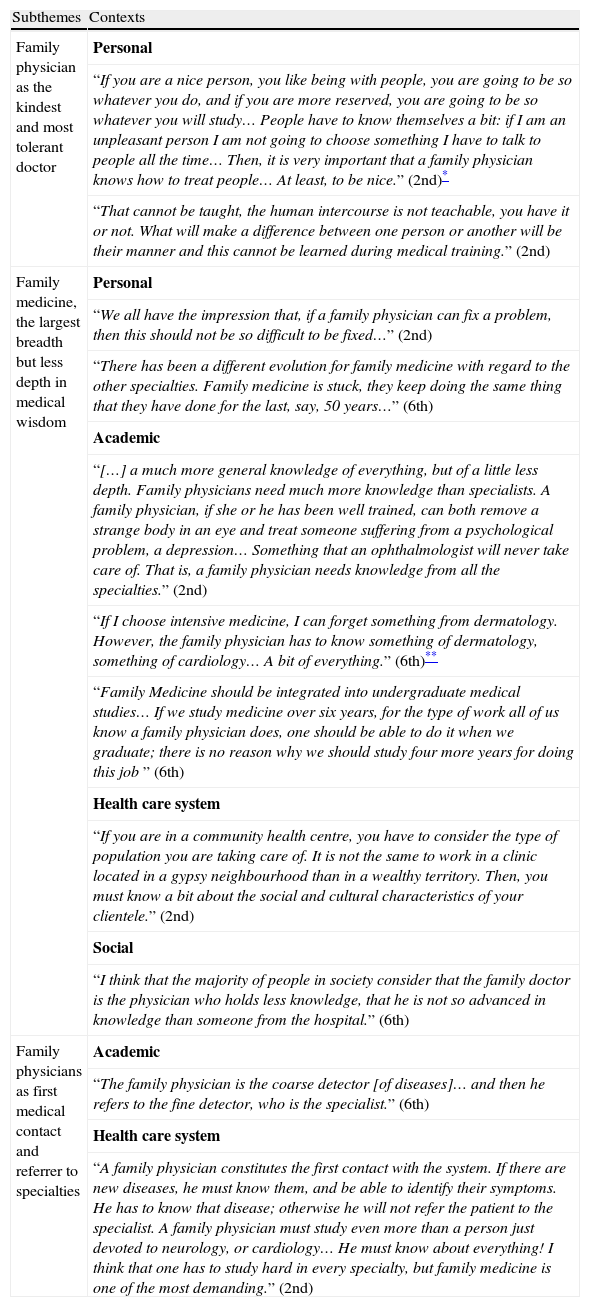
Family medicine knowledge and skills
| Subthemes | Contexts |
| Family physician as the kindest and most tolerant doctor | Personal |
| “If you are a nice person, you like being with people, you are going to be so whatever you do, and if you are more reserved, you are going to be so whatever you will study… People have to know themselves a bit: if I am an unpleasant person I am not going to choose something I have to talk to people all the time… Then, it is very important that a family physician knows how to treat people… At least, to be nice.” (2nd)* | |
| “That cannot be taught, the human intercourse is not teachable, you have it or not. What will make a difference between one person or another will be their manner and this cannot be learned during medical training.” (2nd) | |
| Family medicine, the largest breadth but less depth in medical wisdom | Personal |
| “We all have the impression that, if a family physician can fix a problem, then this should not be so difficult to be fixed…” (2nd) | |
| “There has been a different evolution for family medicine with regard to the other specialties. Family medicine is stuck, they keep doing the same thing that they have done for the last, say, 50 years…” (6th) | |
| Academic | |
| “[…] a much more general knowledge of everything, but of a little less depth. Family physicians need much more knowledge than specialists. A family physician, if she or he has been well trained, can both remove a strange body in an eye and treat someone suffering from a psychological problem, a depression… Something that an ophthalmologist will never take care of. That is, a family physician needs knowledge from all the specialties.” (2nd) | |
| “If I choose intensive medicine, I can forget something from dermatology. However, the family physician has to know something of dermatology, something of cardiology… A bit of everything.” (6th)** | |
| “Family Medicine should be integrated into undergraduate medical studies… If we study medicine over six years, for the type of work all of us know a family physician does, one should be able to do it when we graduate; there is no reason why we should study four more years for doing this job ” (6th) | |
| Health care system | |
| “If you are in a community health centre, you have to consider the type of population you are taking care of. It is not the same to work in a clinic located in a gypsy neighbourhood than in a wealthy territory. Then, you must know a bit about the social and cultural characteristics of your clientele.” (2nd) | |
| Social | |
| “I think that the majority of people in society consider that the family doctor is the physician who holds less knowledge, that he is not so advanced in knowledge than someone from the hospital.” (6th) | |
| Family physicians as first medical contact and referrer to specialties | Academic |
| “The family physician is the coarse detector [of diseases]… and then he refers to the fine detector, who is the specialist.” (6th) | |
| Health care system | |
| “A family physician constitutes the first contact with the system. If there are new diseases, he must know them, and be able to identify their symptoms. He has to know that disease; otherwise he will not refer the patient to the specialist. A family physician must study even more than a person just devoted to neurology, or cardiology… He must know about everything! I think that one has to study hard in every specialty, but family medicine is one of the most demanding.” (2nd) |
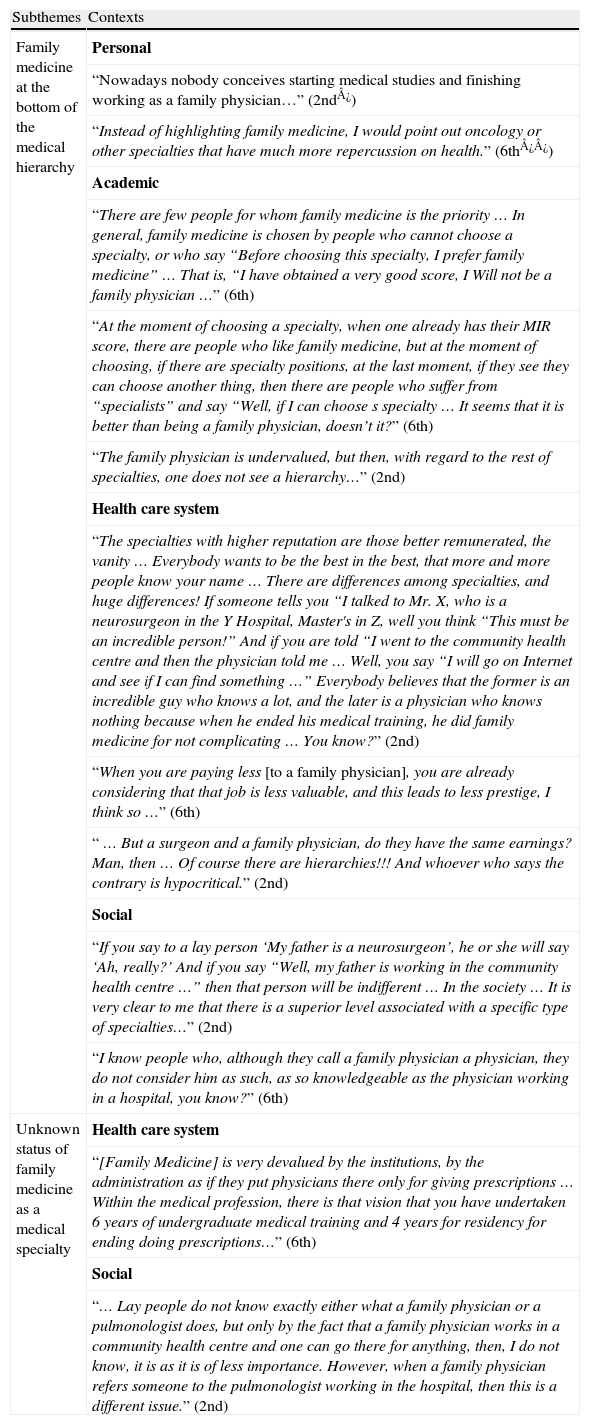
Family medicine prestige
| Subthemes | Contexts |
| Family medicine at the bottom of the medical hierarchy | Personal |
| “Nowadays nobody conceives starting medical studies and finishing working as a family physician…” (2nd¿) | |
| “Instead of highlighting family medicine, I would point out oncology or other specialties that have much more repercussion on health.” (6th¿¿) | |
| Academic | |
| “There are few people for whom family medicine is the priority … In general, family medicine is chosen by people who cannot choose a specialty, or who say “Before choosing this specialty, I prefer family medicine” … That is, “I have obtained a very good score, I Will not be a family physician …” (6th) | |
| “At the moment of choosing a specialty, when one already has their MIR score, there are people who like family medicine, but at the moment of choosing, if there are specialty positions, at the last moment, if they see they can choose another thing, then there are people who suffer from “specialists” and say “Well, if I can choose s specialty … It seems that it is better than being a family physician, doesn’t it?” (6th) | |
| “The family physician is undervalued, but then, with regard to the rest of specialties, one does not see a hierarchy…” (2nd) | |
| Health care system | |
| “The specialties with higher reputation are those better remunerated, the vanity … Everybody wants to be the best in the best, that more and more people know your name … There are differences among specialties, and huge differences! If someone tells you “I talked to Mr. X, who is a neurosurgeon in the Y Hospital, Master's in Z, well you think “This must be an incredible person!” And if you are told “I went to the community health centre and then the physician told me … Well, you say “I will go on Internet and see if I can find something …” Everybody believes that the former is an incredible guy who knows a lot, and the later is a physician who knows nothing because when he ended his medical training, he did family medicine for not complicating … You know?” (2nd) | |
| “When you are paying less [to a family physician], you are already considering that that job is less valuable, and this leads to less prestige, I think so …” (6th) | |
| “ … But a surgeon and a family physician, do they have the same earnings? Man, then … Of course there are hierarchies!!! And whoever who says the contrary is hypocritical.” (2nd) | |
| Social | |
| “If you say to a lay person ‘My father is a neurosurgeon’, he or she will say ‘Ah, really?’ And if you say “Well, my father is working in the community health centre …” then that person will be indifferent … In the society … It is very clear to me that there is a superior level associated with a specific type of specialties…” (2nd) | |
| “I know people who, although they call a family physician a physician, they do not consider him as such, as so knowledgeable as the physician working in a hospital, you know?” (6th) | |
| Unknown status of family medicine as a medical specialty | Health care system |
| “[Family Medicine] is very devalued by the institutions, by the administration as if they put physicians there only for giving prescriptions … Within the medical profession, there is that vision that you have undertaken 6 years of undergraduate medical training and 4 years for residency for ending doing prescriptions…” (6th) | |
| Social | |
| “… Lay people do not know exactly either what a family physician or a pulmonologist does, but only by the fact that a family physician works in a community health centre and one can go there for anything, then, I do not know, it is as it is of less importance. However, when a family physician refers someone to the pulmonologist working in the hospital, then this is a different issue.” (2nd) |
*2nd year medical student; **6th year medical student.
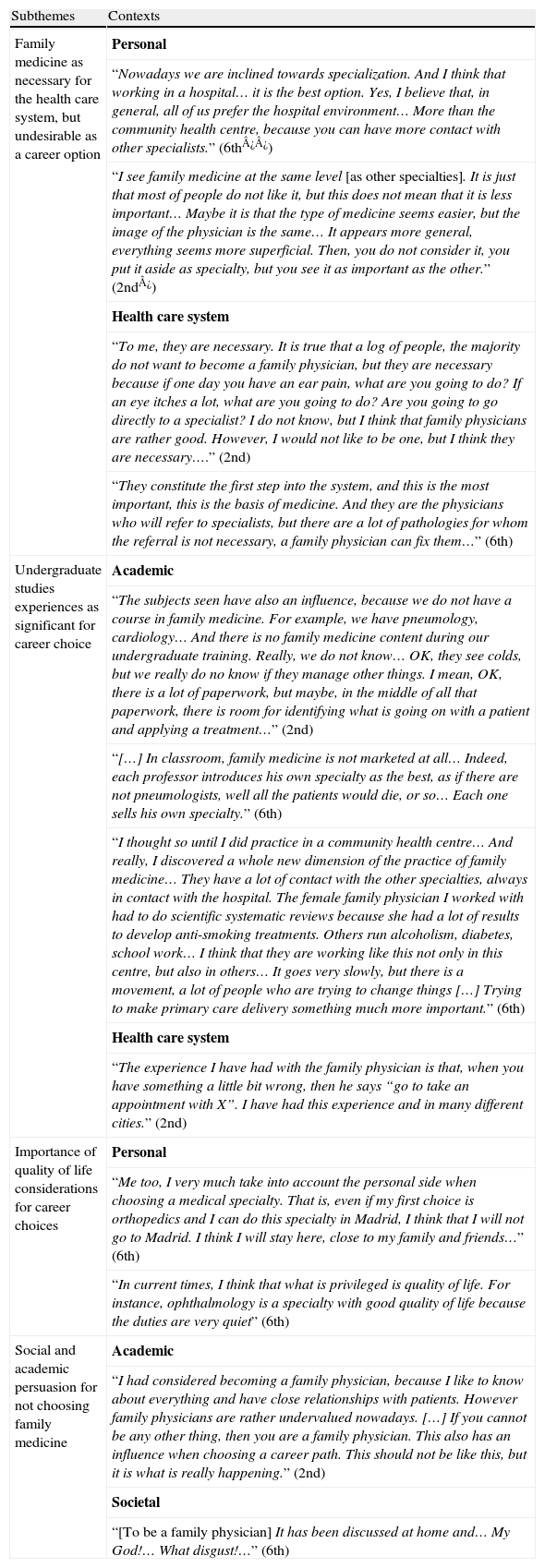
Attitudes vis-à-vis family medicine as a career choice
| Subthemes | Contexts |
| Family medicine as necessary for the health care system, but undesirable as a career option | Personal |
| “Nowadays we are inclined towards specialization. And I think that working in a hospital… it is the best option. Yes, I believe that, in general, all of us prefer the hospital environment… More than the community health centre, because you can have more contact with other specialists.” (6th¿¿) | |
| “I see family medicine at the same level [as other specialties]. It is just that most of people do not like it, but this does not mean that it is less important… Maybe it is that the type of medicine seems easier, but the image of the physician is the same… It appears more general, everything seems more superficial. Then, you do not consider it, you put it aside as specialty, but you see it as important as the other.” (2nd¿) | |
| Health care system | |
| “To me, they are necessary. It is true that a log of people, the majority do not want to become a family physician, but they are necessary because if one day you have an ear pain, what are you going to do? If an eye itches a lot, what are you going to do? Are you going to go directly to a specialist? I do not know, but I think that family physicians are rather good. However, I would not like to be one, but I think they are necessary….” (2nd) | |
| “They constitute the first step into the system, and this is the most important, this is the basis of medicine. And they are the physicians who will refer to specialists, but there are a lot of pathologies for whom the referral is not necessary, a family physician can fix them…” (6th) | |
| Undergraduate studies experiences as significant for career choice | Academic |
| “The subjects seen have also an influence, because we do not have a course in family medicine. For example, we have pneumology, cardiology… And there is no family medicine content during our undergraduate training. Really, we do not know… OK, they see colds, but we really do no know if they manage other things. I mean, OK, there is a lot of paperwork, but maybe, in the middle of all that paperwork, there is room for identifying what is going on with a patient and applying a treatment…” (2nd) | |
| “[…] In classroom, family medicine is not marketed at all… Indeed, each professor introduces his own specialty as the best, as if there are not pneumologists, well all the patients would die, or so… Each one sells his own specialty.” (6th) | |
| “I thought so until I did practice in a community health centre… And really, I discovered a whole new dimension of the practice of family medicine… They have a lot of contact with the other specialties, always in contact with the hospital. The female family physician I worked with had to do scientific systematic reviews because she had a lot of results to develop anti-smoking treatments. Others run alcoholism, diabetes, school work… I think that they are working like this not only in this centre, but also in others… It goes very slowly, but there is a movement, a lot of people who are trying to change things […] Trying to make primary care delivery something much more important.” (6th) | |
| Health care system | |
| “The experience I have had with the family physician is that, when you have something a little bit wrong, then he says “go to take an appointment with X”. I have had this experience and in many different cities.” (2nd) | |
| Importance of quality of life considerations for career choices | Personal |
| “Me too, I very much take into account the personal side when choosing a medical specialty. That is, even if my first choice is orthopedics and I can do this specialty in Madrid, I think that I will not go to Madrid. I think I will stay here, close to my family and friends…” (6th) | |
| “In current times, I think that what is privileged is quality of life. For instance, ophthalmology is a specialty with good quality of life because the duties are very quiet” (6th) | |
| Social and academic persuasion for not choosing family medicine | Academic |
| “I had considered becoming a family physician, because I like to know about everything and have close relationships with patients. However family physicians are rather undervalued nowadays. […] If you cannot be any other thing, then you are a family physician. This also has an influence when choosing a career path. This should not be like this, but it is what is really happening.” (2nd) | |
| Societal | |
| “[To be a family physician] It has been discussed at home and… My God!… What disgust!…” (6th) |
*2nd year medical student; **6th year medical student.
Students describe the special patient–physician relationship established in family medicine as close, continuous in time, and focused on the whole person as distinctive of family medicine practice: “[family medicine] is the most holistic medicine; the physician knows people all their lives and follows them over time” (6th year medical student). Nevertheless, this emphasis on the human relationship is presented in opposition to medical technology. Even 2nd year medical students, for whom human relationships with patients are highly valued at the beginning of their medical training, suggest that over time, technological aspects of medical practice become more and more important. Indeed, for both 2nd and 6th year medical students, family medicine practice appears unattractive because of the absence of ‘technology’.
When students think of family physicians, they draw a very negative picture of the practice. For instance, they perceive that primary care facilities, at most, led to a ‘quasi-administrative’ medical practice, which mainly involves drug prescriptions and referrals to specialists. In addition, although students consider family medicine as a necessary medical field of practice, its content is superficial to them and is focused on issues perceived as simple and easy to diagnose or treat. Therefore, they view family medicine as a practice without intellectual challenges. Yet, 2nd year medical students stress that family medicine practice would be more appropriate as an end-of-career choice.
Another aspect that makes family medicine practice unattractive for medical students is that family physicians’ clientele mainly consists of the elderly. In particular, 2nd year medical students devalue the type of problems this sub-population present, as well as the associated overuse of medical resources. Although students also recognized that all medical specialties can become monotonous, they particularly come down on family medicine in this regard: “You know, for me, between seeing colds every day and seeing strokes every day, I prefer seeing strokes…” (2nd year medical student).
Family physicians represent, for medical students, the figure of the traditional doctor in terms of ‘broad’ practice—rather close to medical practice in rural settings. In addition, they highlight that, in our times, this figure is no longer present in other medical specialties: “[…] I think that what is missing nowadays in many specialties is the faith in a particular physician, that figure that, I think, certain family physicians still exhibit.” Having said this, they also think that family medicine has become more and more exceptional as the current conditions of practice have led family physicians to lose this role.
Family medicine knowledge and skillsStudents think that ‘personality’ is an important factor to take into account when selecting any medical specialty. Since the main feature of the practice of family medicine is the human relationship, a person choosing family medicine should be a tolerant, serene, and kind individual who enjoys human relationships. Most students understand these personal traits to be innate rather than learned; people without these qualities should not select this specialty as a career choice.
Students regard the family medicine discipline as encompassing more knowledge than other specialties. In fact, according to their views, a family physician has to acquire knowledge from all medical specialties, although shallower. Students are conscious that family medicine practice also involves knowledge about the community context within which a family physician operates, something that is particular to family medicine. However, particularly for some 6th year medical students, family medicine knowledge is viewed as opposite to specialty expertise: “It is true that in many specialties (family medicine, internal medicine, paediatrics), one has a larger knowledge base. Nevertheless, in our times the trend is towards specialization. You know about something, and you are the expert on that.” Sixth-year medical students perceive the current four-year residency program in family medicine, after six years of medical undergraduate studies as unnecessary.
Well-known roles of a family physician in the health care system are gatekeeper and care coordinator. All medical students acknowledge these functions, but while 2nd year students point out their importance, 6th year medical students attribute less value to them: “The specialty of family medicine mostly involves the distinction between serious and mild diseases, to decide whether or not it is necessary to urgently refer a patient to the hospital. This is the ability a family physician has to have: to be able to make the distinction between serious and mild problems” (6th year medical student).
Family medicine prestigeFamily medicine is viewed by students as less prestigious than other medical fields, surgery specialties being at the top: “There is a very clear hierarchy in medicine, and family medicine is at the bottom… Above lab but below medical specialties. Surgery has always had much prestige.” This low status is associated with lower salaries, less impressive facilities (community health centre vs. hospital), and a devalued type of knowledge needed to practice (general vs. specific medical knowledge). In addition, the technology used in current medical practice clearly places family medicine at the bottom of the heap: “One becomes a specialist when mastering techniques, apart from the specific theory in your field. The tools used by a family physician are, well, the stick, the stethoscope, and a lot of pens” (6th year medical student).
In addition, students believe that health care decision makers, as well as the population, fail to appreciate family medicine. For the former, this is associated with the high volume of administrative tasks that family physicians have to take on; for the latter, it is due both to family physician's accessibility outside hospital settings and the belief that it is not a specialty: “Only the fact that the family physician works in a community health centre, and one can go there for everything, it looks like family medicine practice is of less importance… People think that, when you finish your undergraduate studies, you can practice as a family physician; they are not aware it is a medical specialty” (2nd year medical student).
For 6th year medical students, the low professional prestige of family medicine practice appears to be concomitant with a lack of clear medical identity from an organicist point of view: “[…] Then, a lay person asks you ‘What type of physician are you? A family physician…? What do you cure?’ What you are going to answer…? A cardiologist treats heart diseases, a nephrologist treats kidney diseases… If you are a family physician, what do you treat…?” In contrast, for 2nd year medical students, the lack of professional recognition appears to be mostly related to the alleged limitations of family medicine practice in the specific Spanish context: “[Family physicians] in Spain are undervalued, but they play an important role in other countries… Here, they have no authority. From this everything goes down, because they do not have the social prestige they used to have…”.
Attitudes vis-à-vis family medicine as a career choiceWhen students are asked to explain the reasons underlying their career choice, they highlight the importance of family physicians as key players in the health care system while pointing out that family medicine is not an option for them. This happens either at the beginning or the end of their undergraduate training. Features discussed above become reasons for not choosing family medicine. Besides this, students’ experiences as health care system users have made them more conscious of professional problems experienced when practicing as a family physician.
Students recognize that they are not exposed to family medicine during their training, so they have little idea of what is really involved in being a family physician: “[…] Maybe this is one of the reasons why we are not attracted by family medicine: because actually we do not know what family medicine is. We finish our undergraduate studies and think that family medicine practice mostly consists of signing drug prescriptions, but this practice might have another content nobody has taught to us” (6th year medical student). In fact, it appears that few good experiences in later training years positively influence student attitudes with regard to family medicine practice: “[…] I always had that idea of the family physician… you arrive there, sit down, get a prescription, and leave. Now, I have known that there is another way, another manner to be a family physician. Yes, it is possible” (6th year medical student).
Quality of life appears to be critical when choosing a specialty, in particular for 6th year medical students. It concerns, for instance, the amount of tasks to be developed or the intensity and number of duties. Yet students consider quality of life specifically related to the city where they will pursue their residency, as well as the possibilities of work afterwards. Surprisingly, this quality of life criterion is considered only for specialties other than family medicine. In addition, it does not appear as a dimension that could support their choice for a family medicine career.
Related to this, one of the particular characteristics of the Spanish health care system is that physicians can work both in public and the private sectors. In this context, family physicians are not seen by the population as a specialty to consider when using private medicine because of the direct access to the rest of specialties available to them. Therefore, family medicine as a career choice appears unattractive to students because of the lower probability of generating additional income when practicing in the private sector.
Finally, all the students stress social pressure from family and relatives to become a specialist other than a family physician, which is viewed as a devalued ‘general’ practitioner: “Now people think that you will finish your studies and you will not be a family physician: you have to be a neurosurgeon and, if possible, in Barcelona… Less than that, you have spent six years of your life, and you have thrown them to the garbage” (2nd year medical student).
Indeed, such a negative influence also exists in the academic environment. According to the students, professors undermine family medicine when they give less importance to the clerkship in this field: “All of them say ‘You will have clerkships in gynecology, in psychiatry, and so on, and it will be great’. And in family medicine, they say it is not necessary; if you have that interest, you can go to a community health centre and ask a family physician if you can stay with him or her during the summer” (6th year medical student).
DiscussionFamily physicians currently constitute 38.1% of physicians in the Spanish National Health Care Service.22 In addition to this low percentage in relation to international standards,23 there has been a clear decline in interest in this specialty among medical students since 2005, according to the positions in family medicine residency that have remained unfulfilled over these last 4 years. This situation combined with, among other features, the high average age of current practicing family physicians and the feminization of the profession, have supported the recent prediction that family medicine will be a medical specialty with higher deficit in Spain by 2025.22
In such a context, the aim of the present investigation has been to explore Spanish medical students’ thoughts and beliefs with regard to family medicine (i.e. reputation), and how their ideas and attitudes about this medical practice have an influence on their career choice (i.e. identification). Consistent evidence suggests that countries with high-quality primary health care systems produce superior individual and population health levels.24 Family physicians are key players of front-line level of care, in which they accomplish an important set of core competencies.25 Paradoxically both 2nd and 6th year medical students participating in our study view the practice of family medicine as monotonous, superficial, and lacking intellectual stimuli. A plausible interpretation of this paradox is twofold: on one hand, students begin their undergraduate medical training with an existing distorted and negative picture of the practice of family medicine. Such reputation results from their interactions with family, relatives, and other lay people, which materialize their perception of loss of professional value of this medical activity at the health care system and societal levels. On the other hand, this diminishing reputation of the practice of family medicine is not challenged during their undergraduate training; on the contrary, our results confirm its reinforcement through student interaction with academic faculties, who privilege medical specialties associated with mastering particular medical technologies in a hospital environment.
Indeed, the trainees’ negative view of the practice of family medicine appears to be sustained by misconceptions about the type of knowledge and skills necessary to be a family physician. For instance, students assimilate ‘broad’ and ‘comprehensive’ knowledge with ‘weak’ medical wisdom, ‘gatekeeper’ and ‘care coordinator’ functions (mainly developed for an elderly clientele) with a lack of medical expertise, and consider that advances in medical knowledge happen in ‘organ-’ or ‘disease-based’ specialties. Accordingly, students display a clear detachment from a medical specialty with such a bad reputation, and consider it afterwards an ‘unattractive career path’.6,26 This has also been reported in other contexts. For instance, as noted in Norway by Albuma and Weestinb27: “[…] low prestige scores are given to diseases and specialties associated with chronic conditions having no specific bodily location with less visible treatment procedures, and with elderly patients”.
Having said this, and according to students’ statements, their misconceptions are mostly the product of ignorance in the discipline that, in turn, appears to be reinforced by the current difficult conditions of the practice for family physicians in the Spanish health care context,28,29 and a medical training environment in which family medicine is not supported as an academic discipline. If the practice of family medicine constitutes a valuable field of medical care for the sake of individuals and populations, in current times as well as in years to come,30,31 then there is room for reconstructing a better reputation of the profession, particularly acting in the two aforementioned contexts.32,33 In this sense, changes in medical curriculum that favour exposure of medical trainees to the content of family medicine and good role models in the early stages of their undergraduate studies have already been documented.34 Furthermore, the development of MSc and PhD academic programs could foster, sustain, and legitimize the generation of specific knowledge of this medical discipline, e.g. clinical management of adult patients suffering from multimorbidities.35 At the same time, it is also crucial to improve labour conditions of family physicians in the health care system. As noted by Martin Zurro36 in relation to the Spanish context: “If the students know and have contact with a family medicine practice and primary health care in which professionals are poorly motivated and encouraged, operate in unsatisfactory work environments, and have limited possibilities of professional and personal development, then the perception of these circumstances will increase the mismatch.” The examination of academic teachers’ view of family medicine, and ultimately the results of the cross-case analysis of this international study will further help understand and explain the complex phenomenon of medical students’ declining interest in family practice.
A number of positions in family medicine residency have remained consistently unfilled in Spain since 2005. If this trend is maintained, and in combination with other phenomena, such as current average age of practicing family physicians and feminization of the profession, family medicine risks becoming the medical specialty with the highest deficit in Spain by 2025.
What this study addsFamily medicine practice has a low reputation among medical students already at the early stages of their academic training, because of the perception of being viewed as monotonous, superficial, and lacking intellectual stimuli.
This view is reinforced during undergraduate training in academic centres, where specialties associated with medical technology practiced in hospital environments are privileged.
The inclusion of family medicine in the medical curriculum, the exposure to good family medicine role models, and policy decisions and actions that improve family medicine prestige and working conditions in the health care system are crucial to modify the negative student view of family medicine as a profession.
This work has been supported by the research grants of Sofia Lopez-Roig and M. Angeles Pastor from the Valencia Government (Dirección General de Política Científica, Consellería de Educación: BEST/2009/061 and BEST/2009/062), Spain, for a 2-month period as Visiting Professors at the Department of Family Medicine, Area of Health Services and Policy Research, Faculty of Medicine, McGill University. It has also been partly funded by the Canadian Institutes for Health Research (CIHR Operating Grant MOP-85044), Canada, as well as by the Fonds pour la recherché en santé du Quebec(FRSQ) Chercheur-boursier Junior 2 to Charo Rodríguez.
We would like first to thank the medical students who agreed to share with the researchers their thoughts and beliefs about family medicine for this study, through their participation in the focus groups. We would like to thank faculty and administrative staff of the Department of Family Medicine, McGill University, for the warmest welcome given to the first two authors during their period as Visiting Professors, in particular to the Head of the Department, Dr. Martin Dawes, and administrative and research officers Rosa Coppola and Bryce Mansell. Finally, the authors are very grateful for the verbatim transcription work of Irene Portilla and Patricia Sánchez.
Members of the international team are Charo Rodríguez, Pierre-Paul Tellier, and Emmanuelle Bélanger (Canada), Gwenola Levasseur, Francois-Xavier Schweyer, and Sandrine Huge (France), Sofía López-Roig and M. Angeles Pastor-Mira (Spain), and Teresa Pawlikowska and Edward Peile (United Kingdom).