This prospective, observational study evaluated transanal dearterialization (THD) efficacy and safety in grade 2–4 hemorrhoids (HD).
MethodsTHD was performed under sedation-locoregional anesthesia in 402 outpatients. Patients had follow-up evaluation 3 days, 2 weeks, 1, 6 and 12 months postoperatively. Postoperative complications and recurrence of symptoms at 12 months were analyzed. The relationship between the learning curve and the number of postoperative complications was studied.
ResultsMean patient age was 46.4 (range 20–85) years. A total of 268 patients (66.6%) were male. Sixteen patients (4.0%) had grade 2 HD, 210 (52.2%) had grade 3 and 176 (43.8%) had grade 4 HD. Surgery lasted 23 (17–34) min. A total of 67 patients had complications: bleeding in 10 patients (2.5%), hemorrhoidal thromboses in 10 (2.5%), perianal fistulas in 5 (1.2%), fissures in 14 (3.5%), urinary retention in 3 (0.8%), residual prolapse in 19 (4.7%), severe anal pain in 3 (0.8%), and perianal abscess in 3 patients (0.8%). Recurrent HD occurred in 6.3% (1/16) of grade 2 HD patients, 5.8% (12/210) of grade 3 patients and 9.7% (17/176) of grade 4 patients. Twelve months after THD, bleeding was controlled in 363 patients (90.5%), prolapse was controlled in 391 (97.3%) and pain markedly improved in 390 patients (97%).
ConclusionTHD appears safe and effective for grade 2–4 HD, and the number of complications decreased with increasing surgeon experience. THD advantages include mild pain, fast recovery, early return to daily activities and low incidence of complications.
El objetivo de este estudio fue evaluar la eficacia y seguridad de la desarterialización hemorroidal transanal (THD) para hemorroides (HD) de grado II-IV.
MétodosEstudio observacional prospectivo de una serie de 402 pacientes a los que se les realizó una THD en régimen de cirugía ambulatoria con analgosedación y anestesia locorregional. Se visitó a los pacientes a los 3 días; 2 semanas, 1, 6 y 12 meses después de la cirugía. Se analizaron las complicaciones postoperatorias y la recurrencia de síntomas a los 12 meses. Se estudió la relación entre la curva de aprendizaje y el número de complicaciones postoperatoria.
ResultadosLa media de edad de los pacientes era 46,4 años (rango: 20-85); 268 pacientes (66,6%) eran hombres; 16 pacientes (4,0%) presentaban HD de grado ii; 210 (52,2%), HD de grado iii y 176 (43,8%), HD de grado iv. La cirugía duró 23 (17-34) min. Hubo complicaciones postoperatorias en 67 pacientes: hemorragia en 10 pacientes (2,5%), trombosis hemorroidal en 10 (2,5%), fístula perianal en 5 (1,2%), fisura en 14 (3,5%), retención urinaria en 3 (0,8%), prolapso residual en 19 (4,7%), dolor anal intenso en 3 (0,8%) y absceso perianal en 3 pacientes (0,8%). La enfermedad hemorroidal recidivó en el 6,3% (1/16) de los pacientes con HD de grado II, en el 5,8% (12/210) de los pacientes con HD de grado III y en el 9,7% (17/176) de los pacientes con HD de grado IV. Doce meses después de la THD, la hemorragia se había solucionado en 363 pacientes (90,5%), el prolapso en 391 (97,3%) y el dolor mejoró significativamente en 390 pacientes (97%).
ConclusiónLa THD es un método seguro y eficaz para las hemorroides de los grados II-IV. Se caracteriza por dolor moderado, recuperación rápida, pronto retorno a las actividades de la vida diaria y baja incidencia de complicaciones.
The incidence of hemorrhoids increases with age, and at least 50% of adults over the age of 50 present some type of hemorrhoid symptoms.1 Hemorrhoidal disease (HD) can cause a considerably negative impact on patients’ quality of life and social wellbeing.2 The treatment of HD has improved progressively during recent decades and has become less invasive and less painful with the introduction of safer procedures in outpatient clinical practice. Low-grade HD is treated satisfactorily with less invasive treatments. The disadvantages of these less invasive methods include the possibility of having to repeat the procedures, recurrence in high-grade HD and the risk of uncommon although serious complications, such as intense pain, bleeding or infection.3–5
The technological advances made in recent years have provided for the development of innovative survival interventions that are less invasive and offer good control of the symptoms with only mild postoperative pain. Stapled hemorrhoidectomy is a procedure introduced by Longo that involves the resection of the rectal mucosa, but it is not considered less invasive.6,7 Transanal hemorrhoid dearterialization (THD) is an innovative, minimally invasive technique introduced by Morinaga in 1995.8 The selective ligation of the terminal branches of the superior rectal artery (SRA) is the cornerstone of the THD technique.8 The objective of this study is to present our experience and results after the use of THD in 408 consecutive ambulatory patients at one single hospital during a period of more than 4 years. Furthermore, the objective of this study was to analyze whether there was a relationship between surgical experience (learning curve) and the number of complications after a THD procedure.
MethodsThe aim of this prospective and observational study was to treat grade II–IV HD. We collected data for 402 patients during a 5-year period (May 2010–December 2014) at the only surgical center in Spain where the THD method was being used.
The preoperative evaluation included proctological examination and an interview. In accordance with the current recommendations for the treatment of HD, THD was only used in those cases in which conservative medical treatment (dietary modifications, stool softeners, topical, and systemic analgesia) and certain simple procedures (rubber band ligation and sclerotherapy) had been used without success.9 When indicated, the patients once again visited the clinic for additional examination and treatment. The night before and the morning of the surgery, enemas were administered with anorectal preparation. All the procedures were done in the outpatient setting, with combined analgosedation and local anesthesia (perianal blockade). Standard intraoperative follow-up included ECG and blood pressure monitoring with pulse oximetry, all non-invasive. After the insertion of the intravenous cannula, all the patients received intravenous antibiotic prophylaxis with 1.0g cefazolin and 500mg metronidazole. The study was approved by the hospital Ethics Committee and all the patients gave their written informed consent before entering into the study.
The local anesthesia solution utilized for the perianal blockade was prepared by mixing 15ml of lidocaine hydrochloride 2% (Galenika, Belgrade, Serbia) with 15ml bupivacaine hydrochloride 0.5% (Marcain, AstraZeneca, Luton, United Kingdom), 10ml NaCl 0.9% and 2ml solution of epinephrine 1:10000 (Adrenalin, Jugoremedia, Zrenjanin, Serbia). 20ml of this solution were injected superficially in the rhombus and 20ml were injected deep in the 4perianal sectors. Intraoperative analgosedation was comprised of midazolam and propofol administered by an expert anesthesiologist.
All the THD procedures were conducted in the lithotomy position with the THD device (THD slide S.p.A., Correggio, Italy) and a special proctoscope equipped with a Doppler catheter and light source.10 The Doppler catheter was aimed toward the surgical window, which allowed for the identification of the artery within the window so it could be ligated selectively.8
The circumference of the lower rectum was divided into 6 sectors (left anterolateral, left lateral, left posterolateral, right posterolateral, right lateral, and right anterolateral) corresponding with the clock positions of 1, 3, 5, 7, 9, and 11 o’clock.11 In addition to the dearterialization of the hemorrhoidal plexus, the procedure often entails mucopexy, which is done with a continuous suture of the mucosa.
We used 2-0 Truglyde absorbable polyglycolic acid suture with a 5/8inch needle and 26.5mm of THD. The last step exposed the rectal mucosa in order to carry out the mucopexy with direct visualization so that it was completely passed through until the proximal vertex of the internal hemorrhoid above the anocutaneous line. Afterwards, the suture was tied loosely in order to lift the prolapse.
At the end of the procedure, a hemostatic sponge (THD Spon-anal, absorbable gelatin sponge) was inserted in the anal duct. The sponge was eliminated with the first bowel movement, but it could also be eliminated beforehand if the patient experienced significant discomfort.
All the interventions were performed by either of the 2 surgeons (MD or ZB). The patients were discharged at least 3h after the conclusion of the surgery and after having met all the criteria for discharge. At the time of discharge, all patients received instructions about treatment with prophylactic antibiotics (500mg of metronidazole in tablets, 3 times a day for 5 days) and the appropriate use of analgesia (1g of paracetamol every 6h for 2 days) and laxatives (Transilane, ispaghula powder for oral suspension 2 times per day). Postoperative pain was measured in all patients with a 4-point Likert-type scale (1=no pain; 2=mild pain; 3=moderate pain; and 4=intense pain).
Patients returned for a follow-up evaluation after 3 days, 2 weeks and 1, 6, and 12 months after surgery. Furthermore, patients were contacted by telephone for daily follow-up until the first follow-up office visit on the third day post-op. The follow-up interviews included questions about the intensity of pain, temperature, bowel movements, and elimination of the anal sponge. On the first postoperative visit, on the third day, the patients received advice about hygiene and diet, and their anal region was examined. The patients were scheduled for additional follow-up visits for 14 days and one, 6 and 12 months after THD, and during these visits there were examined digitally and with anoscopy. Success of the procedure was defined as a significant reduction or resolution of hemorrhoidal bleeding, pain, pressure, and prolapse.
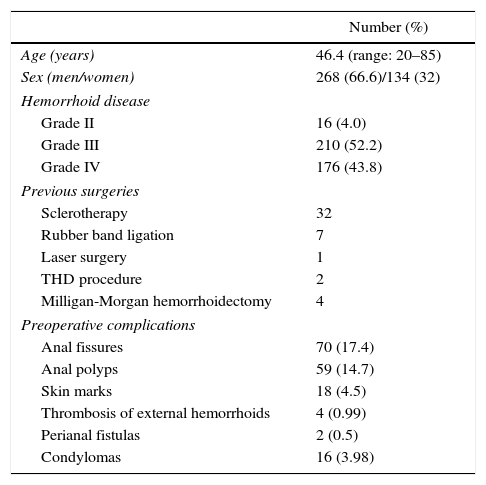
ResultsFrom May 2010 to December 2014, 402 outpatients underwent THD with mucopexy of the mucosa/submucosa. Preoperative inspection revealed ulcerous colitis in 2 patients, spastic colon in one and anal cancer in another 2 patients. The personal and clinical data, including previous treatments and preoperative HD complications, are shown in Table 1.
Personal Data, Previous Surgeries, and Preoperative Complications of the Hemorrhoidal Disease.
| Number (%) | |
|---|---|
| Age (years) | 46.4 (range: 20–85) |
| Sex (men/women) | 268 (66.6)/134 (32) |
| Hemorrhoid disease | |
| Grade II | 16 (4.0) |
| Grade III | 210 (52.2) |
| Grade IV | 176 (43.8) |
| Previous surgeries | |
| Sclerotherapy | 32 |
| Rubber band ligation | 7 |
| Laser surgery | 1 |
| THD procedure | 2 |
| Milligan-Morgan hemorrhoidectomy | 4 |
| Preoperative complications | |
| Anal fissures | 70 (17.4) |
| Anal polyps | 59 (14.7) |
| Skin marks | 18 (4.5) |
| Thrombosis of external hemorrhoids | 4 (0.99) |
| Perianal fistulas | 2 (0.5) |
| Condylomas | 16 (3.98) |
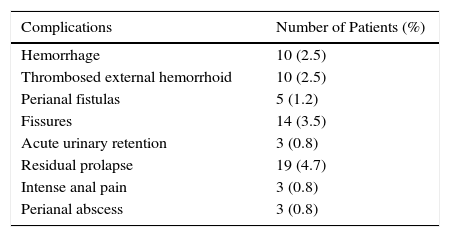
In most cases, the 6 terminal branches of the SRA were located at the 1, 3, 5, 7, 9, and 11 o’clock positions. However, in some cases a clear Doppler signal was detected for secondary hemorrhoidal branches, and sutures were made at those specific point. After the identification of the artery with the best Doppler signal, adequate retention of the artery was confirmed when the Doppler signal was eliminated or significantly reduced after removing the suture and performing a “Z suture”. After tying each suture, the dearterialization was concluded.12 In one case, the delayed bleeding after THD led us to carry out diagnostic colonoscopy, which revealed right colon cancer that had not been diagnosed previously. Postoperative complications were identified and recorded in 67 patients (16.7%; Table 2).
Complications were registered in 42 patients during the first month and in 25 patients within 12 months of surgery. All the complications were treated satisfactorily, but 2 patients required hospitalization for the treatment of their complications. One patient presented a bleeding duodenal ulcer that was diagnosed in the postoperative period by gastroscopy and needed blood transfusions. The second patient was elderly, weak, confined to bed, and with a poor general state of health, who developed a perianal abscess on the sixth day post-op. Probably due to the limited postoperative mobilization, the abscess progressed in spite of the therapeutic approach with incision, drainage, and parenteral antibiotic treatment for the suprasphincter fistula, requiring temporary colostomy followed by inversion of the colostomy 3 months later.
Thirty patients (17 patients with grade IV HD, 12 patients with grade III HDand one patient with grade II HD) needed reoperation because the HD symptoms persisted: 28 patients presented recurring THD, while another 2 patients underwent hemorrhoidectomy. In 6.3% of the patients, recurrent HD was identified: in 6.3% of the patients it was grade II; in 5.7%, grade III; and in 9.7%, grade IV, but in all these patients the resolution of the symptoms was complete after the additional interventions. As the presence of marks on the skin is an expected consequence of long-term HD, it is not considered a complication (Table 1). The skin marks were resected only at the request of the patient.
In a few patients, the operation was combined in the following manner: the THD procedure was combined with polypectomy in 30 patients; with sphincterotomy in 49; with polypectomy and sphincterotomy in 16; with ablation of thrombosed external hemorrhoids in 3; with resection of skin marks in 16 and with radiofrequency ablation of condylomas in 8 patients. Sphincterotomy was repeated in 3 patients, and THD was repeated in 2 patients, both with grade IV HD.
All the procedures were done in the outpatient setting. The mean duration was 23min (range: 17–34min). During the procedure, 6.3 (range: 5–8) ligatures were made to the terminal branches of the SRA. A total of 167 patients (41.54%) reported no postoperative pain; 182 patients (45.27%) reported mild pain that required 1g of oral paracetamol every 6h for 4 days and 53 (13.19%) reported moderate pain requiring analgesia for more than 4 days.
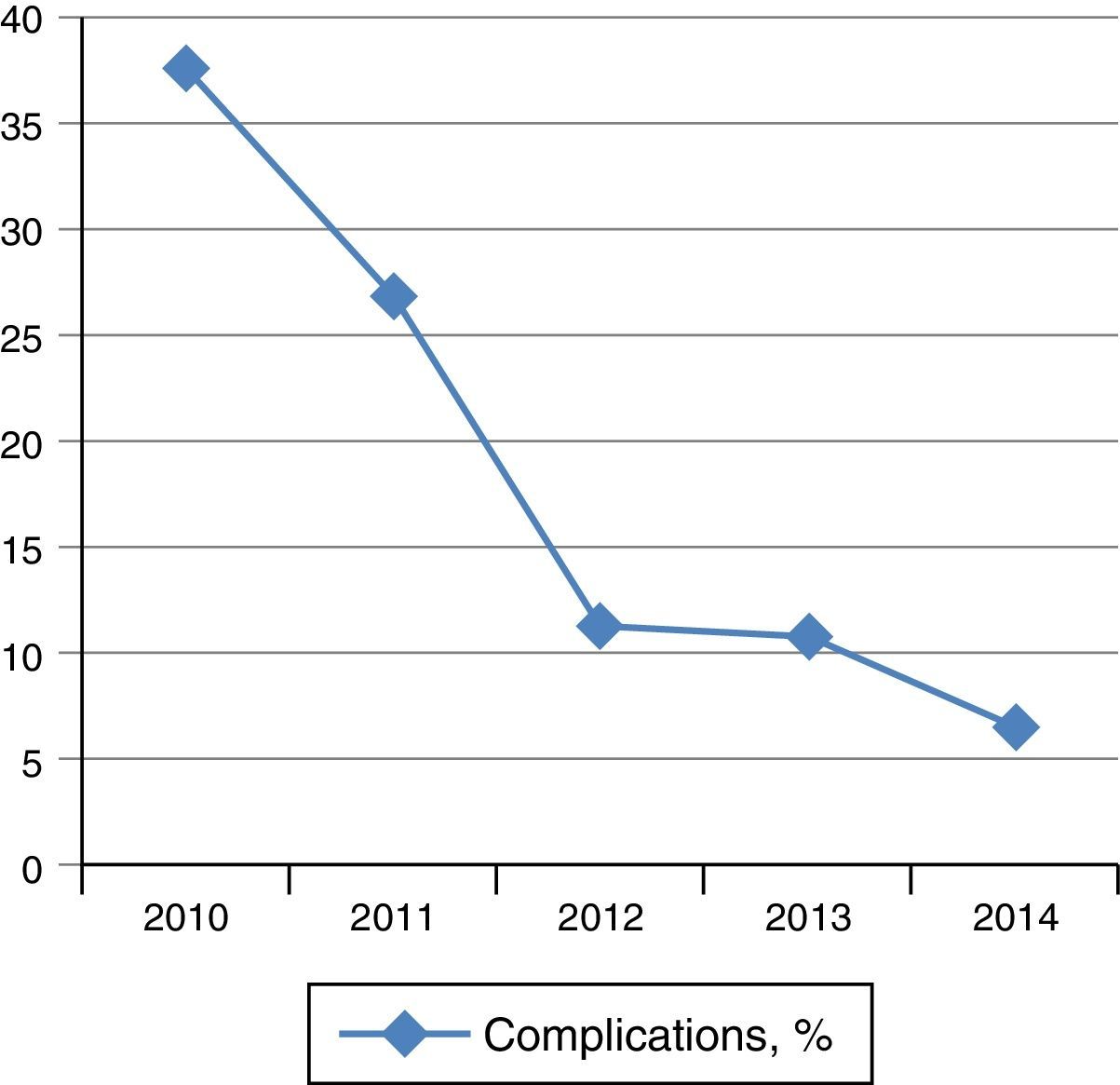
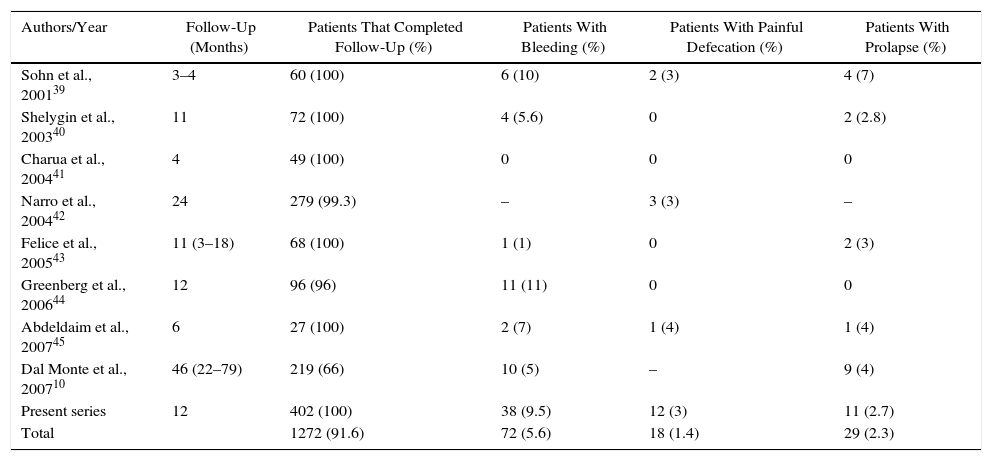
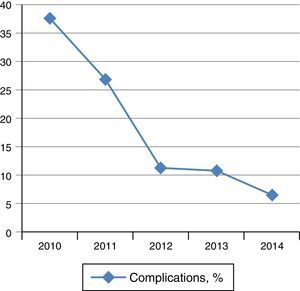
The follow-up evaluation one month after THD revealed that the prolapse, bleeding, pain, and pressure in the anal region were resolved in 97, 88, and 97% of patients, respectively. As for the long-term relief of symptoms, the hemorrhage was controlled in 90.5% of patients, prolapse in 97.3% and pain in 97% of patients 12 months after the intervention (Table 3). Two patients did not attend the scheduled follow-up visits, but the data from 400 patients, whom were followed for a maximum of 55 months, showed a clear reduction in complications from year to year, which shows that there is an obvious learning curve in the improvement of the procedure (Fig. 1).
Clinical Studies About the Treatment of Hemorrhoidal Disease with Doppler-Guided Procedures, in Order by Publication Date.
| Authors/Year | Follow-Up (Months) | Patients That Completed Follow-Up (%) | Patients With Bleeding (%) | Patients With Painful Defecation (%) | Patients With Prolapse (%) |
|---|---|---|---|---|---|
| Sohn et al., 200139 | 3–4 | 60 (100) | 6 (10) | 2 (3) | 4 (7) |
| Shelygin et al., 200340 | 11 | 72 (100) | 4 (5.6) | 0 | 2 (2.8) |
| Charua et al., 200441 | 4 | 49 (100) | 0 | 0 | 0 |
| Narro et al., 200442 | 24 | 279 (99.3) | – | 3 (3) | – |
| Felice et al., 200543 | 11 (3–18) | 68 (100) | 1 (1) | 0 | 2 (3) |
| Greenberg et al., 200644 | 12 | 96 (96) | 11 (11) | 0 | 0 |
| Abdeldaim et al., 200745 | 6 | 27 (100) | 2 (7) | 1 (4) | 1 (4) |
| Dal Monte et al., 200710 | 46 (22–79) | 219 (66) | 10 (5) | – | 9 (4) |
| Present series | 12 | 402 (100) | 38 (9.5) | 12 (3) | 11 (2.7) |
| Total | 1272 (91.6) | 72 (5.6) | 18 (1.4) | 29 (2.3) |
This study presents the data from 402 patients who underwent THD at our institution over a 4-year period. The elevated number of patients in our study is due to the fact that, for several years, our hospital has been the only center in the country to perform THD. This is the first study to present the experience of 2 surgeons who conducted THD in a large number of patients at a single medical center. Festen et al. stated that, compared with the procedure for prolapse and hemorrhoids, the THD procedure is “less invasive, easier to learn and less expensive”.13 As occurs with other surgical procedures, there is “learning curve” for THD, and our data show that the frequency of complications after THD decreased notably from year to year as our surgeons acquired more experience in the procedure.
The objective of the procedure was to reduce the hemorrhoids and return the hemorrhoidal cushions to an anatomical position, while restoring the physiology of the hemorrhoidal plexus with precise localization and fixation of the terminal branches of the SRA, causing the reduction in the arterial blood flow. Some authors report that the distribution of the SRA branches varies greatly and their entry points are directed at the muscle layer of the rectal wall.14 Nonetheless, in the study by Ratto et al., endorectal ultrasound was used to identify 6 sectors, where the terminal branches of the SRA pass through the circumference of the lower rectum. They proposed that the best place to perform hemorrhoid dearterialization is 2cm above the anorectal line.11 Moreover, as the placement of the arteries in this area is superficial (submucosa 2mm thick in 97% of patients), dearterialization is more precise.11
In addition to the dearterialization of the hemorrhoidal plexus, THD often involves mucopexy, which is carried out with a continuous suture of the mucosa by means of clamping and causes firmer adhesion to the deeper layers of the rectal wall due to the fibrosis.10 With this technique, there is no resection of hemorrhoids, the sensitive anoderm is avoided under the anocutaneous line, and the anal anatomy and hemorrhoid tissue are preserved. The venous drainage of hemorrhoids is aggravated by prolapse, so mucopexy corrects the venous flow of the plexus by reducing tension and regenerating connective tissue within the cushions as they diminish, which reduces the frequency of recurrences.10 Mucopexy is done with a continuous suture from the site where the artery is ligated to a level 5–10mm above the anocutaneous line,8 and the sensitive anoderm remains intact. The results of THD procedures are promising, with the recurrence of bleeding in only 5%–20% of patients in most studies13,15–17 and in 9.5% of patients in our series. The results are even better in terms of the recurrence of prolapse, which occurred in only 2.75% of the patients in our series. The prolonged mucopexy in our series probably reached a lower rate of recurrence of HD, but also caused greater pain intensity in the immediate postoperative period. Our results are similar to the data of a study by Giordano et al., in which 70% of the patients presented postoperative pain after mucopexy in grade IV HD.18
In our series, mucopexy was conducted with a continuous suture. The length of the mucopexy was significantly lower in the patients with grade II HD than in the patients with grades III and IV HD, due to a more minor prolapse. The importance of mucopexy in grades II and III HD lies in the safe ligature of terminal branches that are in the superficial submucosal layer and are sutured distally. It is recommended that the distance between each suture of the mucopexy be no larger than 0.5cm. A shorter distance between the sutures has a lesser plication effect and increases the risk for tissue ischemia, while a greater distance increases the risk of premature rupture of the continuous suture and other complications, such as bleeding and prolapse.19 The experience of our practice indicates that the last suture in the mucopexy deserves special attention and should be at least 0.5–1cm above the anocutaneous line because there is the risk for intense pain if the anoderm becomes trapped in the line of sutures.
Several patients with ulcerous colitis and spastic colon were treated with THD, with no complications. The patients with anal carcinoma were sent for evaluation and treatment of the primary disease, and the THD was canceled. No other contraindications were identified in our patients, such as fecal incontinence, rectal prolapse, hemorrhagic disorders, portal hypertension with rectal varices or Crohn's disease.
No fecal incontinence was observed in any of the patients, not even in the cases with simultaneous sphincterotomy, which is similar to a previous study published by Ratto et al.20 The Ratto study used anorectal manometry, rectal volumetric measurement and endoanal ultrasound to evaluate the impact of THD on continence and demonstrated that internal sphincterotomy leads to the repositioning of internal hemorrhoids and fixation in a normal posiition.20
Temporary urinary retention occurred in 3 cases: 2 patients required temporary catheterization, while in another patient the retention resolved spontaneously after several hours. The exact etiology of the urinary retention is unknown, although it may be related with dysfunction of the detrusor muscle or a urethral spasm reflex secondary to pain.21–23 The incidence of urinary retention has varied from 8.6 to 16.7% in different studies18,24,25 and may be influenced by intradural anesthesia, restriction of liquids, and prophylactic analgesia.18,25 The lower incidence of urinary retention observed in our study (0.8%) is explained by the type of anesthesia, which, in our series, was a combination of local anesthesia and analgosedation. Early walking and perianal blockade mean that the operations were able to be done with a very low incidence of urinary retention.26
One patient developed perianal abscess 6 days after surgery. The most plausible explanation was the sitting position in the postoperative period because the patient was older and confined to bed due to his poor health.
In accordance with published recommendations, HD was treated with THD in our study only after conservative medical treatment (diet modifications, stool softeners, topical, and systemic analgesia); rubber band ligation and sclerotherapy were used without success.9
To date, the published data support the use of THD in grades II and III HD if bleeding and pain persist in spite of conservative treatment, while the recurrence of the symptoms is a problem in cases of grade IV HD.12,13,27,28 Because the fear of postoperative pain is the main reason why some patients opt to live with HD,29 it is important to consider that, compared with conventional surgical hemorrhoidectomy, THD is better tolerated, causes significantly less postoperative pain, causes less postoperative complications, and has a faster recovery.30–32
In our study, the data were collected during telephone interviews and during office visits. Most patients complained of mild pain or none at all, while only 53 patients (13.2%) reported moderate pain and required analgesia for more than 4 days. This finding concurs with recently published studies demonstrating that the majority (some 92%) of patients obtained low scores on the visual analog pain scale (1–2 points on a scale of 10) or reported no pain after THD.10,33,34
In accordance with publications that recommend the combination of non-steroid analgesia and paracetamol for mild to moderate pain after hemorrhoidectomy, we administered paracetamol to our patients for pain after THD, although it was not always sufficient. While the use of weak or strong opiates is acceptable for moderate to intense pain,35,36 opiates have several disadvantages, including constipation.36 For this study, a 4-point Likert scale was used to evaluate pain. However, we believe it would be better if future studies evaluated pain after THD in greater detail, with the 10-point visual analog pain scale that is used more frequently.
An important limitation of this study is the fact that only 2 surgeons performed all the THD procedures at a single hospital. Consequently, the reproducibility and generalization of our good results cannot be guaranteed at other institutions. Additional studies are needed at different hospitals, performed by different surgeons, in order to evaluate the reproducibility and generalization of our findings in different settings and different patient populations.
In conclusion, our results indicate that the number of complications after THD decreases as the experience of the surgeon increases. The observed reduction in the number of complications over time is probably due to the greater experience acquired by the surgeons in the procedure over the years. This is similar to other publications that have shown lower rates of complications as the surgeons’ experience increased in other types of surgeries.37,38 The additional benefits of THD include a high rate of reduced HD symptoms, low incidence of complications in general, and very low incidence of serious complications. The data available indicate that THD is a safe, minimally invasive, non-excisional procedure based on the preservation of the anatomy and physiology of the anal canal, which can be used effectively in cases of grade II–IV HD. Studies with a greater number of patients are necessary to better define the value of THD in the treatment of HD.
Authorship/CollaborationsZB evaluated patients, performed surgical interventions, compiled data and edited the manuscript. MD evaluated patients, performed surgical interventions and compiled data. MV compiled data and edited the manuscript. IL evaluated patients and compiled data. MK analyzed data, and reviewed and completed the manuscript. DS provided the anesthesia and wrote the manuscript.
Conflict of InterestsThis study has been conducted with department funds alone. The authors have no conflicts of interest to declare.
Please cite this article as: Bjelanovic Z, Draskovic M, Veljovic M, Lekovic I, Karanikolas M, Stamenkovic D. Desarterialización hemorroidal transanal, un procedimiento seguro y eficaz para el tratamiento ambulatorio de la enfermedad hemorroidal. Cir Esp. 2016;94:588–594.