The aim of this study was to the data from the National Registry of Incisional Hernia (EVEREG) to determine the reality of the treatment of this condition in Spain.
MethodsEVEREG is an online prospective database which has been functioning since July 2012; operations for incisional hernia are anonymously recorded.
ResultsUp to March 2015, 4501 hernias from 95 of the 113 participating hospitals were registered. The mean age of the patients was 62.7, and 56.5% were women, with a mean BMI of 30.2kg/m2; 29.8% presented a high surgical risk (ASA III–V). A total of 93.7% were scheduled surgeries, 88.3% open surgery and 22.2% were recurrent incisional hernias. There were 66.9% hernias after a midline laparotomy, and 81.4% of a transverse diameter of less than 10cm. A mesh was used in 96.2% of cases. Postoperative stay was 5.3 days and 29.1% presented a complication, with a mortality of 0.8%. After a median follow-up of 7.7 months a high rate of recurrence was detected (20.7% per year), especially in hernias that were operated on after a previous repair (18.1% primary vs. 30.6% recurrent; P=.004).
ConclusionThe EVEREG registry is a useful tool to know the current situation of incisional hernia treatment. Analysis of the data shows several points that could be improved: a low rate of follow-up and high recurrence rate.
El objetivo de este estudio fue analizar los datos recopilados en el Registro Nacional de Hernia Incisional (EVEREG) para conocer la situación actual del tratamiento de esta dolencia en España.
MétodosEVEREG es una base de datos prospectiva online en la que, desde julio de 2012, se registraron de forma anónima los datos de las hernias incisionales intervenidas en España.
ResultadosHasta marzo de 2015, se han registrado 4.501 hernias en 95 de los 113 hospitales inscritos. La edad media de los casos fue de 62,7 años, un 56,5% mujeres, con un IMC medio de 30,2kg/m2 y un 29,8% de ellos con riesgo quirúrgico elevado (ASA III-V). Un 93,7% de las intervenciones fueron electivas, el 88,3% por cirugía abierta y el 22,2% fueron hernias recurrentes. El 66,9% correspondían a una hernia tras laparotomía media, en el 81,4% el diámetro transversal fue menor de 10cm. Se empleó una prótesis en el 96,2% de los casos. La estancia postoperatoria fue de 5,3 días, con complicaciones en el 29,1% y con una mortalidad del 0,8%. Tras una mediana de seguimiento de 7,7 meses se ha detectado un elevado índice de recurrencias (20,7% al año), sobre todo en hernias intervenidas tras una reparación previa (18,1% primarias vs 30,6% recidivadas; p=0,004).
ConclusiónEl registro EVEREG es una herramienta útil para conocer la situación actual del tratamiento de la hernia incisional. El análisis de los datos señala como principales elementos susceptibles de mejora el bajo índice de seguimiento y la elevada tasa de recurrencias.
National abdominal wall defect registries began in Sweden in 1992,1 taking advantage of the diffusion of information systems. Nilsson2 in Sweden and Bay-Nielsen3 in Denmark published very interesting initial results in inguinal hernias.
Due to their prevalence, clinical and economic repercussions, and the lack of agreement in their treatment and results, incisional hernias are an important pathology to be audited by means of a registry.
The first attempts at establishing national incisional hernia registries also emerged from the Nordic countries,4 where a multicenter study at 40 hospitals detected wide heterogeneity in treatments and results. The authors came to just one conclusion: the need for improvement. Therefore, a national registry was created.
Meanwhile, in Denmark, the Danish Ventral Hernia Database was established in 2006. Its initial published studies5,6 confirmed the lack of a consensus strategy in the treatment of ventral hernia as well as relevant postoperative morbidity rates. This led to the establishment of improvement processes and the promotion of national conferences to discuss the results and reduce the variability in the processes.
Other European registries include: Herniamed7 in Germany, which registers cases with all types of hernias; Club Hernie in France8 (http://www.club-hernie.com/), with all types of patients treated by a participating group of hospitals and surgeons; and, then there are the registries of the Netherlands and Belgium, which are still in early stages.
In 2011, the European Registry of Abdominal wall HerniaS (EuraHS)9 was created under the auspices of the European Hernia Society (EHS). This online European registry of ventral hernias is a unique and quite interesting initiative that unfortunately has not been met with successful participation.
The Spanish Registry of Incisional Hernias (known as EVEREG) was started in Catalonia in 2012. The initiative quickly extended to the rest of the country in January 2013, with the participation of the Abdominal Wall and Sutures Division of the Spanish Association of Surgeons.
The objective of the present study is to analyze the data collected in the aforementioned registry since its inception in July 2012 until March 2015 and, based on the results, to determine the current treatment status of this prevalent condition and to detect those areas susceptible to improvement where unified action strategies should be applied.
MethodsThis study provides an observational descriptive analysis of the data obtained from EVEREG since its inception until March 2015.
The central database (PostgresSQL version 8.4) used has been designed from a computerized data entry platform called OpenClinica, which is accessible through the Internet (http://www.evereg.es/). On this site, is possible to anonymously record all cases of incisional hernias that have been treated surgically at the participating medical centers. The study protocol has been approved by the Ethics Committees at all the participating hospitals, and the regulations of the Organic Law on Data Protection and Patient Autonomy have been followed.
Inclusion criteria were: hernias that had appeared after laparotomy; and, recurrences after previous incisional or ventral hernia repair.
Exclusion criteria were: other types of primary ventral hernias (umbilical, epigastric, Spiegel).
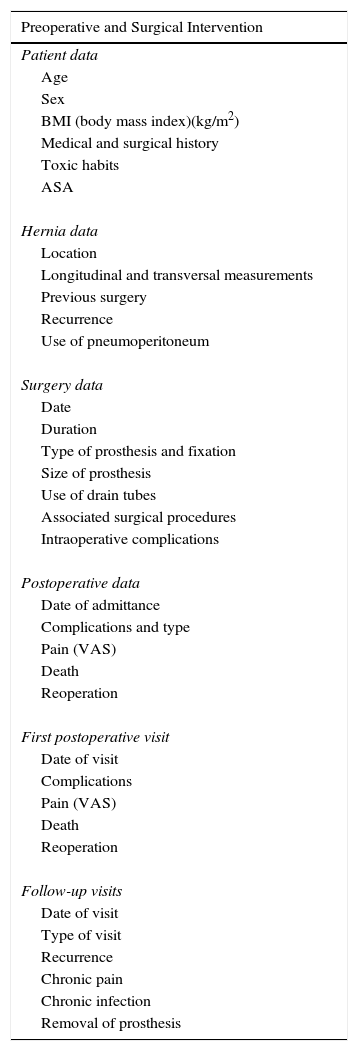
The introduction of a new case generates a unique identification number that is only known by the person in charge at the reporting hospital, thereby ensuring patient anonymity. The registry is for hernias and not for patients, so patients with more than one hernia, or those who have been treated repeatedly for recurrences, may be registered repeatedly. Patients receive an informed consent form for the surgery, in which they accept the collection of data related to their intervention and subsequent follow-up. The variables compiled are demonstrated in Table 1.
Data Compiled in the Registry.
| Preoperative and Surgical Intervention |
|---|
| Patient data |
| Age |
| Sex |
| BMI (body mass index)(kg/m2) |
| Medical and surgical history |
| Toxic habits |
| ASA |
| Hernia data |
| Location |
| Longitudinal and transversal measurements |
| Previous surgery |
| Recurrence |
| Use of pneumoperitoneum |
| Surgery data |
| Date |
| Duration |
| Type of prosthesis and fixation |
| Size of prosthesis |
| Use of drain tubes |
| Associated surgical procedures |
| Intraoperative complications |
| Postoperative data |
| Date of admittance |
| Complications and type |
| Pain (VAS) |
| Death |
| Reoperation |
| First postoperative visit |
| Date of visit |
| Complications |
| Pain (VAS) |
| Death |
| Reoperation |
| Follow-up visits |
| Date of visit |
| Type of visit |
| Recurrence |
| Chronic pain |
| Chronic infection |
| Removal of prosthesis |
Patients were considered to be affected by chronic pain when they presented pain related to surgery (Visual Analog Scale greater than 3) more than 6 months after the initial intervention. Recurrences were defined as all protrusions in the surgical area that the surgeon who explored the patient designated as a recurrence, as well as those diagnosed with imaging studies. Persistent suppuration of the wound more than 6 months after surgery was considered chronic infection.
Nine groups have been established based on the number of hospitals in each Spanish Autonomous Community and their geographical proximity (Andalusia, Catalonia, Madrid, Levante, Northern Zone, Castile-La Mancha, Castile-Leon, Extremadura, and Canary Islands), that meet at least every 6 months to exchange information, coordinate actions, and review results. In each of the regions, a representative has been appointed to attend an annual meeting at which actions are planned, improvements are made in data collection, and the results are reviewed cooperatively. By March 2015, a total of 113 hospitals had joined the initiative (15 tertiary hospitals, 34 general hospitals, 60 regional hospitals, and 4 private medical centers). The geographical distribution and the detailed hospital list of the hospitals can be consulted on the registry website (http://www.evereg.es).
The data are stored on an external server managed by a company employed for this function (SAIL, Servicio de Asesoría a la Investigación y Logística, Barcelona). The company financing the initiative does not have access to the stored data.
Statistical AnalysisThe present study used the data provided in the periodic summaries to which the regional representatives have access. The means, standard deviations, and number of cases for each item were analyzed by the GraphPad Quick Calcs tool (GraphPad Software Inc., La Jolla, CA, USA) (http://www.graphpad.com/quickcalcs/), which provided rapid statistical calculation.
A univariate analysis was conducted using Fisher's exact test or the chi-squared test (χ2) to evaluate the association of the categorical variables and Student's t test for the quantitative variables. A P<.05 was considered significant.
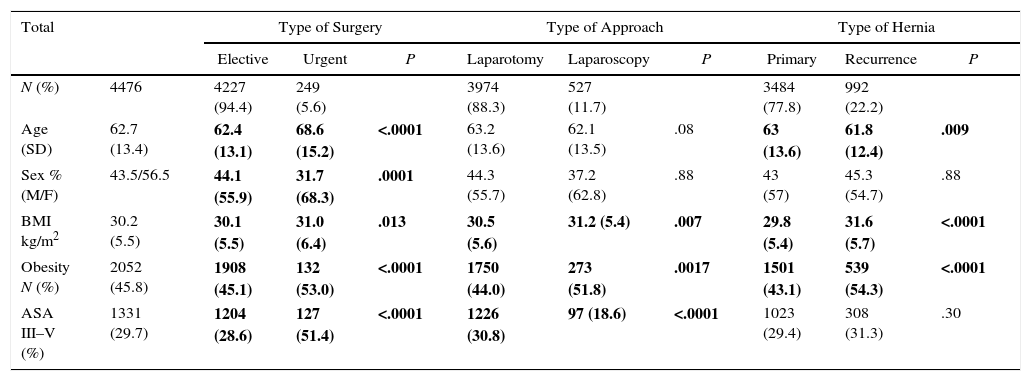
ResultsA total of 4501 hernias (1636hernias/year) were registered between July 2012 and March 2015 at 95 of the 113 participating hospitals; demographic data were available for 4476. Table 2 compares the sociodemographic characteristics from the records (laparotomy vs. laparoscopy, elective vs. urgent surgery, and primary vs. recurrent repairs).
Sociodemographic Characteristics of the Patients According to the Type of Surgery, Approach, and Hernia.
| Total | Type of Surgery | Type of Approach | Type of Hernia | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Elective | Urgent | P | Laparotomy | Laparoscopy | P | Primary | Recurrence | P | ||
| N (%) | 4476 | 4227 (94.4) | 249 (5.6) | 3974 (88.3) | 527 (11.7) | 3484 (77.8) | 992 (22.2) | |||
| Age (SD) | 62.7 (13.4) | 62.4 (13.1) | 68.6 (15.2) | <.0001 | 63.2 (13.6) | 62.1 (13.5) | .08 | 63 (13.6) | 61.8 (12.4) | .009 |
| Sex % (M/F) | 43.5/56.5 | 44.1 (55.9) | 31.7 (68.3) | .0001 | 44.3 (55.7) | 37.2 (62.8) | .88 | 43 (57) | 45.3 (54.7) | .88 |
| BMI kg/m2 | 30.2 (5.5) | 30.1 (5.5) | 31.0 (6.4) | .013 | 30.5 (5.6) | 31.2 (5.4) | .007 | 29.8 (5.4) | 31.6 (5.7) | <.0001 |
| Obesity N (%) | 2052 (45.8) | 1908 (45.1) | 132 (53.0) | <.0001 | 1750 (44.0) | 273 (51.8) | .0017 | 1501 (43.1) | 539 (54.3) | <.0001 |
| ASA III–V (%) | 1331 (29.7) | 1204 (28.6) | 127 (51.4) | <.0001 | 1226 (30.8) | 97 (18.6) | <.0001 | 1023 (29.4) | 308 (31.3) | .30 |
Data with statistically significant differences are shown in bold.
Most operations (94.4%) were conducted as scheduled surgery. Patients who underwent urgent operations were older (68.6 vs. 62.4 years, P<.0001), predominantly women (68.3% vs. 55.9%, P=.0001), more frequently affected by obesity (BMI≥30kg/m2) (53% vs. 45.1%, P<.0001) and had higher surgical risk (ASA III–V 51.4% vs. 28.6%, P<.0001). Associated intestinal resection was performed in 38 patients (15.3%) who were operated on urgently and 48 (1.1%) of those who underwent scheduled surgery.
Laparoscopic surgery was used less frequently than laparotomy (11.7% vs. 88.3%). This group presented significant differences with the laparotomy group: obesity was much more frequent (51.8% vs. 44%, P=.0017) and the anesthetic risk was significantly lower (ASA III–V 18.6% vs. 30.8%, P<.0001).
A significant percentage of hernias treated (22.2%) were recurrences of a previous surgery. These patients presented a significantly younger age than patients who were being treated for the first time (61.8 vs. 63 years, P=.0086) and were more obese (54.3% vs. 43.1%, P<.0001).
The most frequent location of the hernias was a previous midline laparotomy (n=2994; 66.9%). Trocar-site hernias affected 16% of patients (n=718), followed by subcostal (n=242; 5.4%), parastomal (n=174; 3.9%) and McBurney incisional hernias (n=126; 2.8%). The remaining sites affected 4.9% (n=220) of cases. As for the dimensions of the hernias, 3995 patient files had this datum recorded: 509 (12.74%) had a transverse diameter between 10 and 15cm, and 233 (5.83%) had a diameter larger than 15cm. In most cases, prostheses were used to repair the hernias. In 127 (2.8%) patients, the use of mesh patches was not documented.
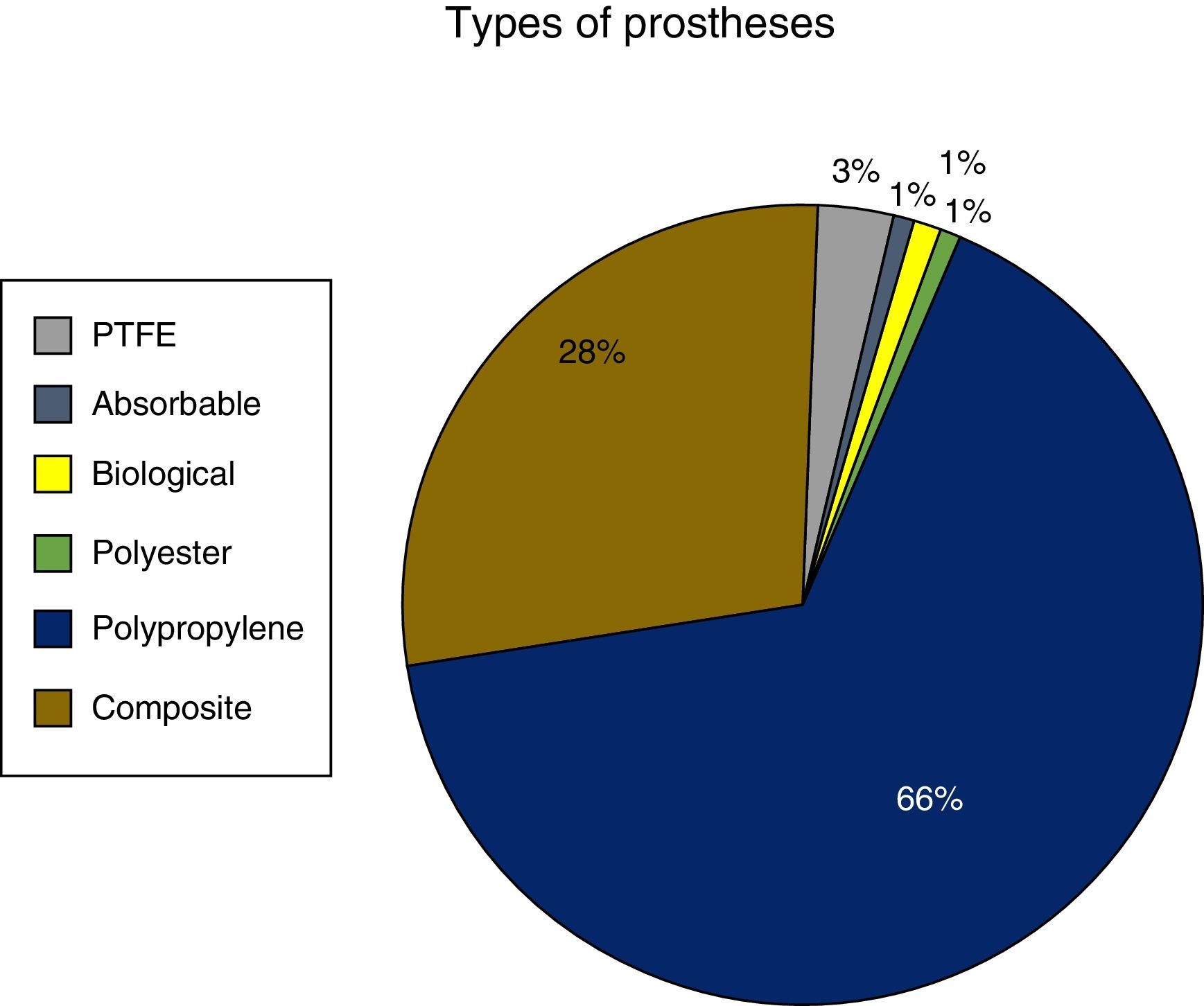
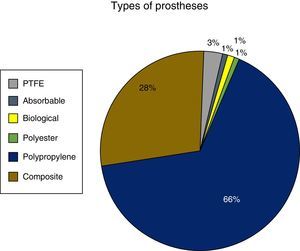
Fig. 1 shows the frequency distribution of the mesh types used. Most repairs were done with polypropylene mesh (66%), followed by composite mesh (28%). Biological implants were hardly used (n=30; 0.7%).
When we analyzed only those patients who received a mesh and were treated by laparotomy (n=3789), the suprafascial position (onlay) was the most frequently used (n=1930, 50.9%). The mesh was placed in either the retromuscular or preperitoneal position (sublay) in 1380 hernias (36.4%). The mesh was used as a bridge (inlay) in 141 cases (n=3.7%), and 2 prostheses were implanted in different positions (combination of a suprafascial prosthesis with a second retromuscular or intraperitoneal prosthesis) in 8.9% of the operations (n=338). In 16.3% of all operations performed by laparotomy (n=617), a separation of components was required.
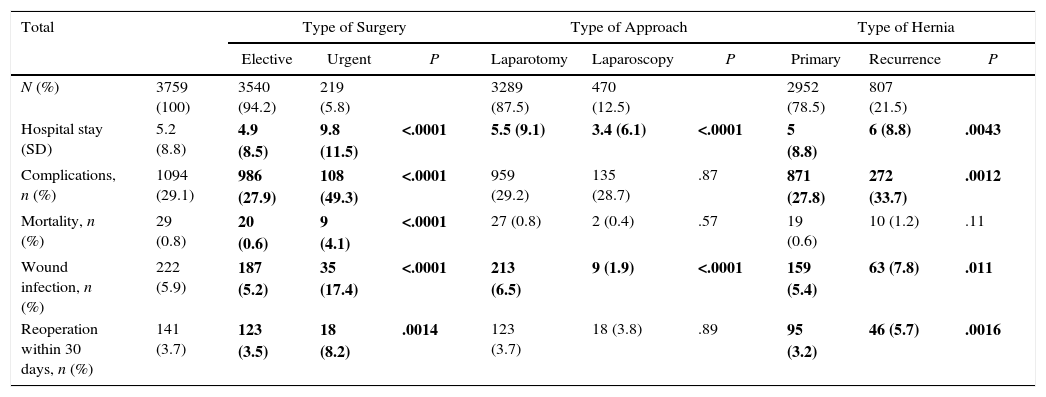
Table 3 summarizes the results of the surgical interventions of the 3759 cases for which we have postoperative data available. Mean hospital stay was 5.2 days, with a significantly longer mean stay in cases that were treated urgently (P<.0001) and shorter stays in laparoscopic hernia repairs (P<.0001).
Postoperative Results.
| Total | Type of Surgery | Type of Approach | Type of Hernia | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Elective | Urgent | P | Laparotomy | Laparoscopy | P | Primary | Recurrence | P | ||
| N (%) | 3759 (100) | 3540 (94.2) | 219 (5.8) | 3289 (87.5) | 470 (12.5) | 2952 (78.5) | 807 (21.5) | |||
| Hospital stay (SD) | 5.2 (8.8) | 4.9 (8.5) | 9.8 (11.5) | <.0001 | 5.5 (9.1) | 3.4 (6.1) | <.0001 | 5 (8.8) | 6 (8.8) | .0043 |
| Complications, n (%) | 1094 (29.1) | 986 (27.9) | 108 (49.3) | <.0001 | 959 (29.2) | 135 (28.7) | .87 | 871 (27.8) | 272 (33.7) | .0012 |
| Mortality, n (%) | 29 (0.8) | 20 (0.6) | 9 (4.1) | <.0001 | 27 (0.8) | 2 (0.4) | .57 | 19 (0.6) | 10 (1.2) | .11 |
| Wound infection, n (%) | 222 (5.9) | 187 (5.2) | 35 (17.4) | <.0001 | 213 (6.5) | 9 (1.9) | <.0001 | 159 (5.4) | 63 (7.8) | .011 |
| Reoperation within 30 days, n (%) | 141 (3.7) | 123 (3.5) | 18 (8.2) | .0014 | 123 (3.7) | 18 (3.8) | .89 | 95 (3.2) | 46 (5.7) | .0016 |
Statistically significant results are shown in bold.
Complications appeared in 29.1% of the cases. The most frequent (80.3% of the total; 879 patients) were related with the surgical incision (hematoma, seroma, and wound infection). Mortality was low (0.8%). A total of 141 patients (3.7%) were reoperated during the first 30 postoperative days. The most frequent causes of reoperation were related with the surgical wound (n=69; 48.9%): hematoma/hemorrhage (n=19); seroma (n=4); wound infection or necrosis (n=54), and others (n=2). Visceral complications arose in 43 cases (30.5%): intestinal perforation (n=16); anastomotic dehiscence (n=4); non-digestive visceral lesion (n=1); bowel obstruction (n=17); mesenteric ischemia (n=4); and hemoperitoneum (n=1). Lastly, 15 patients (10.6%) were reoperated for early recurrence, with an incidence of immediate relapse in the series of 0.4%.
All complications were significantly higher in the group of patients that had undergone urgent surgery. With the exception of mortality, recurrent hernias had a higher rate of complications compared to primary hernias (33.7% vs. 27.8%; P=.0012). In laparoscopic surgery, wound infection was significantly lower than in open surgery (1.9% vs. 6.5%, P<.0001).
We have follow-up data for 1566 cases (35.0%; mean 9.5 months; median 7.7 months). Late-onset complications (chronic infection, chronic pain, or recurrence) were recorded in 316 (20.5%).
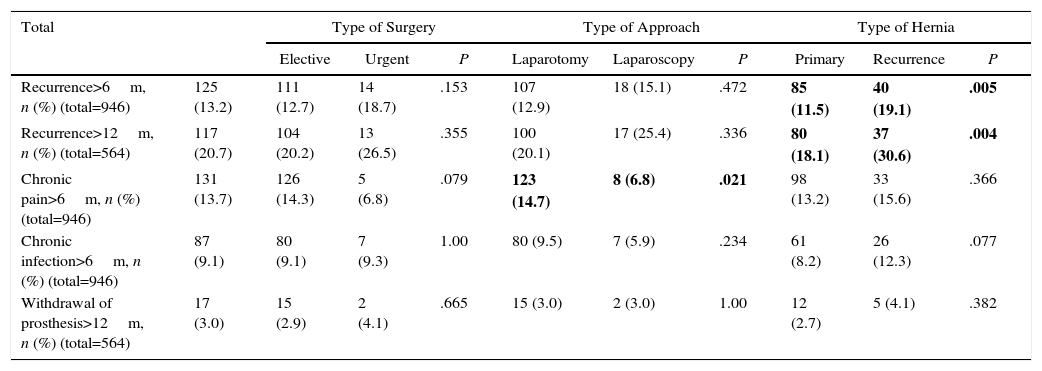
Table 4 shows the follow-up data distributed by groups of records that were monitored for more than 6 months (n=946; 24.3%; median follow-up 12.4 months), and more than one year (n=564; 17.9%; median follow-up 16.4 months). Of note is the high and increasing frequency of recurrences as the follow-up increases (13.2% in cases followed 6 or more months and 20.7% in follow-ups of more than one year), with a higher rate in hernias treated for recurrence of a previous repair after 6 months (P=.005) as well as one year (P=.004).
Postoperative Follow-Up and Late-Onset Complications.
| Total | Type of Surgery | Type of Approach | Type of Hernia | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Elective | Urgent | P | Laparotomy | Laparoscopy | P | Primary | Recurrence | P | ||
| Recurrence>6m, n (%) (total=946) | 125 (13.2) | 111 (12.7) | 14 (18.7) | .153 | 107 (12.9) | 18 (15.1) | .472 | 85 (11.5) | 40 (19.1) | .005 |
| Recurrence>12m, n (%) (total=564) | 117 (20.7) | 104 (20.2) | 13 (26.5) | .355 | 100 (20.1) | 17 (25.4) | .336 | 80 (18.1) | 37 (30.6) | .004 |
| Chronic pain>6m, n (%) (total=946) | 131 (13.7) | 126 (14.3) | 5 (6.8) | .079 | 123 (14.7) | 8 (6.8) | .021 | 98 (13.2) | 33 (15.6) | .366 |
| Chronic infection>6m, n (%) (total=946) | 87 (9.1) | 80 (9.1) | 7 (9.3) | 1.00 | 80 (9.5) | 7 (5.9) | .234 | 61 (8.2) | 26 (12.3) | .077 |
| Withdrawal of prosthesis>12m, n (%) (total=564) | 17 (3.0) | 15 (2.9) | 2 (4.1) | .665 | 15 (3.0) | 2 (3.0) | 1.00 | 12 (2.7) | 5 (4.1) | .382 |
Statistically significant results are shown in bold.
The analysis of the EVEREG results has corroborated the data from other incisional hernia registries10,11 and has confirmed the need to register the results of this disease and probably those of other highly prevalent conditions affecting the abdominal wall.
The first point for improvement of hernia registries would be participation. The voluntary registration system with external financing used in this case, as in other platforms,9 is not optimal. Its voluntary nature means that only the most motivated surgeons participate in this initiative. Therefore, the absence of mandatory registration in our territory probably produces a significant bias in the results, so that we are only at the tip of the iceberg of the problem. Likewise, dependence on external financing, in our case, raises doubts about the longevity of this registry.
We consider the data collected to be reliable because of the motivation of the participants, but there is unequal participation, and some hospitals started out with great momentum only to lose speed over time. In this context, it would be ideal to have either an incentive to register or to make the registration of this activity mandatory or remunerated within the public healthcare system.
Another problem is that hernias are collected rather than patients, and there is no possible individual follow-up. In the current situation, this is the only possible way to store the data on a non-institutional server and preserve patient privacy. This problem affects other European registries that lack the support of the public healthcare administration. However, if we consider only primary repairs, we are reasonably sure that these patients are not duplicated.
The analysis of the demographic data of the cases indicates that incisional hernias appear predominantly in female patients who are older than 60, obese and have a high frequency of associated disease. This is even more pronounced in cases with urgent surgery and recurrent hernias, in which patients are more obese and have significantly higher surgical risk. Therefore, these circumstances must be taken into account during the initial laparotomy in order to maximize precautions during closure or to apply prophylactic measures.
Regarding the surgical approach, the limited use of laparoscopy, which was only used in 11.7% of the cases, is noteworthy. This datum is differential in our country when compared to other registries in which laparoscopy reaches more than 50%.10 A detailed analysis of the reasons for this low use of laparoscopy and measures to increase its utilization is another area that needs improvement.
A very interesting fact is that, in view of what has been collected, a large number of complex hernias were treated surgically. If we consider only recurrent hernias (considered complex by definition),12 more than 22% of the operated hernias met this criterion. The same happened with the percentage of patients with component separation (16.3% of those operated by open surgery). All this is likely to be due to a selection bias due to the predominant participation in the registry of departments that have divisions specialized in abdominal wall surgery.
The postoperative results are similar to those reported in the series of incisional hernias6,10,11: high frequency of minor wound-related complications, increased incidence of complications in urgent surgery and recurrent hernias, and low overall mortality, although especially elevated in patients undergoing urgent surgery.13
Regarding the surgical technique, it is interesting that a significant number of repairs (n=31) are still performed without prostheses, which, in our opinion, seems exceptional, especially when we verified that most of these patients underwent scheduled surgery. This fact has also been detected in other registries, with even higher percentages.10 Although we only have follow-up for more than one year in 9 of them, 4 relapses have been diagnosed (44.4%). Therefore, it once again seems clear that mesh should be used whenever possible in the repair of incisional hernias, as indicated in the literature.14,15
Another notable technical fact is the clear preference of surgeons for the placement of mesh in the suprafascial (onlay) position as opposed to the preference for the retromuscular position (sublay) in the rest of Europe and in the recommendations of certain groups.10,16,17 This shows, as other authors indicate,10 that there are no unanimous criteria for the use of mesh, their position or even the fixation system.
Regarding follow-up, we have observed that patients are subject to poor follow-up, which contributes to the lack of awareness of the actual results of this surgery. It is common for patients to undergo surgery and not be reviewed until one month after surgery. This is probably the main Achilles’ heel of our results, fostered by the usual dynamics of public hospitals in which patient follow-up is not at all promoted and, given the high prevalence of this disease, would be an additional work overload. Just as in neoplasms, it is clear that follow-up studies should be very long (more than 10 years), although this has not been happening in abdominal wall diseases.
Finally, if we consider the figures detected by the registry, we are facing a disturbing situation of incisional hernia recurrences that affects about 20% of patients followed more than one year, with no differences among the different groups. Thus, although there are other late complications (chronic infection and chronic pain), in our opinion, currently the first objective should be to reduce the recurrence rate, as has been done in the case of inguinal hernias. This fact is not exclusive to our registry and is similar to publications by other authors.10
Briefly, the main strengths of the registry are: thoroughness of the data collection; the high number of patients collected; and, the commitment of a relevant number of surgeons in the country to collaborate in the initiative. The main weakness is the lack of uniform treatment criteria and insufficient long-term follow-up, which implies that the rates of late complications need to be carefully analyzed and require updating in order to draw more reliable conclusions.
To conclude, the EVEREG registry is a useful tool to determine the true situation of incisional hernia treatment in Spain. It is necessary to improve and increase data collection in the registry and, particularly, to increase patient follow-up. Also, it is essential to ensure that the largest number possible of General Surgery Departments register their data so that the analysis of the registry is as close as possible to the actual results of the country. The analysis of the data collected to date shows that it is necessary to introduce relevant improvements in the treatment of this disease, especially in terms of reducing the number of recurrences. Therefore, in addition to making progress in the case registration and updating process, comparative studies should be initiated to improve the results obtained until now.
FundingB. Braun has funded the design and storage costs of the EVEREG database.
Conflicts of InterestsThe authors must declare if they are consultants of some prosthetic company and that entails remuneration some.
The authors would like to thank SAIL and Silvia Glahn (B. Braun).
Antonio Utrera González, Hospital Juan Ramón Jiménez, Huelva
José M, Capitán Vallvey, Complejo Hospitalario de Jaén, Jaén
Juan A, Bellido Luque, Hospital Riotinto, Huelva
Paloma Rey, Hospital Comarcal de la Axarquía, Málaga
Matías Pradas, Hospital Comarcal de Ronda, Ronda
Manuel Bustos, Hospital Virgen del Rocío, Sevilla
Joaquim Robres Puig, Consorci Sanitari Integral de l’Hospitalet, Barcelona
Rafael Villalobos, Hospital Arnau de Vilanova, Lérida
Lidia Blay, Hospital de Igualada, Barcelona
Marcos Solà, Hospital de Manresa, Manresa
Miguel Fernández-Layos, Hospital de Manresa, Manresa
Dolors Güell Puigcercos, Hospital de Terrassa, Terrassa
Verónica Alonso, Hospital Dos de Maig, Barcelona
Vicente Ayuso Osuna, Hospital Espíritu Santo, Santa Coloma de Gramanet
Carles Olona Casas, Hospital Joan XXIII, Tarragona
Francisco Martínez Ródenas, Hospital Municipal de Badalona, Badalona
Vasile Veste, Hospital de Olot, Olot,
Jordi Comajuncosas, Hospital Parc Sanitari Sant Joan de Deu, Sant Boi
Carlos Javier Gómez Díaz, Hospital Parc Taulí, Sabadell
Oscar Colomer, Hospital Parc Taulí, Sabadell
Magda Abelló Sala, Hospital Pius, Valls
Carlos Houyuela Alonso, Hospital Plató, Barcelona
Francesc Marsal, Hospital Santa Tecla, Tarragona
Agustín Juan Cano Maldonado, Complejo Hospitalario Universitario, Cartagena
Juan Manuel Rueda Pérez, Complejo Hospitalario Universitario, Cartagena
Rosa Gamón, Hospital General de Castellón, Castellón
Pedro García Peche, Hospital General Universitario Reina Sofía, Elche
Miguel González Valverde, Hospital General Universitario Reina Sofía, Elche
Ramón J, Ferri, Hospital Lluís Alcanyís, Valencia
Elena Martí Ciñat, Hospital Malvarrosa, Valencia
Vicente Barbero, Complejo Hospitalario Virgen de la Salud, Toledo
Fernando Fernández Bueno, Hospital Central de la Defensa, Madrid
Isabel Delgado Lillo, Hospital Clínico San Carlos, Madrid
Juan Jesús Cabeza Gómez, Hospital Clínico San Carlos, Madrid
Joaquín Picazo Yeste, Hospital General de La Mancha, Ciudad Real
Antonio López, Hospital Nuestra Señora del Prado, Talavera de la Reina
José Luis Porrero Carro, Hospital Santa Cristina, Madrid
Teresa Butrón, Hospital Universitario 12 de Octubre, Madrid
Miguel Ángel García Ureña, Hospital Universitario del Henares, Alcalá de Henares
Marta de Mingo, Hospital Universitario Infanta Elena, Madrid
Javier Granell, Hospital Universitario Príncipe de Asturias, Alcalá de Henares
Lucas Blázquez Latre, Complejo Hospitalario de Navarra, Pamplona
Enrique Sanemeterio, Hospital Comarcal de Laredo, Santander
Esther Guisasola, Hospital Universitario, San Sebastián
Ernesto Tobalina Aguirrezábal, Hospital Universitario, Galdakao
Ángel Zorraquino, Hospital de Basurto, Bilbao
Please cite this article as: Pereira JA, López-Cano M, Hernández-Granados P, Feliu X, en representación del grupo EVEREG. Resultados iniciales del Registro Español de Hernia Incisional. Cir Esp. 2016;94:595–602.