Addressing and accommodating client preferences in psychotherapy have been consistently associated with improved treatment outcomes; however, few clinically useful and psychometrically acceptable measures are available for this purpose. The aim of this study was to develop a brief, multidimensional clinical tool to help clients articulate the therapist style they desire in psychotherapy or counseling. An online survey composed of 40 therapy preference items was completed by 860 respondents, primarily female (n=699), British (n=650), White (n=761), and mental health professionals themselves (n=615). Principal components analysis resulted in four scales that accounted for 39% of the total variance: Therapist Directiveness vs. Client Directiveness, Emotional Intensity vs. Emotional Reserve, Past Orientation vs. Present Orientation, and Warm Support vs. Focused Challenge. These scales map well onto dimensions of therapist activity and cover most of the major preference dimensions identified in the research literature. Internal consistency coefficients ranged between .60 and .85 (M=.71). Tentative cutoff points for strong preferences on each dimension were established. The 18-item Cooper-Norcross Inventory of Preferences (C-NIP) is a multidimensional measure with clinical utility, but additional validity data are needed.
Abordar y acomodar las preferencias del cliente en psicoterapia se asoció consistentemente con mejoras en los resultados del tratamiento; sin embargo, pocas medidas clínicamente útiles y psicométricamente aceptables están disponibles para este propósito. El objetivo fue desarrollar una herramienta clínica multidimensional breve para ayudar a que los clientes articulen el estilo terapéutico que desean en la psicoterapia o consejería. Una encuesta online compuesta por 40 ítems de preferencias de terapia fue completada por 860 sujetos, principalmente mujeres (n=699), británicos (n=650), blancos (n=761) y profesionales de la salud mental (n=615). Un análisis de componentes principales aisló cuatro escalas que representan el 39% de la varianza total: Directividad del terapeuta vs. Directividad del cliente, Intensidad emocional vs. Reserva emocional, Orientación pasada vs. Orientación presente y Apoyo caluroso vs. Cambio focalizado. Estas escalas recogen las dimensiones de la actividad del terapeuta y cubren la mayoría de las principales dimensiones de preferencias identificadas en la literatura. Los coeficientes de consistencia interna oscilaron entre 0,60 y 0,85 (M=0,71). Se establecieron puntos de corte provisionales para fuertes preferencias en cada dimensión. El Inventario de Preferencias Cooper-Norcross-18 ítems (C-NIP) es una medida multidimensional con utilidad clínica, pero se necesitan datos adicionales de validez.
In recent years, there has been an increasing emphasis on taking client preferences into account when determining a psychological or medical treatment (National Collaborating Centre for Mental Health, 2010; Straus, Richardson, Glasziou, & Haynes, 2005). Indeed, the international juggernaut of evidence-based practice (EBP) considers patient values as one of the three essential evidentiary sources, along with best reseach evidence and clinican expertise, that require consideration and integration. The American Psychological Association (2006) definition of EBP explicitly expanded “patient values” into “patient characteristics, culture, and preferences”. In so doing, clients assume a more active, prominent position in EBPs in mental health and addictions. In all cases, the integration of client preferences is a defining feature of evidence-based practice in psychology (Norcross, Hogan, & Koocher, 2008).
Client preferences can be defined as “the behaviors or attributes of the therapist or therapy that clients value or desire” (Swift, Callahan, & Vollmer, 2011, p. 302). Three types of client preferences have been proposed in the literature (Swift et al., 2011). Therapist preferences refer to clients’ desires that psychotherapists will have specific personal characteristics, such as being female. Treatment preferences refer to macro-level desires for a particular kind of therapy, such as cognitive-behavioral therapy over a person-centered approach. Finally, role preferences refer to micro-level preferences for particular behaviors, activities and styles of intervention within the therapeutic work, such as a nondirective therapist approach. Role preferences can be further subdivided into therapist role preferences (such as asking questions) and client role preferences (such as reflecting on childhood events) (Cooper & McLeod, 2011; Watsford & Rickwood, 2014).
Research on the relationship between client preferences and therapy outcomes provides strong support for the clinical assessment and empirical investigation of this factor. Meta-analytic findings indicated that clients who received a preferred therapy, as compared with clients who receive a non-preferred therapy, show significantly greater clinical outcomes and satisfaction, and significantly lower dropout rates at a ratio of almost one-to-two (Lindhiem, Bennett, Trentacosta, & McLear, 2014; Swift et al., 2011).
Despite these consistent research findings, there is little evidence that client preferences are routinely being assessed or accommodated in clinical practice. A key reason may be the small number of public tools for assessing client preferences, and those are primarily for research rather than clinical purposes.
Treatment preference vignettesA standard research method for assessing clients’ preferences has been to provide participants with written vignettes (e.g., King et al., 2000) or video recordings (e.g., Devine & Fernald, 1973) of different treatments. Clients are then asked to indicate which of these treatments they would prefer or to rate the strength of their preferences. A parallel in clinical practice is decision aids (The Health Foundation, 2014), which provide patients with information about the different treatments for their condition and support shared decision making. Although primarily available for physical health conditions, decision aids for depression have now been produced, both as a written pamphlet (BMJ Group, 2015b) and as a web-based resource (BMJ Group, 2015a).
The use of decision aids typically lead to greater self-efficacy and improved decision making (The Health Foundation, 2014). However, for clinical purposes, such approaches have several limitations. First, in many instances, they elicit only dichotomous answers (preference for treatment A vs. preference for treatment B), rather than indicating the strength of the respective preferences. The magnitude of preferences may prove critical as clients with strong preferences for—or against—different treatments may respond differently to those who hold only mild preferences (Swift et al., 2011). Second, decision aids elicit only macro-level treatment preferences, and not therapist preferences and role preferences. Third, such decision aids would not prove relevant to integrative or eclectic therapies, which tend to be the modal theoretical orientation of mental health practitioners in the Western developed countries (Norcross & Goldfried, 2005). For integrative clinicians, understanding clients’ role preferences—and particularly what they desire in terms of therapist activity—may be of most value in helping them tailor and adapt their approach.
Extant preference measuresThe Psychotherapy Preferences and Experiences Questionnaire (PEX, version P1) (Sandell, Clinton, Frövenholt, & Bragesjö, 2011) is a 29-item measure that asks respondents to rate, on 6-point Likert-type scales, the extent to which they believed a range of therapist activities, therapist characteristics, and client activities would be helpful for them. The items are grouped according to five subscales, derived from research on coping styles (Dance & Neufeld, 1988): Outward Orientation (directive and problem-solving therapist activities); Inward Orientation (reflective and insight-oriented activities); Support (encouraging and friendly therapist activities); Catharsis (emotionally expressive activities); and Defensiveness (avoidant and emotionally suppressive client activities). The PEX subscales have satisfactory internal consistency (Cronbach's α=.78-.86), with evidence of concurrent (Sandell et al., 2011) and predictive (Levy Berg, Sandahl, & Clinton, 2008) validity.
The PEX also has limitations as a clinical tool. First, although it is titled a preference measure, it is actually a measure of “helpfulness beliefs” (Sandell et al., 2011): the extent to which clients expect to be helped by certain activities. Expectations are related to preferences, but are not synonymous and have with different effects on therapy (Constantino, Glass, Arnkoff, Ametrano, & Smith, 2011; Tracey & Dundon, 1988). Second, the PEX items and scales were developed using an a priori theoretical framework. Hence, they may not represent the most significant dimensions of client preferences. Third, the items on the PEX form a heterogeneous mix of therapist activities, therapist characteristics, and client activities. This means that results from the PEX may be difficult to interpret and apply in clinical practice.
The Counseling Preference Form (CPF) asks respondents to indicate which of 10 therapist activities they would prefer their counsellors to use (Goates-Jones & Hill, 2008). Five of the therapist activities are labelled “insight skills” (e.g., being helped to gain a new perspective on problems) and five therapist activities are labelled “action skills” (e.g., being taught specific skills to deal with problems). Test-retest reliability for the CPF was r=.50. In terms of limitations, the CPF, like the TPEX, is based on a priori assumptions about the key dimensions of client preferences (Goates-Jones & Hill, 2008). It also has limited evidence of reliability and validity. The binary option response format reduces variability of scores, creates restrictions on score ranges, and limits its ability to measure preference strength. The scoring procedure is also based on the assumption that preferences for insight and action skills are opposing ends of a single dimension.
The 90-item Preference for College Counselling Inventory (PCCI) assesses clients’ preferences for therapist characteristics, therapist activities, and client activities (Hatchett, 2015a). Although designed for use in college counseling, its items are potentially relevant to other counseling settings. The PCCI evolved over a series of studies with undergraduates and is divided into three parts. The first part asks seven open questions about preferences for particular therapist characteristics, such as therapist gender and sexual orientation. The second part consists of 32 items focusing on preferences for therapist characteristics and activities, and principal components analysis identified three components labelled Therapist Expertise, Therapist Warmth, and Therapist Directiveness. The third part consists of 28 items focusing on preferences for client activities, and principal components analysis identified two components: Task-oriented Activities and Experiential/Insight-Oriented Activities. Each of the five subscales showed good internal consistency (Cronbach's α=.89-.92). There was some evidence of discriminant validity for the PCCI subscales, with low correlations against a measure of attitudes towards seeking professional help (Hatchett, 2015a).
Limitations of the PCCI include its length (67 items) and development on a non-clinical undergraduate population. Intercorrelations amongst the PCCI subscales are also in the moderate to large range (rmedian=.51), suggesting that there may be a response bias in how the items (all positively keyed) tend to be scored.
Therapy Personalisation Form (TPF)In contrast to the previous preference inventories, the Therapy Personalisation Form was specifically designed and tested for use with clinical populations (Bowen & Cooper, 2012). It comes in two forms: one for use at assessment (TPF-A) and one for use during the therapy itself (TPF). The forms are relatively short (20 semantic differential items) so that they are quick and easy to use as part of routine clinical practice. The items focus solely on clients’ preferences for therapist activities. The items for the inventory were developed by asking 20 therapists about the various dilemmas of practice they experienced in their work with clients, such as when to be challenging or be gentle.
The TPF has been tested for its clinical acceptability in a small clinical sample. Eighteen clients gave it an average mean helpfulness ratings of 3.8 (SD=1.2) and 3.5 (SD=1.0), respectively, on 5-point scales (1=very unhelpful, 2=unhelpful, 3=neither, 4=helpful, 5=very helpful) (Cooper et al., 2015a,b). Comparative ratings were 3.1 for the Working Alliance Inventory—Short Form (Tracey & Kokotovic, 1989) and 3.7 for the Session Rating Scale (Duncan, Miller, Sparks, & Claud, 2003).
The factor structures of the TPF-A and TPF have been examined in two studies. For the TPF-A, a principal components analysis of data from 111 clients at initial assessment identified four factors (Aylindar & Cooper, 2014): Task Focus, Past Focus, Congruence, and Directiveness. For the TPF, as implemented part-way through therapy with 101 clients, three factors were identified (Watson, 2015): Therapist Direction, Past Focus, and Therapist's Use of Self. However, reliabilities on some of the scales were low. The measure also lacks evidence of validity and cut points to identify when clients are indicating strong preferences.
The present studyBuilding on (and indebted to) these previous efforts, the present study was designed to develop a brief, reliable, multidimensional, and clinically useful measure for routine practice to help clients articulate the therapist style that they prefer in psychotherapy or counseling. In addition, we aimed to develop cut points for strong preferences so that the meaning of client preferences would be readily interpretable and clinically useful. The identification of salient preferences is likely to generate the most cost-efficient and powerful guidance to mental health practitioners.
MethodsThe surveyAn online survey was created and hosted using the Qualtrics Survey Software program. The survey consisted of an information page, consent form, demographics questionnaire, and a series of 40 therapy preference items. The demographics questionnaire asked participants to indicate their gender, age, country of residence, and ethnicity (fixed response set). Participants were asked to check one or more boxes to indicate their experience in receiving psychotherapy. They were then asked to indicate if they were a mental health professional, in training or in practice. If they indicated in the affirmative, they were asked their specific profession, and whether they were in training or a qualified/licensed practitioner.
We generated items regarding psychotherapy/counseling preferences in several ways. First, we adapted many items from the TPF. Second, we added items based on a review of other preference measures and related literature on client preferences (e.g., Goates-Jones & Hill, 2008; Sandell et al., 2011). Third, we generated items based on our own clinical and teaching experiences. Fourth we sent three content experts the existing items and asked them to identify any other practice dimensions that they thought most therapists, from most theoretical orientations, would be willing to vary in response to client preferences. Respondents were asked to ensure that the dimensions were framed in such a way that there was no intrinsically “better” pole and no intrinsically “worse” one. All told, the survey contained a total of 40 therapy preference items.
The instructions for this section of the survey read: “On each of the items below, please indicate your preferences for how a psychotherapist or counsellor would work with you. Please click on the appropriate number on each item.” Participants were offered a seven-point sematic differential-type scale (3 to 0 to 3) with labels (“3 indicates a strong preference in that direction”; “2 indicates a moderate preference in that direction”; “1 indicates a slight preference in that direction.” Zero was marked on each scale as indicating “No preference”). We used semantic differential scales, rather than standard unipolar Likert-type items, because we hypothesized that the latter allowed clients to ask for high levels of every therapist activity, or low levels of every therapist activity. Neither would prove feasible to implement within an actual therapeutic relationship.
ParticipantsOver the course of 2 months, 1,105 individuals accessed the survey. Of those, five did not consent to participate and a further 39 did not respond to the consent question. Of the 1,061 consenting participants, 98 (7.6%) did not provide any demographic information or complete the therapy preference part of the survey, and an additional 103 (9.7%) completed the demographic part of the survey but did not complete any therapy preference items. Thus, 860 participants (77.8% of those accessing the survey) participated, with 713 participants completing all preference items.
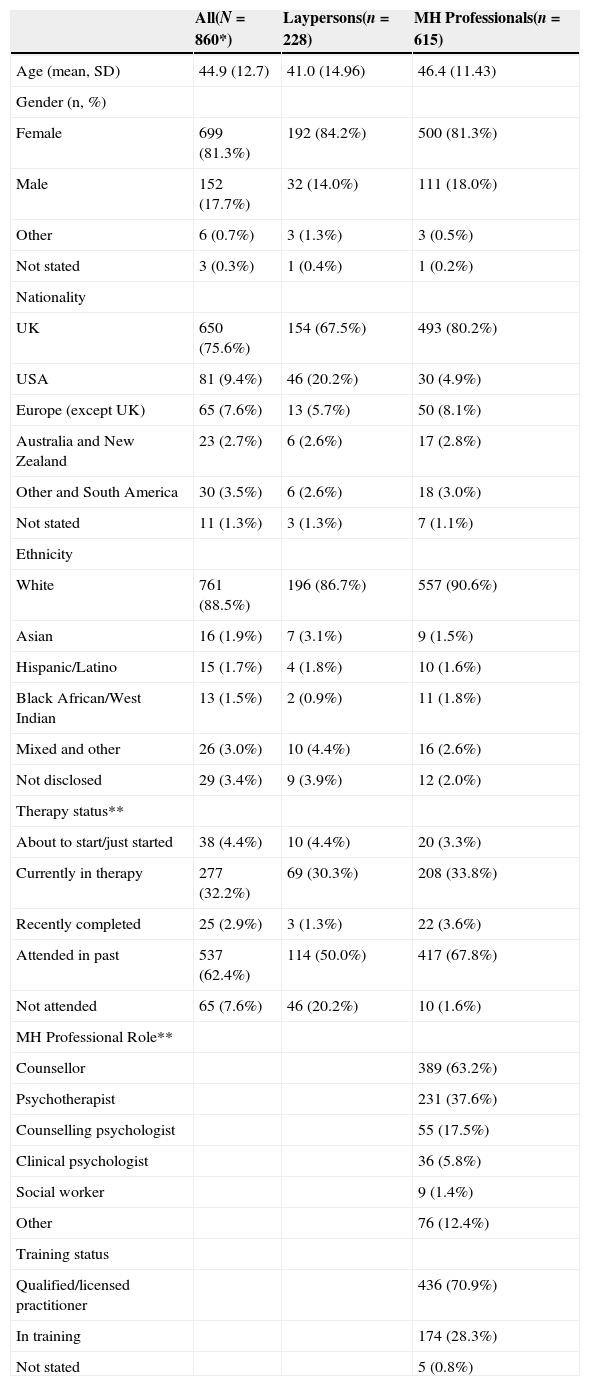
As shown in Table 1, the mean age of the 860 participants was 44.9 years (SD=12.7), and they were primarily female (81.3%). Participants were mainly from the UK (75.6%) and the USA (9.4%). A large majority of participants were of a White ethnicity (88.5%), with smaller numbers of Asian, Hispanic/Latino and Black participants. A majority of the participants were mental health professionals (71.5%): primarily identifying as counsellors (45.2% of full sample), psychotherapists (26.9%), and psychologists (10.6%). Of the full sample, 62% had been in therapy in the past, 32% were currently in therapy, 4% were about to start—or had just started—therapy, 3% had completed therapy in the past month, and only 8% had never attended therapy.
Sample characteristics.
| All(N=860*) | Laypersons(n=228) | MH Professionals(n=615) | |
|---|---|---|---|
| Age (mean, SD) | 44.9 (12.7) | 41.0 (14.96) | 46.4 (11.43) |
| Gender (n, %) | |||
| Female | 699 (81.3%) | 192 (84.2%) | 500 (81.3%) |
| Male | 152 (17.7%) | 32 (14.0%) | 111 (18.0%) |
| Other | 6 (0.7%) | 3 (1.3%) | 3 (0.5%) |
| Not stated | 3 (0.3%) | 1 (0.4%) | 1 (0.2%) |
| Nationality | |||
| UK | 650 (75.6%) | 154 (67.5%) | 493 (80.2%) |
| USA | 81 (9.4%) | 46 (20.2%) | 30 (4.9%) |
| Europe (except UK) | 65 (7.6%) | 13 (5.7%) | 50 (8.1%) |
| Australia and New Zealand | 23 (2.7%) | 6 (2.6%) | 17 (2.8%) |
| Other and South America | 30 (3.5%) | 6 (2.6%) | 18 (3.0%) |
| Not stated | 11 (1.3%) | 3 (1.3%) | 7 (1.1%) |
| Ethnicity | |||
| White | 761 (88.5%) | 196 (86.7%) | 557 (90.6%) |
| Asian | 16 (1.9%) | 7 (3.1%) | 9 (1.5%) |
| Hispanic/Latino | 15 (1.7%) | 4 (1.8%) | 10 (1.6%) |
| Black African/West Indian | 13 (1.5%) | 2 (0.9%) | 11 (1.8%) |
| Mixed and other | 26 (3.0%) | 10 (4.4%) | 16 (2.6%) |
| Not disclosed | 29 (3.4%) | 9 (3.9%) | 12 (2.0%) |
| Therapy status** | |||
| About to start/just started | 38 (4.4%) | 10 (4.4%) | 20 (3.3%) |
| Currently in therapy | 277 (32.2%) | 69 (30.3%) | 208 (33.8%) |
| Recently completed | 25 (2.9%) | 3 (1.3%) | 22 (3.6%) |
| Attended in past | 537 (62.4%) | 114 (50.0%) | 417 (67.8%) |
| Not attended | 65 (7.6%) | 46 (20.2%) | 10 (1.6%) |
| MH Professional Role** | |||
| Counsellor | 389 (63.2%) | ||
| Psychotherapist | 231 (37.6%) | ||
| Counselling psychologist | 55 (17.5%) | ||
| Clinical psychologist | 36 (5.8%) | ||
| Social worker | 9 (1.4%) | ||
| Other | 76 (12.4%) | ||
| Training status | |||
| Qualified/licensed practitioner | 436 (70.9%) | ||
| In training | 174 (28.3%) | ||
| Not stated | 5 (0.8%) |
Note. *Includes 17 participants who did not state professional status.
**Total % may be>100% as participants could endorse more than one answer per question.
The laypeople were significantly younger than the mental health professionals, F(1)=30.54, p<.001. There were also significant differences in location (X2 (7)=52.60, p<.001), with higher proportions of laypeople in the North American samples. The laypeople were less likely to indicate attendance at counseling or psychotherapy in the past (50.0% vs 67.8%, X2 (1)=22.62, p<.001).
Participants who completed the preference items, as compared with those who did not (but completed the demographic section), were distinctive in a few respect. They were more likely to be female (81.5% vs 67.6%, X2 (2)=11.09, p=.004), White (93.9% vs 83.3%, X2 (6)=18.85, p=.004), mental health professionals (71.6% vs 61.9%, X2 (2)=7.92, p=.019), and indicate previous therapy attendance (62.5% vs 48.6%, X2 (1)=7.65, p=.006).
ProcedureTo maximize the representativeness of our sample, we aimed to recruit participants at various stages and levels of involvement with psychotherapy. This ranged from those who had just begun therapy to those who had completed it, and from those who had never attended psychotherapy or counseling to those who professionally conduct it.
To achieve a large and clinically experienced sample, we employed four recruitment strategies. First, notices were placed on social media websites. These invited users of counseling and psychotherapy to complete a measure of therapy preferences and provided a link to the online survey. Mental health professionals were asked to forward the link to clients. Second, notices were placed on the websites of a range of UK counseling services and directories, inviting prospective consumers to access the survey. Third, undergraduates at two universities, one in the US and one in the UK, were invited to complete the survey. Fourth, emails were sent by the authors to select professional contacts in the mental health field. These emails invited recipients to complete it themselves and to forward on the invitation to any clients, trainees, colleagues, networks or listservs that they thought might be interested in participating.
Analysis of the data was conducted using SPSS Statistics 20. One item had been duplicated in the survey and was removed prior to analysis. For the principal components analysis, we excluded cases listwise, such that the data came from the 713 participants who had answered all preference items. To score our items on the 3-0-3 scales, we kept scores on the left hand side of the scale as positive, kept zero as zero, and reverse scored items on the right hand side of the scale. Hence, the scale was scored from +3 to -3, with higher scores indicating a greater preference for the initial/left hand term in the item label.
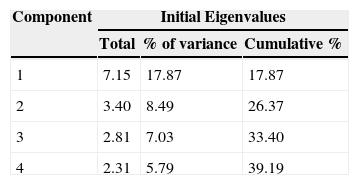
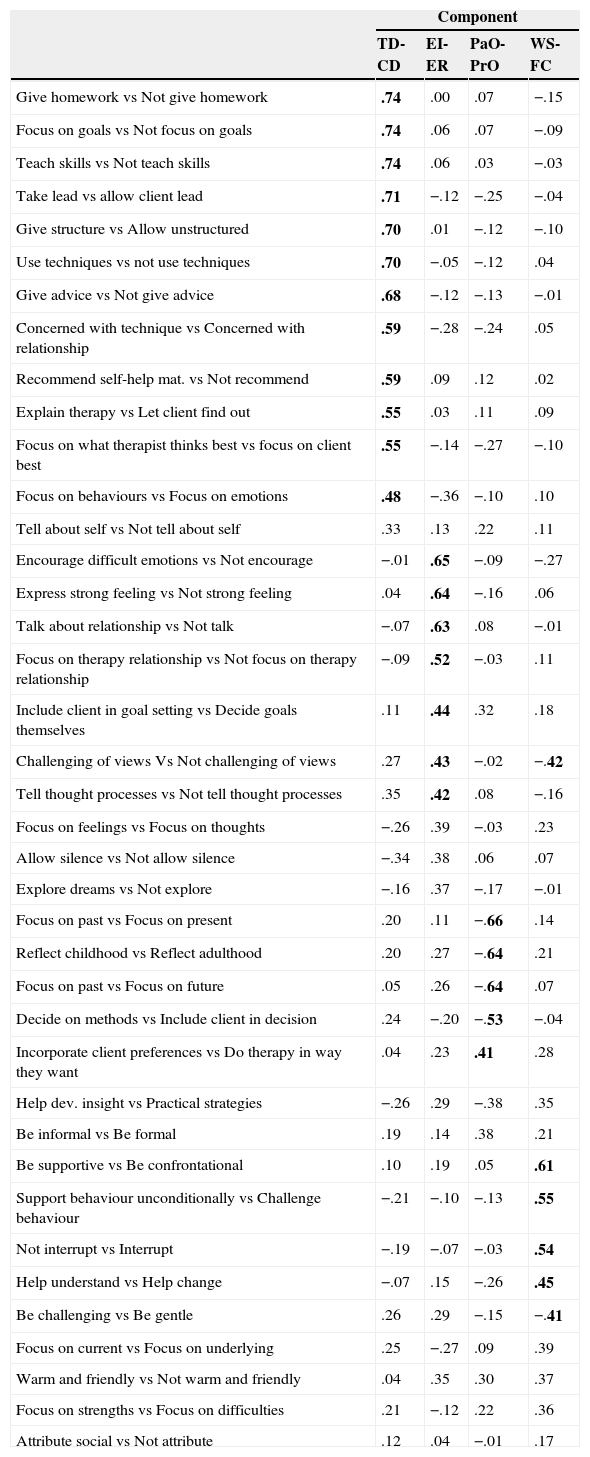
ResultsPrincipal components analysisA principal components analysis (PCA) was conducted using an oblique, direct oblimin rotation on the 39 therapy preference items. Initial tests indicated good levels of factorability: KMO=.86; Bartlett's test, X2 (741)=8421.9, p<.001. An oblique rotation was used because we could not assume independence of the components. Scree plots were performed on the resultant eigenvalues, and visual inspection indicated a distinct “elbow” after the fourth component. Cumulatively, these four components accounted for 39.2% of the overall variance. Table 2 summarizes the eigenvalues and percent of variance explained by the four components. The rotated PCA structure is presented in Table 3. Separate PCAs of the layperson and mental health professional samples yielded the same essential components.
Rotated component structure for four factors using direct oblimin rotation.
| Component | ||||
|---|---|---|---|---|
| TD-CD | EI-ER | PaO-PrO | WS-FC | |
| Give homework vs Not give homework | .74 | .00 | .07 | −.15 |
| Focus on goals vs Not focus on goals | .74 | .06 | .07 | −.09 |
| Teach skills vs Not teach skills | .74 | .06 | .03 | −.03 |
| Take lead vs allow client lead | .71 | −.12 | −.25 | −.04 |
| Give structure vs Allow unstructured | .70 | .01 | −.12 | −.10 |
| Use techniques vs not use techniques | .70 | −.05 | −.12 | .04 |
| Give advice vs Not give advice | .68 | −.12 | −.13 | −.01 |
| Concerned with technique vs Concerned with relationship | .59 | −.28 | −.24 | .05 |
| Recommend self-help mat. vs Not recommend | .59 | .09 | .12 | .02 |
| Explain therapy vs Let client find out | .55 | .03 | .11 | .09 |
| Focus on what therapist thinks best vs focus on client best | .55 | −.14 | −.27 | −.10 |
| Focus on behaviours vs Focus on emotions | .48 | −.36 | −.10 | .10 |
| Tell about self vs Not tell about self | .33 | .13 | .22 | .11 |
| Encourage difficult emotions vs Not encourage | −.01 | .65 | −.09 | −.27 |
| Express strong feeling vs Not strong feeling | .04 | .64 | −.16 | .06 |
| Talk about relationship vs Not talk | −.07 | .63 | .08 | −.01 |
| Focus on therapy relationship vs Not focus on therapy relationship | −.09 | .52 | −.03 | .11 |
| Include client in goal setting vs Decide goals themselves | .11 | .44 | .32 | .18 |
| Challenging of views Vs Not challenging of views | .27 | .43 | −.02 | −.42 |
| Tell thought processes vs Not tell thought processes | .35 | .42 | .08 | −.16 |
| Focus on feelings vs Focus on thoughts | −.26 | .39 | −.03 | .23 |
| Allow silence vs Not allow silence | −.34 | .38 | .06 | .07 |
| Explore dreams vs Not explore | −.16 | .37 | −.17 | −.01 |
| Focus on past vs Focus on present | .20 | .11 | −.66 | .14 |
| Reflect childhood vs Reflect adulthood | .20 | .27 | −.64 | .21 |
| Focus on past vs Focus on future | .05 | .26 | −.64 | .07 |
| Decide on methods vs Include client in decision | .24 | −.20 | −.53 | −.04 |
| Incorporate client preferences vs Do therapy in way they want | .04 | .23 | .41 | .28 |
| Help dev. insight vs Practical strategies | −.26 | .29 | −.38 | .35 |
| Be informal vs Be formal | .19 | .14 | .38 | .21 |
| Be supportive vs Be confrontational | .10 | .19 | .05 | .61 |
| Support behaviour unconditionally vs Challenge behaviour | −.21 | −.10 | −.13 | .55 |
| Not interrupt vs Interrupt | −.19 | −.07 | −.03 | .54 |
| Help understand vs Help change | −.07 | .15 | −.26 | .45 |
| Be challenging vs Be gentle | .26 | .29 | −.15 | −.41 |
| Focus on current vs Focus on underlying | .25 | −.27 | .09 | .39 |
| Warm and friendly vs Not warm and friendly | .04 | .35 | .30 | .37 |
| Focus on strengths vs Focus on difficulties | .21 | −.12 | .22 | .36 |
| Attribute social vs Not attribute | .12 | .04 | −.01 | .17 |
Note. Marker items in bold loaded>.40.
TD-CD=Therapist Directiveness vs. Client Directiveness, EI-ER=Emotional Intensity vs. Emotional Reserve, PaO-PrO=Past Orientation vs. Present Orientation, WS-FC=Warm Support vs. Focused Challenge
In interpreting the components and establishing scales, our primary goal was to develop a brief, practical, and multidimensional tool for routine clinical practice. That is, we privileged clinical utility over psychometric considerations. For this reason, we ensured that each resultant scale had no more than five items, had a clear and coherent clinical interpretation, but that internal consistency was acceptable (Cronbach's α ≥ .60). In constructing scales, we employed a cut off of .40 for individual marker items loading on the component, which is considered appropriate for interpretative purposes (Stevens, 2002).
The first component had 12 marker items with loadings of .40 or greater. High loading items reflected structured, therapist-led, and technique-based therapist style versus an unstructured, client-led, and non-technical therapist style. This component was labelled Therapist Directiveness vs. Client Directiveness (TD-CD). One item was removed because its loading was substantially lower than the other items. The remaining 11 items had an alpha coefficient of .89. However, the six lowest loading items could be removed without substantial loss to internal consistency, leaving five items with the highest loading on the scale (α=.84). Hence, we retained the five highest loading items for this scale, as shown in the Appendix 1.
The second component was defined by seven marker items reflecting the expression of strong emotions and a focus on the therapy relationship versus not focusing on emotions and the relationship. As the relational items indicated a preference for greater intensity and depth of therapeutic work, we labelled this component Emotional Intensity vs. Emotional Reserve (EI-ER). Three of these items were eliminated because they were complex items cross-loading with other scales>.3 and were not conceptually coherent. However, a fifth item, Focus on feelings vs. Focus on thoughts, which loaded on this scale just below our .40 threshold, was conceptually consistent with the other items and increased scale reliability. Hence, we retained five items for this scale (Cronbach's α=.67).
Our third component was defined by three strong items representing a temporal dimension: focusing on the past versus focusing on the present or future. Hence, we labelled this scale Past Orientation vs. Present Orientation (PaO-PrO). As the other marker items had lower loadings on this factor, reduced the internal consistency, and were conceptually inconsistent with this temporal dimension, they were eliminated. That left three items (α=.73) on the scale.
The fourth and final component was defined by six marker items reflecting a dimension of wanting support and understanding versus challenge and confrontation. Hence, we labelled this scale Warm Support vs. Focused Challenge (WS-FC). Based on reliability coefficients and conceptual clarity, we ended with five items (α=.60).
Scale intercorrelations and statisticsScale scores were computed for each participant on each of the four scales. The scores equaled the unweighted sum of each of the items constituting the individual scales. In each case, a higher score indicated a greater preference for the first term in the scale title. As shown in the Appendix, the resultant 18-item instrument contains 5 negatively scored items to decrease an acquiescent response bias.
Scales scores were intercorrelated and revealed modest relationships to each other. A preference for Therapist Directiveness showed a small negative association with a preference for Emotional Intensity (r=-.18), a small positive correlation with a preference for Past Orientation (r=.15), and a moderate negative correlation with a preference for Warm Support (r=-.34). A preference for Emotional Intensity showed a small positive correlation with a preference for Past Orientation (r=.13). All other inter-scale correlations were statistically and practically non-significant.
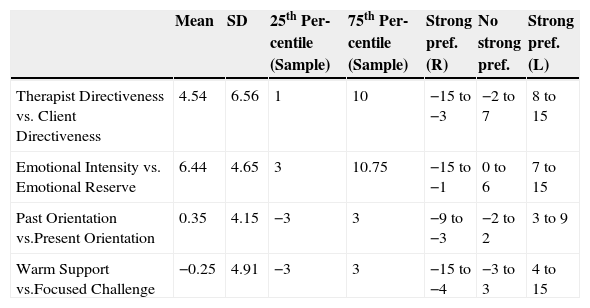
For clinical purposes, we established cut points for strong preferences on our four scales. A “strong” preference was operationally defined as a respondent score in either the top or bottom 25th percentile of the distribution. For this part of our analysis, we used the data from laypersons only as we expected that the therapy preferences of mental health professionals would be strongly influenced by their training, theoretical orientation and experience.
Scores on two scales for the sample were positively skewed (TD-CD and EI-ER, Table 4). This meant that cut points for strong preferences based on those distributions, alone, would have ignored genuine population preferences for more directive and emotionally intense therapist activities. Hence, we opted for a cutting score that was midpoint between: 1. the empirical lower and upper quartiles of the sample distributions of each scale score, and 2. the quartile cutting points based on standardising the scores to the scale mean (0) and sample standard deviation, assuming standard Gaussian distributions for each score. We rounded the midpoint scores downwards (for the lower end scores) and upwards (for the upper end scores). These cut-off scores are presented on the instrument itself, as seen in Appendix 1.
Scale statistics of the C-NIP.
| Mean | SD | 25th Per-centile (Sample) | 75th Per-centile (Sample) | Strong pref. (R) | No strong pref. | Strong pref. (L) | |
|---|---|---|---|---|---|---|---|
| Therapist Directiveness vs. Client Directiveness | 4.54 | 6.56 | 1 | 10 | −15 to −3 | −2 to 7 | 8 to 15 |
| Emotional Intensity vs. Emotional Reserve | 6.44 | 4.65 | 3 | 10.75 | −15 to −1 | 0 to 6 | 7 to 15 |
| Past Orientation vs.Present Orientation | 0.35 | 4.15 | −3 | 3 | −9 to −3 | −2 to 2 | 3 to 9 |
| Warm Support vs.Focused Challenge | −0.25 | 4.91 | −3 | 3 | −15 to −4 | −3 to 3 | 4 to 15 |
Note. Strong pref. (R)=Strong preference for right-hand term in title, Strong pref. (L)=Strong preference for left-hand term in title.
Building on previous efforts, we created a brief, multidimensional, and reliable measure of client therapy preferences for use in routine clinical practice. Through principal component analysis, we ended with an 18-item, 4-scale instrument with acceptable internal consistency that converges well with the practical dimensions along which therapists may be willing to adapt their practice. That instrument, titled the Cooper–Norcross Inventory of Preferences (C–NIP), is presented in the Appendix. It is licensed under the Creative Commons Attribution-NoDerivatives 4.0 International licence so it can be reproduced, used and distributed without payment of any fee as long as it is not changed and its origin acknowledged (by citing this paper).
Dimensions of preferencesThe PCA identified four robust dimensions of client preferences for therapists’ activities: Therapist Directiveness vs. Client Directiveness, Emotional Intensity vs. Emotional Reserve, Past Orientation vs. Present Orientation, and Warm Support vs. Focused Challenge. These components can be compared against the factors that have emerged in analyses of other client preference measures (e.g., Hatchett, 2015a; Levy Berg, Sandahl, & Clinton, 2008; Aylindar & Cooper, 2014; Watson, 2015). As these analyses have been conducted independently, and with separate samples, they provide an opportunity to develop a triangulated understanding of the key dimensions underlying therapy preferences.
Across all of these instruments, two consistent factors have emerged: level of therapist directiveness and amount of therapist support. The desire for therapist direction materialized as the first component in the present analysis, the PEX Outward Orientation factor (Levy Berg et al., 2008), and the Therapist Direction component in the TPF (Watson, 2015). In the PCCI analysis (Hatchett, 2015a), this factor is divided into Therapist Directiveness and Task Oriented activities; and Aylindar & Cooper's (2014) analysis of TPF-A data also distinguished between Directiveness and Task Focus. However, it is not clear how robust this distinction is. The correlation between subscale scores was.42 (Hatchett, 2015a) and in another analysis (Aylindar & Cooper, 2014), the Directiveness dimension showed poor internal consistency. The second dimension of desire for therapist support is found in the present analysis, the Therapist Warmth subscale of the PCCI (Hatchett, 2015a), and the Support subscale of the PEX (Levy Berg et al., 2008).
These two factors, directiveness and support, seem to map closely on to the agency and communion dimensions, respectively, of the interpersonal circumplex (e.g., Horowitz et al., 2006; Wiggins, 1979). The convergence of these client preference dimensions onto this well-established interpersonal model provides further support for the centrality of warmth and directiveness as underlying client preference factors. It also suggests that client preferences for therapist activities may reflect a broader set of interpersonal needs and relational expectations.
In contrast to these two replicated dimensions, the other preference factors that emerged from our—and other—statistical analyses of client preference data have been less consistent. The temporal dimension in our analysis replicated findings from the TPF (Aylindar & Cooper, 2014; Watson, 2015) and bears some proximity to the Inward Orientation dimension in the PEX (Levy Berg et al., 2008). However, Inward Orientation is a broader concept that can refer to insights about present and future experiences, as well as the past. Hence, it may be that these dimensions are somewhat independent. This is supported by our finding that the insight items did not show a strong loading on the Past Orientation vs. Present Orientation dimension.
Our fourth preference component on emotional expression in therapy bore relationship to the PEX dimension of Catharsis (Levy Berg et al., 2008): both referring to the desire for intense emotions. In the PCCI analysis (Hatchett, 2015a), however, the emotionally expressive items, such as “I would like to experience my feelings more intensely,” were on a single dimension with the inward orientation items. In fact, a previous iteration of the PCCI had attempted to separate out scales for emotional- and insight-oriented preferences (Hatchett, 2015b), but the covariations between these subscales were high (r=.70), and they did not factor out in a subsequent analysis (Hatchett, 2015a).
LimitationsThe C–NIP in current form suffers from a number of limitations, both psychometric and practical in nature. Psychometrically, the internal reliabilities on two scales were less than ideal (below .70). However, as the inventory needs to be brief and is intended as the basis for a clinical dialogue, rather than as a formal psychological test, these were considered acceptable for our purposes. Our use of a convenience sample, and particularly one with a high proportion of mental health professionals responding in a client capacity, was also a limitation of the development procedure. As well, this study did not include checks on the concurrent or predictive validity of the measure, its test-retest reliability, or the psychometric properties of the final 18-item measure with a clinical population. Caution is needed, therefore, in using the scale for empirical or clinical purposes until further population-appropriate validity information is available.
Practically, the instrument is limited by skewed response distributions on two of our scales. However, this reflects the clinical reality that clients tend to prefer directive and emotionally intense therapist activities, and our cut points strive for a balance between absolute and relative expressions of strong preferences. As with all preference measures, there are also the limitations that clients may not be able—or willing—to articulate what they want from therapy, and what they articulate may not necessarily be what is of most therapeutic value to them.
Clinical practicesWithin these constraints, the C–NIP can be directly and freely used within clinical settings to initiate a dialogue with clients. Preliminary cut off scores (see Appendix 1) have been developed to facilitate identification of strong preferences. The inventory is quickly and easily hand-scored. Doing so has evidence of client acceptability, even satisfaction (Bowen & Cooper, 2012; Cooper, Wild et al., 2015).
People enter therapy with certain preferences, and it is clear that effectiveness of therapy is closely linked to these. If the therapist's style differs markedly from the patient's ideas about the relationship to which he or she would respond, positive results are less likely to ensue. Addressing and accommodating client preferences have been shown to improve treatment outcomes and reduce client dropout by at least a third (Swift et al., 2011). Through stimulating a dialogue on clients’ preferences for therapy, this inventory can help develop more tailored treatments, which should better meet the needs of individual clients, and which probably leads to improved outcomes and reduced dropout.
Of course, simply because a client desires a particular therapist or relationship style does not mean that the client ought to receive it. Clinical, legal, and transference considerations still operate. It would be naive to assume that clients always know what they want and what is best for them. But if clinicians had more respect for the notion that their clients often sense how they can best be served, fewer relational mismatches and ruptures might ensue.
It is empirically unclear why assessing and addressing client preferences improves outcomes, but clinically we can offer several explanations. First is the act of respectfully asking, which develops collaboration from the outset. Second, initiating the dialogue is an empowering, supportive practice. Third, discussing client preferences (and treatment goals) early in therapy establishes task and role consensus and may correct misconceptions about the therapeutic process. All three of these relationship behaviors—collaboration, support, and consensus—are consistently related to positive therapy outcomes (Norcross, 2011). Fourth, accommodating client preferences probably reduces discrepancies between client desire and therapist behavior. Fifth and final, early in-session discussions about client preferences and the therapeutic work unifies the sessions around change.
The research has identified a couple of important caveats about matching preferences: Accommodate strong preferences whenever possible and conduct all therapy in the client's native language (Griner & Smith, 2006).
On the C-NIP, following the 18 scored formal items are 11 open questions for exploration and discussion with clients, as and where appropriate. These cover broader aspects of the therapeutic work for which research or clinical expertise suggests matching to clients’ strong preferences may be beneficial, such as frequency of sessions (Carey & Mullan, 2007) and format of the therapeutic work (Cooper, McConnachie et al., 2015).
The four dimensions of client preferences converge well with empirical studies of therapist activity and evidence-based therapy adaptations. In particular, decades of research demonstrate the value of adapting the degree of therapist directiveness to client reactance level. Specifically, clients presenting with high reactance benefit more from self-control methods, minimal therapist directiveness, and paradoxical interventions. By contrast, clients with low reactance benefit more from therapist directiveness and explicit guidance. This strong, consistent finding can be expressed as a large effect size (d) averaging .76 (Beutler, Harwood, Kimpara, Verdirame, & Blau, 2011). Other evidence-based therapy adaptations (Norcross, 2011) are probably assisted by the results of client scores on the C-NIP, such as to coping style, culture, spirituality/religion, and stage of change.
Future directionsFurther research is needed to explore the clinical utility of the C-NIP. This research can include both client and therapist ratings of the helpfulness of the measure. There is a need for further norming and psychometric studies, using the 18-item set, with more diverse samples. More broadly, there is a need to develop a clearer understanding of factors underlying client preferences. This includes establishing whether therapist directiveness and task focus, and past focus and insight orientation, are heterogeneous or homogenous dimensions. Research might also benefit from drawing on theoretical models, as Levy Berg and colleagues (2008) have done with coping styles. For instance, research into attachment styles (Ainsworth, Blehar, Waters, & Wall, 1978) could be utilized to develop and test the desire for warm support on the C-NIP and other dimensions of interpersonal preferences. From the present research, the interpersonal circumplex may prove a fruitful source for developing and refining preference measures (Horowitz et al., 2006).
Thanks to Suzan Aylindar, Maria Bowen, Angela Couchman, Audrey D’Costa, Chris Evans, John McLeod, John Mellor-Clark, Brian Murray, Regina Pauli, Joshua Swift, Vicki Watson and Bobbi Vollmer.
Portions of this article were presented by the second author in a keynote address at the 8th International Congress of Clinical Psychology, Granada, Spain, November 2015.