We present a clinical case of a 40-year-old woman diagnosed with acute myocardial infarction (AMI) in Killip I who was admitted to our hospital. She experienced complications in the haemodynamic lab and in the operating room, including cardiogenic and anaphylactic shock requiring ventricular assist support.
Conservative management support with inotropes and vasopressors in cardiogenic shock has been shown to be insufficient in many patients to maintain adequate perfusion and prevent irreversible multiple organ dysfunction syndrome. For this reason, short-term mechanical circulatory support systems are increasing substantially. The objective of this article is to develop optimal and individualised care plans using the NANDA, NOC, NIC taxonomies.
Clinical observationAn evaluation based on Virginia Henderson’s basic needs was made, and two altered needs stood out: breathing and circulation. The patient required mechanical ventilation and mechanical circulatory support.
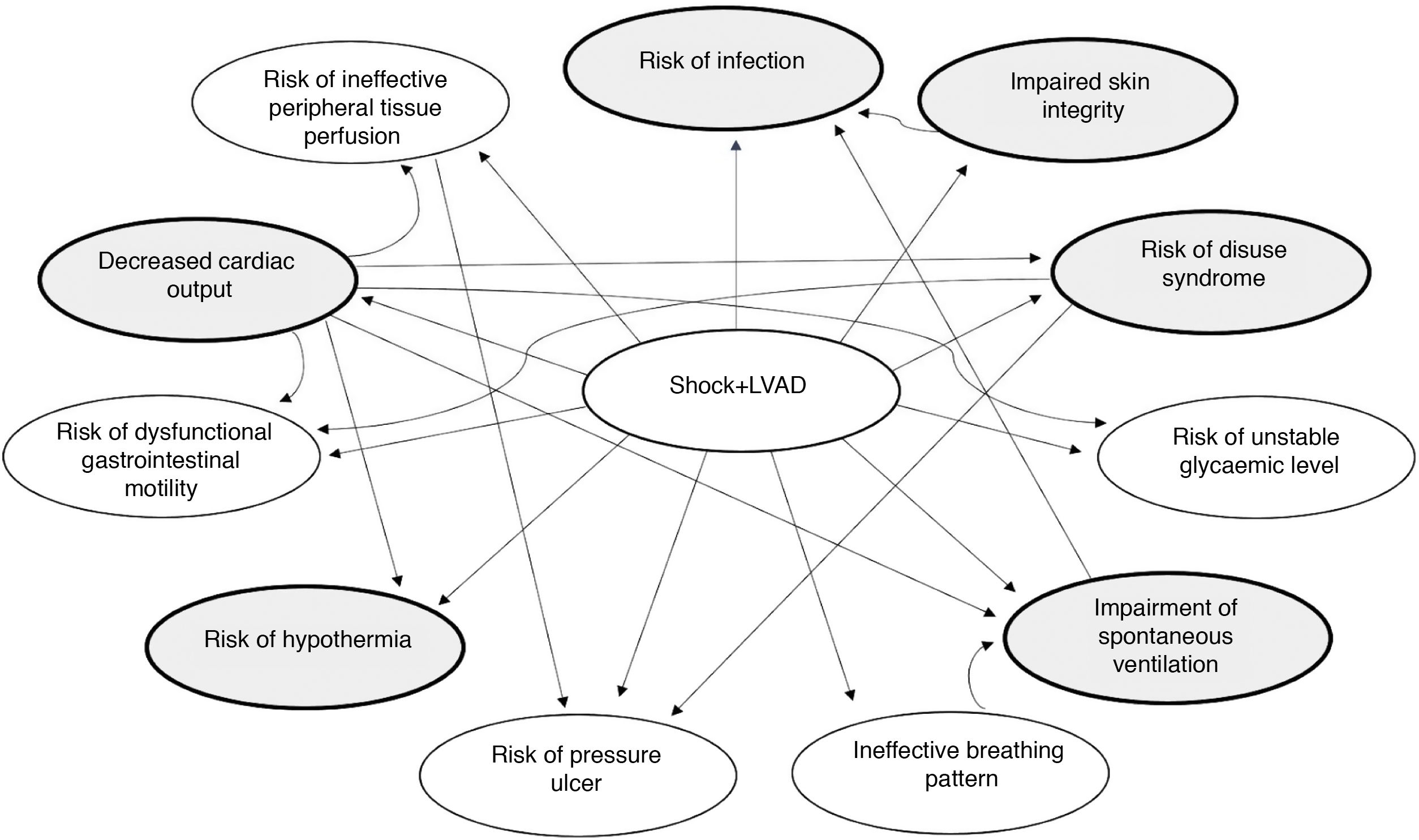
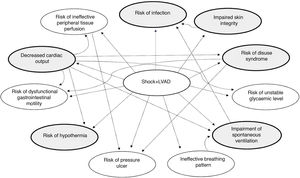
InterventionsIn relation to the highlighted needs, six diagnoses were prioritized according to the NANDA taxonomy using the Análisis de Resultado del Estado Actual (AREA) (Outcome-Present State Test (OPT)) model: risk of decreased cardiac output, impaired spontaneous ventilation, impaired tissue integrity, risk of disuse syndrome, risk of infection and risk of hypothermia.
Discussion and conclusionsOutcome criteria scores showed a favourable evolution after 96 h. The development of a standardized NANDA-NOC-NIC language allowed us to organize the nursing care plan.
Se presenta un caso clínico de una mujer de 40 años que acude a nuestro centro por infarto agudo de miocardio (IAM) en clase Killip I donde presenta una serie de complicaciones en el laboratorio de hemodinámica y quirófano, entre ellas un shock cardiogénico y anafiláctico necesitando soporte de asistencia ventricular.
El tratamiento del shock cardiogénico incluye el uso de terapias de asistencia circulatoria cuando el tratamiento médico ha sido insuficiente y pueden ser un puente a decisión ya que conceden tiempo para evaluar la situación del paciente y tener en cuenta las diferentes opciones terapéuticas existentes.
El objetivo de este artículo es desarrollar un plan de cuidados óptimo e individualizado utilizando la taxonomía NANDA-NOC-NIC.
Observación clínicaSe realizó una valoración de enfermería según las necesidades de Virginia Henderson donde destacaron dos necesidades alteradas: respiración y circulación, ya que la paciente precisó de ventilación mecánica invasiva (VMI) y requirió soporte de asistencia circulatoria mecánica.
IntervencionesDe acuerdo con las necesidades destacadas, se priorizaron seis diagnósticos según la taxonomía NANDA utilizando el modelo de Análisis de Resultado del Estado Actual (AREA): riesgo de disminución del gasto cardíaco, deterioro de la ventilación espontánea, deterioro de la integridad tisular, riesgo del síndrome de desuso, riesgo de infección y riesgo de hipotermia.
Discusión y conclusionesLos criterios de resultados evidenciaron una evolución favorable pasadas 96 h. El desarrollo del lenguaje estandarizado NANDA-NOC-NIC nos permitió organizar el plan de cuidados enfermero.
Cardiogenic shock is, by definition, circulatory failure due to a cardiac dysfunction resulting from right ventricular, left ventricular or biventricular failure.1 Cardiogenic shock occurs in 5%–7% of patients who suffer an acute myocardial infarction (AMI), being more common in those patients who have suffered an AMI with elevated ST.2
The European Society of Cardiology (ESC) guidelines contain a section exclusively devoted to cardiogenic shock and its treatment.3
Treatment for cardiogenic shock includes the use of circulatory support therapies when medical treatment has been insufficient and these can offer a bridge to decision making as they allow time to assess the patient’s situation and to consider the different therapeutic options available.3,4
Another serious complication that may occur in the haemodynamic lab treating the AMI, is allergic reaction to the iodinated contrast, leading to anaphylactic shock.5,6
The clinical case we present combines the 2 complications in the case of a 40-year-old patient who suffered a mixed cardiogenic and anaphylactic shock, requiring circulatory ventricular assist support.
The aim was to show a clinical case with presentation of a personalised care plan using NANDA-NOC-NIC7 taxonomy.
Case descriptionWe present a clinical case of a 40-year-old woman, with a history of Hodgkin’s lymphoma in 2016, who was transferred by the emergency medical services (EMS) to our centre for AMI in Killip class I. Emergency coronary angiography via right radial route was performed in which coronary artery disease of the anterior descending coronary artery was observed. Coinciding with the infusion of iodinated contrast medium the patient presented with tachycardia and hypotension, followed by an episode of bronchospasm. The patient was diagnosed with anaphylactic and cardiogenic shock and adrenaline, corticosteroids and antihistamines were administered.
She then presented with cardiorespiratory arrest (CRA) due to ventricular fibrillation and advanced cardiopulmonary resuscitation (CPR) was started, recovering spontaneous circulation after 20 min. A cardiac ultrasound was performed showing severe ventricular dysfunction with an ejection fraction of 20%.
A few minutes later she suffered a second CRA and the cardiovascular surgery team was contacted. It was decided to proceed with the implantation of an Extracorporeal Membrane Oxygenation venous artery (ECMO-VA) and an intra-aortic balloon pump (IABP) in the haemodynamics laboratory for subsequent revascularisation with thromboaspiration and balloon dilatation of the anterior descending and circumflex arteries.
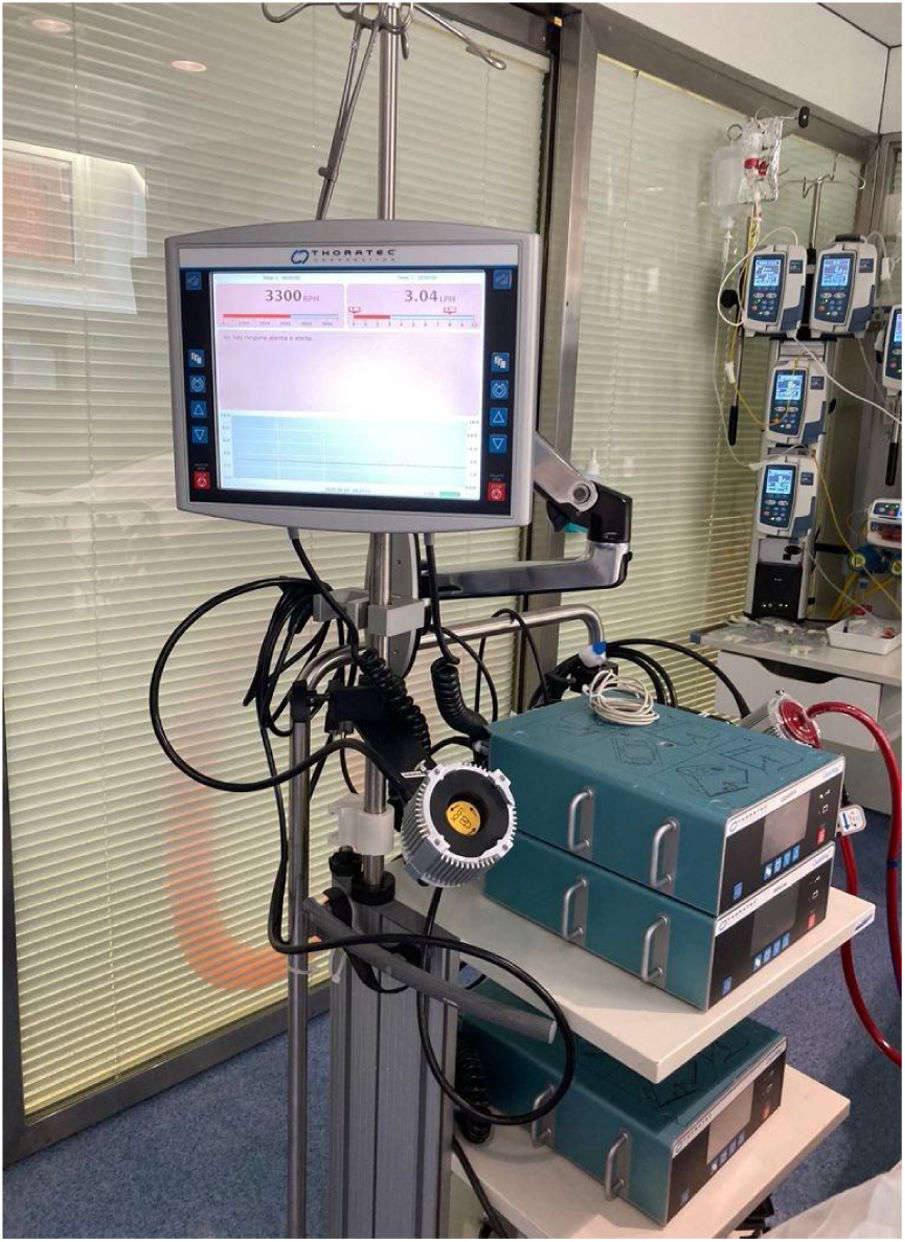
The patient presented with critical ischaemia of the lower extremities due to the presence of the arterial cannula and the balloon in both femoral arteries. It was therefore decided to take her to the operating theatre for conversion to a central left ventricular assist device (LVAD) (Fig. 1) and repair of both femoral arteries. Once the procedure was completed, she was transferred to the intensive care unit (ICU) with an open chest for better clinical management.
During her stay in the ICU she required 3 sternal revision due to bulging smarck and bleeding from the mediastinal drains, support with vasoactive drugs and support, as mentioned above, with a LVAD.
After 72 h the patient remained haemodynamically stable, the vasoactive support could be reduced and the LVAD was withdrawn.
Nursing assessmentWhen the patient was admitted to our ICU a nursing assessment was carried out 6 h after admission, in keeping with the Virginia Henderson 14-need model:
- •
Breathe normally: orotracheal intubation connected to invasive mechanical ventilation (IMV) in volume control mode (VC); FiO2: .55; PEEP: 5. Active humidification, secretions with haematic debris through the endotracheal tube.
- •
Eat and drink adequately: Carrier of Salem nasogastric tube in intermittent aspiration, moderate bilious debit. Carrier of parenteral nutrition administered by central venous catheter. Abdomen soft and depressible.
- •
Eliminate body wastes: bladder catheter wearer, correct urine output with clear urine. Wearing a nappy as a precaution.
- •
Move and maintain desirable postures: bedridden patient. Supine decubitus with pillow on the feet to avoid clubfoot. Barthel index 0 (totally dependent).
- •
Sleep and rest: sedoanalgesia con propofol and remifentanil.
- •
Select suitable clothes – dress and undress: dependent due to physical immobility and sedation.
- •
Maintain body temperature: afebrile, heat transfer through LVAD heater and forced air warming blanket. Lower extremities pale and cold with pulses present but weak.
- •
Keep the body clean and well groomed and protect the skin: daily hygiene of the bedridden critically ill patient, LVAD carrier, totally dependent. Patient with open chest and surgical wounds (insertion of ECMO and IABP cannulas). Skin hydration and application of hyperoxygenated fatty acids to prevent pressure ulcers. Normohydrated skin.
- •
Avoid dangers in the environment and avoid injuring others: use of bedrails, identification bracelet. Measures to prevent infection of catheters and surgical wounds. Compliance with Zero Pneumonia and Zero Bacteraemia protocols.
- •
Communicate with others: incapable of communicating. Richmond Agitation Sedation Scale (RASS) −5: very deep sedation.
- •
Worship according to one’s faith: agnostic. No advance directives.
- •
Work in such a way that there is a sense of accomplishment: patient active before admission.
- •
Play or participate in various forms of recreation: active social life, rides a motorcycle at the week-ends.
- •
Learn, discover or satisfy curiosity: the patient was attending courses on painting and English in her free time.
For the development of the care plan, the nursing diagnoses (ND) according to the NANDA taxonomy and the potential or real collaboration problems that the patient presented during her stay in the ICU were described. The development of the standardised NANDA-NOC-NIC language in the clinical case presented allowed us to methodologically organise the nursing work, facilitating recording and standardising practice.
The AREA model was used to detect the ND principles (Fig. 2). This resulted in 6 principal diagnoses, 2 of which were directly derived from the LVAD.
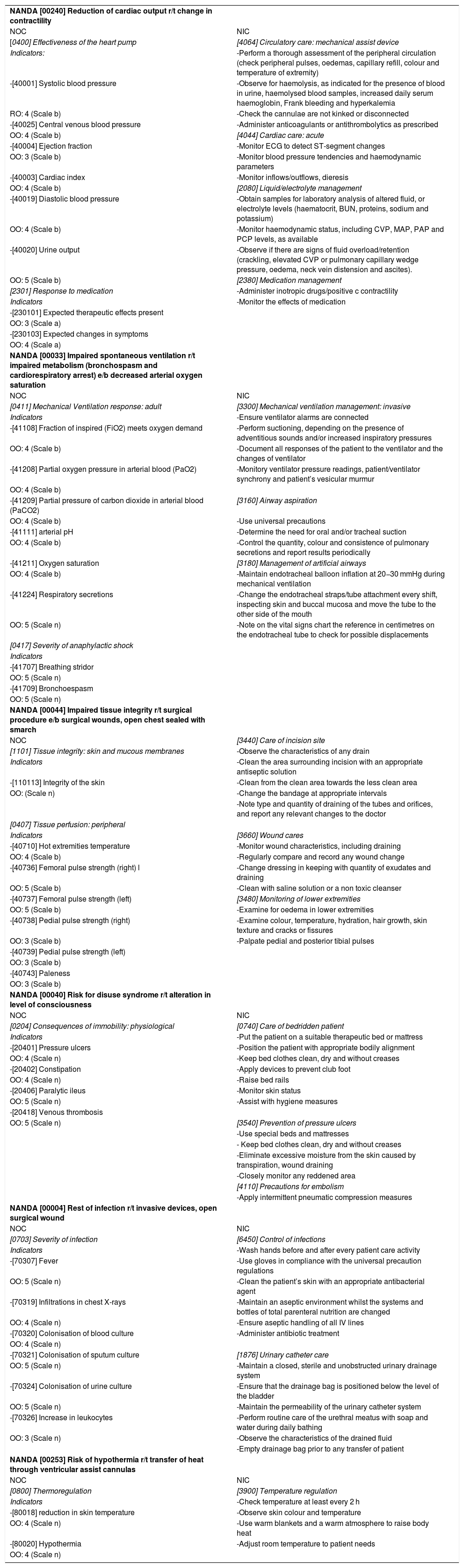
Table 1 contains the care plan with the ND (NANDA), the objectives (NOC) and interventions (NIC) with outcome and activity markers.
ICU care plan.
| NANDA [00240] Reduction of cardiac output r/t change in contractility | |
| NOC | NIC |
| [0400] Effectiveness of the heart pump | [4064] Circulatory care: mechanical assist device |
| Indicators: | -Perform a thorough assessment of the peripheral circulation (check peripheral pulses, oedemas, capillary refill, colour and temperature of extremity) |
| -[40001] Systolic blood pressure | -Observe for haemolysis, as indicated for the presence of blood in urine, haemolysed blood samples, increased daily serum haemoglobin, Frank bleeding and hyperkalemia |
| RO: 4 (Scale b) | -Check the cannulae are not kinked or disconnected |
| -[40025] Central venous blood pressure | -Administer anticoagulants or antithrombolytics as prescribed |
| OO: 4 (Scale b) | [4044] Cardiac care: acute |
| -[40004] Ejection fraction | -Monitor ECG to detect ST-segment changes |
| OO: 3 (Scale b) | -Monitor blood pressure tendencies and haemodynamic parameters |
| -[40003] Cardiac index | -Monitor inflows/outflows, dieresis |
| OO: 4 (Scale b) | [2080] Liquid/electrolyte management |
| -[40019] Diastolic blood pressure | -Obtain samples for laboratory analysis of altered fluid, or electrolyte levels (haematocrit, BUN, proteins, sodium and potassium) |
| OO: 4 (Scale b) | -Monitor haemodynamic status, including CVP, MAP, PAP and PCP levels, as available |
| -[40020] Urine output | -Observe if there are signs of fluid overload/retention (crackling, elevated CVP or pulmonary capillary wedge pressure, oedema, neck vein distension and ascites). |
| OO: 5 (Scale b) | [2380] Medication management |
| [2301] Response to medication | -Administer inotropic drugs/positive c contractility |
| Indicators | -Monitor the effects of medication |
| -[230101] Expected therapeutic effects present | |
| OO: 3 (Scale a) | |
| -[230103] Expected changes in symptoms | |
| OO: 4 (Scale a) | |
| NANDA [00033] Impaired spontaneous ventilation r/t impaired metabolism (bronchospasm and cardiorespiratory arrest) e/b decreased arterial oxygen saturation | |
| NOC | NIC |
| [0411] Mechanical Ventilation response: adult | [3300] Mechanical ventilation management: invasive |
| Indicators | -Ensure ventilator alarms are connected |
| -[41108] Fraction of inspired (FiO2) meets oxygen demand | -Perform suctioning, depending on the presence of adventitious sounds and/or increased inspiratory pressures |
| OO: 4 (Scale b) | -Document all responses of the patient to the ventilator and the changes of ventilator |
| -[41208] Partial oxygen pressure in arterial blood (PaO2) | -Monitory ventilator pressure readings, patient/ventilator synchrony and patient’s vesicular murmur |
| OO: 4 (Scale b) | |
| -[41209] Partial pressure of carbon dioxide in arterial blood (PaCO2) | [3160] Airway aspiration |
| OO: 4 (Scale b) | -Use universal precautions |
| -[41111] arterial pH | -Determine the need for oral and/or tracheal suction |
| OO: 4 (Scale b) | -Control the quantity, colour and consistence of pulmonary secretions and report results periodically |
| -[41211] Oxygen saturation | [3180] Management of artificial airways |
| OO: 4 (Scale b) | -Maintain endotracheal balloon inflation at 20−30 mmHg during mechanical ventilation |
| -[41224] Respiratory secretions | -Change the endotracheal straps/tube attachment every shift, inspecting skin and buccal mucosa and move the tube to the other side of the mouth |
| OO: 5 (Scale n) | -Note on the vital signs chart the reference in centimetres on the endotracheal tube to check for possible displacements |
| [0417] Severity of anaphylactic shock | |
| Indicators | |
| -[41707] Breathing stridor | |
| OO: 5 (Scale n) | |
| -[41709] Bronchoespasm | |
| OO: 5 (Scale n) | |
| NANDA [00044] Impaired tissue integrity r/t surgical procedure e/b surgical wounds, open chest sealed with smarch | |
| NOC | [3440] Care of incision site |
| [1101] Tissue integrity: skin and mucous membranes | -Observe the characteristics of any drain |
| Indicators | -Clean the area surrounding incision with an appropriate antiseptic solution |
| -[110113] Integrity of the skin | -Clean from the clean area towards the less clean area |
| OO: (Scale n) | -Change the bandage at appropriate intervals |
| -Note type and quantity of draining of the tubes and orifices, and report any relevant changes to the doctor | |
| [0407] Tissue perfusion: peripheral | |
| Indicators | [3660] Wound cares |
| -[40710] Hot extremities temperature | -Monitor wound characteristics, including draining |
| OO: 4 (Scale b) | -Regularly compare and record any wound change |
| -[40736] Femoral pulse strength (right) l | -Change dressing in keeping with quantity of exudates and draining |
| OO: 5 (Scale b) | -Clean with saline solution or a non toxic cleanser |
| -[40737] Femoral pulse strength (left) | [3480] Monitoring of lower extremities |
| OO: 5 (Scale b) | -Examine for oedema in lower extremities |
| -[40738] Pedial pulse strength (right) | -Examine colour, temperature, hydration, hair growth, skin texture and cracks or fissures |
| OO: 3 (Scale b) | -Palpate pedial and posterior tibial pulses |
| -[40739] Pedial pulse strength (left) | |
| OO: 3 (Scale b) | |
| -[40743] Paleness | |
| OO: 3 (Scale b) | |
| NANDA [00040] Risk for disuse syndrome r/t alteration in level of consciousness | |
| NOC | NIC |
| [0204] Consequences of immobility: physiological | [0740] Care of bedridden patient |
| Indicators | -Put the patient on a suitable therapeutic bed or mattress |
| -[20401] Pressure ulcers | -Position the patient with appropriate bodily alignment |
| OO: 4 (Scale n) | -Keep bed clothes clean, dry and without creases |
| -[20402] Constipation | -Apply devices to prevent club foot |
| OO: 4 (Scale n) | -Raise bed rails |
| -[20406] Paralytic ileus | -Monitor skin status |
| OO: 5 (Scale n) | -Assist with hygiene measures |
| -[20418] Venous thrombosis | |
| OO: 5 (Scale n) | [3540] Prevention of pressure ulcers |
| -Use special beds and mattresses | |
| - Keep bed clothes clean, dry and without creases | |
| -Eliminate excessive moisture from the skin caused by transpiration, wound draining | |
| -Closely monitor any reddened area | |
| [4110] Precautions for embolism | |
| -Apply intermittent pneumatic compression measures | |
| NANDA [00004] Rest of infection r/t invasive devices, open surgical wound | |
| NOC | NIC |
| [0703] Severity of infection | [6450] Control of infections |
| Indicators | -Wash hands before and after every patient care activity |
| -[70307] Fever | -Use gloves in compliance with the universal precaution regulations |
| OO: 5 (Scale n) | -Clean the patient’s skin with an appropriate antibacterial agent |
| -[70319] Infiltrations in chest X-rays | -Maintain an aseptic environment whilst the systems and bottles of total parenteral nutrition are changed |
| OO: 4 (Scale n) | -Ensure aseptic handling of all IV lines |
| -[70320] Colonisation of blood culture | -Administer antibiotic treatment |
| OO: 4 (Scale n) | |
| -[70321] Colonisation of sputum culture | [1876] Urinary catheter care |
| OO: 5 (Scale n) | -Maintain a closed, sterile and unobstructed urinary drainage system |
| -[70324] Colonisation of urine culture | -Ensure that the drainage bag is positioned below the level of the bladder |
| OO: 5 (Scale n) | -Maintain the permeability of the urinary catheter system |
| -[70326] Increase in leukocytes | -Perform routine care of the urethral meatus with soap and water during daily bathing |
| OO: 3 (Scale n) | -Observe the characteristics of the drained fluid |
| -Empty drainage bag prior to any transfer of patient | |
| NANDA [00253] Risk of hypothermia r/t transfer of heat through ventricular assist cannulas | |
| NOC | NIC |
| [0800] Thermoregulation | [3900] Temperature regulation |
| Indicators | -Check temperature at least every 2 h |
| -[80018] reduction in skin temperature | -Observe skin colour and temperature |
| OO: 4 (Scale n) | -Use warm blankets and a warm atmosphere to raise body heat |
| -[80020] Hypothermia | -Adjust room temperature to patient needs |
| OO: 4 (Scale n) |
CVP: central venous pressure; ECG: electrocardiogram; ICU: intensive care unit; MAP: mean arterial pressure; PAP: pulmonary arterial pressure; PCP: pulmonary capillary pressure.
Likert scales to evaluate outcome indicators:
Scale a: 1: severely compromised; 2: considerably compromised; 3: moderately compromised; 4: slightly compromised; 5: not compromised.
Scale b: 1: severe deviation from normal range; 2: considerable deviation from normal range; 3: moderate deviation from normal range; 4: slight deviation from normal range; 5: no deviation from normal range.
Scale n: 1: severe; 2: considerable; 3: moderate; 4: slight; 5: none.
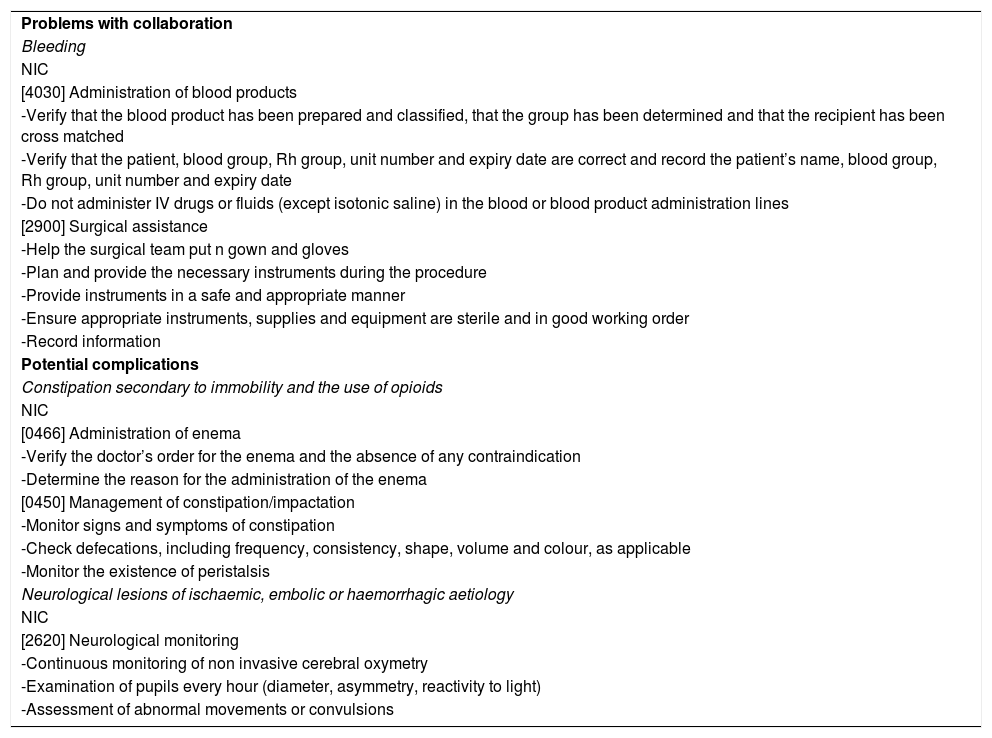
Table 2 describes the collaboration problems and potential complications.
Potential complications and problems with collaboration.
| Problems with collaboration |
| Bleeding |
| NIC |
| [4030] Administration of blood products |
| -Verify that the blood product has been prepared and classified, that the group has been determined and that the recipient has been cross matched |
| -Verify that the patient, blood group, Rh group, unit number and expiry date are correct and record the patient’s name, blood group, Rh group, unit number and expiry date |
| -Do not administer IV drugs or fluids (except isotonic saline) in the blood or blood product administration lines |
| [2900] Surgical assistance |
| -Help the surgical team put n gown and gloves |
| -Plan and provide the necessary instruments during the procedure |
| -Provide instruments in a safe and appropriate manner |
| -Ensure appropriate instruments, supplies and equipment are sterile and in good working order |
| -Record information |
| Potential complications |
| Constipation secondary to immobility and the use of opioids |
| NIC |
| [0466] Administration of enema |
| -Verify the doctor’s order for the enema and the absence of any contraindication |
| -Determine the reason for the administration of the enema |
| [0450] Management of constipation/impactation |
| -Monitor signs and symptoms of constipation |
| -Check defecations, including frequency, consistency, shape, volume and colour, as applicable |
| -Monitor the existence of peristalsis |
| Neurological lesions of ischaemic, embolic or haemorrhagic aetiology |
| NIC |
| [2620] Neurological monitoring |
| -Continuous monitoring of non invasive cerebral oxymetry |
| -Examination of pupils every hour (diameter, asymmetry, reactivity to light) |
| -Assessment of abnormal movements or convulsions |
When care in the cardiac ICU had terminated and prior to transfer to the coronary ICU, an assessment of outcomes obtained (OO) was made. The 5-point Likert scale was used for assessment of NOC outcomes.
Reflection on the caseThe occurrence of anaphylactic shock in a patent with Killip I infarction aggravated the situation causing mixed shock, developing into treatment-refractory CRA, necessitating the implantation of an ECMO in situ. Acute arterial ischaemia of both lower extremities made it necessary to implant a LVAD in order to remove the ECMO and IABP.
Due to this previous situation the patient was admitted to our ICU in an unstable condition and an individualised care plan was drawn up using care plans for patients on ventricular support as a guide.8
Among the main limitations which arose was the difficulty in movements due to the open chest. It was not possible to put the patient on her side to assess her skin periodically and prevent pressure ulcers forming on her back and sacral region. However, we placed special emphasis on ensuring the patient’s parenteral nutrition and keeping the air mattress anti-bedsore-mode activated.
When the care plan was created we believed it important to consider constipation as a potential problem since this is a highly important need which is often ignored in the ICU. Sixty three per cent of patients admitted to the ICU suffer from constipation, which is why we wanted to stress the importance of making nursing professionals aware of the relevance of a correct elimination pattern.9
We wish to indicate that on review of the literature to support the creation of the care plan, one difficulty we encountered was that there were no similar articles to be found with which to contrast our care plan with and we found no NIC relating to care of the patient with a sternal aperture. Further research is needed and analysis of nursing care cases according to the NANDA-NOC-NIC taxonomy in this type of patient.
ConclusionApplication of nursing care using standard taxonomies allows us to assess patient progress at any time and the effectiveness of nursing activity, ensuring quality care. Knowledge of techniques and anticipation of real or potential problems helped to resolve this extremely urgent situation to achieve patient stability. We wish to stress the responsibility of the nursing personnel since nursing activities are essential for good development of care.
FinancingThe authors declare they have not received any financing for completing this study.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Martínez Font S, López Domènech G, Juan Esgleas S, Ruiz Falqués C, Soler Selva M. Shock mixto en paciente con infarto agudo de miocardio: intervenciones enfermeras. Enferm Intensiva. 2021;32:230–237.