Background/Objective: Childhood maltreatment (CM) has been associated with revictimization and post-traumatic stress disorder (PTSD). However, this relation is hardly examined in South European countries, and in community samples. We tested these associations in a convenience sample of 1,200 Portuguese adults in the community. Method: Data were collected using self-report questionnaires, the Post Traumatic Diagnostic Scale (PDS) and the Childhood Trauma Questionnaire–Short Form (CTQ-SF). Odds ratios, logistic and hierarchical regression were used to analyze the data. Results: Exposure to CM increased more than twofold the risk of being revictimized and threefold a PTSD diagnosis. Highly prevalent traumatic events such as accidents were associated with CM. More than 30% of adults with PTSD were exposed to emotional abuse. After adjusting for demographics, emotional abuse remained a significant predictor for revictimization and PTSD, having the largest effect on the prediction of PTSD severity (β=.24). Conclusions: Findings underline the injurious potential of emotional abuse during childhood in adults in the community. More knowledge is needed about the mechanisms linking CM with further traumatic exposure and PTSD across the lifespan to better inform preventive and therapeutic actions.
Antecedentes/Objetivo: El maltrato infantil (MI) se ha asociado con la revictimización y con el trastorno de estrés postraumático (TEPT). Sin embargo, esta relación es poco conocida en los países del Sur de Europa y en muestras comunitarias. Estas asociaciones se analizaron en una muestra de conveniencia compuesta por 1.200 adultos portugueses. Método: Los datos fueron obtenidos usando la Escala de Diagnóstico Post Traumático (PDS) y el Cuestionario de Trauma Infantil-Versión corta (CTQ-SF), y analizados con odds ratios y regresiones logísticas y jerárquicas. Resultados: La exposición a MI aumentó más del doble el riesgo de percibir revictimización y tres veces el diagnóstico de TEPT. Los eventos traumáticos frecuentes, como accidentes, se asociaron con CM. Más del 30% de los adultos diagnosticados con TEPT indicaron haber sufrido abuso emocional. Tras ajustar por factores demográficos, el abuso emocional predijo significativamente la revictimización y fue el predictor con mayor efecto en la gravedad del TEPT (β=0,24). Conclusiones: Nuestros hallazgos confirman el potential nocivo del abuso emocional en la infancia para los adultos de la comunidad. Se necesita más conocimiento sobre los mecanismos que relacional el MI con la exposición traumática y el TEPT para informar mejor sobre posibles acciones preventivas y terapéuticas.
Although exposure to early adversity is accepted as risk factor for poor health across lifespan, the underlying mechanisms for this relation remain hardly understood (Moffitt, 2013). Child maltreatment (CM) consists of abusive or neglectful acts perpetrated by parents or caregivers, having the potential to “harm, potentially harm or threaten a child” (Gilbert et al., 2009, p. 68). It has been associated with mental problems in adults, particularly post-traumatic stress disorder (PTSD) (Breslau et al., 2014; Scott, Smith, & Ellis, 2010). Although physical abuse (PA) and sexual abuse (SA) have been the most studied CM forms, emotional abuse (EA), physical neglect (PN) and emotional neglect (EN) occur as frequent as well. Based on a series of meta-analyses, estimated worldwide prevalence was 177 for PA, 267 for EA, 113 for SA and 163 for neglect (N) per 1,000 inhabitants (Stoltenborgh, Bakermans-Kranenburg, Alink, & van IJzendoorn, 2015).
Consequences of CM can remain relatively unnoticed in the short term and become manifest in later life stages (Pratchett & Yehuda, 2011). CM takes place during sensitive developmental periods, occurs mostly in chronic patterns and is frequently perpetrated by emotionally important figures/persons (Pratchett & Yehuda, 2011). Such specificities are thought to have consequences for the individual's biological (e.g., sensitization of the HPA-axis), cognitive and social functioning (e.g., negative cognitions about the self and others, impaired intimate relationships), which have been found to be consistent risk factors for PTSD (DiGangi et al., 2013).
The proposed version of the International Classification of mental health disorders specified complex PTSD as resultant of exposure to chronic stressors, such as PA and SA during childhood (Keeley et al., 2016). However, such stressors are often hidden by subsequent traumatic events. Looking into the nature of symptoms and better assessing pre-trauma risk factors can improve the prevention and the selection of treatment protocols for PTSD (DiGangi et al., 2013; Keeley et al., 2016; Timimi, 2014).
Revictimization refers to the exposure of subjects who were victimized during childhood to subsequent traumatic events (TEs) (Widom, Czaja, & Dutton, 2008). Experiencing adversity during childhood was found to increase the risk for exposure to additional TEs across the lifespan (Miron & Orcutt, 2014; Widom et al., 2008). Sexual abuse and PA were found to be predictive of revictimization in psychiatric inpatient men (Cloitre, Tardiff, Marzuk, Leon, & Portera, 2001), in victims of substantiated CM (Widom et al., 2008) and in a community sample (Desai, Arias, Thompson, & Basile, 2002). Emotional abuse and SA during childhood predicted adult rape in college women, while PA did not (Messman-Moore, Walsh, & DiLillo, 2010). In subjects with substantiated CM, PA and SA and N predicted further exposure to TEs (physical assault/abuse, sexual assault/abuse, kidnapping and/or stalking and having a family/friend murdered or commit suicide) (Widom et al., 2008).
Problems such as emotional dysregulation (Messman-Moore et al., 2010; Young & Widom, 2014) and failure to discriminate non-threat and threat related cues (Chu, Bryant, Gatt, & Harris, 2016) were found among CM exposed adults. These factors can reduce the ability for subjects to identify risks and to display adequate protective behaviors. Sleeping disorders were also suggested to increase the risk for accidents among CM subjects (Kendall-Tackett, 2002).
Although revictimization studies among CM victims do exist, findings are overrepresented for women and for exposure to SA and PA (Widom et al., 2008). Analyzed samples are frequently biased: they consisted of substantiated cases and/or economically disadvantaged groups which have an increased risk for exposure to cumulative adversity, or–the opposite–university college students having a better educational achievement (a protective factor for CM consequences) (Connolly, 2014). Moreover, as most CM cases go undetected (Gilbert et al., 2009), more knowledge is required about the risk for revictimization among subjects in the community.
Although exposure to TEs is highly frequent in subjects in the community, only a minority develops PTSD. Adults exposed to CM, particularly PA and SA, were found to have a larger risk for PTSD diagnosis and greater symptom severity than those who were not (Breslau et al., 2014). Exposure to substantiated CM in young adults predicted PTSD to an extent of about five times higher than those who were not exposed to CM (Scott et al., 2010). Similarly, Widom (1999) found that approximately 30% of victims of substantiated CM fulfilled diagnostic criteria for PTSD (37.5% for SA, 32.7% for PA and 30.6% for N). However, for low-income Brazilian outpatients, EA, SA and EN predicted significantly PTSD, but PA and PN did not (Grassi-Oliveira & Stein, 2008). Therefore, variability is expected in the associations between forms of CM and PTSD.
While there is evidence linking CM and PTSD in specific groups, such as subjects with substantiated CM and clinical samples, such links are far less known in community samples, particularly in South European countries (Gilbert et al., 2009). More knowledge is required about how forms of CM relate to subsequent traumatic exposure and PTSD in diverse cultural contexts.
Portugal has been placed among the countries highly affected by mental health disorders in Europe, with a lifetime prevalence of 42.7% (Caldas de Almeida & Xavier, 2013). Exposure to moderate to severe CM was found in about 14.7% of adults in the Portuguese community, with PA and SA having lower prevalence in Portugal than in other countries (Dias, Sales, Hessen, & Kleber, 2014). Prevalence of PTSD has been estimated in 7.8% (De Albuquerque, Soares, De Jesus, & Alves, 2003); sexual assault, violent death of family members or friends and war were reported as the most frequent TEs.
Portuguese society is still very much affected by the memories of the violent Colonial Wars in which about one million men participated between 1961 and 1975 (Ribeiro et al., 2011). A recent study among Croatian war veterans underlined the large psychiatric and somatic comorbidity for those with PTSD (Britvić et al., 2015). Despite war exposure may result in PTSD, pre-war risk factors such as CM may play a significant role in the development of the disorder. Due to the large number of war veterans, Portugal is a relevant setting to examine how the various CM forms and the background of war relate to PTSD.
Portuguese society is also plagued by high numbers of road accidents. Although fatalities have decreased in last years, the number of accidents and wounded victims have raised (Autoridade Nacional de Segurança Rodoviária, 2017). An association between CM and accidents has been suggested by Kendall-Tackett (2002).
The study of risk factors for poor mental health is a priority for Portugal, as well as for other countries. Given the evidence about how CM affects mental health, and considering that PTSD has a large psychiatric and somatic comorbidity, figuring as one of the most frequent disorders in CM persons, we investigated how these variables are related in adults in a Portuguese community sample. We examined the risks for traumatic exposure (revictimization) and for PTSD associated with CM. In addition, we investigated the effects of different forms of CM in the prediction of PTSD severity.
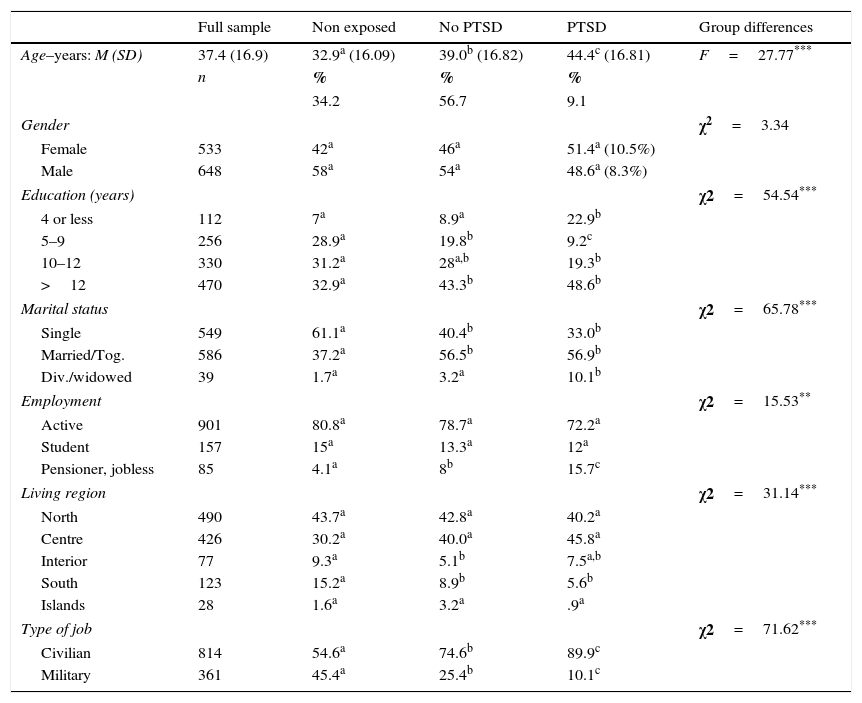
MethodParticipantsA convenience sample of 1,213 adults aged between 18 and 82 years was established with data collected in the national project “Children of Colonial War: post-memory and representations” (Ribeiro et al., 2011). Participants were recruited through personal contacts with the research team and expanded by the snowball technique. Inclusion criteria were having an age equal or larger than 18 years and Portuguese nationality. After being contacted by phone or email, participants agreed to be voluntarily assessed by health professionals at Oporto University, at the Center for Social Studies and at the Military Camp of Santa Margarida. Data collection took place between January 2008 and December 2009. No information was available about non-compliance rates. Thirteen subjects were excluded because they completed less than 90% of the questionnaires. Sample characteristics are presented in Table 1.
Sample and group demographics (N=1,200).
| Full sample | Non exposed | No PTSD | PTSD | Group differences | |
|---|---|---|---|---|---|
| Age–years: M (SD) | 37.4 (16.9) | 32.9a (16.09) | 39.0b (16.82) | 44.4c (16.81) | F=27.77*** |
| n | % | % | % | ||
| 34.2 | 56.7 | 9.1 | |||
| Gender | χ2=3.34 | ||||
| Female | 533 | 42a | 46a | 51.4a (10.5%) | |
| Male | 648 | 58a | 54a | 48.6a (8.3%) | |
| Education (years) | χ2=54.54*** | ||||
| 4 or less | 112 | 7a | 8.9a | 22.9b | |
| 5–9 | 256 | 28.9a | 19.8b | 9.2c | |
| 10–12 | 330 | 31.2a | 28a,b | 19.3b | |
| >12 | 470 | 32.9a | 43.3b | 48.6b | |
| Marital status | χ2=65.78*** | ||||
| Single | 549 | 61.1a | 40.4b | 33.0b | |
| Married/Tog. | 586 | 37.2a | 56.5b | 56.9b | |
| Div./widowed | 39 | 1.7a | 3.2a | 10.1b | |
| Employment | χ2=15.53** | ||||
| Active | 901 | 80.8a | 78.7a | 72.2a | |
| Student | 157 | 15a | 13.3a | 12a | |
| Pensioner, jobless | 85 | 4.1a | 8b | 15.7c | |
| Living region | χ2=31.14*** | ||||
| North | 490 | 43.7a | 42.8a | 40.2a | |
| Centre | 426 | 30.2a | 40.0a | 45.8a | |
| Interior | 77 | 9.3a | 5.1b | 7.5a,b | |
| South | 123 | 15.2a | 8.9b | 5.6b | |
| Islands | 28 | 1.6a | 3.2a | .9a | |
| Type of job | χ2=71.62*** | ||||
| Civilian | 814 | 54.6a | 74.6b | 89.9c | |
| Military | 361 | 45.4a | 25.4b | 10.1c | |
Note. Group demographics sharing the same letter in lines (a, b, c) do not differ significantly.
The Childhood Trauma Questionnaire–Short Form (CTQ-SF) (Bernstein et al., 2003) is a widely used retrospective and self-report questionnaire with 28 items. It assesses the frequency of five forms of CM occurring during childhood–like being hit (PA), verbally mistreated (EA), not having enough food (PN), being forced to assist or do something sexual (SA) and not having a supportive family (EN) (ranging from 1 to 5 respectively - never, rarely, sometimes, often, or, very often true). The CTQ-SF presented good psychometric properties with Cronbach's alpha varying between .61 for PN and .95 for SA in clinical populations (Bernstein et al., 2003), and between .58 for PN and .94 for SA (Scher, Stein, Asmundson, McCreary, & Forde, 2001) in community samples. Results for time stability and convergent and divergent validity were considered good (Bernstein et al., 2003). In the Portuguese population, the original CTQ-SF factorial structure was confirmed in a community sample of 746 subjects and Cronbach's alpha varied between .47 for PN and .79 for EN, with .84 for the overall scale (Dias et al., 2013). In the current sample, Cronbach's alfa were .45 for PN, .71 for SA, .74 for EA, .77 for PN, .79 for EN and .84 for the overall CTQ-SF. We used the Bernstein and Fink (1998) cut-off points to classify CM with clinical significance in each scale: EA ≥13; PA ≥10; SA ≥8; EN ≥15; PN ≥10. For the overall scale we used the cut-off point of one standard deviation above the average.
The Posttraumatic Diagnostic Scale is a 49-item scale to assess PTSD as defined by DSM-IV (PDS) (Foa, Cashman, Jaycox, & Perry, 1997). It comprises of four parts: exposure to TEs; symptoms of re-experiencing, avoidance and hyperarousal, and PTSD severity (17 items, classified in a four-point frequency scale (0 - Not at all or only one time; 1–Once a week or less/once in a while; 2 - 2 to 4 times a week/half the time; 4 - 5 or more times a week/almost always), and the impairment for various life-domains. Psychometric properties of the original version showed good internal consistency (alpha coefficient of .92), good test-retest reliability and a convergent validity of .82 (Foa et al., 1997). In a community sample of 404 Portuguese subjects, the original factor structure was confirmed. Internal consistency was found to be good, varying between .81 for hyperarousal and .92 for severity (Ribeiro et al., 2011). In the analyzed sample, PDS had an internal consistency of .83 for avoidance, .85 for hyperarousal, .89 for re-experiencing and .93 for PTSD severity.
The PTSD diagnosis was assessed applying the criteria of the DSM-IV: exposure to TEs accompanied by at least one symptom of re-experiencing, three or more of avoidance and two or more of increased arousal, with significant impact in daily activities.
ProcedureIn this ex post facto investigation, subjects were considered revictimized when they identified subsequent TEs as assessed by the PDS after being exposed to CM, as measured by the CTQ-SF. The research protocol included informed consent, questions about socio-demographics listed in Table 1 and the instruments mentioned above. Research was conducted under the Declaration of Helsinki. The data collection was approved by the Ethical Commission of the Military Hospital of Coimbra and by the Portuguese Commission for Data Protection (CNPD) in Portugal, and all participants signed an informed consent.
Data analysisData were analyzed using SPSS (version 21). Statistical analyses included ANOVA, Chi-square and the student's t tests to compare demographics and CM scores in groups with different traumatic exposure and PTSD status. Odds ratios and logistic regressions were applied to studying the risk for revictimization and PTSD associated to CM. Hierarchical regression was used to investigate the contribution of demographics, CM and TEs to predict PTSD severity. Missing data were treated using mean imputation. Additional details over the data analysis are mentioned in the results section.
ResultsGroup differencesBased on exposure to TEs and PTSD symptoms, the large sample (N=1,200) was divided into three groups: 1. non-exposed to TEs, 2. exposed with PTSD, and 3. exposed without PTSD. The groups compared were equivalent in terms of gender but not in terms of age, education, marital status, employment, region of residence and percentage of civilians and military. Group demographics are detailed in Table 1. Subjects exposed to TEs with PTSD had the highest scores for all CM forms (p ≤ .001), while those who were not exposed to TEs scored lower on CM except for SA. Scores for SA did not differ significantly between the non-exposed and exposed groups.
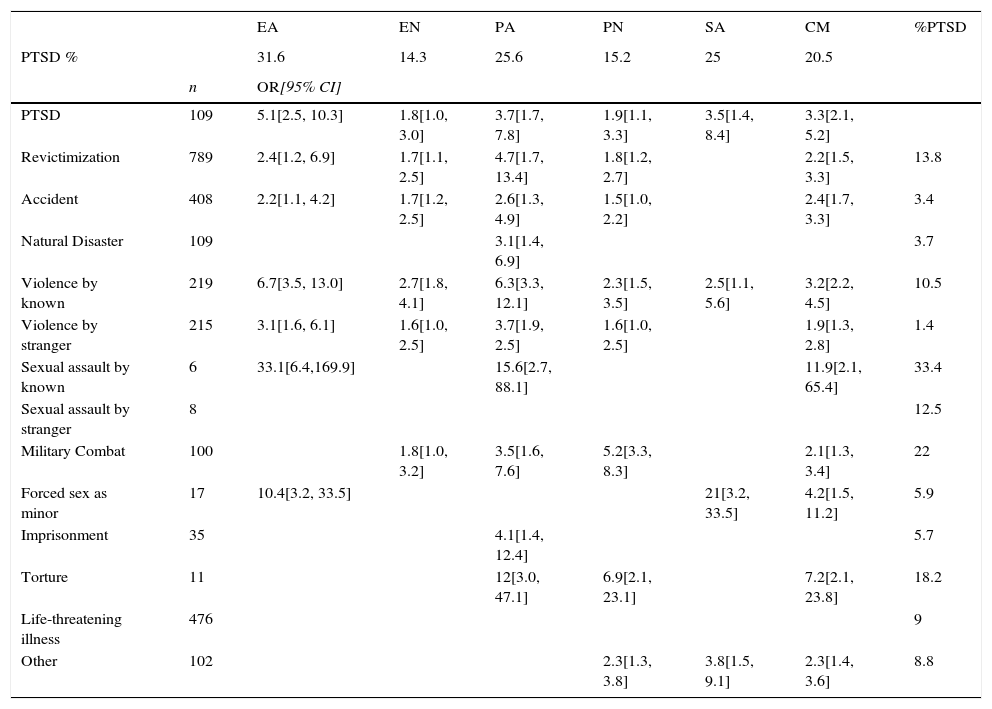
Traumatic exposure and PTSD diagnosisAbout 66% of subjects were exposed to any TE and 9.1% developed PTSD. Females had a PTSD prevalence of 10.5% and males 8.3%. The TEs most experienced were life-threatening illness and any type of accident. The highest percentage of PTSD diagnosis was found among subjects exposed to sexual assault by a known person, combat in war and torture, while the lowest was for violence by a stranger, accidents and natural disasters (Table 2).
Risk for revictimization and PTSD diagnosis associated with moderate or severe exposure to child maltreatment (N=1,200).
| EA | EN | PA | PN | SA | CM | %PTSD | ||
|---|---|---|---|---|---|---|---|---|
| PTSD % | 31.6 | 14.3 | 25.6 | 15.2 | 25 | 20.5 | ||
| n | OR[95% CI] | |||||||
| PTSD | 109 | 5.1[2.5, 10.3] | 1.8[1.0, 3.0] | 3.7[1.7, 7.8] | 1.9[1.1, 3.3] | 3.5[1.4, 8.4] | 3.3[2.1, 5.2] | |
| Revictimization | 789 | 2.4[1.2, 6.9] | 1.7[1.1, 2.5] | 4.7[1.7, 13.4] | 1.8[1.2, 2.7] | 2.2[1.5, 3.3] | 13.8 | |
| Accident | 408 | 2.2[1.1, 4.2] | 1.7[1.2, 2.5] | 2.6[1.3, 4.9] | 1.5[1.0, 2.2] | 2.4[1.7, 3.3] | 3.4 | |
| Natural Disaster | 109 | 3.1[1.4, 6.9] | 3.7 | |||||
| Violence by known | 219 | 6.7[3.5, 13.0] | 2.7[1.8, 4.1] | 6.3[3.3, 12.1] | 2.3[1.5, 3.5] | 2.5[1.1, 5.6] | 3.2[2.2, 4.5] | 10.5 |
| Violence by stranger | 215 | 3.1[1.6, 6.1] | 1.6[1.0, 2.5] | 3.7[1.9, 2.5] | 1.6[1.0, 2.5] | 1.9[1.3, 2.8] | 1.4 | |
| Sexual assault by known | 6 | 33.1[6.4,169.9] | 15.6[2.7, 88.1] | 11.9[2.1, 65.4] | 33.4 | |||
| Sexual assault by stranger | 8 | 12.5 | ||||||
| Military Combat | 100 | 1.8[1.0, 3.2] | 3.5[1.6, 7.6] | 5.2[3.3, 8.3] | 2.1[1.3, 3.4] | 22 | ||
| Forced sex as minor | 17 | 10.4[3.2, 33.5] | 21[3.2, 33.5] | 4.2[1.5, 11.2] | 5.9 | |||
| Imprisonment | 35 | 4.1[1.4, 12.4] | 5.7 | |||||
| Torture | 11 | 12[3.0, 47.1] | 6.9[2.1, 23.1] | 7.2[2.1, 23.8] | 18.2 | |||
| Life-threatening illness | 476 | 9 | ||||||
| Other | 102 | 2.3[1.3, 3.8] | 3.8[1.5, 9.1] | 2.3[1.4, 3.6] | 8.8 | |||
Note. Odds ratios are all significant for p ≤ .05. EA–emotional abuse, EN–emotional neglect, PA–physical abuse, PN–physical neglect, SA–Sexual abuse, CM–total score of child maltreatment, n–number of subjects exposed to TEs.
About 79.5% of subjects self-reporting moderate/severe CM were also exposed to subsequent TEs, with 51.7% referring to accidents. The odds for TEs in adulthood were about two times higher for persons exposed to moderate to severe CM compared to other non CM-exposed, as presented in Table 2. The probability of revictimization was larger for subjects exposed to moderate/severe EA and PA. Exposure to EA was found to increase the probability for subsequent sexual assault and interpersonal violence to the greatest extent. PA increased the odds of exposure to torture, violence by someone familiar and imprisonment. Exposure to EN and PN was associated with revictimization to a lesser extent than other forms of CM. Nevertheless, PN increased the probability of being exposed to combat and torture more than fivefold. In addition, EN raised the likelihood of exposure to violence by familiar and unknown subjects, and accidents.
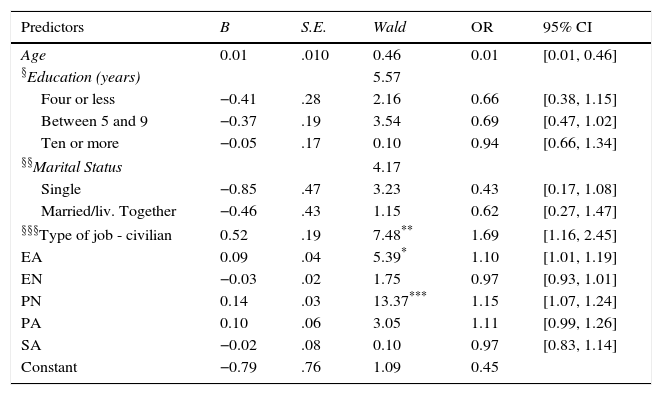
Logistic regression was applied to studying the risk of revictimization (exposure to TEs) associated with demographic variables (age, marital status, education and type of job) and CM forms. These variables were chosen because they were found to be significant predictors for TEs after applying simple logistic regressions. The model presented in Table 3 significantly distinguished between subjects who were exposed to TEs and those who were not (chi-square=110.96, with p ≤ .001). A Nagelkerke's R2 of .13 indicated a small effect of predictors on the grouping variable with a correct classification of 68.8% (34.3% for those not exposed and 86.7% for those exposed). Civilian job, EA and PN significantly predicted the risk for revictimization.
Revictimization predicted by demographics and child maltreatment (N=1,200).
| Predictors | B | S.E. | Wald | OR | 95% CI |
|---|---|---|---|---|---|
| Age | 0.01 | .010 | 0.46 | 0.01 | [0.01, 0.46] |
| §Education (years) | 5.57 | ||||
| Four or less | −0.41 | .28 | 2.16 | 0.66 | [0.38, 1.15] |
| Between 5 and 9 | −0.37 | .19 | 3.54 | 0.69 | [0.47, 1.02] |
| Ten or more | −0.05 | .17 | 0.10 | 0.94 | [0.66, 1.34] |
| §§Marital Status | 4.17 | ||||
| Single | −0.85 | .47 | 3.23 | 0.43 | [0.17, 1.08] |
| Married/liv. Together | −0.46 | .43 | 1.15 | 0.62 | [0.27, 1.47] |
| §§§Type of job - civilian | 0.52 | .19 | 7.48** | 1.69 | [1.16, 2.45] |
| EA | 0.09 | .04 | 5.39* | 1.10 | [1.01, 1.19] |
| EN | −0.03 | .02 | 1.75 | 0.97 | [0.93, 1.01] |
| PN | 0.14 | .03 | 13.37*** | 1.15 | [1.07, 1.24] |
| PA | 0.10 | .06 | 3.05 | 1.11 | [0.99, 1.26] |
| SA | −0.02 | .08 | 0.10 | 0.97 | [0.83, 1.14] |
| Constant | −0.79 | .76 | 1.09 | 0.45 | |
Note. Model confirmed by Hosmer and Lemeshow test χ2 =6.97, with p=.540, with Nagelkerke's R2=.13.
Reference category for §Education - higher education;§§Marital status–widowed/divorced;§§§Type of job–military.
We found that the probability of PTSD diagnosis increased more than three times in CM subjects (OR=3.3, 95% CI [2.1, 5.2]), as described in Table 2. Emotional abuse, PA and SA increased the probability of PTSD to the greatest extent. Emotional abuse was found in 31.6%, a larger percentage than that of subjects exposed to PA or SA.
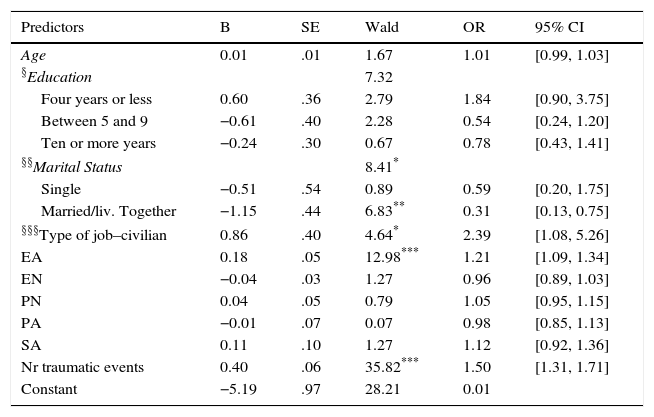
In addition, we studied the risk for PTSD using logistic regression and including demographic variables (age, education, marital status and type of job), forms of CM and the number of TEs. The analyzed model significantly predicted subjects with and without PTSD diagnosis (chi-square=133.70, p ≤ .001; Nagelkerke's R2=.24) and identified 90.9% of subjects correctly (99.2% without and 11% with diagnosis). From the included set of predictors, marital status, type of job, EA and the number of TEs were significant (Wald p<.05) (Table 4).
Logistic regression predicting PTSD diagnosis by demographics, child maltreatment and number of traumatic events (N=1,200).
| Predictors | B | SE | Wald | OR | 95% CI |
|---|---|---|---|---|---|
| Age | 0.01 | .01 | 1.67 | 1.01 | [0.99, 1.03] |
| §Education | 7.32 | ||||
| Four years or less | 0.60 | .36 | 2.79 | 1.84 | [0.90, 3.75] |
| Between 5 and 9 | −0.61 | .40 | 2.28 | 0.54 | [0.24, 1.20] |
| Ten or more years | −0.24 | .30 | 0.67 | 0.78 | [0.43, 1.41] |
| §§Marital Status | 8.41* | ||||
| Single | −0.51 | .54 | 0.89 | 0.59 | [0.20, 1.75] |
| Married/liv. Together | −1.15 | .44 | 6.83** | 0.31 | [0.13, 0.75] |
| §§§Type of job–civilian | 0.86 | .40 | 4.64* | 2.39 | [1.08, 5.26] |
| EA | 0.18 | .05 | 12.98*** | 1.21 | [1.09, 1.34] |
| EN | −0.04 | .03 | 1.27 | 0.96 | [0.89, 1.03] |
| PN | 0.04 | .05 | 0.79 | 1.05 | [0.95, 1.15] |
| PA | −0.01 | .07 | 0.07 | 0.98 | [0.85, 1.13] |
| SA | 0.11 | .10 | 1.27 | 1.12 | [0.92, 1.36] |
| Nr traumatic events | 0.40 | .06 | 35.82*** | 1.50 | [1.31, 1.71] |
| Constant | −5.19 | .97 | 28.21 | 0.01 | |
Note. Model confirmed by Hosmer and Lemeshow test χ28.34, with p=.401, Nagelkerke's R2=.24.
Reference category for §Education-higher education;§§Marital status–widowed/divorced;§§§Type of job–military.
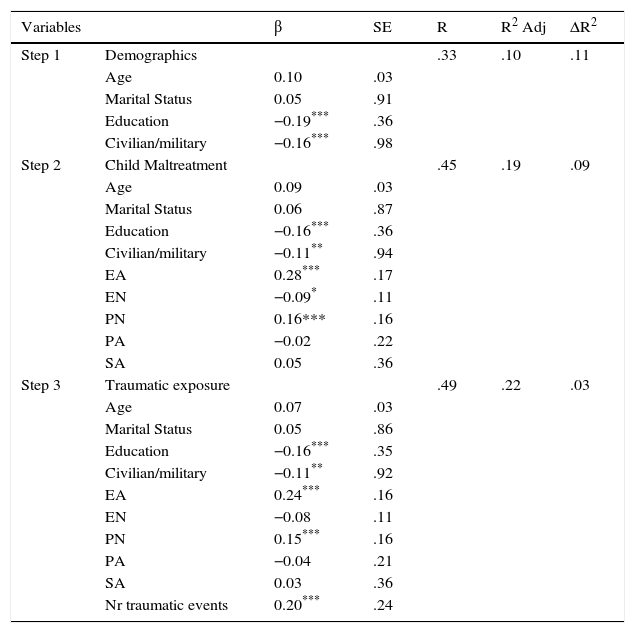
A three-stage hierarchical multiple regression predicting PTSD severity was applied to studying the contribution of demographics (age, education, marital status and type of job), forms of CM and the number of TEs. A significant contribution was found for all the stages, as confirmed by Fisher's significance test (p ≤ .001). At stage one, demographics accounted for 10.2% of the variation in PTSD severity. Introducing forms of CM at stage two explained an additional 9.5%, and the number of TEs added 3% of explained variance at stage three. At the third step, education, type of job, EA, PN and the number of TEs were significant predictors. Emotional abuse had the largest standardized regression weight (β=.24). Together, the variables explained 22.4% of the variance in PTSD severity (F (10,752)=23.17, p ≤ .001). Table 5.
Results of hierarchical regression predicting PTSD severity by demographics, child maltreatment and traumatic exposure (N=753).
| Variables | β | SE | R | R2 Adj | ΔR2 | |
|---|---|---|---|---|---|---|
| Step 1 | Demographics | .33 | .10 | .11 | ||
| Age | 0.10 | .03 | ||||
| Marital Status | 0.05 | .91 | ||||
| Education | −0.19*** | .36 | ||||
| Civilian/military | −0.16*** | .98 | ||||
| Step 2 | Child Maltreatment | .45 | .19 | .09 | ||
| Age | 0.09 | .03 | ||||
| Marital Status | 0.06 | .87 | ||||
| Education | −0.16*** | .36 | ||||
| Civilian/military | −0.11** | .94 | ||||
| EA | 0.28*** | .17 | ||||
| EN | −0.09* | .11 | ||||
| PN | 0.16*** | .16 | ||||
| PA | −0.02 | .22 | ||||
| SA | 0.05 | .36 | ||||
| Step 3 | Traumatic exposure | .49 | .22 | .03 | ||
| Age | 0.07 | .03 | ||||
| Marital Status | 0.05 | .86 | ||||
| Education | −0.16*** | .35 | ||||
| Civilian/military | −0.11** | .92 | ||||
| EA | 0.24*** | .16 | ||||
| EN | −0.08 | .11 | ||||
| PN | 0.15*** | .16 | ||||
| PA | −0.04 | .21 | ||||
| SA | 0.03 | .36 | ||||
| Nr traumatic events | 0.20*** | .24 | ||||
Note. SE: Standard error.
Our study adds evidence about the long-term consequences of CM in adults in the community. Self-reported CM was associated with a two-fold risk for exposure to new traumatic events and three-fold for PTSD diagnosis. More than 30% of adults with PTSD reported moderate or severe EA during childhood. Moreover, EA remained significantly associated with revictimization and PTSD after adjusting for demographics. While previous studies underlined the consequences of PA and SA, our findings strengthen the assumption that EA can be even more harmful than other forms of CM. Although it figures among the most frequent CM forms (Stoltenborgh et al., 2015) it is rarely a motive for specific measures for child protection.
Clinicians and researchers need to be aware of the injurious potential of other less evident risk factors that can contribute to traumatic exposure and PTSD across the lifespan. The identification of pre-trauma risk factors for PTSD is valuable in the sense that it can help to tailor intervention protocols targeting more efficiently PTSD and related comorbidities (Britvić et al., 2015; DiGangi et al., 2013). Health professionals need to look “outside the box” and pay more attention to the identification of etiologic and maintenance factors for PTSD and its associated features (Keeley et al., 2016; Timimi, 2014).
In our sample, a 9.1% risk for PTSD was found. This was slightly larger than De Albuquerque et al. (2003) found in the Portuguese population (7.8%). A life-threatening disease, accidents or having someone close suffering them were mentioned as most frequent TEs. However, subjects exposed to sexual assault, war exposure and torture had the highest percentages of risk for PTSD. These findings clearly indicate that war is a relevant traumatic event for the Portuguese society. Nevertheless, civilians were at higher risk for revictimization and PTSD than military personnel. This is remarkable as military duties involve exposure to potential TEs and as the Portuguese military was exposed to many hardships in the Colonial Wars. A possible explanation is that military training exerts a protective effect in terms of the perception of threatening events, providing subjects with higher thresholds for experiencing events as traumatic. This finding deserves further investigation as it can elucidate about potential resilience mechanisms for PTSD.
Exposure to accidents, the second most frequent TE, was found to be significantly associated with all CM forms except SA. This result is particularly relevant because of the high incidence of car accidents in Portugal. It is likely that CM persons may have impaired skills for risk perception (Chu et al., 2016) and for emotional regulation (Messman-Moore et al., 2010) and consequently, a greater vulnerability for exposure to accidents. Another potential explanation refers to the lack of sleep in CM persons suffering from PTSD and related comorbidities (Britvić et al., 2015; Kendall-Tackett, 2002). When these hypotheses are confirmed, specific actions are needed to assess and improve the quality of sleep, the risk perception and emotion regulation in vehicle motorists exposed to CM.
Remarkably, PA and SA did not predict PTSD severity in our sample, as previously found (Breslau et al., 2014). This finding confirms that consequences for CM forms may vary depending for instance, on the cultural background of analyzed samples.
To our knowledge, this is the first study on the relations between CM, traumatic exposure and PTSD among Portuguese adults. We confirmed that CM increases the risk for traumatic exposure and PTSD in adults in the community, and that EA is an important predictor, although previous studies underlined more often the injurious potential for PA and SA. Because we analyzed diverse forms of traumatic exposure in adults, we learned that common life events such as accidents can be linked to CM. As we used a community sample, our findings are less biased than those focused on subjects with substantiated CM or clinical groups. However, uncertainty about the representativeness of the Portuguese sample imply caution in generalizing our findings.
We used robust self-report instruments validated in Portuguese samples, although the PN subscale of the CTQ-SF was found to have low internal consistency. It is well known that recall bias can reduce the reliability and effectiveness of retrospective assessments (Bernstein et al., 2003). Although the use of anonymous self-report questionnaires may facilitate the disclosure of CM experiences, one should be careful with statements about causality. The PTSD diagnosis has been defined according to DSM-IV, and not to DSM-5, but current PTSD prevalence was found not to differ significantly when both editions were compared (O’Donnell et al., 2014).
Our findings reinforce that prevention of CM, particularly EA, must be improved. Agencies for child protection and health care need to join efforts to stop EA and to broaden interventions to prevent CM-associated risk for revictimization and PTSD across the lifespan. The routine screening for diverse CM forms among clients suffering from PTSD and related comorbidities can contribute to the improvement of therapeutic interventions. The prospective investigation about how emotional processing, sleep and risk detection occurs in maltreated versus non-maltreated adults can shed light about pathways linking CM, revictimization and PTSD, and better inform preventive and intervention programs.
This work was funded by the Fundação para a Ciência e Tecnologia, Portugal (SFRH/BD/68995/2010). We would like to thank the Faculty of Social Sciences of Utrecht University for its hosting conditions; Margarida Calafate Ribeiro for the consent to use the data; Dave Hessen for the statistical support; Fernando Estevez-Lopez for the editing of the Spanish abstract.