Our aim was to analyze both metabolic control and chronic complications of type 2 diabetes mellitus (T2D) patients regularly attended in primary care during a 3 years of follow-up in the Community of Madrid (Spain).
MethodsFrom 2007 to 2010 we prospectively included 3268 patients with T2D attended by 153 primary care physicians from 51 family health centers. An prospective cohort study with annual evaluation over 3 years to the same population was performed. We measured the goals of control in diabetic patients and the incidence of chronic complications of diabetes during the study period.
ResultsA significant decrease in serum glucose levels (143±42mg/dl vs 137±43mg/dl, p<0.00), HbA1c (7.09±1.2% vs 7.02±1.2%, p<0.00), total cholesterol (191.4±38mg/dl vs 181.5±36mg/dl, p<0.00), LDL cholesterol (114.7±31mg/dl vs 105.5±30mg/dl, p<0.00) and triglyceride levels (144.5±93mg/dl vs 138±84mg/dl, p<0.00) during study period was documented. On the contrary, a significant elevation in HDL cholesterol levels was observed (49.2±14mg/dl vs 49.9±16mg/dl, p<0.00). The incidence of diabetic complications throughout the study period was low, with a incidence of coronary heart disease of 6.2%, peripheral arterial disease 3%, ischemic stroke 2.8%, diabetic foot 11.2%, nephropathy 5.9%, retinopathy 4.5%, and neuropathy 3%.
ConclusionMetabolic control in T2D patients attended in primary care in the Community of Madrid throughout 3 years is adequate and is accompanied by low percent of chronic diabetic complications during this period of follow-up.
Nuestro objetivo ha sido analizar el control metabólico y las complicaciones crónicas de pacientes con diabetes mellitus tipo 2 (DM2) que acudían regularmente a consultas de asistencia primaria durante 3 años de seguimiento en la Comunidad de Madrid (España).
MétodosDesde 2007 a 2010, 153 médicos de asistencia primaria de 51 centros de salud familiares incluyeron prospectivamente 3268 pacientes con DM2. Se realizó un estudio de cohorte prospectivo con evaluación anual de la misma población durante 3 años. Se determinaron los objetivos de control y la incidencia de complicaciones crónicas de la diabetes.
ResultadosSe comprobaron descensos significativos de los niveles séricos de glucosa (143±42mg/dl frente a 137±43mg/dl, p<0,00), HbA1c (7,09±1,2% frente a 7,02±1,2%, p<0,00), colesterol total (191,4±38mg/dl frente a 181,5±36mg/dl, p<0,00), colesterol LDL (114,7±31mg/dl frente a 105,5±30mg/dl, p<0,00) y triglicéridos (144,5±93mg/dl frente a 138±84mg/dl, p<0,00) durante el período del estudio. Por el contrario, se observó una elevación significativa de los niveles de colesterol HDL (49,2±14mg/dl frente a 49,9±16mg/dl, p<0,00). La incidencia de complicaciones diabéticas durante el período del estudio fue baja: enfermedad coronaria 6,2%, enfermedad arterial periférica 3%, ictus isquémico 2,8%, pie diabético 11,2%, nefropatía 5,9%, retinopatía 4,5% y neuropatía 3%.
ConclusiónEl control metabólico de los pacientes con DM2 atendidos en asistencia primaria en la Comunidad de Madrid durante 3 años era adecuado e iba acompañado de un porcentaje bajo de complicaciones crónicas durante este período de seguimiento.
Type 2 diabetes mellitus (T2D) is one of the chronic diseases that have increased both its prevalence and incidence in the last 50 years.1,2 The prevalence is about 5% and its incidence varies from 12 to 36 per 10,000 inhabitants per year. In Spain the prevalence of T2D is around 6%, with a range from 4.8% to 18.7%, according to the population studied population.3 The PREDIMERC study the Community of Madrid refers a global prevalence of T2D of 8.1%, being higher in men (10.2%) compared to women (6%).4
Epidemiological evidence indicates that T2D is an independent risk factor for macrovascular and microvascular disease. Cardiovascular disease is one of the main causes of increased morbidity and death of T2D population. The cardiovascular risk is two-fold in T2D than in people without diabetes. In our National Health Care System, the diagnosis, treatment and follow-up of the majority of T2D patients rests on the primary care physician. Only those T2D patients with chronic complications or with difficulties in clinical management are referred to the endocrinologist. T2D is a complex disease which requires an intensive, individual approach and multidisciplinary management.5–7 It has been demonstrated that intensified treatment of T2D with adequate control of blood pressure, body mass index, serum glucose, and lipid profile is beneficial to prevent chronic complications.7–11 That is why the appropriate metabolic control with reduction and prevention of the cardiovascular risk factors have been considered the first line of treatment for T2D.12
Our aim was to analyze the grade of metabolic control and the chronic complications evolution in the setting of clinical practice in primary care through 3 years of follow-up.
Patients and methodsStudied cohortThe Diabetes Type 2 Study (Evolution Study Diabetes 2) is an observational, prospective cohort study of 3268 T2D outpatients sampled from 56 primary health care centers recruited from the metropolitan urban area of Madrid (Spain). Study patients were selected by simple random sampling by participating general practitioners (n=163) using the list of patients with a T2D diagnosis in their computerized clinical records. Data were collected by general practitioners at baseline visit (2007) and annually during the follow-up period (2007–2010). These data were recorded in electronic Case Report Forms. After collection, all data were internally audited to ensure quality. This involved randomly selecting 50 of the participating general practitioners and reviewing the clinical records they produced. There was strong data consistency (higher than 88% for all variables). The study was approved by the Institutional Review Board of the Ramón y Cajal Hospital (Madrid, Spain) and conducted in accordance with the principles of the Declaration of Helsinki.
Physical examination and analytical studyAll patients were subjected to anamnesis, physical examination, and biochemical tests. The following variables were collected at baseline visit: age, gender, and duration of T2D (years). Further data were collected at baseline and each follow-up visit: fasting plasma glucose (FPG), glycated hemoglobin (HbA1c), systolic (SBP) and diastolic blood pressure (DBP), total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), smoking status (current smoker, former smoker, non-smoker), body mass index (BMI), and history of cardiovascular events (myocardial infarction or stroke).
BMI was calculated as weight/height2 (kg/m2). Those patients with BMI ≥30kg/m2 were considered obese. Blood pressure was measured using a checked, calibrated sphygmomanometer. After a 5-min rest period a first reading was taken, followed by a second reading 5min later. The mean result was then calculated, and parameters of good control were: baseline FPG level <126mg/dl, HbA1c level of <7%, TG <150mg/dl, TC <200mg/dl, LDL-C <100mg/dl and HDL-C >50mg/dl for women and >40mg/dl for men. HbA1c was measured using high performance liquid chromatography (Diabetes Control and Complications Trial [DCCT]-aligned). We assessed the prevalence of chronic complications such as previously reported.13
Statistical analysisData are expressed as mean (mean±standard deviation (SD)) for quantitative variables of normal distribution, as median (interquartile range) for quantitative variables of normal distribution and as absolute number and percentage (%) for qualitative variables with its confidence interval (CI) 95% of the analyzed independent variables on the dependent variable. Incident of diabetic complications was analyzed using adjusted hazard ratios (HR) and corresponding 95% CI were estimated using an extension of Cox proportional hazards models for updated variables. The analysis of the results with hierarchical or multilevel models was unnecessary because there is no evidence that the variance between the primary health care centers for the HbA1c variable is different from zero (p=0.34); and the coefficient correlation intraclass has a value of 0.036. The comparative study of quantitative variables of normal distribution test was performed using Student's t-test. Finally, for comparison of proportions or percentages of qualitative variables chi-squared test was used. A value of p<0.05 was considered statistically significant. All statistical analyses were performed using SPSS (Statistical Package for the Social Sciences for Windows, version 19.0).
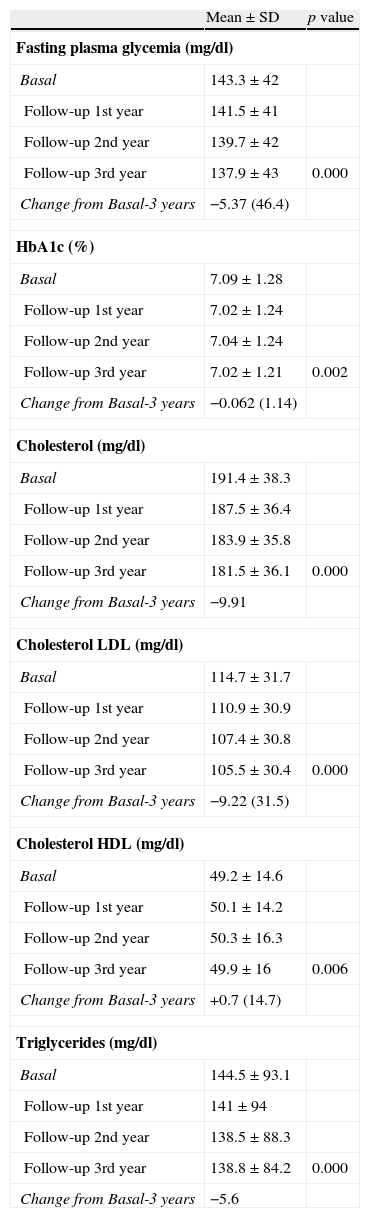
ResultsWe recruited 3268 patients with T2D (mean age 68.8±10.9 years); 49.7% women and 50.3% men; median duration of the disease 6 years (range, 1–35 years). Table 1 shows the evolution of biochemical parameters during the study period. A significance decrease in FPG levels (from 143.3mg/dl to 137.0mg/dl, p<0.00), HbA1c (from 7.09% to 7.02%, p<0.00), TC (from 191.4mg/dl to 181.5mg/dl, p<00), LDL-C (from 114.7 to 105.5mg/dl, p<0.00) and TG (from 144.5mg/dl to 138.8mg/dl, p<0.00) was observed. On the contrary, a significantly elevation in HDL-C levels (from 49.2mg/dl to 49.9mg/dl, p<0.00) was documented.
Evolution of biochemical parameters during the study.
| Mean±SD | p value | |
| Fasting plasma glycemia (mg/dl) | ||
| Basal | 143.3±42 | |
| Follow-up 1st year | 141.5±41 | |
| Follow-up 2nd year | 139.7±42 | |
| Follow-up 3rd year | 137.9±43 | 0.000 |
| Change from Basal-3 years | −5.37 (46.4) | |
| HbA1c (%) | ||
| Basal | 7.09±1.28 | |
| Follow-up 1st year | 7.02±1.24 | |
| Follow-up 2nd year | 7.04±1.24 | |
| Follow-up 3rd year | 7.02±1.21 | 0.002 |
| Change from Basal-3 years | −0.062 (1.14) | |
| Cholesterol (mg/dl) | ||
| Basal | 191.4±38.3 | |
| Follow-up 1st year | 187.5±36.4 | |
| Follow-up 2nd year | 183.9±35.8 | |
| Follow-up 3rd year | 181.5±36.1 | 0.000 |
| Change from Basal-3 years | −9.91 | |
| Cholesterol LDL (mg/dl) | ||
| Basal | 114.7±31.7 | |
| Follow-up 1st year | 110.9±30.9 | |
| Follow-up 2nd year | 107.4±30.8 | |
| Follow-up 3rd year | 105.5±30.4 | 0.000 |
| Change from Basal-3 years | −9.22 (31.5) | |
| Cholesterol HDL (mg/dl) | ||
| Basal | 49.2±14.6 | |
| Follow-up 1st year | 50.1±14.2 | |
| Follow-up 2nd year | 50.3±16.3 | |
| Follow-up 3rd year | 49.9±16 | 0.006 |
| Change from Basal-3 years | +0.7 (14.7) | |
| Triglycerides (mg/dl) | ||
| Basal | 144.5±93.1 | |
| Follow-up 1st year | 141±94 | |
| Follow-up 2nd year | 138.5±88.3 | |
| Follow-up 3rd year | 138.8±84.2 | 0.000 |
| Change from Basal-3 years | −5.6 | |
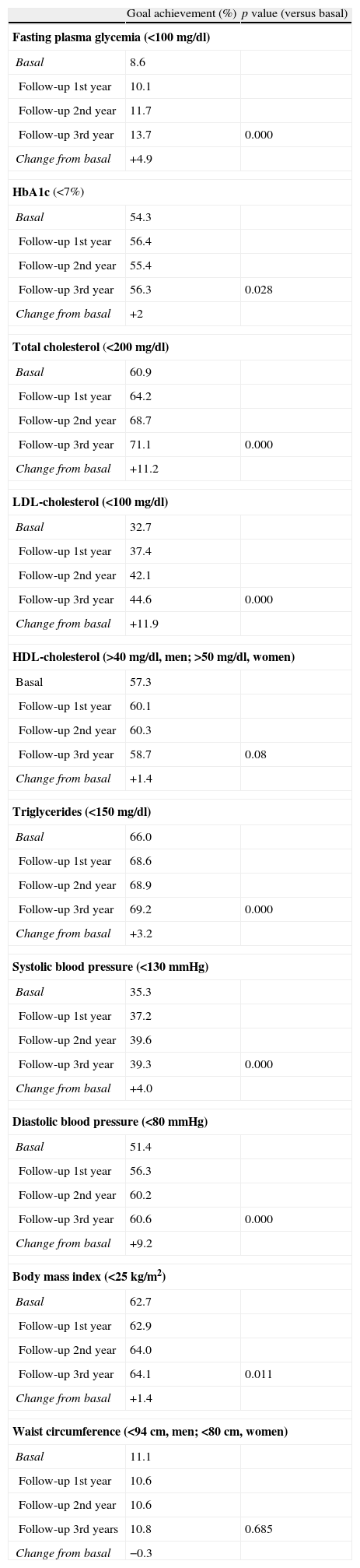
Table 2 shows the percentage of T2D patients who reached treatment goals of the American Diabetes Association (ADA).14 There was an increment of 4.9% of patients with FPG <100mg/dl, 2% with HbA1c <7%, 11.2% in TC, 11.9% in LDL-C, 1.4% in HDL-C, 3.2% in TG. There was also a significant increment of T2D patients with adequate degree of control in both SBP (4%), DBP (9.2%) and normal weight (1.4%). There was no change in waist circumference. The number of smokers decreased about 3%, with a final percentage of smokers around 11%.
Goal achievement % of T2D patients with standards of Medical Care in Diabetes Care 2012.
| Goal achievement (%) | p value (versus basal) | |
| Fasting plasma glycemia (<100mg/dl) | ||
| Basal | 8.6 | |
| Follow-up 1st year | 10.1 | |
| Follow-up 2nd year | 11.7 | |
| Follow-up 3rd year | 13.7 | 0.000 |
| Change from basal | +4.9 | |
| HbA1c (<7%) | ||
| Basal | 54.3 | |
| Follow-up 1st year | 56.4 | |
| Follow-up 2nd year | 55.4 | |
| Follow-up 3rd year | 56.3 | 0.028 |
| Change from basal | +2 | |
| Total cholesterol (<200mg/dl) | ||
| Basal | 60.9 | |
| Follow-up 1st year | 64.2 | |
| Follow-up 2nd year | 68.7 | |
| Follow-up 3rd year | 71.1 | 0.000 |
| Change from basal | +11.2 | |
| LDL-cholesterol (<100mg/dl) | ||
| Basal | 32.7 | |
| Follow-up 1st year | 37.4 | |
| Follow-up 2nd year | 42.1 | |
| Follow-up 3rd year | 44.6 | 0.000 |
| Change from basal | +11.9 | |
| HDL-cholesterol (>40mg/dl, men; >50mg/dl, women) | ||
| Basal | 57.3 | |
| Follow-up 1st year | 60.1 | |
| Follow-up 2nd year | 60.3 | |
| Follow-up 3rd year | 58.7 | 0.08 |
| Change from basal | +1.4 | |
| Triglycerides (<150mg/dl) | ||
| Basal | 66.0 | |
| Follow-up 1st year | 68.6 | |
| Follow-up 2nd year | 68.9 | |
| Follow-up 3rd year | 69.2 | 0.000 |
| Change from basal | +3.2 | |
| Systolic blood pressure (<130mmHg) | ||
| Basal | 35.3 | |
| Follow-up 1st year | 37.2 | |
| Follow-up 2nd year | 39.6 | |
| Follow-up 3rd year | 39.3 | 0.000 |
| Change from basal | +4.0 | |
| Diastolic blood pressure (<80mmHg) | ||
| Basal | 51.4 | |
| Follow-up 1st year | 56.3 | |
| Follow-up 2nd year | 60.2 | |
| Follow-up 3rd year | 60.6 | 0.000 |
| Change from basal | +9.2 | |
| Body mass index (<25kg/m2) | ||
| Basal | 62.7 | |
| Follow-up 1st year | 62.9 | |
| Follow-up 2nd year | 64.0 | |
| Follow-up 3rd year | 64.1 | 0.011 |
| Change from basal | +1.4 | |
| Waist circumference (<94cm, men; <80cm, women) | ||
| Basal | 11.1 | |
| Follow-up 1st year | 10.6 | |
| Follow-up 2nd year | 10.6 | |
| Follow-up 3rd years | 10.8 | 0.685 |
| Change from basal | −0.3 | |
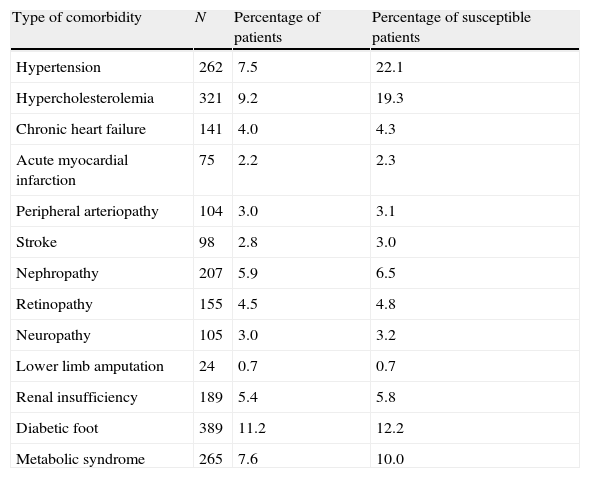
In Table 3 we can see the incidence of complications through 3 years of follow-up in our T2D population. It is important to point out the high incidence of hypercholesterolemia and hypertension and diabetic foot, especially when we study the DM2 susceptible of the complication as we can see.
Incidence of chronic diabetic complications through 3 years of follow-up.
| Type of comorbidity | N | Percentage of patients | Percentage of susceptible patients |
| Hypertension | 262 | 7.5 | 22.1 |
| Hypercholesterolemia | 321 | 9.2 | 19.3 |
| Chronic heart failure | 141 | 4.0 | 4.3 |
| Acute myocardial infarction | 75 | 2.2 | 2.3 |
| Peripheral arteriopathy | 104 | 3.0 | 3.1 |
| Stroke | 98 | 2.8 | 3.0 |
| Nephropathy | 207 | 5.9 | 6.5 |
| Retinopathy | 155 | 4.5 | 4.8 |
| Neuropathy | 105 | 3.0 | 3.2 |
| Lower limb amputation | 24 | 0.7 | 0.7 |
| Renal insufficiency | 189 | 5.4 | 5.8 |
| Diabetic foot | 389 | 11.2 | 12.2 |
| Metabolic syndrome | 265 | 7.6 | 10.0 |
We here report the results of the annual monitoring for 3 consecutive years of a cohort of 3268 T2D patients followed in daily clinical practice by primary care family physicians in the Community of Madrid (Spain). We have previously reported the degree of control of cardiovascular risk factors and prevalence of chronic complications in people with T2D in our community.13 We think that our results are interesting because, this is the first report of a important cohort of T2D, during long time (3 years of evolution), and they represent the real clinical practice of T2D and show the clinical evolution and metabolic objectives of diabetes in all the Community of Madrid. We found a good metabolic control in our T2D population with persistence over time along with a low incidence of chronic complications of T2D in the long term, as it has been previously reported in Japanese population.15 There are not many studies reported on chronic complications or they do not cover all the communities. The majority of them have been performed either in hospital population or in a low number of diabetics.16–18 In our survey, it is noteworthy the high number of recruited diabetics with a 3-year follow-up. It allows us to know not only the degree of metabolic control and health indicators in our T2D population but also the incidence of the chronic diabetic complications. We could compare with other recently published studies that also analyze the clinical practice in primary care and, in the future compare ethnical differences between groups or cultures.15
It is also important to point out the increase of the number of diabetics who reached a normal BMI <25kg/m2; however, the waist circumference did not modify, indicating that the reduction in BMI was not due to the loss of abdominal fat loss, a well known and established risk factor for insulin resistance and cardiovascular disease.
Lim et al. have reported that the first 7 days after reduced energy intake, fasting blood glucose and hepatic insulin sensitivity fell to normal and intrahepatic lipid decreased by 30%.19 Over the 8 weeks of dietary energy restriction, beta cell function increased toward normal and pancreatic fat decreased.20 Though a restriction of dietary energy intake in individuals with T2D can return of a better beta cell function and hepatic glucose output and could be responsible, at least in part, by a better HbA1c.19,20
We found an improvement over time of the treatment goals in our population. Both SBP and DBP significantly improved achieving the goals in 39.3% and 60.6% for SBP and DBP, respectively. This improvement was higher in DBP than in SBP as it has been reported by others.21 Our results regarding treatment goals related to blood pressure are better than others which got adequate good control of blood pressure in 15.1% of T2D patients.22
We know from the United Kingdom Prospective Diabetes Study (UKPDS), the first study that confirmed that T2D patients with a better glycemic control, reduced the morbidity and mortality.9 Other studies as the STENO study confirmed these results.23 On the contrary, the ACCORD study has shown, the use of intensive therapy compared with standard therapy to target normal HbA1c levels for 3.5 years increased mortality and did not significantly reduce major cardiovascular events in patients with T2D.24 In our study, we found that the mean HbA1c levels in T2D population were better than in other recent studies,23,24 and this improvement continue over time, as have been previously reported.15 We got a high percentage (55.1%) of T2D patients with HbA1c levels below <7% over the time of the study. When we study the lipids levels, we observed that the mean LDL-C significantly decreased over time with 44.6% of T2D patients with LDL-C <100mg/dl, this percentage was higher than that found in other studies.23–27 An important finding in our study, was the elevated percentage (69.2%) of T2D patients who reached TG <150mg/dl.
Another significant aim of this study was to know the incidence of chronic diabetic complications in our population. It is important to note that we found a reduced incidence of complications during the study period. We have previously reported the low baseline prevalence of complications in T2D in our population13 and we observed a similar prevalence of diabetic complications to other studies, except for retinopathy that was lower (8%) than reported (10–30%).18,28 This could be explained by underdiagnosis,28 as the retinopathy study was not registered in all patients, being collected only in 77.2% of patients. As we have referred previously, the study was performed in routine clinical practice conditions and not done in a specially selected study population. In fact, the Rochester study,29 performed under routine conditions, showed a 4-year cumulative incidence similar to that found in our study.6
Ours results are in follow-up year agreement with other studies that suggested that recent improvements in diabetes care should decrease the progression of late diabetic complications, as we can found in our study which showed a low incidence of diabetic complications, along with and a lower cardiovascular disease complications than the Oman study.30
Our study has some limitations. One of them is the possibility of occurrence of selection bias of patients, assuming that the consultant study population is not representative of the target population. Another potential bias could be the main motivation of the professionals for control and monitoring of people with T2D which could improve the results of the study. We must also note the short time of follow-up for analyzing the development of chronic complications of the disease. Another limitation of the study is that, at baseline, the patients had an excellent control of the disease. However, the study allows us to have a global vision about the T2D in our population and to analyze the evolution of those risk factors over time.8 It is important to appreciate that the patients were following by primary care, for that reason, they are not representative of the population normally attended by specialized care which usually shows higher percentage of diabetic chronic complications.
In summary, we conclude that the degree of metabolic control in T2D patients attended by primary care in the Community of Madrid (Spain) is adequate improving over time. On the other hand, the prevalence of chronic complications of T2D patients in this population is low without significant changes in the period of 3 years of follow-up.
Conflicts of interestAuthors declare no conflicts of interests for the present study.
This study was supported by the official funding agency for biomedical research of the Spanish Government, Instituto de Salud Carlos III (ISCIII), P08/90596 and PS09/00680.Investigators associated
A. Alayeto (CS Mar Báltico); A. Alonso-Menéndez (CS Las Fronteras); T. Alonso-Safont (CS Mar Báltico); B. Álvarez-Embarba (CS Hermanos Garcia-Noblejas); C.Álvarez-Hernandez (CS Canillejas); E. Álvarez-Navarro (CS Canal de Panamá); A.M. Arias-Salgado (CSPotosi); A. Arnaiz (CS Pacifico); M. Arnalte (CS Andrés Mellado); G. Artiach (CS Jazmin); S. Artola (CS María Jesús Hereza); E. Barrios (CS Cerro Almodovar); L. Barutell (CS Andrés Mellado); D. Beamud (CS Felipe II); M.J. Bedoya (CS María Jesús Hereza); C. Bello (CS Virgen del Cortijo); A. Benítez (CS Vicente Muzas); F. Blanco (CS Santa Hortensia); M. Caballero (CS Barajas); M.E. Calonge(CS Hermanos Garcia Noblejas); R. Calvo-Arregui (CS Doctor Cirajas); E. Calvo-García (CSManzanares); M. Camarero (CS Barajas); M. Canals (CS Las Calesas); A. Cano (CS Canillejas); P. Carreño (CS General Fanjul); P. Casado (CS Canillejas); S. Castellanos (CS Mirasierra); J. Castro (CSBenita de Avila); M.A. Cava (CS Ciudad Jardin); I. Cerrada (CS Campamento); C. Chamorro (CSAquitania); C. Díaz (CS Castilla La Nueva); M. Dominguez (CS Barajas); E.M. Donaire (CS Artilleros); F. Endrino (CS Doctor Cirajas); R. de Felipe (CS Pintores); R. Fernandez-Fernandez (CS Canal dePanamá); M.I. Fernández-Ferrero(CS Benita de Avila); J. Fernández-Garcia (CS Ibiza); M. Fernández-Quesada (CS Gandhi); M.R. Ferreras (CS Doctor Cirajas); M.I. Galán (CS Castillo de Uclés); P. Gallego (CS Castilla la Nueva); M.A. García-Alonso (CS Benita de Avila); S. García-Carmona (CS Hermanos García Noblejas); M.C. Garcia-Cubero (CS Alpes); F. García-García (CS Jazmin); M.I. García-García (CSLas Fronteras) E. García-Virosta (CS Canillejas); B. García-Serrano (CS Benita de Avila); P. Gil (CS Benita de Ávila); M.J. Gomara (CS Potosí); M.S. Gómez-Criado (CS Ciempozuelos); E. Gómez-Navarro (CS Estrecho de Corea); C. González-Benito (CS Artilleros); E. González-Romero (CS Rafael Alberti); C. Gonzalo (CS Castillo de Uclés); I. Hernández-Colau (CS Hermanos Garcia Noblejas); I. Herreros-Hernanz (CS Las Calesas); M.C. de Hoyos (CS Laín Entralgo); R. Iglesias-González (CS Laín Entralgo); M.J. Iglesias-Iglesias (CS Monovar); J. Innerarity (CS Sanchinarro); A. Jaime (CS Ciudad Jardín); A. Jiménez (CS Laín Entralgo); E. López-Burillo (CS Estrecho de Corea); M.C. López-Gutiérrez (CS Doctor Cirajas); E. López-Parra (CS Cerro Almodobar); C. López-Rodriguez (CS Ciudad Jardín); M.B. López-Sabater (CS Meco); L. López-Sediles (CS Pacífico); A. (CS General Fanjul); P. Martín-Calvo (CS Canal de Panamá); M.R. Martín-Cano (CS Canillejas); M. Martínez-García (CS Martín de Vargas); J. Martínez-Irazusta (CS Juncal); A. Mas (CS Virgen del Cortijo); A.I. Menéndez (CS Valleinclán); T. Mesonero (CS Ciudad Jardín); M. de Miguel (CS Virgen Del Val-Juan de Austria); C. Montejo (CS Canillejas); M.C. Montero-García (CS Ciudad Jardín); C. Montero-Lizana (CS Ciudad Jardín); A. Montilla (CS Benita de Ávila); J.R. Moracho (CS Estrecho de Corea); A. Morán (CS Juncal); A. Muñóz (CS Las Fronteras); M.A. Murchante (CS Benita de Ávila); P. Nogales (CS Las Aguilas); S. Núñez (CS Torrelaguna); O. Olmos (CS Jazmín); M.C. Ortega (CS Ciudad Jardín); I. Parra (CS Vicente Muzas); M.E. Pejenaute (CS Mar Báltico); I. Peña-Sainz (CS Jazmín); O. de la Peña (CS Rafael Alberti); C. Pérez-de la Campa (CS Doctor Cirajas); F.C. Pérez-Sánchez (CS Martín De Vargas); N. Pertierra (CS Monovar); M. Piñera (CS Avenida de Aragón); S. Pulido (CS Artilleros); G. Reviriego (CS Barajas); C. Reyes (CS Mar Báltico); G. Rodríguez-Castro (CS Benita de Ávila); C. Rodríguez-Gallego (CS Martín de Vargas); M.A. Rodríguez-Posada (CS Sanchinarro); J. Roldán (CS Castilla La Nueva); M.T. Rollán (CS María Jesús Hereza); A. Rosillo (CS Tres Cantos II); C. Ruíz (CS Castillo de Uclés); J. Sagredo (CS Los Rosales); F.J. San Andrés (CS Las Calesas); R. Santana (CS Doctor Cirajas); M.L. Santiago (CS Castilla La Nueva); M.T. Sanz-de la Fuente (CS Santa Hortensia); M.M. Sanz-Pascual (CS Alameda de Osuna); R. Sartre (CS Santa Hortensia); R. Serrano-Martín (CS Martín de Vargas); A.M. Serrano-Ortíz (CS Pavones); M.E. Serrano-Serrano (CS Los Fresnos); P. Serrano-Simarro (CS Barajas); A. Siguero (CS Canillas); A.M. Sobrado (CS Alameda de Osuna); S. Soto (CS Aquitania); M. Suarez (CS Los Rosales); J. Suero (CS Jazmin); B. de Llama (CS Entrevias), I. Tello (CS Las Fronteras); E. Tutor (CS Benita de Ávila); E. Vaquero (CS Monovar); I. Vázquez (CS Rafael Alberti); M.P. Zazo (CS Campamento); C. Zúñiga (CS Canillejas) S. Merino-Martin (CS Silvano), R. Yehuda-Salama Cohen (CS Alpes), L. de Vicente-Aymat (CS Dr. Cirajas), T. Salamanca Sánchez-Escalonilla (CS Entrevías), C. González-Fernández (CS Entrevías), A. Maestro-Martin (CS Fronteras), S. De la Iglesia-Moreno (CS García NOblejas), M. Martin-Bun (CS General anjul), M.J. Mansilla-Bermejo (CS Martin Vargas), C. Revuelto-García (CS Sanchinarro), S. Casado-González (CS Virgen del Cortijo).