Background/Objectives: This study aimed to explore the psychometric properties of BI-AAQ (Body-Image Acceptance and Action Questionnaire) and the body image psychological flexibility role as a mediator in a pervasive path towards binge eating in Brazilian samples. Method: This cross-sectional study was conducted in clinical (overweight or obese women currently in treatment for weight loss; n= 330) and non-clinical (general population; n= 682) groups of women. Results: BI-AAQ has one-factor structure, excellent internal consistency, ability to detect differences between groups and measurement invariance across samples. It was also negatively associated with self-compassion and positively associated with binge eating severity, drive for thinness and self-criticism. Conclusions: This study provides data confirming the robust psychometric properties of BI-AAQ in qualitatively different samples. Furthermore, an additional study conducted in a clinical sample of women with overweight or obesity revealed that body image psychological inflexibility has emerged as a partial and significant mediator of the effect of self-criticism and drive for thinness on binge eating severity.
Antecedentes/Objetivo: Este estudio tuvo como objetivo explorar las propiedades psicométricas del BI-AAQ (Body-Image Acceptance and Action Questionnaire) y el papel mediador de la inflexibilidad psicológica relacionada con la imagen corporal en una trayectoria nociva hacia la ingesta compulsiva en muestras brasileñas. Método: Este estudio transversal se llevó a cabo en grupos clínicos (mujeres con sobrepeso u obesidad actualmente en tratamiento para la pérdida de peso; n= 330) y no clínicos (grupo de población general; n= 682) de mujeres. Resultados: BI-AAQ presenta la estructura de un factor, excelente consistencia interna, capacidad para detectar diferencias entre grupos e invariancia de medida entre diferentes muestras. Sus puntuaciones se asociaron negativamente con la autocompasión y positivamente con la severidad de la compulsión alimentaria, búsqueda de la delgadez y autocrítica. Conclusiones: Este estudio proporcionó datos que confirman que el BI-AAQ tiene propiedades psicométricas sólidas en muestras cualitativamente diferentes. Además, un estudio adicional efectuado en una muestra clínica de mujeres con sobrepeso u obesidad reveló que la inflexibilidad psicológica relacionada con la imagen corporal emergió como mediadora parcial y significativa del efecto de la autocrítica y de la búsqueda de la delgadez sobre la severidad de la compulsión alimentaria.
The role of body image dissatisfaction (BID) in the aetiology of disordered eating has been a target of empirical research (e.g., Brechan & Kvalem, 2015; Dakanalis et al., 2016; Dakanalis, Zanetti, Riva, & Clerici, 2013). It has been suggested that although BID is a rather common experience among females (Runfola et al., 2013), only a small percentage engage in disordered eating (Smink, van Hoeken, & Hoek, 2012). This seems to suggest that being dissatisfied with one's body image is a factor that might interact with other involved mechanisms. Recent theoretical approaches to psychological suffering have pointed out for the role of psychological inflexibility in several psychopathological symptoms (e.g. Paulus, Vanwoerden, Norton, & Sharp, 2015; Pinto-Gouveia, Gregorio, Dinis, & Xavier, 2012). Psychological inflexibility encompasses an inability to be in the present moment, as well as actions motivated by avoidance of difficult internal experiences - usually at the expense of desired valued life goals (Hayes, Strosahl, & Wilson, 1999). As so, psychological inflexibility has been associated with disordered eating (e.g. Moore, Masuda, Hill & Goodnight, 2014). For example, it was found positive associations between rigid avoidance strategies and dysfunctional eating behaviours (Cowdrey & Park, 2012). Also, it was observed that patients with binge eating disorder were less willing to experience negative emotions (Leehr et al., 2015). Conversely, psychological flexibility has been negatively correlated with overall disordered eating-related problems (e.g. Masuda & Latzman, 2012).
Psychological inflexibility is usually assessed by the Acceptance and Action Questionnaire (AAQ-II; Bond et al., 2011), even though concerns have been raised due to its lack of specificity to drawing conclusions to different clinical conditions (Wendell, Masuda, & Le, 2012). It is argued that using content-specific measures is a better suited strategy (Sandoz, Wilson, Merwin, & Kelllum, 2013), as it seems that content-specific measures are sensitive to detect significant effects in cases where general measures did not (Gifford et al., 2004). Thus, in order to tackle this limitation by providing an instrument capable of measuring psychological flexibility specifically related to body image, the Body Image–Acceptance and Action Questionnaire was developed (BI-AAQ; Sandoz et al., 2013).
It is proposed that body image flexibility (BIF), i.e., being willing to experience difficult body image internal events (e.g. perceptions, sensations, feelings, memories and thoughts) without judgments or defences, plays an important role in the disordered eating (Wendell et al., 2012). For instance, BIF seems to be a protective factor against disordered eating behaviour in low body mass index (BMI<20) females (Hill, Masuda, & Latzman, 2013), and is negatively correlated with internalization of thinness, body dissatisfaction, disordered eating thoughts (Timko, Juarascio, Martin, Faherty, & Kalodner, 2014), eating disorder symptomatology, food and weight concerns (Ferreira, Pinto-Gouveia, & Duarte, 2011; Sandoz et al., 2013) and positively associated with self-compassion (Ferreira et al., 2011). Moreover, it seems that women with less BIF endorse more disordered eating behaviours than those with greater BIF (Moore et al., 2014) and present more body dissatisfaction and drive for thinness (Ferreira et al., 2011).
Additionally, the construct underlying BI-AAQ seems to fit perfectly with conceptualizations of binge eating as a result from attempts to avoid and/or control difficult internal experiences (e.g. Gianini, White, & Mashed, 2013; Leehr et al., 2015). It is well-known that binge eating is a severe health problem associated with the development and maintenance of overweight and comorbidities with physical and psychiatric conditions (Kessler et al., 2013; Striegel-Moore et al., 2000).
Nevertheless, there is a lack of research on the underlying processes of binge eating - this topic has yet to be explored and can shed new light on the specific mechanisms of change needed in clinical interventions (Dakanalis et al., 2015). For instance, there are considerable evidence that self-criticism predicts the occurrence of binge eating (Duarte, Pinto-Gouveia, & Ferreira, 2014; Dunkley & Grilo, 2007) and that self-judgement is positively associated with drive for thinness (Ferreira, Pinto-Gouveia, & Duarte, 2013b). Additionally, the literature has suggested that drive for thinness is positively correlated with body dissatisfaction in women (Ferreira, Pinto-Gouveia, & Duarte, 2013a). However, the mechanisms underlying these associations are not explored, especially in women with binge eating behaviours. One hypothesis is that drive for thinness and self-critical thinking have the purpose of avoiding body-related internal experiences associated to social threats (see Gilbert, 2005), in which binge eating behaviours function as an avoidance strategy to block those experiences. Nevertheless, to our knowledge, this has not been empirically tested.
In line with this, the BI-AAQ seems to be a valuable measure that can help clarify the role of BIF in the prevention and treatment of dysfunctional eating behaviours. In fact, its potential applicability to a wide range of weight concerns makes it a very useful tool. However, the unavailability of BI-AAQ's translation and validation studies into different languages and cultures, as well as the lack of additional psychometric studies, limit its utility.
Regarding the BI-AAQ's factorial structure, Exploratory Factor Analyses (EFA) separately conducted in two independent college student samples, corroborated the proposed 12-items and one-factor structure (Sandoz et al., 2013). However, the original validation study did not perform a Confirmatory Factor Analysis (CFA) in order to test whether or not the proposed structure had a good fit to the data. This limitation was overcome by the Portuguese (Ferreira et al., 2011) and Persian (Izaadi, Karimi, & Rahmani, 2013) validation studies, which have both confirmed its one-factor structure.
Yet, as far as we know, there are no other studies regarding BI-AAQ's psychometric properties. Thus, no study on its measurement invariance was conducted which prevents us from establishing that BI-AAQ measures the same construct, in the same way, when responded by qualitatively distinct groups (Widaman & Reise, 1997). Hence, one major goal of the current study is to conduct a multi-group factor analysis in order to test the BI-AAQ's measurement invariance.
Furthermore, as acknowledged by the original authors, the generalizability of their findings will also depend on the BI-AAQ's validation in clinical samples, as well as in different cultures (Sandoz et al., 2013). Therefore, and taking into consideration that all factorial structure analyses of BI-AAQ were conducted in non-clinical samples, it is crucial to also confirm its structure in a sample composed of participants from clinical contexts.
Considering this background, the present study aims: (1) to translate the BI-AAQ into Brazilian-Portuguese; (2) to confirm its factorial structure and measurement invariance across clinical and non-clinical groups; (3) to study its internal consistency, concurrent validity and its sensibility to detect differences between groups; and (4) to test whether body-image inflexibility emerges as a mediator of the effect of drive for thinness and self-criticism on binge eating severity in a clinical sample of women with overweight and obesity in treatment for weight loss.
MethodDesign and ethical aspectsThis is a cross-sectional study. Samples in which this study was conducted were part of a major research project that aims to explore eating behaviours and emotional-related difficulties in adult women. This major project was approved by the Scientific Committee of Psychology Faculty (official letter n° 014/2013) and also by the Research Committee of Pontifical Catholic University of Rio Grande do Sul (PUCRS), Brazil. All participants provided written informed consent after being briefed about the aims of the study and its voluntary and confidential nature.
Data collectionTwo independent samples were used in this study. The general population group was composed of women who were awaiting transportation or services in the Porto Alegre¿s Bus Station and in three citizens’ bureaus, respectively. The clinical group comprised women with overweight or obesity in medical treatment for weight loss in a public hospital in Porto Alegre. Inclusions criteria: a) female; b) age between 18 and 60 years; c) 5 or more years of education. Moreover, in order to be part of the clinical group, participants had to present a Body Mass Index (BMI) ≥ 25 (kg/m2).
Translation and adaptationTwo independent researchers (both Brazilian and fluent in English) adapted the BI-AAQ to Brazilian-Portuguese and made a back-translation to English. Then, a committee of three experts in both the underlying construct of BI-AAQ and in transcultural validations was formed with the purpose of evaluating and deciding which adaptation of each item should integrate the preliminary version of the scale. Afterwards, an analysis of each item of the preliminary version was conducted, taking into consideration the clarity of language, the practical pertinence for the target culture and the theoretical relevance, according to a 5-point Likert scale (see Cassepp-Borges, Balbinotti, & Teodoro, 2010). Then the Content Validity Coefficient was calculated (see Hernández-Nieto, 2002) and all 12 items presented CVC ≥ 8. Finally, a pilot study was conducted in a sample of 22 Brazilian adults (being 45.5%, n= 10 females), with an average of 13.59 years of education (SD=3.32), and of 32.45 years of age (SD=10.22). Regarding marital status, the majority were single (62.8%; n=15) followed by married (31.8%, n=7). This pilot study showed that BI-AAQ was clearly understood, so the final version was consolidated and the data collection was initiated.
ParticipantsThe statistical analyses were performed in the following samples.
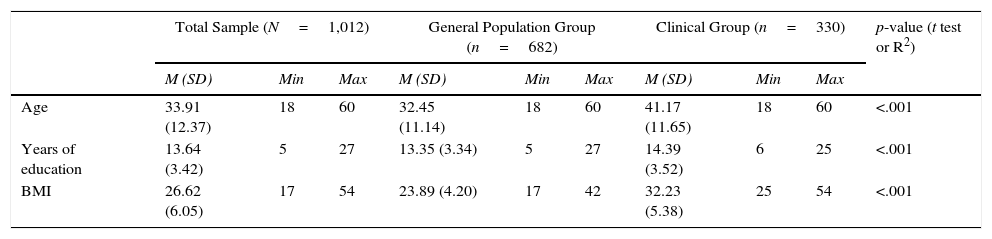
Sample 1: composed of two groups (general population, n=682; and clinical group, n=330), which comprises 1,012 participants. Table 1 presents the socio-demographic characteristics of the total sample and of each group.
Sociodemographic characteristics of Sample 1.
| Total Sample (N=1,012) | General Population Group (n=682) | Clinical Group (n=330) | p-value (t test or R2) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M (SD) | Min | Max | M (SD) | Min | Max | M (SD) | Min | Max | ||
| Age | 33.91 (12.37) | 18 | 60 | 32.45 (11.14) | 18 | 60 | 41.17 (11.65) | 18 | 60 | <.001 |
| Years of education | 13.64 (3.42) | 5 | 27 | 13.35 (3.34) | 5 | 27 | 14.39 (3.52) | 6 | 25 | <.001 |
| BMI | 26.62 (6.05) | 17 | 54 | 23.89 (4.20) | 17 | 42 | 32.23 (5.38) | 25 | 54 | <.001 |
| n | % | n | % | n | % | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Marital status | ||||||||||
| Married/cohabiting | 366 | 36.2 | 189 | 27.7 | 177 | 53.6 | <.001 | |||
| Divorced | 70 | 6.9 | 36 | 5.3 | 34 | 10.3 | ||||
| Widowed | 9 | .9 | 4 | 0.6 | 5 | 1.5 | ||||
| Single | 567 | 56 | 453 | 66.4 | 114 | 34.5 | ||||
| Occupational status | ||||||||||
| Retired | 52 | 5.1 | 17 | 2.5 | 35 | 10.6 | <.001 | |||
| Employed | 603 | 59.6 | 377 | 55.3 | 226 | 68.5 | ||||
| Unemployed | 357 | 35.3 | 288 | 42.2 | 69 | 20.9 | ||||
Sample 2: this was a subgroup from the clinical group of Sample 1 (n= 294) composed of participants who responded the following set of measures: BI-AAQ, SCS, BES and EDI-2. This subgroup presented a mean age of 41.87 years old (SD= 11.47), an average of 14.66 (SD= 3.54) years of education and of 32.38 (SD= 5.25) of BMI. Regarding marital status, 34% (n= 100) were single, 54.8% (n= 161) were married/cohabiting, 9.9% (n= 29) divorced and 1.4% (n= 4) were widowed. Additionally, the majority of participants were employed (70.1%, n= 206), followed by unemployed (18.7%, n= 55) and retired (11.2%, n= 33).The clinical and non-clinical groups from Sample 1 were used to perform the analyses aimed to confirm the BI-AAQ's factorial structure, its measurement invariance across groups as well as its ability to detect differences between them. Sample 2 was used to conduct the concurrent validity and mediational analyses.
MeasuresBody Image Acceptance and Action Questionnaire (BI-AAQ; Sandoz et al., 2013). This is a 12-item 7-point Likert-like scale (from 1 never true to 7 always true) of psychological (in)flexibility specifically developed for assessing (in)flexible responding to body-related thoughts and feelings. BI-AAQ resulted from a pool of 46 items adapted from other general AAQ versions, which were submitted to an item-total correlation analysis, where items with item-total correlations <.30 were omitted (n=17). The remaining 29 items were submitted to a Principal Factor Analysis (PFA) and to a Parallel Analysis (PA). Those results revealed a single factor structure accounting for 34.4% of the variance, where 26 items had factor loading above .40. So, in order to produce a shorter length measure, 12 items with factor loadings above .60 were retained. Finally, the 12-items version was re-examined in an independent sample where the PFA and the PA were replicated. Results supported the stability of the one-factor structure, which accounted for 54% of the variance (Sandoz et al., 2013). Additionally, the BI-AAQ's Portuguese validation have also performed a PFA and its results indicated a one-factor solution accounting for 63.36% of the variance (Ferreira et al., 2011). This one-factor 12-items solution was confirmed through CFA analyses in the Portuguese and Persian studies (Ferreira et al., 2011; Izaadi et al., 2013). Internal consistency analysis revealed an excellent Cronbach's alpha (α=.92 and α=.93) in the original validation sub-studies.
Self-Compassion Scale (SCS; Neff, 2003; Brazilian version: Souza & Hutz, 2016) is a 26-item 5-point Likert self-report measure (from 1=almost never to 5=almost always) developed to assess trait levels of self-compassion. Although SCS was initially designed to grasp three components that interact with each other (self-kindness versus self-judgment, common humanity versus isolation and mindfulness versus over-identification), it can also be used as a two-factor structure measure: one factor that assess self-compassion attitude (sum of self-kindness, common humanity and mindfulness) and one factor of a self-criticism attitude (sum of self-judgement, isolation and over-identification). This two-factor structure has adequate model fit and good internal consistency (α=.91 for self-compassion and α=.89 for self-criticism) (Costa, Marôco, Pinto-Gouveia, Ferreira, & Castilho, 2015).
Eating Disorder Inventory (EDI-2; Garner, Olmsted, & Polivy, 1983). Composed by eight subscales represented by a total of 64-items. The respondents have to rate the frequency in which what is described in each item reflects their experience, according to a 6-point Likert scale (from Always to Never) through which they rate the extent to which the items reflect their experience. For the current study, it was only used the Drive for Thinness (DT) subscale. The Portuguese validation found an excellent internal consistency for DT subscale (α= .91; Machado, Gonçalves, Martins, & Soares, 2001), corroborating the findings from the original study which observed α=.85.
Binge Eating Scale (BES; Gormally, Black, Daston, & Rardin, 1982). This measure is composed of 62 statements (arranged in 16 items) used to evaluate the severity of binge eating symptoms. For each item participants have to decide which statement (between three or four alternatives) better applies to them. Then, a score from 0 to 3 is assigned for each marked statement and the total score is calculated. Higher scores indicate higher binge eating severity. BES has high internal consistency in the original study (Gormally et al., 1982) as well as the Brazilian version (α=.89; Freitas, Lopes, Appolinario, & Sichieri, 2002).
Analytical strategiesDescriptive statistics were assessed through SPSS statistics software (v.20; SPSS Inc., Chicago, IL), while the Confirmatory Factor Analysis (CFA) and Multigroup Analysis (MA) were performed using AMOS software (v.19, SPSS Inc., Chicago, IL). Outliers were assessed through the squared Mahalanobis Distance (MD2) considering values of p1 and p2<.05 (Marôco, 2010). Normality was assessed according to values of Skewness (Sk) and Kurtosis (Ku), where values of Sk>|3| and Ku>|10| indicate severe violations of normality (Kline, 2010). Cases with missing values were excluded since they were completely at random and less than 5% of cases (Tabachnick & Fidell, 2014), according to the results from the Missing Value Analysis (MVA) procedure, which is provided by SPSS. A Confirmatory Factor Analysis (CFA) was performed to test if the one-factorial structure proposed by the authors of BI-AAQ (Sandoz et al., 2013) had good adjustment to the data. A combination of goodness-of-fit indices was used as suggested by Kline (2010): Tucker-Lewis Index (TLI), Comparative Fit Index (CFI), Goodness of Fit Index (GFI), Incremental Fit Index (IFI, also known as BL89), Relative Fit Index (RFI) and Normed Fit Index (NFI). TLI, RFI and NFI can vary between 0 and 1 - and the closer to 1, the better the fit of the model. CFI, IFI and GFI values ≥ .90 indicate a good fit (Hu & Bentler, 1999). Finally, the local adjustment was assessed both by standardized factor weights and the individual reliability of the items, considering of λ ≥ .50 and R2 ≥ .25 (Hair, Black, Babin, & Anderson, 2014), respectively. Maximum Likelihood was used as the estimation method (since the BI-AAQ response rate have 7 points–see Rhemtulla, Brosseau-Liard, & Savalei, 2012). Moreover, a chi-square test of differences was calculated (as described in Marôco, 2010) to test whether the final model has better fit to the correlational structure of the items than the original one. Internal consistency was assessed by Cronbach's alpha (values of α>.70 indicates adequate reliability - Kline, 2000). A multi-group analysis was conducted to test the measurement invariance across clinical and non-clinical groups (through the comparison of the unconstrained model with a model in which factor loadings were constrained; Byrne, 2016). Furthermore, the BI-AAQ's ability to detect differences between groups was analysed through a Student's T Test. Cohen's d was calculated to verify effect size which can be small (]0.2; 0.49]), intermediate (]0.5; 0.79] or large (≥.80) (Cohen, 1988). Concurrent validity was assessed by Pearson's correlations between the BI-AAQ, BES, SCS and Drive for Thinness (EDI Subscale). Finally, the mediational study was conducted through a Path Analysis using Maximum Likelihood as the estimation method. A bootstrap method with 2,000 resamples was performed, as it is one of the most reliable and powerful method to evaluate the significance of the direct, indirect and total standardized effects (Marôco, 2010) providing greater statistical power and confidence interval precision regardless of sample size, effect size or level of statistical significance (Mallinckrodt, Abraham, Wei, & Russell, 2006). A 95% bias-corrected confidence interval was considered (Kline, 2010).
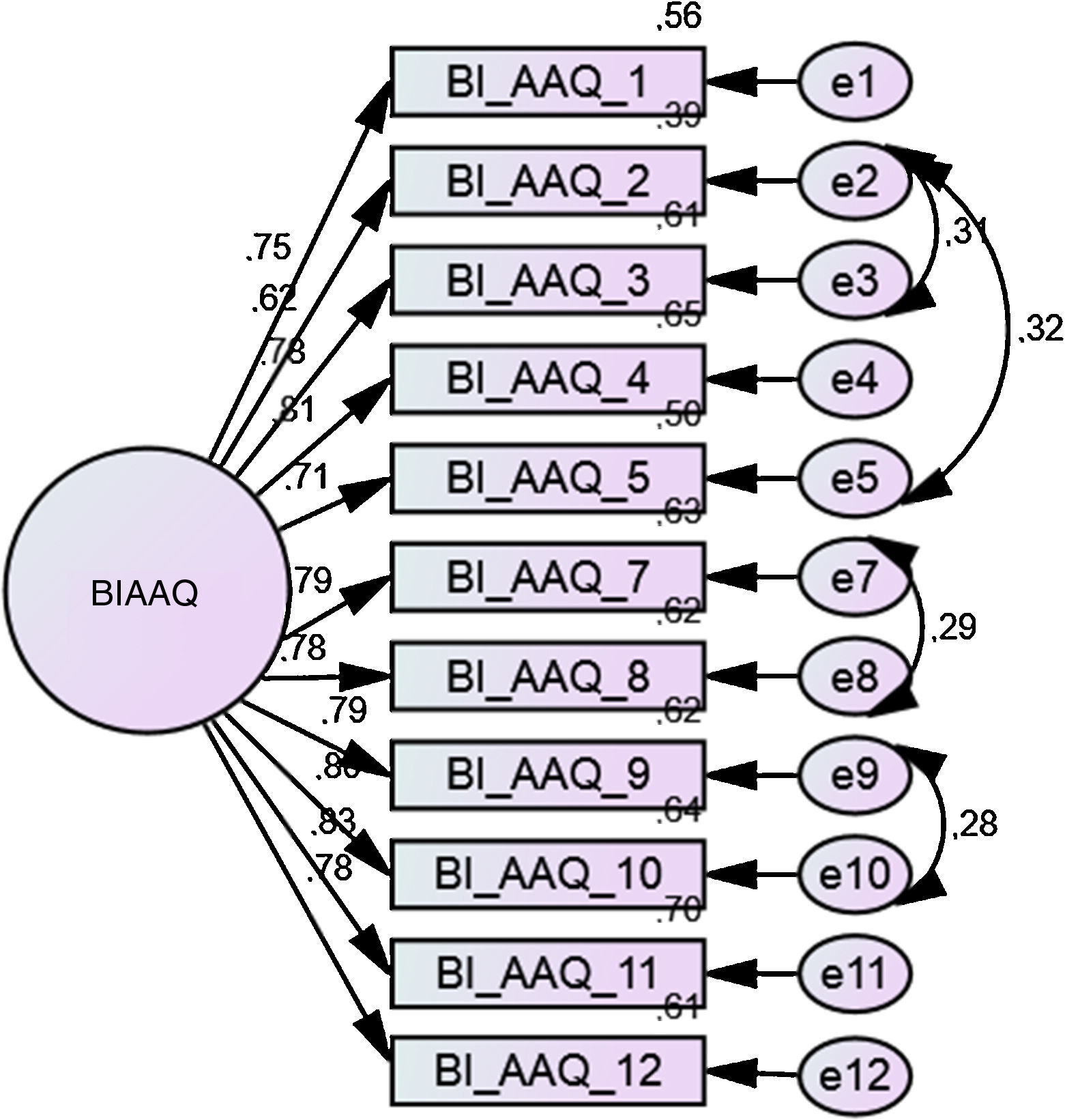
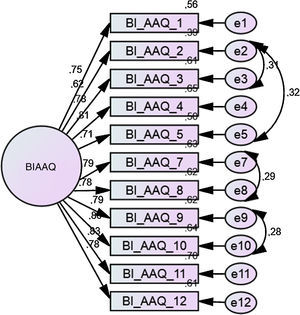
ResultsConfirmatory Factor AnalysisThe initial model was specified with all items pertained to a single factor, as proposed by the authors of BI-AAQ (Sandoz et al., 2013), which demonstrated a poor fit (χ2(54) =793.08; p<.001; CFI=.91; GFI=.87; TLI=.89; IFI= .91; RFI= .885; NFI= .90). Regarding local adjustment, all items presented high values of factor weights and individual reliability (λ≥ .64 and R2≥ .41, respectively) with exception of item 6 which presented λ≥ .44 and R2≥ .20.
The global model fit would be improved through the correlation between several pairs of item's errors according to the modification indices. However, it was only theoretically justifiable the correlation of the following pairs of item's errors: 2&3 (disturbing internal experiences regarding body shape and/or weight), 2&5 (excessive worry about the body), 7&8 (necessity to feel better or in control about body-related difficulties and its consequences for one's life), and 9&10 (influence of dissatisfaction with weight on one's life). It is a common procedure to add paths to the model correlating errors of items from the same factor, as long as these correlations have theoretical reasons (i.e. similar content or formulation; Marôco, 2010). Thus, the model was modified through the addiction of the aforementioned paths.
Even though the modified model presented an increase in the global fit indices (χ2(50) =424.27; p<.001; CFI=.95; GFI=.93; TLI=.94; IFI= .95; RFI= .93; NFI= .95), the local adjustment of item 6 still presented factor weights and individual reliability bellow the expected (λ≥ .45 e R2≥ .20, respectively). Furthermore, according to the values of “alpha if item deleted”, all items are contributing for the internal consistency of this measure with the exception of item 6 (its exclusion would increase the Cronbach's alpha from α=.93 to α=.94). Finally, the communalities’ analysis indicate that all items presented values ≥.47 with the exception of item 6, which presented the lowest value (.23). Thus, taking into consideration all these data together, we decided to exclude item 6 from the model. Therefore, a final model with 11 items was specified maintaining the same error's correlations that were made in the last model (see Figure 1). The final model presented a good global fit and did not show problems in the local adjustment (λ≥ .62; R2≥ .39).
Additionally, a chi-square difference test confirmed that the final model presented a significantly improvement when compared to the modified model (Δχ2(10)=33.835; p< .05). It is also worth mentioning that the final model presented lower levels of MECVI (.438) than the modified one (.476), showing that the final model presents better validity in the studied populations.
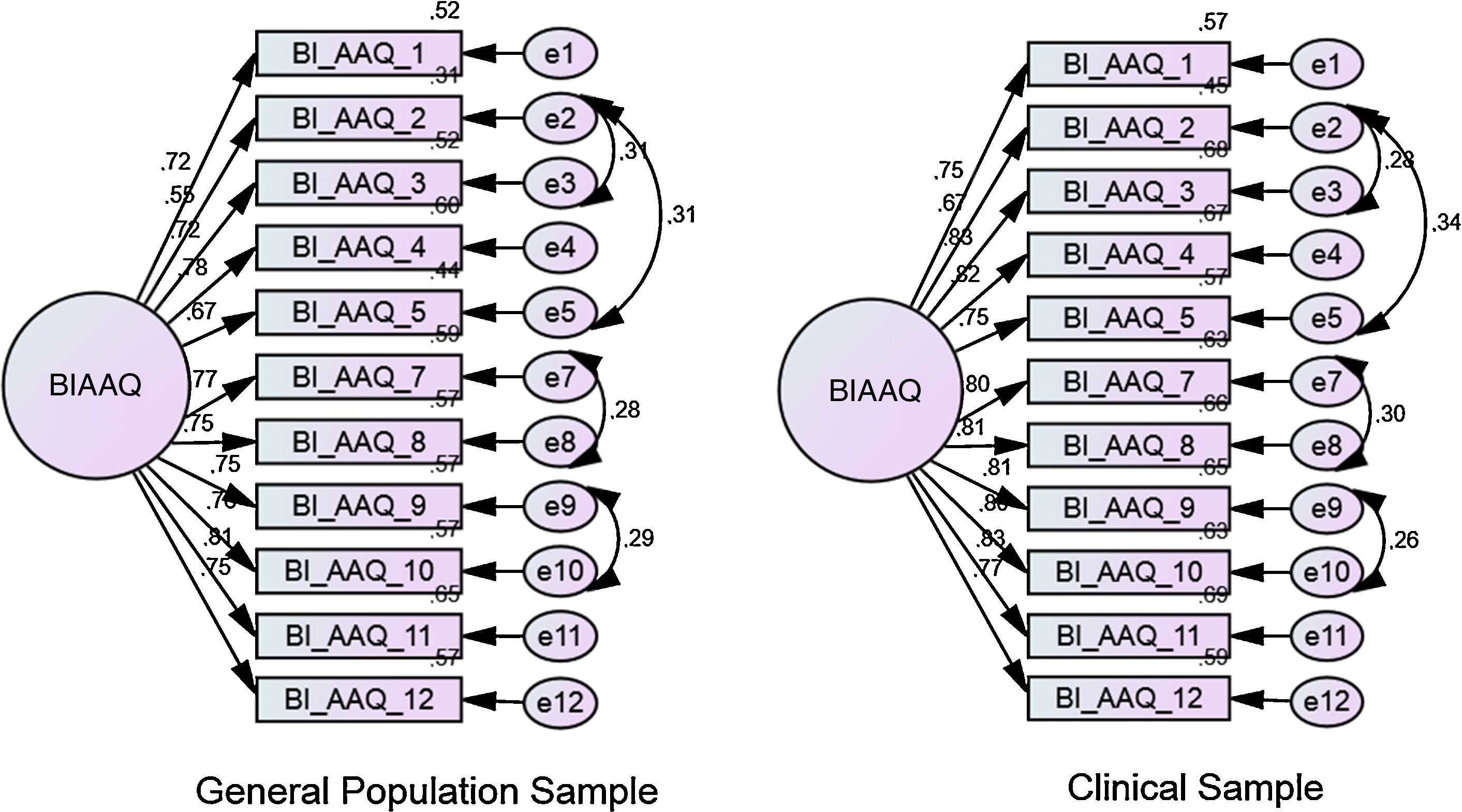
Multi-group analysisThe final model presented good fit indices, high values of factor weights and individual items reliability (λ≥ .55 e R2≥ .31). Figure 2 presents the standardized factor weights and individual reliability of the items in each group.
No differences were detected in regard to factor weights (Δχ2(1)=1.911; p= .167), showing measurement invariance.
Internal consistencyBI-AAQ presented a Cronbach's alpha of α=.94, α=.95 and α=.93, in the total sample, clinical and non-clinical groups, respectively.
Ability to detect differences between groupsSignificant differences between clinical and non-clinical groups were found (t(622)= -11.19; p<.001), being the scores of the clinical group higher than the ones in the general population group: means of 45.98 (SD= 17.48) and 33.08 (SD= 16.60), respectively. Cohen's d showed an observed value of .76.
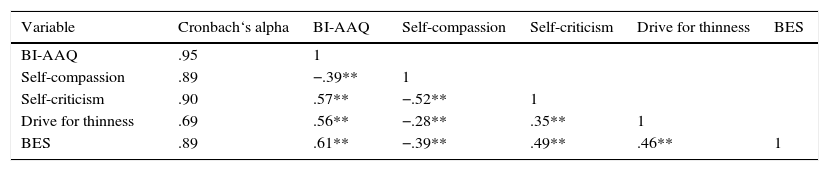
Concurrent validityCorrelations between the BI-AAQ and binge eating severity, drive for thinness, self-criticism and self-compassion were presented in Table 2 together with the values of internal consistency (Cronbach's alpha) obtained for all variables in the current study.
Correlation between BI-AAQ and variables in study (Sample 2, n=294).
| Variable | Cronbach‘s alpha | BI-AAQ | Self-compassion | Self-criticism | Drive for thinness | BES |
|---|---|---|---|---|---|---|
| BI-AAQ | .95 | 1 | ||||
| Self-compassion | .89 | −.39** | 1 | |||
| Self-criticism | .90 | .57** | −.52** | 1 | ||
| Drive for thinness | .69 | .56** | −.28** | .35** | 1 | |
| BES | .89 | .61** | −.39** | .49** | .46** | 1 |
Note: **Correlation is significant at .01 level; BI-AAQ: Body-Image Acceptance and Action Questionnaire; Self-Compassion domain of SCS (Self-Compassion Scale); Self-criticism domain of SCS; Drive for Thinness subscale of Eating Disorder Inventory-2; BES: Binge Eating Scale.
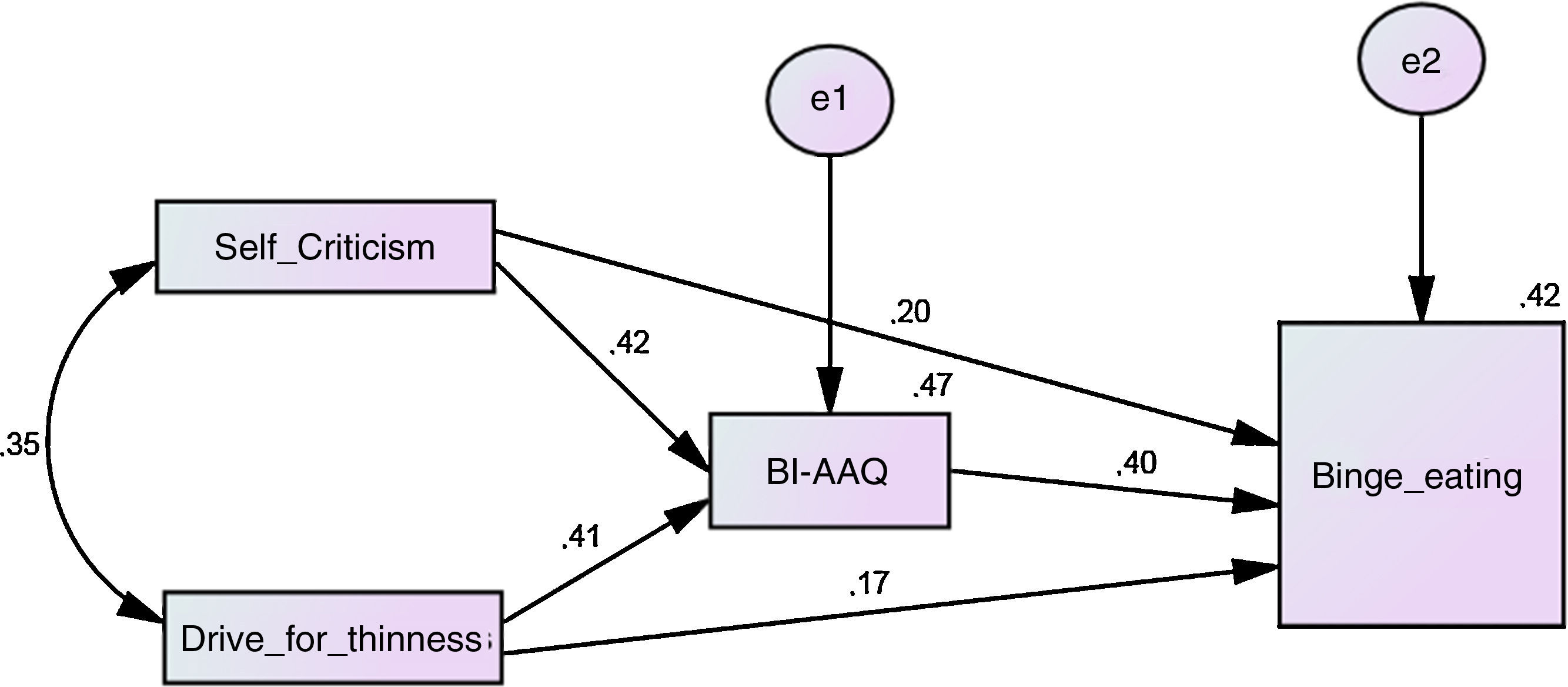
A mediational study tested a theoretical model in which the role of body image psychological inflexibility mediated the effect of self-criticism and drive for thinness on binge eating severity (Figure 3). This was a fully saturated model (containing 10 parameters), so the model fit indices were neither tested nor reported since fully saturated models always produce a perfect adjustment to the data.
Results showed a significant standardized total effect of self-criticism and drive for thinness on binge eating behavior (Self-criticism: β=.36; 95% CI=[.27; .45]; p=.001; Drive for thinness: β=.33; 95% CI=[.25; .41]; p=.001), as well as a positive and significant standardized indirect effect (through body image psychological inflexibility) of both variables on binge eating (Self-criticism: β=.17; 95% CI=[.11; .23]; p=.001; Drive for thinness: β=.16; 95% CI=[.11; .22]; p=.001). The standardized direct effect of the mediator on the criterion variable was significant (β=.40; 95% CI=[.30; .51]; p=.001). Finally, the standardized direct effect of self-criticism and drive for thinness still significant in the presence of the mediator (Self-criticism: β=.19; 95% CI=[.09; .28]; p=.001; Drive for thinness: β=.16; 95% CI=[.07; .25]; p=.004), which indicates a partial and significant mediation. The model explained 42% of binge eating severity.
Discussion/ConclusionsPrevious studies on the factor structure of BI-AAQ are scarce and were mainly conducted in college student's samples (Izaadi et al., 2013; Sandoz et al., 2013) or in general population samples (Ferreira et al., 2011). The current study included a clinical sample in its factorial analysis addressing previous limitations and expanding the knowledge of BI-AAQ’ robustness and clinical utility.
Regarding the factorial structure, the Brazilian version of BI-AAQ resulted in a one-factor structure composed of 11 items, since the item 6 was excluded from the scale. This decision was based on the data regarding global and local adjustment, modification indices, factor weights and individual reliability. Corroborating our choice is the fact that item 6 had the lowest psychometric properties (namely the lowest values of standardized regression weights, squared multiple correlations, corrected item-total correlations and communalities) when compared to all the other items in the BI-AAQ's Portuguese version. Also regarding item 6 performance in the Portuguese validation, it was observed that the Cronbach's alpha value would slightly increase from .94 to .94 by excluding this item (Ferreira et al., 2011). Moreover, both in the second and third studies conducted in the original BI-AAQ's validation, it was found that item 6 was not contributing to the observed Cronbach's Alpha values (i.e., in case of item 6 exclusion, the observed internal consistency would have stayed unaltered). Finally, while most item-total correlations were over .62 in the second study of BI-AAQ's validation, the item 6 only presented a correlation of .39 (Sandoz et al., 2013).
About this topic, it is interesting to note how the items are structured and what they are assessing. BI-AAQ's items were developed using general terms to assess psychological states related to body-image (e.g., “worrying”/“thinking”/to “care too much”/“to feel bad”/“to feel better”/“to think” about weight, body and/or body shape – items 1-3, 5, 7, 11; to “change”/to “control” thoughts and/or feelings about body weight and/or shape-items 4 and 8; “to feel fat”/“feeling fat” – items 6 and 10; to “control” weight-item 9; to be bothered by body weight and/or shape – item 12) together (or not – see item 2) with possible consequences in one's life (e.g., having difficulties in living a valued life, to make any serious plans, to have better control over life, to do other things or to have better relationships-items 1, 4, 7-9, 11-12; to “shut down” – item 3; to waste too much time-item 5; having “problems” in life – item 10). Nevertheless, while the aforementioned items have used general terms (which makes it easier for respondents to identify themselves with the situations described), the item 6 seems to assess a specific strategy used in order to deal with a body image-related internal experience (i.e., “If I start to feel fat, I try to think about something else” – item 6). Thus, in our opinion, the poorer psychometric properties observed in item 6 can be explained by its narrower content: it seems to assess a specific avoidance strategy (i.e., distraction) rather than the more broadly function of psychological inflexibility.
The final model (without item 6) presented a good local adjustment, with high levels of factor weights and individual reliabilities in the remaining items. The Brazilian version of the BI-AAQ also showed a good global fit. These results are in accordance with the Persian, Portuguese and the original validations, which also supported the BI-AAQ's one-factor structure (Ferreira et al., 2011; Izaadi et al., 2013; Sandoz et al., 2013).
Furthermore, we found that the Brazilian version of the BI-AAQ has an excellent internal consistency (α=.94 total sample, α=.93 general population group, and α=.95 clinical group). These results are in line with previous studies of BI-AAQ, as the Persian, Portuguese and the original validations found internal consistencies of α=.87 (Izaadi et al., 2013), α=.95 (Ferreira et al., 2011) and of α=.92 (Sandoz et al., 2013), respectively. Results also showed that all 11 final items were contributing to the internal consistency of the measure.
Moreover, the multi-group analysis showed structural invariance, showing that its structure remains stable across our different samples. To our knowledge, this is the first study that tested the invariance of the factorial structure of BI-AAQ.
Furthermore, BI-AAQ's ability to detect differences between clinical and non-clinical groups was also corroborated, since significant differences between groups were detected with intermediate effect sizes (the clinical group had higher scores than the general population group). Similar results were found in the Portuguese validation, where the measure discriminated between a diagnosed eating disorder sample and a general population sample, with the clinical group reporting lower body image flexibility (Ferreira et al., 2011).
Regarding concurrent validity, results from correlational analyses showed that BI-AAQ is positively correlated with self-compassion and negatively correlated with self-criticism, drive for thinness and binge eating severity. Therefore, the previous hypothesis that body image psychological inflexibility would be negatively related with other general psychological flexibility and acceptance constructs and positively related with psychopathology and eating and weight difficulties was confirmed. These results are in line with previous findings associating body image psychological inflexibility with less self-compassion (Ferreira et al., 2011), more eating disorder symptomatology, higher food and weight concerns, internalization of thinness, disordered eating thoughts and behaviours, and body dissatisfaction (Ferreira et al., 2011; Hill et al., 2013; Sandoz et al., 2013; Timko et al., 2014).
The current study also extends the literature on body image psychological inflexibility, by providing new data regarding its role as a mediator of the effect of the self-criticism and drive for thinness on binge eating severity. Previous empirical data have already reported the pervasive effect of self-criticism and drive for thinness on binge eating psychopathology (e.g. Duarte et al., 2014; Dunkley & Grilo, 2007), but the underlying mechanisms through which this effect occurs was still underexplored. Our results seem to suggest that a self-to-self way of relating characterized by criticism and put-down associated with a drive for thinness (i.e., intense desire to lose weight, excessive fear of gaining weight associated with an extreme pursuit of thinness; Garner et al., 1983) impacts on binge eating behaviors in part due to the unwillingness to experience difficult internal experiences related to body image and the consequent efforts to avoid these experiences. This seems to empirically corroborate recent conceptualizations, in which binge eating is presented as an emotional regulation strategy (e.g. Gianini et al., 2013; Leehr et al., 2015). Therefore, other previous findings also seems to be in line with these results, as it was suggested that body image psychological flexibility seems to lessen the impact of body image dissatisfaction (a well-established predictor of eating psychopathology) on dysfunctional eating behaviors (Ferreira et al., 2011), while another study concluded that nuclear eating disorder's features arise as a result of a self-critical attitude (Pinto-Gouveia, Ferreira, & Duarte, 2014).
Regarding clinical implications, our results suggest that future interventions should target the inflexible responding to body-related thoughts and feelings, as it seems to contribute to binge eating severity when self-criticism and drive for thinness are present. About this topic, a clinical approach for women with binge eating disorder, in which an accepting and mindful way of relating to one's difficult internal experiences was taught and trained, has been shown to be beneficial (e.g. Masuda, Hill, Melcher, Morgan, & Twohig, 2014). Nevertheless, it is important to bear in mind that the current results also suggest that self-criticism and drive for thinness seem to directly impact binge eating severity. These data seem to point out for the necessity to not only promote a more accepting and mindful stance towards body-related internal experiences, but also to target self-criticism itself. Perhaps it might be important to develop a more self-compassionate way of relating to one's perceived defects and failures, as this seems to be an effective way of diminishing self-criticism (e.g. Leaviss & Uttley, 2015).
Furthermore, it is important to consider some limitations in the current study. For one, its cross-sectional design, which prevents interpretations of causality. Moreover, our samples were convenience-based and exclusively composed of women, which may narrow the generalization of the current results to other genders.
Overall, this was the first study that demonstrated the factorial invariance of BI-AAQ in different samples. The Brazilian version of BI-AAQ presents a one-factor structure, excellent internal consistency, discriminant and concurrent validities. Additionally, this study adds new information on the role of body-image inflexibility in binge eating.
FundingThis work was supported by the CNPq (National Council for Scientific and Technological Development – Brazil; Reference: 408697/2013-0), CAPES (Coordination for the Improvement of Higher Education Personnel – Brazilian Ministry of Education; BEX Process number 0514/12-8) and FAPERGS (Foundation for Research Support of the State of Rio Grande do Sul – Brazil; Reference: 2263–2551/14-4SIAFEM). None of the sponsors have participated in the design, collection, analysis, interpretation of data, writing the report, or in the decision to submit the article for publication in this journal.