General practitioners (GP) in Spain do not have access to rapid tests and adherence to guidelines is usually suboptimal. The aim of the study is to evaluate the estimated number of antibiotics that could have been saved if GPs had appropriately used these tests and had followed the guidelines.
DesignObservational study.
SettingPrimary care centres from eight Autonomous Communities in Spain.
ParticipantsGPs who had not participated in previous studies on rational use of antibiotics.
InterventionGPs registered all the cases of pharyngitis and lower respiratory tract infections (LRTI) during 15 working days in 2015, by means of a 47-item audit.
Main measurementsActual GPs’ antibiotic prescription and estimated number of antibiotics that could have been saved according to recent guidelines.
ResultsA total of 126 GPs registered 1012 episodes of pharyngitis and 1928 LRTIs. Antibiotics were given or patients were referred in 497 patients with pharyngitis (49.1%) and 963 patients with LRTI (49.9%). If GPs had appropriately used rapid antigen detection tests and C-reactive protein tests and had strictly followed current guidelines, antibiotics would have been given to 7.6% and 15.1%, respectively, with an estimated saving of 420 antibiotics in patients with sore throat (estimated saving of 84.5%; 95% CI: 81.1–87.4%) and 672 antibiotics in LRTIs (estimated saving of 69.8%,95% CI: 67.1–72.5%).
ConclusionsGP adherence to guidelines and a correct introduction of rapid tests in clinical practice in Spain could result in a considerable saving of unnecessary prescription of antibiotics in pharyngitis and LRTIs.
Los médicos de familia (MF) en España no tienen acceso a pruebas rápidas y la adherencia a las guías clínicas es subóptima. El objetivo del estudio es evaluar el número estimado de antibióticos que podrían ahorrarse si los MF hubiesen usado las pruebas correctamente y hubieran seguido las guías.
DiseñoEstudio observacional.
EmplazamientoCentros de atención primaria en 8 Comunidades Autónomas.
ParticipantesMF que no habían participado en estudios anteriores sobre uso racional de antibióticos.
IntervenciónLos MF registraron los casos de faringitis e infecciones del tracto respiratorio inferior (ITRI) durante 15 días en 2015, mediante un audit de 47 ítems.
Mediciones principalesPrescripción real de antibióticos realizada por los MF y antibióticos que se hubiesen ahorrado en base a las guías clínicas.
Resultados126 MF registraron 1.012 faringitis agudas y 1.928 ITRI. Se prescribieron antibióticos o fueron derivados 497 pacientes con faringitis (49,1%) y 963 con ITRI (49,9%). Si los MF hubiesen usado pruebas rápidas de detección antigénica y proteína C reactiva y hubieran seguido las directrices, se hubieran dado antibióticos al 7,6% y al 15.1%, respectivamente, con un ahorro estimado de 420 antibióticos en pacientes con faringitis (84,5%; IC 95%: 81,1-87,4%) y 672 antibióticos en pacientes con ITRI (69.8%, IC 95%: 67.1-72.5%).
ConclusionesLa adherencia de los MF a las guías clínicas y una correcta introducción de las pruebas rápidas en la práctica clínica en España podrían reducir de forma considerable la prescripción innecesaria de antibióticos en la faringitis aguda y en las ITRI.
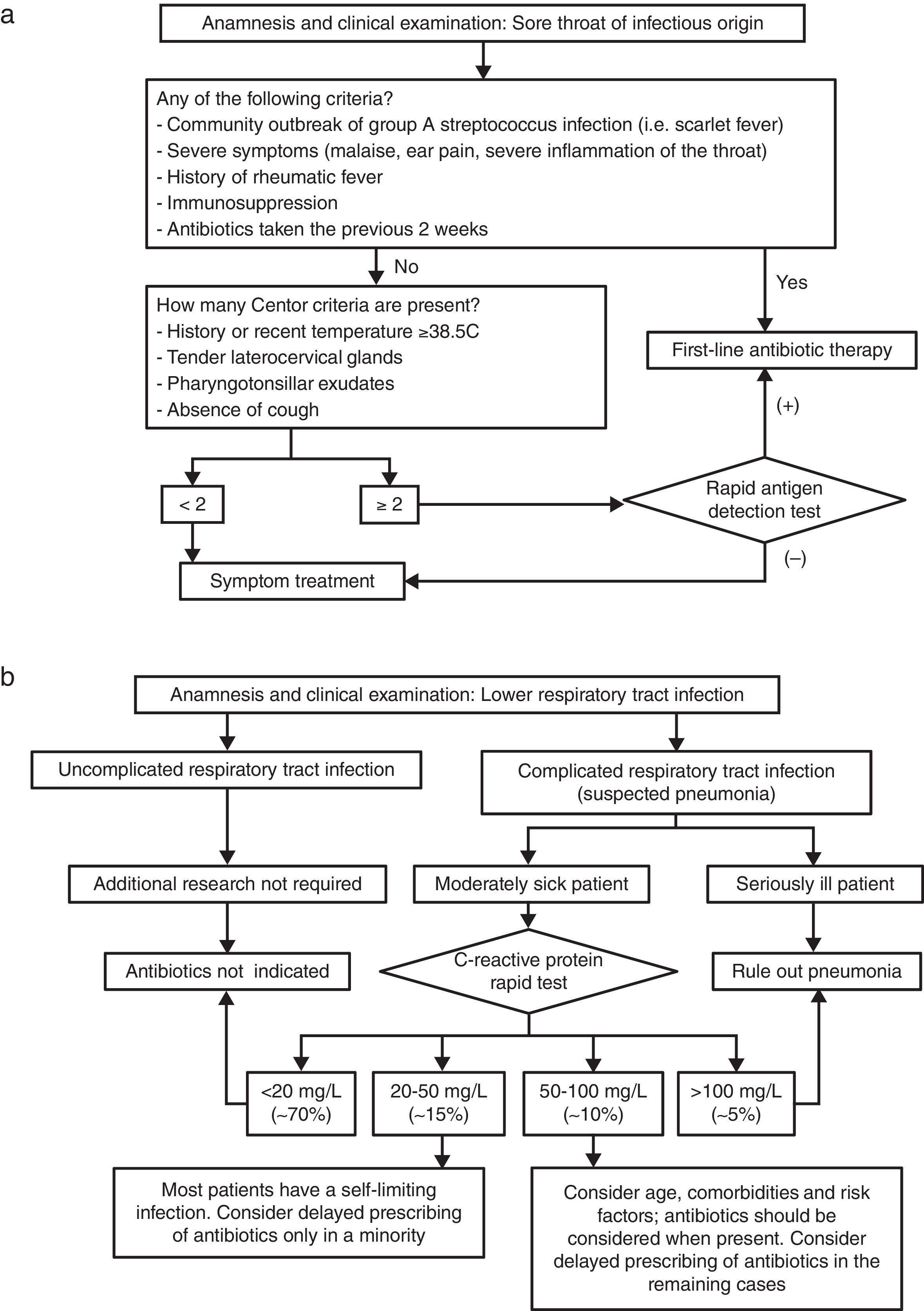
Most clinical guidelines recommend antibiotic prescribing for patients with sore throat when the infection is severe and in patients with group A β-haemolytic streptococcus (GABHS) infection.1 However, identifying patients with GABHS only on clinical grounds is difficult. Most countries recommend the use of rapid antigen detection tests (RADT) in patients with suspected streptococcal infections as this practice has been associated with a reduction of inappropriate use of antibiotics.2 Spanish guidelines recommend these tests to be performed specifically in patients with at least two Centor criteria—history of fever, tender cervical nodes, pharyngeal exudates and/or absence of cough.3 When it comes to lower respiratory tract infections (LRTI), systematic reviews have suggested that antibiotics do not make any difference in the course of influenza and modify the course of acute bronchitis only marginally.4,5 However, they are recommended in acute exacerbations of chronic obstructive pulmonary disease (COPD), mainly when purulent sputum is present and in all cases of pneumonia.5 Identifying patients with pneumonia has also shown to be challenging in primary care when it is only based on symptoms, signs and examination.6 Used as an adjunct to clinical examinations by general practitioners (GPs) the C-reactive protein (CRP) rapid test has also shown to reduce antibiotic use in these infections.7
Despite the compelling evidence about the benefits of having these rapid tests in primary care, their availability in Spanish surgeries is scarce. However, GPs in our country prescribe antibiotics in over 60% of cases of acute pharyngitis and acute bronchitis.8 Inappropriate antibiotic use has adverse medical consequences and contributes to microbial antibiotic resistance.9 We carried out a European-funded study aimed at promoting the rational use of antibiotics. In 2015 we selected a sample of GPs who had never used rapid tests in their consultations and compared the use of antibiotics with the current clinical guidelines estimating the number of antibiotics that could have been saved if GPs had appropriately used these tests and had followed the guidelines properly.
MethodsNational coordinators from each of the eight participating Autonomous Communities invited local GPs to participate. They were requested to register individuals aged 14 or older with acute pharyngitis (including acute tonsillitis) and LRTIs over a 3-week period from January to March 2015 by means of a 47-item chart providing relevant information about the infectious disease. On this sheet, the physician attending the patient noted different specific parameters of medical care, including the age and gender of the patient, the number of days with symptoms, presenting signs such as fever, cough, odynophagia, pharyngeal exudates, presence of tender cervical nodes, dyspnoea, increase in sputum volume and purulence of sputum, diagnosis (pharyngitis, acute bronchitis, influenza, acute exacerbation of chronic bronchitis or COPD, pneumonia), infection severity on a 5-item scale, performance of chest radiograph, pulse oximetry, rapid antigen detection tests and CRP rapid tests, antibiotic treatment or not, allergy or not to penicillin, whether the patient requested an antibiotic, significant comorbidities and referral to another healthcare setting.
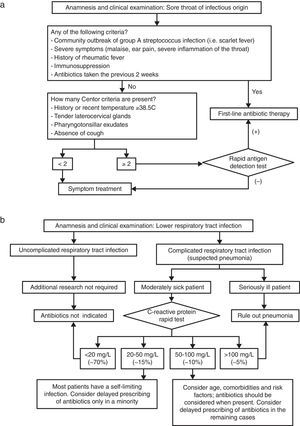
This information was compared to the recent Spanish guidelines in the case of pharyngitis3 (Figure 1a). Although our guidelines on LRTIs recommend the utilisation of CRP their use is negligible in Spain. Thus, algorithms provided in the current guidelines describe the usual practice of undertaking a thorough physical examination asking GPs to request radiological study when the suspicion of pneumonia is very likely. Therefore, we used the recent Dutch guidelines as the comparator for this study classifying patients into three different severity groups, considering the use of CRP only when there was an intermediate risk (Figure 1b).10
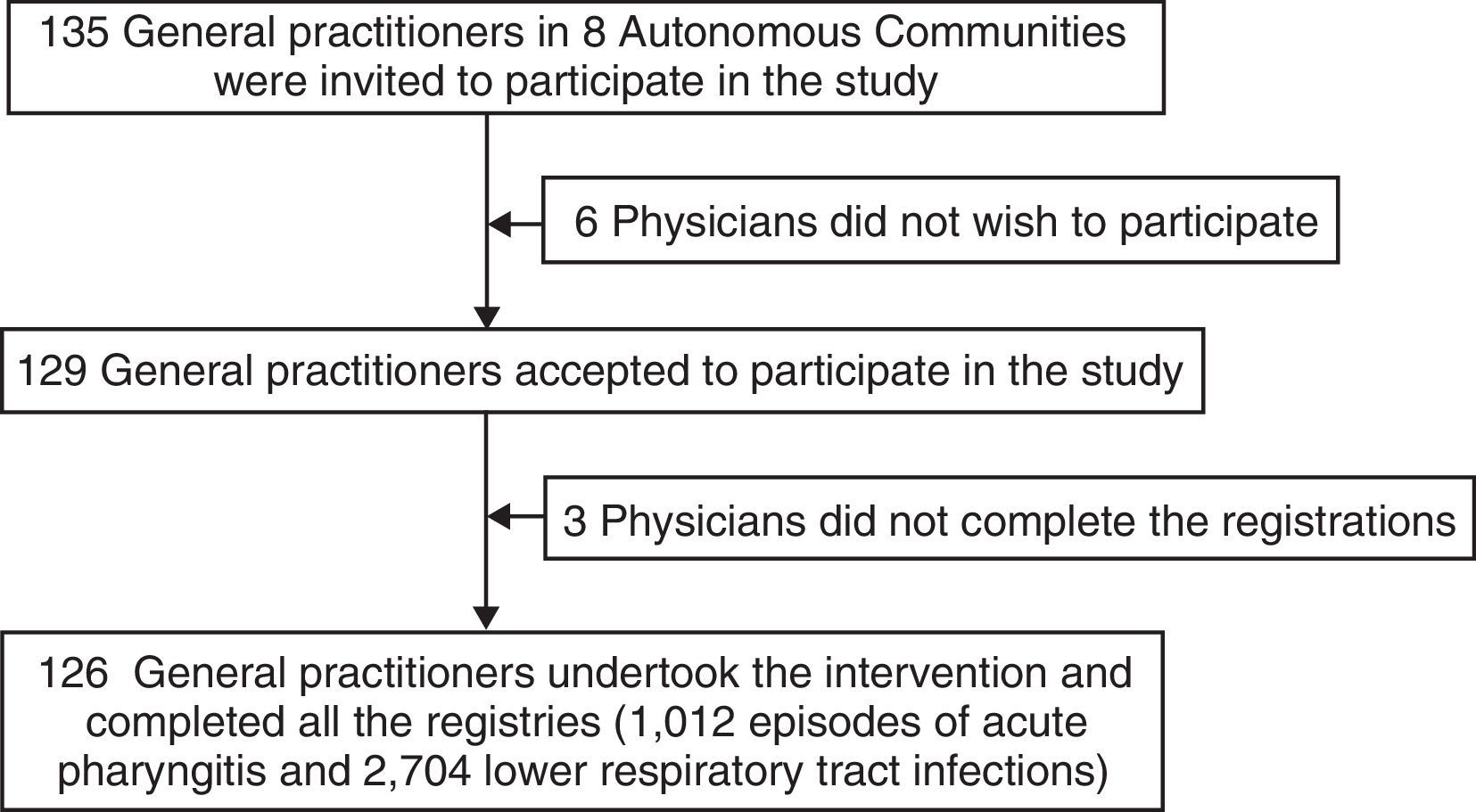
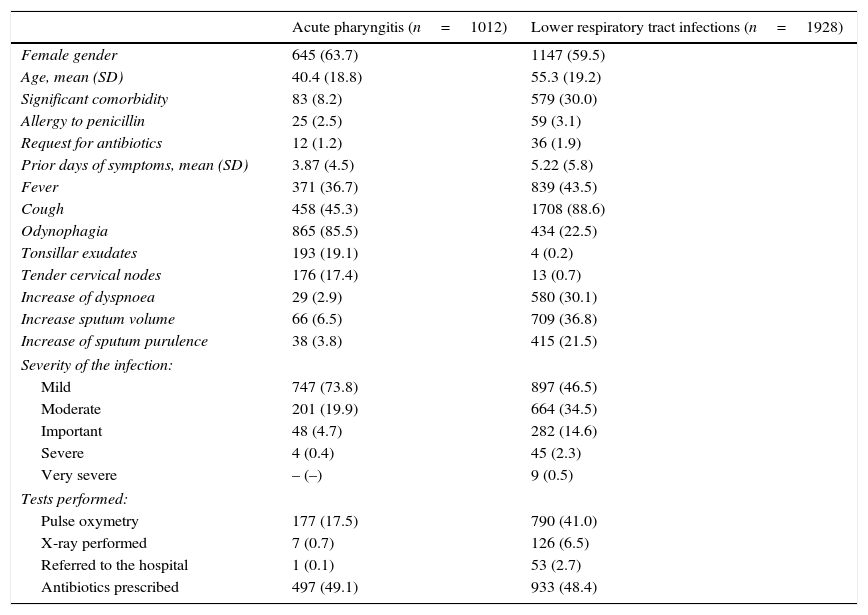
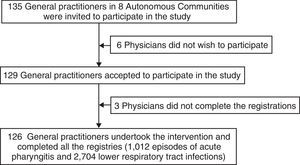
A total of 135 GPs were invited to participate in this study but 6 declined. Three GPs did not deliver the registries. At last, a total of 126 GPs registered 1012 episodes of acute pharyngitis and 1928 LRTIs. The characteristics of these patients are described in Table 1. In terms of symptoms and signs, the most frequently reported among patients with LRTIs was the presence of cough, observed in 88.6% of the cases; conversely, the leading symptom in patients with acute pharyngitis was odynophagia, found in 85.5% of the cases. Although GPs judged the severity of the infections as relatively mild, illness severity was rated higher among patients with LRTI. A total of 53 patients with LRTI were referred to hospital (2.7%).
Characteristics of the contacts with acute pharyngitis and lower respiratory tract infections. Number (%) unless otherwise specified.
| Acute pharyngitis (n=1012) | Lower respiratory tract infections (n=1928) | |
|---|---|---|
| Female gender | 645 (63.7) | 1147 (59.5) |
| Age, mean (SD) | 40.4 (18.8) | 55.3 (19.2) |
| Significant comorbidity | 83 (8.2) | 579 (30.0) |
| Allergy to penicillin | 25 (2.5) | 59 (3.1) |
| Request for antibiotics | 12 (1.2) | 36 (1.9) |
| Prior days of symptoms, mean (SD) | 3.87 (4.5) | 5.22 (5.8) |
| Fever | 371 (36.7) | 839 (43.5) |
| Cough | 458 (45.3) | 1708 (88.6) |
| Odynophagia | 865 (85.5) | 434 (22.5) |
| Tonsillar exudates | 193 (19.1) | 4 (0.2) |
| Tender cervical nodes | 176 (17.4) | 13 (0.7) |
| Increase of dyspnoea | 29 (2.9) | 580 (30.1) |
| Increase sputum volume | 66 (6.5) | 709 (36.8) |
| Increase of sputum purulence | 38 (3.8) | 415 (21.5) |
| Severity of the infection: | ||
| Mild | 747 (73.8) | 897 (46.5) |
| Moderate | 201 (19.9) | 664 (34.5) |
| Important | 48 (4.7) | 282 (14.6) |
| Severe | 4 (0.4) | 45 (2.3) |
| Very severe | – (–) | 9 (0.5) |
| Tests performed: | ||
| Pulse oxymetry | 177 (17.5) | 790 (41.0) |
| X-ray performed | 7 (0.7) | 126 (6.5) |
| Referred to the hospital | 1 (0.1) | 53 (2.7) |
| Antibiotics prescribed | 497 (49.1) | 933 (48.4) |
SD, standard deviation.
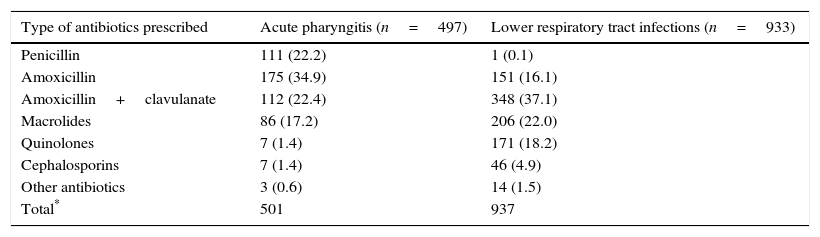
Antibiotics were prescribed to 497 patients, accounting for 49.1% of the cases. The antibiotic most commonly prescribed was amoxicillin, with 34.9% of the cases in whom antibiotics were given, followed by amoxicillin+clavulanate and penicillin V (Table 2). A total of 297 patients had no Centor criteria, 330 presented only one, 236 had two, 104 had three and 45 presented the four criteria. Antibiotics were given to 26.9%, 32.4%, 75.6%, 91.3% and 91.1% of the cases, respectively. Four patients had a severity score greater than 3. RADTs should have been performed in non-severe patients with two or more Centor criteria (in 383 cases, 37.8%). Assuming that 18–22% of patients with at least a Centor score of two have a true group A β-haemolytic streptococcus infection on the basis of previous studies,3 antibiotics should have been prescribed in only 77 patients (7.6% of all the cases of sore throat and two or more Centor criteria). In addition, 185 antibiotics prescribed in non-severe patients with less than two Centor criteria were inappropriately given. So, if GPs had appropriately used RADTs and had strictly followed current guidelines, up to 84.5% of the antibiotics prescribed could have been saved (95% CI: 81.1–87.4%).
Antibiotics prescribed to the contacts with acute pharyngitis and lower respiratory tract infections. Number (%).
| Type of antibiotics prescribed | Acute pharyngitis (n=497) | Lower respiratory tract infections (n=933) |
|---|---|---|
| Penicillin | 111 (22.2) | 1 (0.1) |
| Amoxicillin | 175 (34.9) | 151 (16.1) |
| Amoxicillin+clavulanate | 112 (22.4) | 348 (37.1) |
| Macrolides | 86 (17.2) | 206 (22.0) |
| Quinolones | 7 (1.4) | 171 (18.2) |
| Cephalosporins | 7 (1.4) | 46 (4.9) |
| Other antibiotics | 3 (0.6) | 14 (1.5) |
| Total* | 501 | 937 |
The 126 GPs prescribed antibiotics or referred patients to hospital in 963 cases (49.9%). An antibiotic was given in 933 patients (48.4%). The leading antibiotic was amoxicillin+clavulanate which was prescribed in 348 patients (37.1%), followed by macrolides (22%), quinolones (18.2%), and amoxicillin (16.1%) (Table 2).
A total of 1076 infections were diagnosed with acute bronchitis, 542 influenza, 247 acute exacerbations of chronic bronchitis or COPD and 63 had pneumonia. A total of 777 patients presented an uncomplicated respiratory tract infection for which antibiotics should have not been prescribed. However, GPs gave them in 160 (20.6%) of these cases. A total of 157 patients were considered as seriously ill and should have all received antibiotics or been referred to a hospital setting. However, antibiotics were withheld and patients not referred to hospital in 5.7% of these cases. A total of 993 patients had an intermediate risk and antibiotics were prescribed in 655 (66%) of the cases; all these patients except 53 with a severity score greater than 3 should have been tested with the aid of the CRP rapid test as stated by current guidelines (602 patients, 31.2% of all the LRTI). Assuming that 70% of the CRP determinations in this population have levels less than 20mg/L and 15% have concentrations ranging from 20 to 50mg/L according to medical literature, only 90 should have been treated with these drugs.7 It means that if GPs had followed the guidelines appropriately, antibiotics should have only been given to 291 patients (15.1%), with an estimated saving of 69.8% (95 CI: 67.1–72.5%).
DiscussionThe main conclusion of this study is that up to 84.5% of the antibiotics given to patients with pharyngitis and 69.8% given to LRTI patients can have been saved with the proper use of rapid tests. However, the participating GPs had seldom or never used either of the two rapid tests mentioned in this study and had not previously participated in any other study on the rational use of antibiotics. One of the limitations of the present study is that GPs participated on a voluntary basis and their prescribing habits may not represent the average use of antibiotics in our country.11 GPs who are more interested in research prescribe more appropriately than GPs in general, and this fact can explain why the antibiotic prescribing rate observed in the present study was slightly lower than 50% in both infections. A registration such as that used in our study might not have contained all the variables needed for making a therapeutic decision, but the most important variables were included, and the information provided was sufficient for further comparison with the clinical guidelines. The strength of our study is its large sample size with detailed documented consultations, enabling us to compare this information with that provided in the guideline recommendations.
The costs related to the antibiotics saved were not calculated in this study. Neither did we consider the costs of the rapid tests, days off work and visits to the healthcare services. Another limitation of the study is the fact that we considered a hypothetical situation of having access to point-of-care tests and these tests had been appropriately used by GPs who had followed the existing guidelines. However, evidence clearly states that guidelines adherence by GPs in respiratory tract infections is not optimal, either in terms of when antibiotics are indicated or with the usage of first-line antibiotics.12,13 In the present study, the types of antibiotics prescribed reflect that guidelines are scarcely used in our country since penicillin, which is considered the first-choice drug for GABHS infection, was the third antibiotic most frequently given to patients with acute pharyngitis whereas amoxicillin and clavulanic acid were the most commonly used in LRTI, when they are only recommended as first-choice drugs in acute exacerbations of COPD but not in other respiratory tract infections. Oddly enough, macrolides accounted for 22% of the antibiotics prescribed in patients with LRTI, and amoxicillin, considered as the first-line antibiotic in most of the LRTIs ranked fourth in our study.
According to the current clinical guidelines RADT should have been used in 37.8% of the episodes of acute pharyngitis and CRP concentrations should have been determined in 31.2% of the LRTIs. Antibiotics should have only been prescribed with positive RADT results and with CRP levels greater than 50mg/L as well as in all severe patients. Likewise, antibiotics should have been withheld in patients with less than two Centor criteria, in all the uncomplicated LRTIs and in the cases with CRP levels less than 20mg/L. Taking all these requisites into account the saving of antibiotics would have been considerable; however, both the utilisation of rapid tests in the countries where these tests have widely been used over the last years and the no utilisation of antibiotics in case of negative results are far from being optimal.14 Notwithstanding, considering the weaknesses of the study and their inference insight this paper shows that the correct introduction of rapid tests in clinical practice in Spain could result in a considerable saving of unnecessary antibiotic prescribing.
- •
Antibiotics are often overprescribed for respiratory tract infections.
- •
The use of rapid tests in primary care has been shown to be useful in reducing the unnecessary prescription of antibiotics in respiratory tract infections.
- •
We carried out this study aimed at knowing what the estimated saving of antibiotics in pharyngitis and lower respiratory tract infections would have been if general practitioners had correctly used rapid antigen detection tests in cases of pharyngitis and C-reactive protein in cases of lower respiratory tract infections with intermediate risk.
- •
Both point-of-care tests should have been used in about one third of the patients with these infections and their appropriate use on a regular basis would result in a considerable saving of antibiotic prescribing.
Study funded by TRACE (Translational Research on Antimicrobial resistance and Community-acquired infections in Europe).
Conflicts of interestCL reports having a grant from the Fundació Jordi Gol i Gurina for a research stage at the University of Cardiff. He also reports receiving research grants from the European Commission (Sixth & Seventh Programme Frameworks and Horizon 2020), Catalan Society of Family Medicine, and Instituto de Salud Carlos III. The other authors have nothing to declare.
Happy Audit Study Group: Local coordinators: Andalucía: Juan de Dios Alcántara, Yanina Maldonado. Baleares: Susana Munuera, Jana Ribas. Canarias: Gloria Guerra. Galicia: Marina Cid. Madrid: Manolo Gómez. Rioja: Jesús Ortega. Asturias: Guillermo García. Valencia: Vicenta Pineda, M, José Monedero.
We wish to acknowledge the 126 GPs who voluntarily participated in the study: Andalucía: Ainhoa Mestriatua, Amalia Filella, Antonio Hernández, Antonio Paniagua, Auxiliadora Sanchis, Beatriz Luque, Eduardo Ávila, Guillermo Velázquez, Idoioa Arrillaga, Irene Padial, M. Antonia Máximo, M. Jesús Remesal, Marta Bernal, Mercedes Moreno, M. Encarnación Peláez, Pablo Cabezas, Pedro Fernández-Nieto, Pilar Carretero, Rosario Serrano, Vanessa Parra. Baleares: Aberlado Corrales, Adriano Mayrata, Blanca Martínez, Daniel Bestard, Etel Oliver, Gabriel Moragues, F. Javier Rezola, Joana Tortella, Lucia Ugarriza, Magdalena Servera, Maite Corredor, Margarita Fornés, Mercedes Gutiérrez, Miguel Román, Natalia Serrano, J. Francisco Palmer, Salvador J. Gestoso, Silvia Vega, Susana Pons, Prado García. Canarias: Caridad Sánchez, Margarita García, M. Elena Martín, Marta Moreno, Ricardo Koch. Galicia: Coral Díez, Elena Lorenzo, Esther López, J. Antonio Gómez, Luis Fuciños, J. Luis López, Lucía Rodríguez, M. Esther González, M. Jesús Colas, M. Pilar Pintos, M. Teresa Ríos. Madrid: Adela Moreno, Álvaro García, Ana Ibarra, Ángeles Lagos, M. Arantzazu Murciano, Ascensión Lázaro, Belén de la Fuente, Blanca Matilla, Cristina Moral, M. Elena Gerez, M. Elena Hermida, M. Elena Rodríguez, Gema García, Gema Val, Guillermina López, Irmina Saldaña, Jaime Marín, Juana M. Torres, Laura Santos, M. José Lucena, M. Asunción Rosado, M. Mar Sánchez, Rosa M. González, M. Teresa Cobos, M. Mar García, M. Eugenia López, M. Jesús Ferrer, Patricia Navarro, Renata Muñoz, Rocío Susana Ruiz, Rosario López, Silvia de las Heras, Teresa Mazarro. Rioja: Ana M. Gómez, Ana M. Vázquez, Ascensión Aicua, Diego Beni, Elvira Moreno, M. Ángeles Espeso, M. Carmen Aurensanz, M. José Palomo, Nieves Calavia, Sabino Ornia. Asturias: Alfonso García, Alicia Rodríguez, Cristina Pérez, Herminia Menéndez, Juan Carlos Bango, Azucena Deopatria, J. Ignacio Rodríguez-Arias, Leonor Fuentes, Teresa Díaz, Pablo Belderraín, Rocío Fernández, Rosa Rodríguez, Rubén Villa. Valencia: Adela Moreno, Amparo Meneu, Ángeles Pérez, Belén Persiva, Blanca Folch, Carmen Hernández, Helena Molina, Juan Alamar, M. Pilar Roca, M. Luisa Tregón, Nuria Mallén, Rosa Carrión, M. Teresa Amorós, Teresa Chirivella.