Atherogenic dyslipidemia is an important risk factor for cardiovascular disease. We aim to determine atherogenic dyslipidemia prevalence in primary care patients at moderate-very high cardiovascular risk and its associated cardiovascular risk perception in Spain.
MethodsThis cross-sectional study included 1137 primary care patients. Patients had previous cardiovascular disease, diabetes mellitus, SCORE risk ≥3, severe hypertension or dyslipidemia. Atherogenic dyslipidemia was defined as low HDL-C (<40mg/dL [males], <50mg/dL [females]) and elevated triglycerides (≥150mg/dL). A visual analog scale was used to define a perceived cardiovascular disease risk score.
ResultsMean age was 63.9±9.7 years (64.6% males). The mean BMI was 29.1±4.3kg/m2, and mean waist circumference 104.2±12.7cm (males), and 97.2±14.0cm (females). 29.4% were smokers, 76.4% had hypertension, 48.0% were diabetics, 24.7% had previous myocardial infarction, and 17.8% peripheral arterial disease. European guidelines classified 83.6% at very high cardiovascular risk. Recommended HDL-C levels were achieved by 50.1% of patients and 37.3% had triglycerides in the reference range. Target LDL-C was achieved by 8.8%. The overall atherogenic dyslipidemia prevalence was 27.1% (34.1% in diabetics). This prevalence in patients achieving target LDL-C was 21.4%. Cardiovascular risk perceived by patients was 4.3/10, while primary care physicians scored 5.7/10.
ConclusionsWhen LDL-C levels are controlled, atherogenic dyslipidemia is more prevalent in those patients at highest cardiovascular risk and with diabetes. This highlights the importance of intervention strategies to prevent the residual vascular risk in this population. Both patients and physicians underestimated cardiovascular risk.
La dislipidemia aterogénica representa un factor de riesgo importante de enfermedad cardiovascular. Se pretende determinar la prevalencia de dislipidemia aterogénica en pacientes de atención primaria con riesgo cardiovascular de moderado a muy alto y la percepción de riesgo cardiovascular asociado en España.
MétodosEstudio transversal que incluyó 1.137 pacientes de atención primaria. Los pacientes presentaban enfermedad cardiovascular previa, diabetes mellitus, SCORE ≥3, hipertensión arterial severa o dislipidemia. La dislipidemia aterogénica se definió como C-HDL bajo (<40mg/dl [hombres], <50mg/dl [mujeres]) y triglicéridos elevados (≥150mg/dl). Para definir la puntuación de percepción de riesgo de enfermedad cardiovascular se utilizó una escala visual analógica.
ResultadosLa edad media fue de 63,9±9,7 años (64,6% hombres). El IMC promedio fue de 29,1±4,3kg/m2, y la media del perímetro de la cintura de 104,2±12,7cm (hombres) y 97,2±14,0cm (mujeres); el 29,4% eran fumadores, el 76,4% hipertensos, el 48,0% diabéticos, el 24,7% tenían antecedentes de infarto de miocardio y el 17,8% enfermedad arterial periférica. El 83,6% se clasificaron como pacientes de muy alto riesgo cardiovascular según las guías europeas. El 50,1% de los pacientes alcanzaron los niveles recomendados de C-HDL y el 37,3% tenían los triglicéridos dentro del rango. El 8,8% consiguieron niveles objetivo de C-LDL. La prevalencia general de dislipidemia aterogénica fue del 27,1% (34,1% en diabéticos). Esta prevalencia en los pacientes que alcanzaron niveles objetivo de C-LDL fue del 21,4%. El riesgo cardiovascular percibido por los pacientes fue de 4,3/10, mientras que sus médicos de atención primaria puntuaron un 5,7/10.
ConclusionesCuando se controlan los niveles de C-LDL la dislipidemia aterogénica es más prevalente en aquellos pacientes con mayor riesgo cardiovascular y diabéticos, lo que pone de manifiesto la importancia de las estrategias de intervención para prevenir el riesgo vascular residual en esta población. Tanto pacientes como médicos subestimaron el riesgo cardiovascular.
Atherogenic dyslipidemia involves decreased levels of high-density lipoprotein cholesterol (HDL-C) and increased triglycerides1 and is associated to qualitative alteration in low-density lipoprotein colesterol (LDL-C) which are smaller and denser. This condition has been associated to increased cardiovascular risk and is perceived as highly prevalent in the primary care setting. It is typically seen in patients with obesity, metabolic syndrome, insulin resistance, and type 2 diabetes mellitus (type 2 DM).2,3 While several epidemiological studies have examined the prevalence of lipid abnormalities, most have focused only on total cholesterol (TC) levels. A large study conducted in 2006 on working people undergoing routine check-up in Spain obtained a prevalence of dyslipidemia of 64% (TC ≥200mg/dL, LDL-C ≥160mg/dL, triglycerides ≥200mg/dL, or HDL-C <40/50mg/dL), and TC ≥240mg/dL of 15%.4 Vegazo et al. in the same year found that one out of four patients who attended outpatient clinics of the Spanish health service had been diagnosed with dyslipidemia without diagnostic specific reference levels specified.5 Results of a metaanalysis including 47 cross-sectional studies in Spain published between 1990 and 2003 on the main cardiovascular risk factors prevalence showed that 23% of middle-aged adults had TC ≥250mg/dl and 50–60% had TC ≥200mg/dL.6 In line with these results, a more recent study on 11,554 patients conducted in Spain found that about 50% had hypercholesterolemia (TC ≥200mg/dL or drug treatment).7
Numerous studies have shown a continued and gradual relationship between serum cholesterol, mainly LDL-C, and total mortality due to ischemic heart disease,8–14 as well as the association of LDL-C reductions and European guidelines recommend LDL-C below 100 or 70mg/dl for high and very high cardiovascular risk patients.
Moreover despite obtaining LDL-C targets, the number of new events remains inappropriately high. This situation is referred to residual cardiovascular risk and, apart from non-lipid conditions, lipoprotein alterations beyond LDL-C concentrations could have a role, particularly low HDL-C and high triglycerides (atherogenic dyslipidemia). Two subgroup analyses of two studies identify atherogenic dyslipidemia subgroup as a group of patients that could obtain benefit of correcting the lipoprotein abnormalities,15,16 suggesting that a good global control of dyslipidemia is essential in prevention of cardiovascular disease. The objective of this study was to assess the prevalence of atherogenic dyslipidemia among adult patients at moderate to high cardiovascular risk seen in primary care, and to examine grade of control on serum lipid components and patients’ and physicians’ perceptions of cardiovascular risk.
Patients and methodsThis was an epidemiological, cross-sectional and multicenter study conducted in Spanish population with moderate to very high cardiovascular risk. Patients were consecutively selected from primary care centers between June 2011 and November 2011 with the participation of 432 investigators. The investigators and sites were selected from every Spanish region ensuring the representativeness of each one, weighting the population size of each region and balancing the civic and rural origin as well as the proportion between southern and northern regions. The study included patients ≥18 years of age who fulfilled at least one of the following criteria 1: previous cardiovascular disease (coronary event, cerebrovascular event or peripheral arterial disease); (2) type 2 DM or type 1 DM with microalbuminuria; (3) hypertension, dyslipidemia, smoking or other risk factors (Systematic Coronary Risk Evaluation [SCORE] risk≥3); or (4) severe forms of hypertension or dyslipidemia (hypertension stage 2–3, LDL-C >190mg/dL, triglycerides >500mg/dL). Exclusion criteria were patients with chronic inflammatory diseases, neoplastic diseases, hepatic cirrhosis or alcohol abuse and thyroid disease. The study was approved by the Ethics Committee of Hospital Clínic (Barcelona, Spain), and all enrolled patients provided signed informed consent.
The variables collected included anthropometric and sociodemographic data (age, gender, menopausal status, weight, height, body mass index, and waist circumference), blood pressure, SCORE, and clinical history at study inclusion (hypertension, diabetes mellitus, hyperlipidemia, cardiovascular disease, microalbuminuria and other relevant diseases). Participants were also interviewed to determine their smoking, alcohol and exercise habits. Laboratory determinations included: TC, triglycerides, HDL-C, LDL-C, non-HDL-C, blood glucose and hemoglobin A1c levels. Perception of cardiovascular risk, either in patient and the physician, was given by marking a 100mm visual analog scale from 0 (absence of risk) to 100 (maximum risk). Data were also recorded on whether the patient was taking any lipid-modifying drugs without specifying the medication.
Cardiovascular risk was considered to be moderate if SCORE ≥1% to ≤5%, high if SCORE >5% to <10% or DM without other risk factors, and very high when patients had a SCORE >10%, DM with microalbuminuria or associated risk factors, or previous cardiovascular disease (coronary event, cerebrovascular event, peripheral arterial disease). Atherogenic dyslipidemia was defined by high triglyceride levels (>150mg/dL) and low HDL-C (<40 in men and <50mg/dL in women). LDL-C was assumed to be well-controlled if the LDL-C was <115mg/dL, <100mg/dL and <70mg/dL in moderate, high, and very high risk patients, respectively. Considering that 5% of the patients included initially would not be valid for the final analysis, the sample size was estimated to be 1728 patients (alpha error: 0.05%; precision: 2.1%) to calculate the prevalence of dyslipidemia based on the data of mix hiperlipidemia of 25.7% reported by Vegazo et al.5 Quantitative variables were analyzed with measures of central tendency (mean, median) and dispersion (standard deviation, 25th percentile, 75th percentile, minimum, and maximum). Qualitative variables were studied with frequencies and percentages of each of the possible responses. The 95% confidence interval (CI) was calculated for the variables of interest. Means were compared with the Student's t test for independent data. Quantitative data that did not follow a normal distribution were analyzed with the Mann–Whitney non-parametric test, and possible associations between the qualitative variables were studied with the χ2 test. Multiple logistic regression analysis was performed to quantify the association between cardiovascular risk perceived by patients and each of the cardiovascular risk factors. Correlation indexes to assess the patient's perception of the risk and the clinical objectives (Pearson or Spearman depending on variable distribution) were calculated. A p-value less than 0.05 was considered significant. All analyses were performed with the Statistical Package for the Social Sciences (SPSS) version 17.
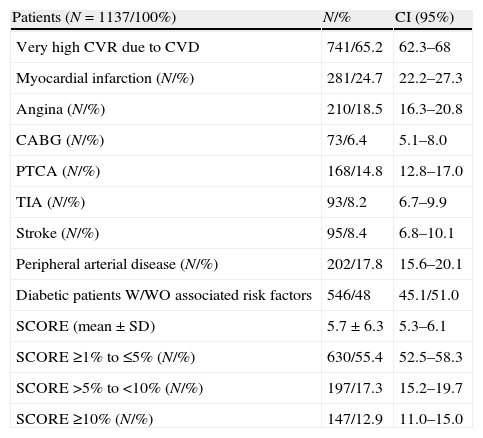
ResultsPatient characteristicsOf the 1322 patients enrolled in the present study, 185 were excluded for unmet selection criteria, resulting in a final sample of 1137 evaluable patients. Table 1 shows the most relevant sociodemographic and clinical characteristics of the included patients.
Socio-demographic and clinical characteristics of the evaluable patients.
| Patients (N=1137/100%) | CI (95%) | |
| Age (years) (mean±SD) | 63.9±9.7 | 63.3–64.5 |
| Men (N/%) | 734/64.6 | 61.7–67.3 |
| Smoking (N/%) | 334/29.4 | 26.7–32.1 |
| Former smoking (N/%) | 350/30.8 | 28.1–33.6 |
| BMI (kg/m2) (mean±SD) | 29.1±4.3 | 28.8–29.4 |
| Men: waist circumference (cm) (mean±SD) | 104.2±12.7 | 103.2–105.2 |
| Women: waist circumference (cm) (mean±SD) | 97.2±14.0 | 95.6–98.8 |
| Hypertension (N/%) | 869/76.4 | 73.9–78.9 |
| SBP (mmHg) (mean±SD) | 140.5±17.3 | 139.5–141.5 |
| DBP (mmHg) (mean±SD) | 81.3±10.8 | 80.6–82.0 |
| Treated for hypertension N/%) | 824/94.8 | 93.1–96.2 |
| DM (N/%) | 546/48.0 | 45.1–51.0 |
| Type 2 DM (N/%) | 490/43.1 | 40.2–46.0 |
| Glucose (mg/dL) (mean±SD) | 140.6±45.8 | 136.7–144.5 |
| Hb1Ac (%)(mean±SD) | 7.2±1.2 | 7.1–7.3 |
| Treated for Type 2 DM (N/%) | 466/95.1 | 92.8–96.8 |
BMI, body mass index; CI, confidence interval; DBP, diastolic blood pressure; DM, diabetes mellitus; SBP, systolic blood pressure.
As shown in Table 2, myocardial infarction was the most frequently suffered coronary event (24.7%). Previous cerebrovascular events (transitory ischemic attack and stroke) were reported by less than 10% of patients and 17.8% had peripheral arterial disease. Approximately half of the patients had SCORE ≥1% to ≤5%. Nevertheless, 83.6% of all patients were classified as having very high cardiovascular risk.
Determinants of cardiovascular risk level of study patients.
| Patients (N=1137/100%) | N/% | CI (95%) |
| Very high CVR due to CVD | 741/65.2 | 62.3–68 |
| Myocardial infarction (N/%) | 281/24.7 | 22.2–27.3 |
| Angina (N/%) | 210/18.5 | 16.3–20.8 |
| CABG (N/%) | 73/6.4 | 5.1–8.0 |
| PTCA (N/%) | 168/14.8 | 12.8–17.0 |
| TIA (N/%) | 93/8.2 | 6.7–9.9 |
| Stroke (N/%) | 95/8.4 | 6.8–10.1 |
| Peripheral arterial disease (N/%) | 202/17.8 | 15.6–20.1 |
| Diabetic patients W/WO associated risk factors | 546/48 | 45.1/51.0 |
| SCORE (mean±SD) | 5.7±6.3 | 5.3–6.1 |
| SCORE ≥1% to ≤5% (N/%) | 630/55.4 | 52.5–58.3 |
| SCORE >5% to <10% (N/%) | 197/17.3 | 15.2–19.7 |
| SCORE ≥10% (N/%) | 147/12.9 | 11.0–15.0 |
CABG, coronary artery bypass graft; CI, confidence interval; PTCA, percutaneous transluminal coronary angioplasty; TIA, transitory ischemic attack.
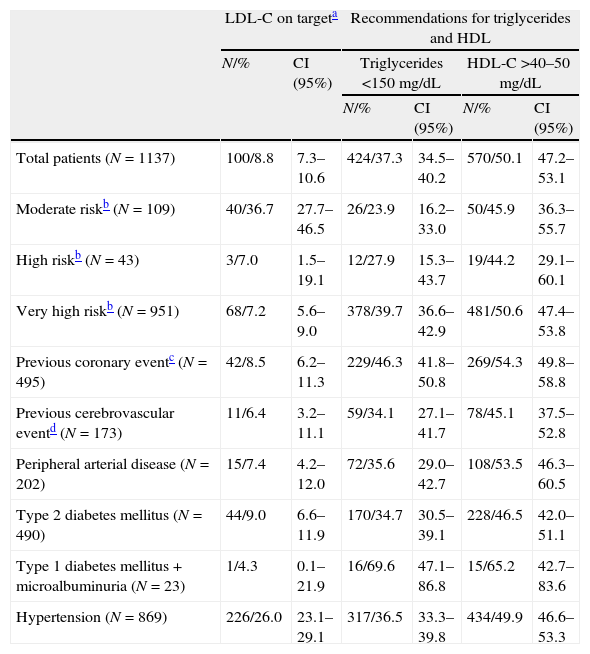
Percentages of patients with controlled levels for each lipoprotein component according to their cardiovascular risk are presented in Table 3. Target LDL-C levels were achieved in 8.8% of all patients (Table 3). However, LDL-C control was much lower in patients with high or very high cardiovascular risk and among those with cardiovascular events or DM, without exceeding 10% in any case. Overall, there was a higher percentage of patients achieving recommended levels of triglycerides (<150mg/dL) and HDL-C (>40–50mg/dL), although in most cases less than half of the patients were controlled. In addition, the secondary goal for non-HDL-C (<130mg/dL) was only achieved by 5.4%, 2.3% and 4.6% of very high, high and moderate risk patients, respectively.
Control of lipid parameters in the study patients according to their cardiovascular risk.
| LDL-C on targeta | Recommendations for triglycerides and HDL | |||||
| N/% | CI (95%) | Triglycerides <150mg/dL | HDL-C >40–50mg/dL | |||
| N/% | CI (95%) | N/% | CI (95%) | |||
| Total patients (N=1137) | 100/8.8 | 7.3–10.6 | 424/37.3 | 34.5–40.2 | 570/50.1 | 47.2–53.1 |
| Moderate riskb (N=109) | 40/36.7 | 27.7–46.5 | 26/23.9 | 16.2–33.0 | 50/45.9 | 36.3–55.7 |
| High riskb (N=43) | 3/7.0 | 1.5–19.1 | 12/27.9 | 15.3–43.7 | 19/44.2 | 29.1–60.1 |
| Very high riskb (N=951) | 68/7.2 | 5.6–9.0 | 378/39.7 | 36.6–42.9 | 481/50.6 | 47.4–53.8 |
| Previous coronary eventc (N=495) | 42/8.5 | 6.2–11.3 | 229/46.3 | 41.8–50.8 | 269/54.3 | 49.8–58.8 |
| Previous cerebrovascular eventd (N=173) | 11/6.4 | 3.2–11.1 | 59/34.1 | 27.1–41.7 | 78/45.1 | 37.5–52.8 |
| Peripheral arterial disease (N=202) | 15/7.4 | 4.2–12.0 | 72/35.6 | 29.0–42.7 | 108/53.5 | 46.3–60.5 |
| Type 2 diabetes mellitus (N=490) | 44/9.0 | 6.6–11.9 | 170/34.7 | 30.5–39.1 | 228/46.5 | 42.0–51.1 |
| Type 1 diabetes mellitus+microalbuminuria (N=23) | 1/4.3 | 0.1–21.9 | 16/69.6 | 47.1–86.8 | 15/65.2 | 42.7–83.6 |
| Hypertension (N=869) | 226/26.0 | 23.1–29.1 | 317/36.5 | 33.3–39.8 | 434/49.9 | 46.6–53.3 |
CI, confidence interval; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
LDL-C on target depending of global cardiovascular risk of the patients: moderate risk: LDL-C <115mg/dL; high risk: LDL-C <100mg/dL; very high risk: LDL-C <70mg/dL.
Moderate risk was considered when SCORE ≥1% to ≤5%; high risk was considered when SCORE >5% to <10%; very high risk patients were considered those with SCORE ≥10% or presence of type 2 DM, type 1 DM (with microalbuminuria), presence of a previous coronary event or cerebrovascular event or peripheral arterial disease.
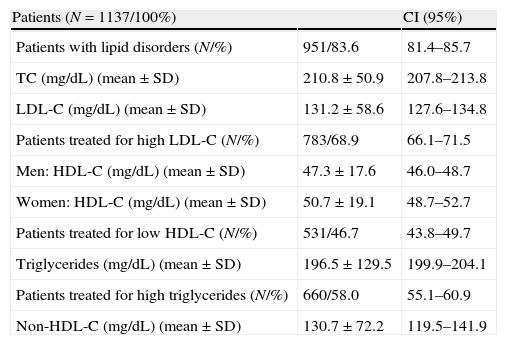
The overall prevalence of atherogenic dyslipidemia (triglycerides >150mg/dL and HDL-C <40mg/dL in men, <50mg/dL in women) was 27.1% (CI: 24.5–29.8). Most of the patients were treated for high triglycerides and LDL-C (mean TG levels of 196.5±129.5mg/dL and mean LDL-C levels 131.2±58.6mg/dL). Nevertheless, HDL-C values were within the recommended range (47.3±17.6mg/dL in men and 50.7±19.1mg/dL in women) and overall less than half of the patients received treatment for increasing HDL-C levels (Table 4).
Characteristics of the dyslipidemia.
| Patients (N=1137/100%) | CI (95%) | |
| Patients with lipid disorders (N/%) | 951/83.6 | 81.4–85.7 |
| TC (mg/dL) (mean±SD) | 210.8±50.9 | 207.8–213.8 |
| LDL-C (mg/dL) (mean±SD) | 131.2±58.6 | 127.6–134.8 |
| Patients treated for high LDL-C (N/%) | 783/68.9 | 66.1–71.5 |
| Men: HDL-C (mg/dL) (mean±SD) | 47.3±17.6 | 46.0–48.7 |
| Women: HDL-C (mg/dL) (mean±SD) | 50.7±19.1 | 48.7–52.7 |
| Patients treated for low HDL-C (N/%) | 531/46.7 | 43.8–49.7 |
| Triglycerides (mg/dL) (mean±SD) | 196.5±129.5 | 199.9–204.1 |
| Patients treated for high triglycerides (N/%) | 660/58.0 | 55.1–60.9 |
| Non-HDL-C (mg/dL) (mean±SD) | 130.7±72.2 | 119.5–141.9 |
CI, confidence interval; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; TC, total cholesterol.
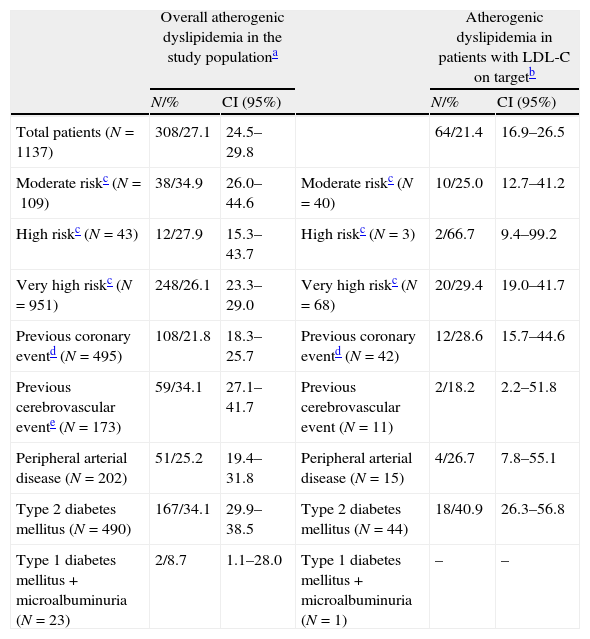
Prevalence of atherogenic dyslipidemia in the study groups according to their cardiovascular risk was also assessed (Table 5). Prevalence ranged from 26.1% in very high risk patients to 34.9% in moderate risk patients. Table 5 also shows that the prevalence of dyslipidemia in patients with LDL-C on target was 21.4% (CI: 16.9–26.5). The highest rates were reported in high risk patients (66.7%) and type 2 DM patients (40.9%).
Prevalence of atherogenic dyslipidemia in the study populations according to their cardiovascular risk.
| Overall atherogenic dyslipidemia in the study populationa | Atherogenic dyslipidemia in patients with LDL-C on targetb | ||||
| N/% | CI (95%) | N/% | CI (95%) | ||
| Total patients (N=1137) | 308/27.1 | 24.5–29.8 | 64/21.4 | 16.9–26.5 | |
| Moderate riskc (N=109) | 38/34.9 | 26.0–44.6 | Moderate riskc (N=40) | 10/25.0 | 12.7–41.2 |
| High riskc (N=43) | 12/27.9 | 15.3–43.7 | High riskc (N=3) | 2/66.7 | 9.4–99.2 |
| Very high riskc (N=951) | 248/26.1 | 23.3–29.0 | Very high riskc (N=68) | 20/29.4 | 19.0–41.7 |
| Previous coronary eventd (N=495) | 108/21.8 | 18.3–25.7 | Previous coronary eventd (N=42) | 12/28.6 | 15.7–44.6 |
| Previous cerebrovascular evente (N=173) | 59/34.1 | 27.1–41.7 | Previous cerebrovascular event (N=11) | 2/18.2 | 2.2–51.8 |
| Peripheral arterial disease (N=202) | 51/25.2 | 19.4–31.8 | Peripheral arterial disease (N=15) | 4/26.7 | 7.8–55.1 |
| Type 2 diabetes mellitus (N=490) | 167/34.1 | 29.9–38.5 | Type 2 diabetes mellitus (N=44) | 18/40.9 | 26.3–56.8 |
| Type 1 diabetes mellitus+microalbuminuria (N=23) | 2/8.7 | 1.1–28.0 | Type 1 diabetes mellitus+microalbuminuria (N=1) | – | – |
CI, confidence interval; LDL-C, low-density lipoprotein cholesterol.
Atherogenic dyslipidemia was considered when level of triglycerides >150mg/dL plus HDL-C >40–50mg/dL.
LDL-C on target was defined as LDL-C <115mg/dL (moderate risk patients), LDL-C <100mg/dL (high risk patients) and LDL-C <70mg/dL (very high risk patients), except for the total population where LDL-C was considered to be on target if <100mg/dL.
Moderate risk was considered when SCORE ≥1% to ≤5%; High Risk was considered when SCORE >5% to <10%; very high risk patients were considered those with SCORE ≥10% or presence of type 2 DM, type 1 DM (with microalbuminuria), presence of a previous coronary event or cerebrovascular event or peripheral arterial disease.
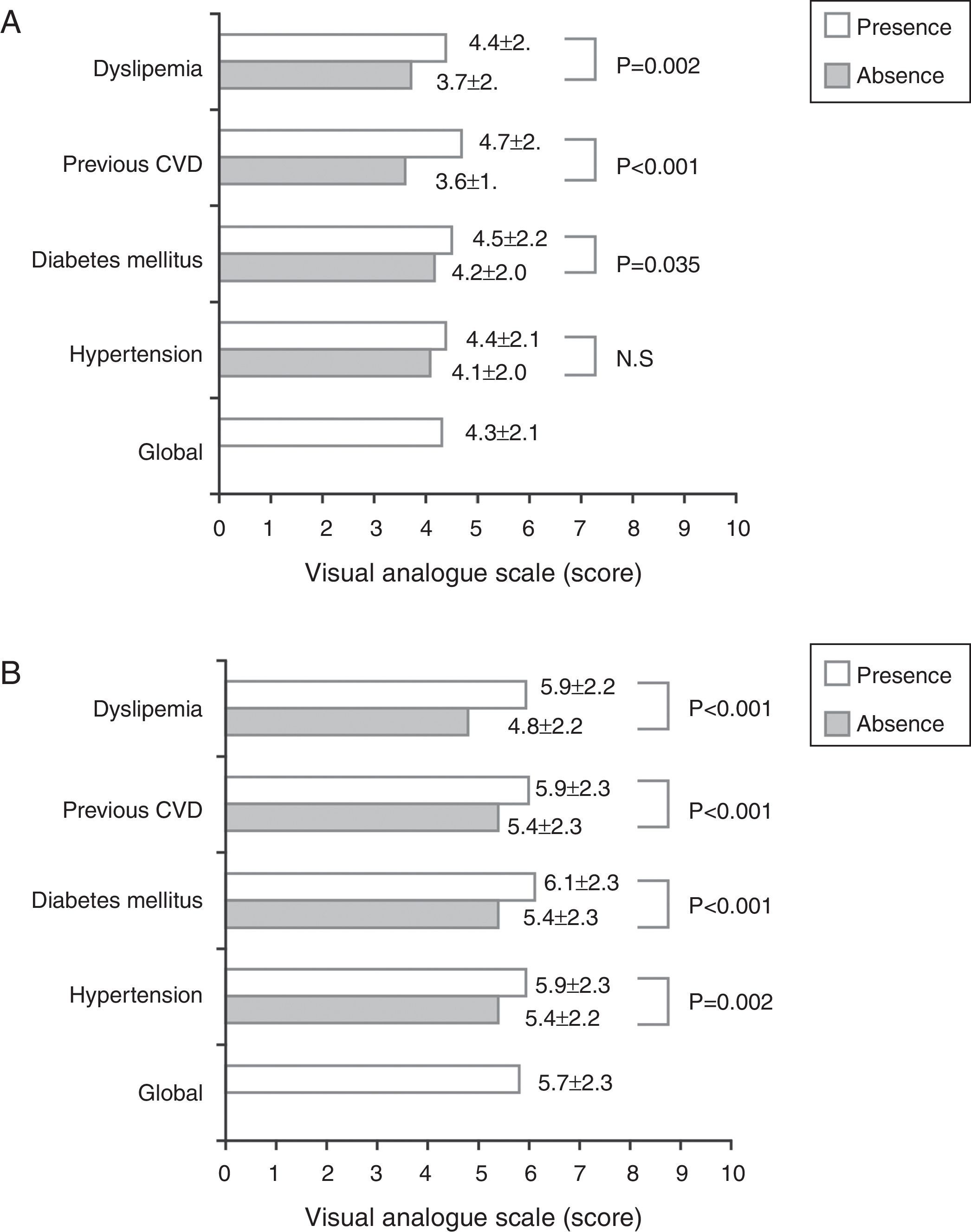
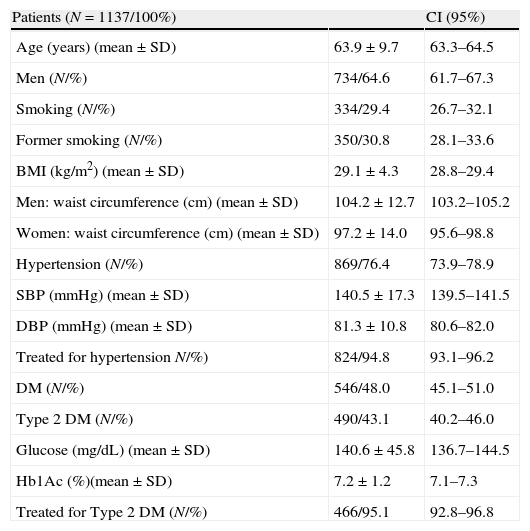
Overall, physicians’ subjective perception of cardiovascular risk on 10 point visual analog scale was slightly higher than patients’ perception (5.7 and 4.3, respectively). A significant positive correlation was found between patients’ and physicians’ perceived risk of cardiovascular disease and their actual calculated risk based on SCORE (p≤0.002). Moreover, patients’ perception of cardiovascular risk correlated positively with systolic (r=0.107, p=0.001) and diastolic blood pressure values (r=0.065, p=0.042), and negatively with non-HDL-C levels (r=−0.45, p=0.002). As shown in Fig. 1, patients with dyslipidemia, previous CVD and DM risk perceived a higher cardiovascular risk in comparison with patients not having these diseases. Cardiovascular risk perceived by physicians also differed significantly between presence and absence of dyslipidemia, previous CVD, DM and hypertension in study patients. In a multivariate analysis only the presence of established cardiovascular disease as a risk factor was independently associated with higher subjective perception of cardiovascular risk (OR=11.0; 95%CI: 8.4–13.6).
DiscussionIn our study, approximately half of the patients at moderate to very high cardiovascular risk had controlled levels of HDL-C and triglycerides, and one in four patients had low HDL-C and raised triglycerides simultaneously. Few studies have assessed the prevalence of AD among Spanish primary care patients at cardiovascular risk. Lahoz et al. reported a prevalence of 13% of patients with AD in a study involving 7823 subjects with established coronary artery disease.17 Of the participants, 26.3% had low HDL-C and 39.7% had elevated triglycerides. González-Juanatey et al. found a very similar prevalence of AD, close to 15%, in a Spanish population at high cardiovascular risk defined as having previous cardiovascular disease, DM and/or risk SCORE ≥5%.18 In our case low HDL-C was observed in 25.3% of patients and 37.8% had elevated triglycerides. Prevalence of AD reported in these two previous studies was lower than that of our study probably due to the participants’ atherosclerotic profile, and the elevated number of patients receiving lipid-lowering treatment (80.3% and 100% of patients, respectively). When compared to the abovementioned studies a higher rate of obesity, DM, lipid disorders and smokers was observed in our patients.
It is worth pointing out that the clinical characteristics of our patients suggested an elevated percentage of patients with metabolic syndrome, especially because of the high percentage of hypertensive patients, with abdominal obesity and impaired glucose tolerance. It is known that AD is typical of type 2 DM and one of the defining components of metabolic syndrome. In addition, patients with DM treated with statins often have relatively low levels of LDL-C but abnormal HDL-C and triglycerides, remaining at substantial risk of a cardiovascular event.19,20 Hermans et al. found a prevalence of AD of 35% in type 2 DM patients.21 This percentage is similar to that observed in our diabetic patients (30%) and rose to 41% in those patients with LDL-C on target. The fact that almost half of our study patients had DM along with the probable high rate of metabolic syndrome, this might also explain the overall high prevalence of AD observed in our population. Additionally, we found a high prevalence of poor control of LDL-C. Only 8.8% of patients had achieved the recommended targets. Several studies showed similar target achievement rates for this lipoprotein,18,22–24 and a worse control in patients with higher cardiovascular risk.18 Thus, our results corroborated that a high proportion of patients do not meet target levels of LDL-C, particularly in high-risk cases, even though therapy for AD is directed to first lowering serum LDL-C levels.
Previous studies have investigated the awareness and perception of patients and health professionals concerning the risk of cardiovascular events. As a novel aspect of the present study, we have examined risk perceptions among patients at moderate to high cardiovascular risk and their physicians using a visual analog scale. A significant, though weak, positive correlation was found between perceived risk of heart disease and estimated risk with SCORE charts. However, patients scored a mean of 5/10 regarding their perception of cardiovascular risk, and physicians did not score much higher (6.8/10). Considering that 83% of the population were classified as very high-risk patients (SCORE >10%, DM, previous CVD), these results indicate a low perception of cardiovascular risk, especially among the study patients. Despite using a different methodology, our findings are consistent with those of previous studies. Firstly, physicians tend to not use cardiovascular risk calculators25,26 and underestimate the absolute cardiovascular risk of their patients.27,28 Secondly, primary care patients often perceive cardiovascular risk inaccurately,29,30 and the bias tends to be toward inappropriate optimism,31,32 also in selected populations with established high risk of CVD.33–35 Furthermore, when we studied the influence of cardiovascular risk factors on perceived risk, multivariate logistic regression showed that only established CVD was significantly associated with a higher risk perception by study patients. In contrast, risk factors such as DM were not found to be an independent risk factor for cardiovascular events. A study evaluating the knowledge level of stroke risk factors among primary care patients found that DM had the lowest identification rate as a risk factor.36 Other studies also showed a considerable percentage of patients who did not recognize this condition as a risk factor.37,38 This may lead to general underestimation of risk in our study population since a significant proportion of patients have DM.
In addition to detecting that a high percentage of patients did not achieve target levels of LDL-C, an important proportion of cases have low HDL-C and high triglycerides, even when LDL-C levels were controlled. Therefore, our results underscore the extent of the residual risk in the study population at high cardiovascular risk. Awareness of the percentage of patients presenting AD in this subgroup of patients is crucial, since pharmacological and life style intervention to raise HDL-C and lower triglycerides may help to reduce residual risk. Importantly, major cardiovascular events occur more frequently in patients with AD than in those with isolated high triglycerides and low HDL-C.39 Our results also showed that a high number of patients with cardiovascular risk factors who may be eligible for prophylactic interventions to lower their risk are treated inadequately. Only about half of the patients were prescribed medicines to raise HDL-C or decrease triglycerides concentration. Possible explanations are low perception of cardiovascular risk by both patients and physicians. Subjective risk factor perception is an important component of the motivation to change unhealthy life styles and comply with medical prevention strategies, so strategies are needed to improve perception of the actual risk for heart disease.
Our study did not reach the planned sample size but it was more than 1000 patients. The authors ignore if this fact may affect the prevalence calculation but recommend take caution when considering our results.
The cross-sectional nature of our study did not allow to infer causal relationships. Moreover, the potential to generalize our findings is limited due to possible selectivity bias; the selection of primary care centers and physicians was not randomized.
Responsabilidades éticasProtección de personas y animalesLos autores declaran que para esta investigación no se han realizado experimentos en seres humanos ni en animales.
Confidencialidad de los datosLos autores declaran que han seguido los protocolos de su centro de trabajo sobre la publicación de datos de pacientes y que todos los pacientes incluidos en el estudio han recibido información suficiente y han dado su consentimiento informado por escrito para participar en dicho estudio.
Derecho a la privacidad y consentimiento informadoLos autores declaran que en este artículo no aparecen datos de pacientes.
FundingThis study was funded by Ferrer Gelos S.A.
Conflicts of interestThe authors state that Dr. Emilio Ferrer works for Ferrer International. Dr. Emilio Masana has collaborated with Ferrer International in advising for this article and with Laboratorios Dr. Esteve, Merck Sharp Dome, Danone, Sanofi aventis, Novartis as an advisor and/or performing presentations.
The authors want to thank to all the investigators who participated in the study. The investigators are listed in Annex 1.
Agustí Queral Fonollos, Dispensari MC-Mutual Tortosa,Tortosa (Tarragona); Aida Valverde Farre, Centro Médico FEDEAR, Barcelona (Barcelona); Alberto Batalla Celorio, Consulta privada, Gijón (Asturias); Alberto Costo Campoamor, Consulta privada, Cáceres (Cáceres); Alejandro Mesías Prego, Consulta privada, Ferrol (La Coruña); Alfonso Matia Portilla, Consulta privada, Valladolid (Valladolid), Alfonso Nuñez Cirera, Consulta privada, Barcelona (Barcelona); Alicia Briera Masso, Consulta privada, Barcelona (Barcelona), Álvaro Ortega Gutiérrez, Consulta privada, Sevilla (Sevilla); Amador Velarde Escoriza, Consulta privada, Córdoba (Córdoba); Amparo Marco Martínez, Consulta privada, Madrid (Madrid); Ana Expósito Rando, C.S. Miraflores, Zaragoza (Zaragoza); Ana Franch Molas, Consulta privada, Gerona (Gerona); Ana Troncoso Gil, Consulta privada, Lérida (Lérida); Andrés Carrillo Ruiz, Hospital Puerta del Mar, Cádiz (Cádiz); Andrés Pérez Garrido, Consulta Cardiología Dr. Garrido, Mérida (Badajoz); Andrés Santiago Souto, Clínica Médica Andrés Santiago, Pontevedra (Pontevedra); Ángel Donoso Berrobianco, Consulta Privada, Málaga (Málaga); Ángel Galvez Delgado, Residencia Mediterrania II, Barcelona (Barcelona); Ángel Luis López González, Consulta atención primaria, Málaga (Málaga); Ángel Riveiro Pérez, Clínica Rosalmar, Melide (La Coruña), Consulta privada, Santpedor (Barcelona); Antonio Cimbora Ortega, Consulta privada, Mérida (Badajoz), Antonio Cruz Gutiérrez, Consulta privada, Torredonjimeno (Jaén); Antonio Cumplido Pérez, Clínica Talavera, Talavera La Real (Badajoz); Antonio De La Cruz Renovales, Consulta Privada, Valencia (Valencia); Antonio Feria Herrera, Consulta privada, Linares (Jaén); Antonio Gonzalez Ibáñez, ABS Santa Eulalia Nord, Hospitalet (Barcelona); Antonio Marin Prieto, C.S. Blanca, Blanca (Murcia); Antonio Moya Moya, Consulta Privada, Castellar del Vallés (Barcelona); Antonio P. Martínez Barselo, C.S. Hijar, Híjar (Teruel); Antonio Pérez Fernández, Consulta Privada, Cádiz (Cádiz); Antonio Robles Iniesta, Clínica Robles Navarro, Valencia (Valencia); Antonio Serrano Hernández, Consulta Privada, Bilbao (Vizcaya); Aurelio Núñez Centeno, Consulta Privada, Carballo (La Coruña); Cándido Rodríguez Vázquez, Hospital Clínico, Badajoz; Carlos Alberto Nazara Otero, Clínica Medicina Interna, Pontevedra (Pontevedra); Carlos Alfredo López Giménez, Consulta Privada, Cáceres(Cáceres); Carlos Culebras Cáceres; Consulta Privada, Las Palmas de Gran Canaria (Las Palmas); Carlos Ferreres Bautista, Consulta Privada, Castellón (Castellón); Carlos González Juanatey, Consulta Privada, Lugo (Lugo); Carlos Martín Zamora, Centro Médico O Grove, O Grove (Pontevedra); Carlos Merino Martínez, Merino Laboratorio, Oviedo (Asturias); César A. Romero García, Clínica Dr. Romero, Pontevedra (Pontevedra); César Barbolla Sancho, Clínica Barbolla, Pontevedra (Pontevedra); César Vidal González, Consulta privada, Siero (Asturias); Coral Güemes Vázquez, Consulta privada, Viveiro (Lugo); Crescencio Camacho Vázquez, Consulta privada, Huelva (Huelva); Cristina Escobairo Platero, ABS Santa Eulalia Nord, Hospitalet (Barcelona); Cristobal Navas Navas, Centro médico Gema, Mataró (Barcelona); Daniel Cepero García, Consulta Privada, Almería (Almería); Daniel Mejías Hidalgo, Consulta Privada, Granada (Granada), David Gremer Luengos, Consulta Privada, Palma de Mallorca (Mallorca), Diego Ferrer Marín-Blázquez, Consulta Privada, Cieza (Murcia); Domingo J. Rubira López, C.S. Cieza, Cieza (Murcia); Driss Melehi El Assali, Hospital Universitario de Albacete, Albacete (Albacete); Eddi Velázquez Arias, Clínica Velázquez Roldán Cardio, Madrid (Madrid), Eduard Castellarnau Ibáñez, Consulta privada, Barcelona (Barcelona); Eduardo Antolin Saez, C.S. Miguel Servet, Alcorcón (Madrid); Eduardo Martínez de Moretin, Hospital Puerto Real (Cádiz); Eduardo Molina Navarro, Consulta privada, Granada (Granada); Eduardo Uribe Echeverría Martínez, Policlínica Guipúzcua, Donostia (Guipúzcoa); Elisabet Sánchez Pujol, Centre Medic Caldes, Caldas (Barcelona); Emilio Armada Rodríguez, Consulta privada, Orense (Orense); Emilio Rodríguez García, Consulta privada, Orense (Orense); Emilio Suárez-Lledo Alemany, Consulta privada, Gijón (Asturias); Enrique Canelles Gamir, Consulta privada, Valencia (Valencia); Enrique Garcia Martín, C.S. Onil, Onil (Alicante); Enrique Rodilla Sala, Clínica Wesfalia, Valencia (Valencia); Enrique Sardaña Álvarez, IG Group Sanitari, Tarragona (Tarragona); Esteban Domarco Escolar, Centro Médico Gabitema, Alcalá de Henares (Madrid); Euclides Real Rojas, Consulta privada, Ponteceso (La Coruña); Eusebio Suárez Fernández, Consulta privada, Jaén (Jaén); Francisco Javier Moreno Bandera, Consulta privada, Inka (Valencia); Francisco Javier Peñafiel Martínez, Consulta privada, Almería (Almería); Federico Iglesias Fernández, Consulta privada, Cariño (La Coruña); Felina Melvis Anaya Blanco, Consulta privada, Barcelona (Barcelona); Felipe Ferre Larrosa, C.S. Espinardo, Murcia (Murcia); Felisa Fernández Fernández, Consulta privada, Orense (Orense); Fernando Dolz Andrés, Consultorio Misericordia, Reus (Tarragona); Fernando Sabatel López, Consulta privada, Granada (Granada); Fernando Urtasun Brito, Consulta privada, Las Palmas de Gran Canaria (Las Palmas); Fernando Wanguemert Pérez, Centro Médico CARDIAVANT, Las Palmas de Gran Canaria (Las Palmas); Florentino Casal Alvarez, Clínica Casal, Gijón (Asturias); Francesc Planas Ayma, Clínica privada, Badalona (Barcelona); Francesc Solé Llorens, Consulta Dr. Solé, Sabadell (Barcelona); Francisco Azorín Esteban, Consulta privada, Elche (Alicante); Francisco Carmona Segura, Consulta privada, Posadas (Sevilla); Francisco Carrero Reyes, Consulta privada, Las Cabezas (Córdoba); Francisco Javier Ampudia Blasco, Clínica Alemania, Manises (Valencia); Francisco Javier Cecilio Montero, C.S. Porriño, Porriño (Pontevedra); Francisco Javier Escoda Martínez, Consulta privada, Montbrio del Camp (Tarragona); Francisco Javier Luque Olmedo, Consulta privada, Sevilla (Sevilla); Francisco Jesús Expósito, Consulta privada, Castro de Rei (Lugo); Francisco Jesús Astudillo Martin, Consulta privada, Sevilla (Sevilla); Francisco López Rincón, Consulta privada, Algeciras (Cádiz); Francisco Torres Calvo, Consulta privada, Málaga (Málaga); Gabriel Giménez Pérez, Consulta privada, Barcelona (Barcelona); Gemma Sesmilo León, Institut Dexeus, Barcelona (Barcelona); Gerardo González Guillén, Centro médico de Taco S.L., La Laguna (Sta Cruz de Tenerife); Gerardo Iglesias Lobejón, Clínica Gerardo Iglesias, Lugo (Lugo); Ginés Delgado Cerrillo, Consulta privada, Córdoba (Córdoba); Gonzalo Concheiro Coello, Sanatorio Concheiro, Ordes (La Coruña); Gonzalo Guzzo Merello, Consulta privada, Madrid (Madrid); Gregorio Manzano García, Consulta privada, Córdoba (Córdoba); Guillermo Pérez Toledo, Consulta privada, Las Palmas de Gran Canaria(Las Palmas); Herminio Fernández Gavilán, Consulta privada, La Línea (Cádiz); Hugo Polanco Pérez, Consulta privada, Alicante (Alicante); Ignacio Echeverria Lucotti, Meca del Castillo, Cieza (Murcia); Ignacio González Sánchez, Consulta privada, Sabadell (Barcelona); Ignacio López Pavón, C.A.P. Doctor Vilaseca, Santa Coloma de Gramenet (Barcelona); Ignacio Ruiz Martínez, Centro Médico Boadilla, Boadilla del Monte (Madrid); Ignacio Sainz Hidalgo, Centro Médico Fisiocard, Sevilla (Sevilla); Inmaculada Monreal Mauri, Consulta privada, Mataró (Barcelona); Isabel Palma Baro, Consulta privada, Córdoba (Córdoba); Isidoro Carmona de Torres, Consulta privada, Sevilla (Sevilla); Isidoro Martínez Olivares, Consulta privada, Valencia (Valencia); José Antonio Galán Velasco, C.S. Villoria, Villoria (Salamanca); Javier Andrés Novales, Consulta privada, Bilbao (Vizcaya); Javier Mora Robles, Consulta privada, Málaga (Málaga); Javier Rodriguez Argüeso; Consulta privada, Alicante (Alicante); Javier Saez-Torres Viso, C.S. Chapela, Redondela (Pontevedra); Jesús Arrobas Vacas, Centro Cardiológico Dr. Fernández de Soria, Badajoz (Badajoz); Jesus Fernández Baizan, Clínica Foncalada, Oviedo (Asturias); Jesús Gutierrez De La Peña, Clínica privada, Algeciras (Cádiz); Jesús Luengo Agüero, Clínica privada, Leganés (Madrid); Jesús Luís Montoya Arocena, Consulta privada, Valencia (Valencia); Jesús Maria Subinas Elorriaga, Clínica privada, Bilbao (Vizcaya); Jesus Palomo Del Arco, C.S. Guijuelo, Guijuelo (Salamanca); Joan Prunera Pruñanosa, Consulta privada, Sabadell (Barcelona); Joaquín Cano Nieto; Consulta privada, Málaga (Málaga); Joaquín Pechuan Asensio, Consulta privada, Granada (Granada); Joaquín Ruiz De Castroviejo, Consulta privada, Córdoba (Córdoba); Joaquina Belchi Navarro; Consulta privada, Valencia; Jorge García Alemán; Consulta privada, Málaga (Málaga); Jorge Sales Sanz; Consulta privada, Valencia (Valencia); Jorge Vega Fernández, Consulta privada, Cáceres (Cáceres); José Ángel H. Fernández Martínez, Consulta privada, La Coruña (La Coruña); José Antonio García Donaire, Clínica Santa Elena, Madrid (Madrid); José Antonio Garrido García, Consulta privada, Oviedo (Asturias); José Antonio Gordo Martínez, Consulta privada, Fuenlabrada (Madrid); José Antonio Jiménez Plata, Consulta privada, Sevilla (Sevilla); José Antonio Lastra Galán, Consulta privada, León (León); José Antonio Mariscal Bernat, Consulta privada, Castellón (Castellón); José Antonio Montes Valles, Consulta privada, Oviedo (Asturias); Jose Antonio Romero Hinojosa, Consulta privada, Granada (Granada); José Blanco Castiñeira, Consulta privada, La Coruña (La Coruña); José Bronsoms Artero, Consulta privada, Gerona (Gerona); José Carlos Porro Fernández, Consulta privada, Madrid (Madrid); José Contreras Gilbert, Consulta Privada, Sevilla (Sevilla); José Coronado Martínez, Centro Salud Ramonete, Ramonete (Murcia); José Enrique Rubiols Giménez, Consulta Privada, Valencia (Valencia); José Francisco Felipe Olivero, Consultorio Rambla Pulido, Santa Cruz de Tenerife (Santa Cruz de Tenerife); José Francisco Muñoz Mascarell, Consulta Privada, Valencia (Valencia); Jose Gómez Yelo, Consulta Privada, Murcia (Murcia); Jose Ignacio Chagoyen Latienda, Consulta Privada, Arcos de la Frontera (Cádiz); José Javier Gómez Barrado, Consulta Privada, Cáceres (Cáceres); José Javier Grillo Perez, Consulta Privada, La Orotova (Santa Cruz de Tenerife); José Juan Vázquez Cobaleda, Consulta Privada, Sevilla (Sevilla); José Lluis Montserrat Carrio, CEMAR, Barcelona (Barcelona); José Luis Colomer Marti, Consulta Privada, Paiporta (Valencia); José Luis Delgado Prieto, Consulta Privada, Málaga (Málaga); José Luis Ortiz Lozano, Consulta Privada, Jaén (Jaén); José Luis Ruiz Araguat, Clinicas del L¿Ebre, Tortosa (Tarragona); José Luis Vega Barbado, Consulta Privada, Valladolid (Valladolid); José Luís Vidal Martín, Consulta Privada, Valencia (Valencia); José Manuel Franco Zapata, Consulta Privada, Córdoba (Córdoba); José Manuel Garcia Almeida, Consulta Privada, Málaga (Málaga); José Manuel Garrido Sampedro, Consulta Privada, Orense (Orense); José Manuel Herranz González, Consulta Privada, La Coruña (La Coruña); José Manuel Lage Parente, Consulta Privada, Orense (Orense); José Manuel Monge García, Consulta Privada, Puerto de Santa María (Cádiz); José Maria Jiménez Páez, Consulta Privada, Córdoba (Córdoba); José Maria Millán Simo, Consulta médica S.C., Sevilla (Sevilla); José Maria Saavedra Rodríguez, Consulta Privada, Las Palmas de Gran Canaria (Las Palmas); José Martínez Valls, Consulta Privada, Ontinyent (Valencia), José Neldo Prieto Sendín, Clínica Dr. Prieto, Vigo (Pontevedra); José R. Saenz De Ugarte Arejula, Consulta Privada, Bilbao (Vizcaya); José Revert López, Consulta Privada, Valencia (Valencia); José Sánchez Ferrer, Consulta Privada, Redoban (Alicante); Jose Vicente Fenollar Aparicio, Consulta Privada, Valencia (Valencia); José Zurro Hernandez, Consulta Privada, Valladolid (Valladolid); Joseba Muñoz Díaz, C.R. Aldakorra, Tolosa (Guipuzcoa); Josefina Olivares Alcolea, Ctro Especialidades Médicas Llucmajor, Llucmajor (Mallorca); Josep Boladeras Sabater, Juaneda Urgencias Médicas, Pollença (Mallorca); Josep Joan Carreras Fígols, Consulta privada Plaça Independència, Gerona (Gerona); Josep Maria Sala Médico, Consulta Privada, Pineda de Mar (Barcelona), Juan Antonio Arazola Pérez, Consulta Privada, Huelva (Huelva); Juan Antonio García Arnes, Consulta Privada, Málaga (Málaga); Juan Carlos García López, Hospital General de Albacete, Albacete (Albacete); Juan Carlos Montequi Fitera, Consulta Privada, Madrid (Madrid); Juan Enrique Pereñiguez, C. S. Espinardo, Murcia (Murcia); Juan Francisco Andrade Bellido, Consulta Privada, Pozoalcón (Jaén); Juan Francisco Novoa Rodríguez, Consulta Privada, O Porriño (Pontevedra); Juan García-Valdecasas Valverde, Consulta Privada, Granada (Granada); Juan José Linares Linares, Consulta Privada, Granada (Granada); Juan Luís Hernández Juan, Clínica Monasterio, Elda (Alicante); Juan Manuel Beltrán Beltrán, Clínica Privada, Castellón (Castellón); Juan Manuel Supulveda Manzanares, Centro Médico Quintanar Servicios Medicos S.L., Quintanar de la Orden (Toledo); Juan Ortega Bernal, Clínica Privada, Cartagena (Murcia); Juan Quiroga López, Capio Hospital de Día Talavera, Talavera de la Reina (Toledo); Juan Ramón Crespo Garcia, Consulta Dr. Crespo, Gijón (Asturias); Juan Ramon Siles Rubio, Clínica del Río, Estepona (Málaga); Juan Ribot Pérez, Consulta Privada, Girona (Girona); Juana Fraile Gómez, Consulta Privada, Badajoz (Badajoz); Julio Fernández Romero, Consulta Privada, Murcia (Murcia); Julio Jímenez Franco, Consulta Privada, Valencia (Valenci
a), Justo Torres Romero, Consulta Privada, Valladolid (Valladolid); Lorenzo García Haba, Consulta Privada, Bargas (Toledo); Lorenzo Jiménez Alfonso, Consulta Privada, Cehegin (Murcia); Lucas Cano Calabria, Clínica Novo Santi Petri, Santi Petri (Cádiz); Luis Alberto Gómez Gómez, Centro privado, Llucmajor (Mallorca); Luis Antonio Fernández-Lázaro, Consulta Privada, Bilbao (Vizcaya); Luis Banchs Galtes, Consulta Privada, Mataró (Barcelona); Luis Carlos Fernández Leoz; Sanatorio Covadonga, Gijón (Asturias); Luís Cerón Garcia, Centro de Salud Capuchinos, Salamanca (Salamanca); Luis F. Cabañas Enríquez, Consulta Privada, Talavera (Toledo); Luís Lerga Paz, Consulta Privada, Málaga (Málaga); Luís Pedro Febles Bethencourt, Hospital de Bellevue, Puerto de la Cruz (Santa Cruz de Tenerife); Luís Richard Rodríguez, C.S.de Jijona, Jijona (Alicante); Luís Sanchez Escalada, Policlínica Lopez de Hoyos, Madrid (Madrid); Maria Dolors Guitart Tolosa, Consulta Privada, Manresa (Barcelona); Maria Teresa Arguisjuela Hermida, Consulta Privada, Sevilla (Sevilla); María Montserrat Lopez Sans, ABS Santa Eulalia Nord, Hospitalet (Barcelona); María Rosario Guillen Benzal, Consulta Privada, Sevilla (Sevilla); Mabel Tizon Vázquez, Nuestra Señora de Fátima, Madrid (Madrid); Manuel Andreu Ruiz, Consulta Privada, Cambrils (Tarragona); Manuel Aparici Feal, Consulta Privada, La Coruña; Manuel Bravo Díaz, Consulta Privada, Baños de la Encina (Jaén); Manuel Cervera del Pino, Consulta Privada, Lleida (Lleida); Manuel Duran Caballero, Consulta Privada, Sevilla (Sevilla); Manuel Fernandez Bercher, Consulta Privada, Córdoba (Córdoba); Manuel Godoy Montes, Centro médico de especialistas, Valencia (Valencia); Manuel Granell Font, Consulta Privada, Castellón (Castellón); Manuel José Vicente Arroyo, Centro de Salud Los Capuchinos, Salamanca (Salamanca); Manuel Quiros Valera, Consulta Privada, Sevilla (Sevilla); Manuel Ramos Rodríguez, Centro de Salud Guijuelo, Salamanca (Salamanca); Manuel Rayo Gutiérrez, Clínica Cardiorreal, Ciudad Real (Ciudad Real); Manuel Torres Pascual, Consulta Privada, Orihuela (Alicante); Manuel Valor Beltrán, Policlinica Guillén de Castro, Valencia (Valencia); Manuel Vida Gutierrez, Consulta Privada, Almería (Almería); Manuela Liceran Sanandres, ABS Santa Eulalia Nord, L’Hospitalet de Llobregat (Barcelona); Marcos García Aguado, Consulta Privada, Madrid (Madrid); Maria del Mar Lucena Merino, Consulta Privada, Ciudad Real (Ciudad Real); María Dolores Martínez Sanchez, Consulta Privada, Cádiz (Cádiz); María Dulce Pina Barrios; Consulta Privada, Ciudad Real (Ciudad Real); María Gema Godoy Tundidor, Centro Médico Godoy, Madrid (Madrid); Marti Fradera Subirana, Consulta Privada, Canet de Mar (Barcelona); Martín Jorge Alvear Garcia, Consulta Privada, Noia (La Coruña); Matías Cegarra Ortiz, Clínica centro médico Aguilas, Aguilas (Murcia); Maximino González Fernández, Consulta Privada, León (Léon); Medardo J Melián Martín, Consulta Privada, Lugo (Lugo); Miguel Ángel Palos Ortega, Clinica Sant Josep, Manresa (Barcelona); Miguel Campo de Juan, Consulta Privada; Sabadell (Barcelona); Miguel Estanislao González Fernández, Clínica Compostela, Vigo (Vigo); Miguel González Herrero, Consulta Privada, Sabadell (Barcelona); Miguel Pelayo Martínez, Consulta Privada, Almería (Almería); Miguel Quesada Charneco, Consulta privada, Granada (Granada); Mohsen Abedianzadeh Timar, Consulta privada, Castelldefells (Barcelona); Montse Llop Moreno, Consulta privada, Barcelona (Barcelona); Montserrat Fernández, Centro Cor Lleida, Lérida (Lérida); Nicolás Salvador Guzmán, CAP de Xixona, Xixona (Alicante); Nicolás Torres Vázquez, Consulta privada, Sevilla (Sevilla); Norberto Herrera Gutierrez, Consulta privada, Lucena (Córdoba); Oscar Guzmán Ruiz, Consulta privada, Ciudad Real (Ciudad Real); Óscar Llorian Fernández-Rivera, Consulta privada, Gijón (Asturias); Patricia Gili Martínez-Meco; Hospital Virgen de la Luz, Cuenca (Cuenca); Pedro Cabeza Lainez; Consulta privada, Cádiz (Cádiz); Pedro José De La Paz Gutierrez, Policlínico Curbelo, Güimar (Tenerife); Pedro Pinto González, Consulta privada, Ávila (Ávila); Pedro Vigil-Escalera González, Sanatorio Begoña, Gijón (Asturias); Pilar Baillo Falo, Centro Médico Pilar Baillo, Cervera (Lérida); Pilar Prieto Castro, Centro Saüde Xermade, Xermade (Lugo); Rafael Alqhai Alqhai; Consulta privada, Palma del Rio (Córdoba); Rafael Castellano Cerviño; Centro Saude Pobra de Brollón, Pobra de Brollón (Lugo); Rafael Fernández de Soria, Centro Cardiología Dr. Fernández de Soria, Bajadoz (Badajoz); Rafael Fernández Martínez, Consulta privada, Orgiva (Granada); Rafael Sola Casado, Consulta privada, Almería (Almería); Ramiro Antuña de Alaiz, Consulta privada, Gijón (Asturias); Ramón Cuevas Verdú, Consulta privada, Xátiva (Valencia); Ricardo Huerta Blanco, Consulta privada, Telde (Las Palmas de Gran Canarias); Ricardo Lopez Tiñena, C.M.Q.R. Centro Médico, Reus (Tarragona); Ricardo Navarro Tarin, Consulta Privada, Valencia (Valencia); Rosa María Roca Auledas, Consulta Privada, Mataró (Barcelona); Rosendo Marcos Sarmiento; Consulta Privada, Aller (Asturias); Roser Valent Ferrer, Consulta Privada, Gerona (Gerona); Salvador Alnela Rambla, Consulta Privada, Castellón (Castellón); Salvador Blanch, Consulta Privada, Valencia (Valencia); Salvador Criado de Reina, Consulta Privada, Puente Genil (Córdoba); Salvador Moreno Onorato, Consulta Privada, Puerto Llano (Ciudad Real); Salvador Sitjar Martínez de Sas, Consulta Privada, Barcelona (Barcelona); Samir Tuma Maroky; Consulta Privada; Barcelona (Barcelona); Sergio Vera Pérez; Consulta Privada, Guardamar (Alicante); Severino Pérez Fernández, Consulta Privada, Cáceres (Cáceres); Taha Taha Abdulclal, Consulta Privada, Madrid (Madrid); Tarif Kseibi Alhousseini, Consulta Privada, Madrid (Madrid); Teresa Laso Morales, Clínica Nuosalud, Majadahonda (Madrid); Tomás De Vega Santos, Consulta Privada, Santander (Santander); Tomas Echeverría García, Centro Cardiológico ONDARSÁN (Consulta particular), San Sebastián (Guipúzcoa); Tomás Manuel Alberola Rigal, Consulta Privada, Alicante (Alicante); Vicente Brossa Loidi, Consulta Privada, Barcelona (Barcelona); Vicente Ignacio Arrarte Esteban; Hospital Internacional Medimar; Alicante (Alicante); Vicente Martínez Lillo, Consulta Privada, Alicante (Alicante); Vicente Navarro Tarin, Consulta Privada, Valencia (Valencia); Xavier Martínez Álvarez, Consulta Privada, Mollet del Vallés (Barcelona); Xesus Manuel Suárez García, Policlínico Co.Sa.Ga, Ourense (Ourense); Yolanda García Vázquez, Consulta Privada, Castelldefels (Barcelona); Youssef Nakhle El Mokabare, Centro médico Santa Ursula, Santa Úrsula (Santa Cruz de Tenerife).