Background/Objective: Social skills training (SST) is frequently included in the treatment of social anxiety disorder (SAD) in both children and adolescents, although there is no empirical evidence to support it. Consequently, our objective is to study the role and effects of SST in the treatment of a sample of adolescents with SAD. Method: A total of 108 adolescents diagnosed with generalized social phobia were randomly assigned to two treatment conditions (with and without SST) and a control group waiting list (WLCG). The evaluation included self-report measures, observational tests and blind evaluators. Results: Both interventions significantly reduced the number of social situations feared/avoided with respect to the WLCG, which worsened. Likewise, both interventions were effective but the group with SST obtained better results in the post-test and follow-ups, as well as a lower dropout rate (6:1). Conclusions: The use of SST reduces the dropout rate of treated adolescents and increases the effectiveness of the Intervention Program for Adolescents with Social Phobia.
Antecedentes/Objetivo: El entrenamiento en habilidades sociales (EHS) se incluye frecuentemente en el tratamiento del trastorno por ansiedad social (TAS) tanto en niños como en adolescentes, pese a que no existe evidencia empírica que lo respalde. En consecuencia, nuestro objetivo es estudiar el papel y los efectos que produce el EHS en el tratamiento de una muestra de adolescentes con TAS. Método: Un total de 108 adolescentes diagnosticados con fobia social generalizada fueron asignados aleatoriamente a dos condiciones de tratamiento (con y sin EHS) y a un grupo control lista de espera (GCLE). La evaluación incluyó medidas de autoinforme, tests observacionales y evaluadores ciegos. Resultados: Ambas intervenciones redujeron significativamente el número de situaciones sociales temidas/evitadas respecto del GCLE, que empeoró. Asimismo, ambas fueron eficaces pero el grupo con EHS obtuvo mejores resultados en el post-test y en los seguimientos, así como una tasa menor de abandonos (6:1). Conclusiones: El uso del EHS reduce la tasa de abandono de los adolescentes tratados e incrementa la eficacia del Programa de Intervención en Adolescentes con Fobia Social.
Social phobia (SP) or social anxiety disorder (SAD) has a prevalence of approximately 7% among children and adolescents in the United States (American Psychiatric Association (APA), 2013) and between 8 and 12.06% in Spanish adolescents (Olivares, Olivares-Olivares, & Macià, 2014). Empirical evidence shows that cognitive behavioral therapy (CBT) has been shown to be efficacious for SAD and is considered the first-choice psychological intervention for the disorder (American Psychological Association (APA), 2016). However, despite the good results, there is general agreement on the need to improve the range of effectiveness and efficiency of these treatments (Bornas, de la Torre-Luque, Fiol-Veny, & Balle, 2017; McAleavey, Castonguay, & Golfried, 2014; Nunes, Ayala-Nunes, Pechorro, & La Greca, 2018; Wersebe, Lieb, Meyer, Hofer, & Gloster, 2018; Wersebe, Lieb, Meyer, Miche et al., 2018).
From our point of view, increasing the effectiveness and efficiency of SAD treatment could be achieved by (1) the study of the role and relative contribution of each of its components and their interactions (see Ale, McCarthy, Rothschild, & Whiteside, 2015); (2) the implementation of alternative strategies to the conventional clinical format that would resolve low treatment motivation would resolve low treatment motivation and practical barriers to attending sessions (Olivares-Olivares, Olivares, Macià, Macià, & Montesinos, 2016); and (3) a greater understanding of the variables that facilitate or hinder adherence to treatment (Hawley, Rector, & Laposa, 2016).
In children and adolescents, the most used components in the treatment of SAD are psychoeducational, social skills training (SST), exposure, and “homework” (Cederlund, 2013). Of these, only the relevance of exposure seems certain, both in the adult population and child-juvenile population (Ale et al., 2015). We know very little about the need for and the opportunity to include SST in SAD group treatment (see Barkowski et al., 2016) because its role is still unclear in the adult population (Beidel et al., 2014) or in the juvenile (Olivares et al., 2014). However, as we have indicated, it is frequently included in the treatment of SAD in the child-juvenile population probably because it is assumed to be basic for social adaptation (Essau et al., 2014; Redondo-Pacheco, Parra-Moreno, & Luzardo-Briceño, 2015), without conclusive empirical evidence supporting it, either generally or as to who might benefit (Barkowski et al., 2016). However, we can affirm that the presence of SST and exposure generally produces good results in the reduction/elimination of SAD in adults (Beidel et al., 2014) and in children and adolescents (National Institute for Health and Care Excellence (NICE), 2013).
Therefore, it is necessary to continue providing empirical evidence to help clarify the opportunity and the need to include SST as part of a clinician-rated gold-standard protocol for the or the adolescent population with SAD. Therefore, our objectives are (a) to provide evidence to quantify the effect size attributable to the presence/absence of SST in the treatment of SAD and (b) to analyze SST's role when the treatment is applied with and without this component.
MethodParticipantsWe administered the Social Phobia and Anxiety Inventory (SPAI; Turner, Beidel, Dancu, & Stanley, 1989) to 2,505 students in the third and fourth year of Compulsory Secondary Education (Enseñanza Secundaria Obligatoria, ESO) and first year of High School (Bachillerato) in seven randomly selected public and state-subsidized high schools from the Spanish region of Murcia.
In the second stage of the study, we selected participants based on a previously determined cut-off point cutoff-point (SPAI-SP ≥97; Olivares, García-López, Turner, La Greca, & Beidel, 2002). Participants in this subset were assessed with the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV-C; Silverman & Albano, 1996): 132 met the criteria for the diagnosis of generalized social phobia (GSP). They and their parents were informed of the assessment results. Inclusion criterion: meet the requirements for GSP diagnosis (American Psychiatric Association (APA), 2000); 108 met the criteria (M=15.4 years; SD=1.11; range: 14–17; 63% were female). Exclusion criteria: not presenting written consent signed by at least one parent or equivalent, meeting the diagnostic criteria for severe psychopathology (e.g., depression or narcissistic disorder), long history of substance abuse, aggressive behavior, missing three consecutive treatment sessions, and not having previously received psychological or psychiatric treatment.
MeasuresEvaluation of participants’ expectations (outcome expectancy, OE). At pretest, we used an ad hoc one-item scale (range: 0–5) in which participants indicated the extent to which they hoped to improve from treatment (0=Not at all; 5=A lot). All participants completed the following measures at pretest, post-test, and follow-up.
The Social Phobia and Anxiety Inventory (SPAI; Turner et al., 1989). In this application, the SPAI-SP subscale showed an internal consistency of .89 (Cronbach's alpha).
Anxiety Disorders Interview Schedule for DSM-IV. Child Version (ADIS-IV-C; Silverman & Albano, 1996). In this application with a Spanish adolescent population, the value of k oscillated between .83 and .91.
The number of social situations feared and/or avoided (NSSFA) was quantified based on the information initially provided by participants in the SP section of ADIS-IV-C; these data were used to calculate the clinical significance of the treatment effect.
Personal Report of Confidence as a Speaker (PRCS; Gilkinson, 1942). In this application, the value of α was .89.
Rosenberg Self-Esteem Scale (RSE; Rosenberg, 1965). In our investigation, its internal consistency was .90 (Cronbach's α).
The Rathus Assertiveness Schedule (RAS; Rathus, 1973). In this application, Cronbach's alpha internal consistency was .78.
Duration of eye contact (DEC) with the examiner is quantified through its registration in an observation test and was also performed at pretest, post-test, and follow-up. It included three interviews with each participant, who had to initiate and maintain a conversation with a stranger for 3min. The topics were participants’ expectations about the psychological treatment (pretest), their personal assessment of the treatment received and suggestions for improvement (post-test), a description/assessment of the difficulties they had faced and how they had solved them (follow-up). This test was led by two examiners of different genders, with more than two years of experience in the treatment of individuals with SAD. Each interacted with participants of the opposite sex and were trained not to initiate or carry the weight of the conversation with the participants not to initiate the conversation but they should confront/solve the difficulties might arise.
After obtaining the written consent of participants and their parents, each participant's performance was filmed with a video camera to record the total DEC with the examiner. The recordings were viewed and coded by two independent observers previously trained for the purpose. Interobserver correlations were high: k=.91.
Adherence to treatment (ATT). This variable was quantified as a function of the “homework” performed and the “number of training sessions” attended.
ProcedureThis research was granted permission by the Ethical Research Committee of the University of Murcia. Fourteen trained examiners performed the assessment. They were grouped in opposite-sex pairs of individuals who are graduates in psychology and were trained to independently carry out their tasks. Two participated in the pretreatment evaluation, two in the screening (pretest), six in the clinical interview, two performed the post-treatment evaluation, and two others the follow-up. All were blinded to treatment, and the reliability coefficient for GSP diagnosis was good (k=.86).
The selected adolescents and their parents were sent a letter that presented the objectives, structure, content, and other issues related to the intervention. They were also advised that they could clarify any doubts by requesting a private meeting or by telephone conversation with an expert on the toll-free number provided to them.
The 108 participants with GSP were randomly assigned to one of three experimental conditions: Waiting-list control group (WLCG 64% girls) or one of two treatment groups the intervention in adolescents with social phobia (IAFS 62% girls) and IAFS without the SST (IAFS-R 65% girls), with 36 participants in each group.
We chose a two-factor partially repeated measures experimental design. The repeated measures factor contained data recorded at different times, and the between-subject factor was the IAFS, which was divided into two categories (IAFS and IAFS-R). For ethical reasons, after the post-test, participants in the WLCG and the dropouts were offered the possibility of joining a non-experimental treatment group.
The treatment was applied by two psychology graduates, of different genders and with more than ten years of experience treating groups of adolescents with GSP; the roles of therapist and co-therapist were randomly assigned. Treatment integrity was controlled using two identical manuals (see Olivares, 2005), except in the section on SST (IAFS and IAFS-R). Therapists’ knowledge of the program was controlled by two interviews conducted independently by two observer interviewers, who followed a structured interview previously prepared by two psychologists with broad experience in applying the IAFS Program. The items covered the most relevant aspects of the programs’ content, structure, and development. The IAFS consists of 12 weekly 90-min group treatment sessions. The program's basic components are as follows:
Educational component. Information about the contents of the treatment is provided, presenting an explanatory model of SP, planning the desired achievements—target behaviors—and reviewing the individual's expectations for the treatment.
SST. This includes contents/activities such as starting and maintaining conversations, assertiveness, paying and accepting compliments, making and keeping friends, and training in public speaking.
Exposure. This is the core of the program, and most activities revolve around it. Both in vivo—simulated and real—and imaginary types of exposure are used.
Cognitive restructuring techniques. This component is aimed at teaching the participants to identify the negative automatic thoughts they generate when they evoke past situations, anticipate social situations, or are immersed in a social situation that triggers anxiety responses.
At the end of the group sessions, homework assignments are given. The sessions are devoted to monitoring the difficulties encountered in the homework assignments and dealing with issues related to the content and activities of the group sessions. The IAFS-R is a written version of the IAFS manual, built ad hoc, in which all its content is structured identical to full version (IAFS) except in the section dedicated to the SST. To control for reactivity by frustration, the groups were treated in different places, to prevent them from being aware of the existence of the other; both places were two classrooms in public teaching centers with identical layout and furniture, furthermore the treatment was applied in the same time slot.
Participants had two hours a week, on two separate, predetermined days, for individual telephone consultations during which they could request information about the homework and resolve doubts about the contents given during the treatment sessions.
Statistical analysisStatistical analyses were performed with the SPSS 19.0 program. The magnitude of the effect size (ES) was interpreted following Cohen (1988). Positive values of d indicate better results from the group that comes first in the comparison. As the experimental mortality exceeded 10% in one of the groups, the loss of participants was controlled by imputation of lost data; the outcome data of these dropouts were included in intent-to-treat analyses using multiple imputation. Thus, data analysis was based on all patients who were assigned to one of the three study arms. The clinical significance of the results was calculated from the reduction/elimination and increase of the NSSFA. To control inflation of the type I error rate, the Bonferroni correction procedure was applied so that, to maintain the nominal significance level at 5%, the critical probability level associated with the contrast statistic result had to be equal to or less than 0.017 (αB=α/3=0.05/3=0.017).
ResultsEquivalence of experimental conditions in the pretestThe study of the equivalence of the groups in the pretest did not show statistically significant differences in the variables: age, sex distribution, family history of SP, alcohol consumption, or cannabis-related disorders. Similarly, no statistically significant differences were found with the dependent variables, contemplating and without contemplating the abandonments, except in the variables RSE (p=.016) and RAS (p=.021), whose averages in the IAFS were higher than in the IAFS-R. There were also no significant differences between the treatment groups for OE, in the pretest, and only when the data of those who completed the treatment were analyzed.
Equivalence between dropouts and completersThe percentage of dropouts in the IAFS-R was 33.3% (12 participants), 5.6% (2 participants) in the IAFS group, and 0% in the WLCG. The differences were statistically significant between the three groups [RV (2)=20.03, p<.0001] and between IAFS and IAFS-R [2 (1)=8.86, p=.003].
To study their equivalence, both groups (14 vs. 58) were compared. There were no significant differences in age [t (70)=−0.92, p=.358] or in sex [2 (1)=1.91, p=.166], although the number of women was greater (78.6% vs. 58.6%). There were no significant differences in family history of SP (RV (1)=0.70, p=.402), alcohol consumption (RV (1)=0.07, p=.781) and cannabis consumption=0.04, p=.840). In the last three analyses, we applied the likelihood ratio test because the conditions required for the chi-square test had not been met.
There were also no significant differences in the dependent variables and in comorbidity, except in OE in favor of the completers and in the panic attacks that were more frequent in the dropouts (64.3% vs. 25.9%). Those who dropped out reported higher NSSFA and scored more in SPAI-SP, RAS. This trend was also found in dysthymic disorder (85.7% vs. 74.1%).
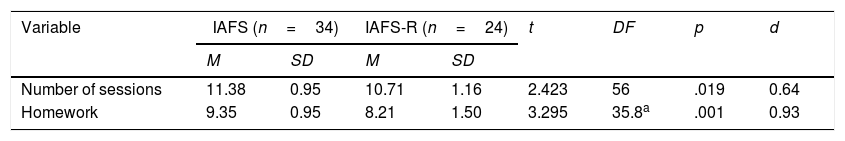
Adherence to the treatment by completersThe IAFS obtained magnitudes higher than the IAFS-R with statistically significant differences in the two measured variables (see Table 1). The effect size (ES) was medium and high.
Adherence to the treatment of the completers.
| Variable | IAFS (n=34) | IAFS-R (n=24) | t | DF | p | d | ||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| Number of sessions | 11.38 | 0.95 | 10.71 | 1.16 | 2.423 | 56 | .019 | 0.64 |
| Homework | 9.35 | 0.95 | 8.21 | 1.50 | 3.295 | 35.8a | .001 | 0.93 |
n, group size; M, mean SD, standard deviations; t, Student's comparison test; DF, degrees of freedom; p, probability level associated with the t test; d, the effect size index.
Treatment groups showed improvements from pretest to post-test in all variables analyzed; in WLCG only the variable RAS showed an improvement. To examine in which groups the differences occurred, post hoc comparisons were made (Table 2).
Results of pre–post change and follow-up.
| Pretest–post-test | Variable | IAFS1 | IAFS-R1 | WLCG1 | Resultsa | |||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||
| NSSFA | 5.64 | 1.81 | 3.05 | 2.89 | −0.58 | 0.84 | F(2, 66)=85.71, p<.001 | |
| DEC | 9.39 | 2.91 | 5.00 | 4.52 | −0.33 | 0.63 | F(2, 61)=87.45, p<.001 | |
| SPAI-SP | 41.28 | 20.21 | 25.50 | 24.83 | −4.78 | 9.23 | F(2, 78)=53.28, p<.001 | |
| PRCS | 20.97 | 15.13 | 15.75 | 19.99 | −3.53 | 4.29 | F(2, 69)=27.81, p<.001 | |
| RAS | 32.42 | 17.55 | 19.78 | 21.89 | 2.25 | 15.96 | F(2, 98)=23.79, p<.001 | |
| RSE | 3.44 | 3.19 | 3.89 | 4.39 | −0.36 | F(2, 74)=18.50, p<.001 | ||
| Post hoc | Variableb | IAFS1 vs. IAFS-R1 | IAFS vs. WLCG1 | IAFS-R vs. WLCG1 | |||
|---|---|---|---|---|---|---|---|
| Pretest–post-test | p | d | p | d | p | d | |
| NSSFA | <.0001 | 1.06 | <.0001 | 4.37 | <.0001 | 1.69 | |
| DEC | <.0001 | 1.14 | <.0001 | 4.56 | <.0001 | 1.64 | |
| SPAI-SP | .012 | 0.69 | <.0001 | 2.90 | <.0001 | 1.60 | |
| PRCS | .428 | 0.29 | <.0001 | 2.18 | <.0001 | 1.32 | |
| RAS | .023 | 0.63 | <.0001 | 1.78 | .0001 | 0.90 | |
| RSE | .876 | −0.11 | <.0001 | 1.50 | <.0001 | 1.28 | |
| Variable | IAFS1 | IAFS-R1 | ct | d | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Pretest–follow-up 1 | NSSFA | 6.53 | 2.22 | 3.72 | 3.22 | t(62.2)=4.30, p<.001 | 1.00 |
| DEC | 9.83 | 3.32 | 5.72 | 5.12 | t(60)=4.03, p<.001 | 0.94 | |
| SPAI-SP | 58.80 | 23.11 | 36.86 | 34.31 | t(61.3)=3.18, p=.002 | 0.74 | |
| PRCS | 38.00 | 18.78 | 28.36 | 27.02 | t(62.4)=1.75, p=.084 | 0.41 | |
| RAS | 46.83 | 20.50 | 30.39 | 30.09 | t(61.7)=2.71, p=.009 | 0.63 | |
| RSE | 6.61 | 3.95 | 5.80 | 6.16 | t(59.6)=0.66, p=.512 | 0.15 | |
| Pretest–follow-up 2 | NSSFA | 6.75 | 2.61 | 3.86 | 3.36 | t(66)=4.07, p<.001 | 0.95 |
| DEC | 10.08 | 3.31 | 6.28 | 5.34 | t(58.5)=3.63, p=.001 | 0.85 | |
| SPAI-SP | 75.92 | 31.52 | 44.64 | 40.76 | t(65.8)=3.64, p=.001 | 0.85 | |
| PRCS | 54.05 | 22.64 | 36.39 | 34.49 | t(60.4)=2.56, p=.013 | 0.60 | |
| RAS | 57.39 | 22.61 | 31.72 | 30.16 | t(64.9)=4.08, p<.001 | 0.95 | |
| RSE | 9.36 | 6.49 | 6.89 | 7.63 | t(68.3)=1.14, p=.143 | 0.35 |
n=36; M, mean; SD, standard deviations; NSSFA, number of social situations feared and/or avoided; DEC, duration of eye contact with the examiner; SPAI-SP, The SPAI-Social phobia subscale; PRCS, Personal Report of Confidence as a Speaker; RAS, The Rathus Assertiveness Schedule; RSE, Rosenberg Self-Esteem Scale.
The Brown–Forsythe F test was applied because the assumption of homogeneity of variances was not satisfied in any case.
The groups receiving treatment showed highly significant changes in their favor, with large ES. The WLCG did not show any. The IAFS vs. IAFS-R was favorable to the first one of five variables, but not in PRCS, despite the fact that ES was favorable and significant, Cohens's d=0.20, and not in PRCS because ES was superior in IAFS-R. The study of pretest follow-up changes at 6 months (Table 2) also shows significant differences in favor of IAFS in five of the seven variables, with ES being relevant and favorable to it. Analysis of the pretest follow-up changes at 12 months shows that both groups presented improvements, but the changes in IAFS were superior and with significant differences in their favor, except in PRCS. All ESs were above 0.50 except in PRCS (Table 2).
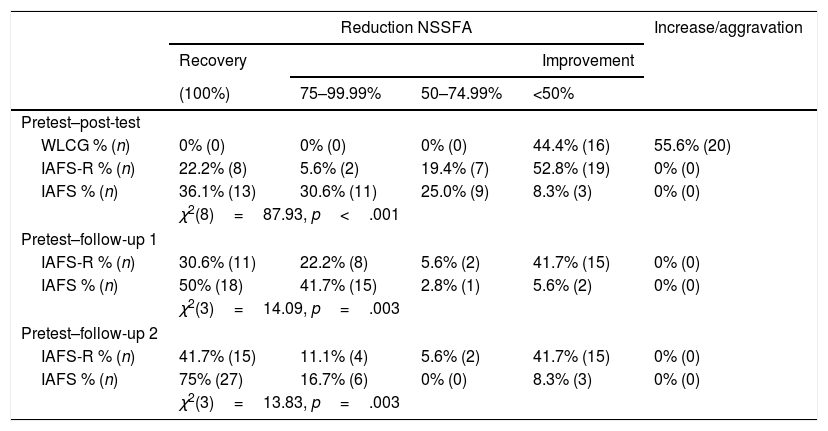
Analysis of the clinical significance of the changesWe assessed participants based on the reduction/elimination of the number of feared and/or avoided social situations they reported at pretest (ADIS-IV-C) using three criteria: (a) recovery (100% remission—the criteria required by the DSM-IV for the diagnosis of GSP are no longer met); (b) improvement/remission between 99.99% and 0% of NSSFA; and (c) increase/aggravation in NSSFA. To verify possible differences, we applied the chi-square test to each contingency table. Assessment of the equivalence of the groups at pretest did not show statistically significant differences between experimental conditions.
In the study of clinical significance of changes (Table 3) in the pretest–post-test, statistically significant differences were observed between the three experimental conditions. Analysis showed that these were significant in: (a) IAFS vs. IAFS-R [2 (3)=19.31, p<.001) because the percentage of participants with a reduction of less than 50% of NSSFA in IAFS-R was 52.8% compared to 8.3% in IAFS; (b) IAFS vs. WLCG [2 (4)=61.89, p<001] and IAFS-R vs. WLCG [2 (4)=37.26, p<.001] because in both cases the reduction of NSSFA was greater in the treatment groups.
Clinical significance of treatment effects.
| Reduction NSSFA | Increase/aggravation | ||||
|---|---|---|---|---|---|
| Recovery | Improvement | ||||
| (100%) | 75–99.99% | 50–74.99% | <50% | ||
| Pretest–post-test | |||||
| WLCG % (n) | 0% (0) | 0% (0) | 0% (0) | 44.4% (16) | 55.6% (20) |
| IAFS-R % (n) | 22.2% (8) | 5.6% (2) | 19.4% (7) | 52.8% (19) | 0% (0) |
| IAFS % (n) | 36.1% (13) | 30.6% (11) | 25.0% (9) | 8.3% (3) | 0% (0) |
| χ2(8)=87.93, p<.001 | |||||
| Pretest–follow-up 1 | |||||
| IAFS-R % (n) | 30.6% (11) | 22.2% (8) | 5.6% (2) | 41.7% (15) | 0% (0) |
| IAFS % (n) | 50% (18) | 41.7% (15) | 2.8% (1) | 5.6% (2) | 0% (0) |
| χ2(3)=14.09, p=.003 | |||||
| Pretest–follow-up 2 | |||||
| IAFS-R % (n) | 41.7% (15) | 11.1% (4) | 5.6% (2) | 41.7% (15) | 0% (0) |
| IAFS % (n) | 75% (27) | 16.7% (6) | 0% (0) | 8.3% (3) | 0% (0) |
| χ2(3)=13.83, p=.003 | |||||
Note. %, percentage of participants meeting criteria; n, number of participants meeting the criterion.
In the pretest-follow-up comparison at 6 months, significant differences were found between IAFS and IAFS-R, with the first presenting a higher percentage of recoveries and improvements (between 75% and 99.99%). In the study at 12 months, the differences between IAFS and IAFS-R were also significant because the first one presented recoveries greater than the second, with superiority in improvements between 75% and 99.99%, but not lower than 75%.
DiscussionRegarding our first objective, the pretest–post-test changes (Table 2) show that all ES were relevant (d =0.20) and favorable to IAFS, except in RSE in the pretest–post-test time, in which IAFS-R momentarily reached better results than IAFS. In all follow-ups this trend is reversed and the IAFS group improves much more than the IAFS-R group. This data can be interpreted as a momentary effect of the over-effort to be performed by completers the IAFS-R, because in the pretest groups were not equivalent in this variable (showing the IAFS better scores than the IAFS-R). At the 12-month follow-up (Table 2), the IAFS superiority is confirmed once again because all ES are relevant and favorable to it. The results of clinical significance (Table 3) also show that the differences between IAFS and IAFS-R were significant and favorable to the former because their recovery and improvement rates (between 75% and 99.99%) were clearly higher.
On the other hand, the achievements of the completers of both groups increased in the follow-up, as is generally the case in CBT (Swan & Kendall, 2016). These achievements were most strongly in the IAFS treatment group. The most reasonable explanation is that participants continued to apply and improve their learning upon completion of treatment.
Our second objective was to analyze SST's role. In general, the results reveal SST's protective role against dropouts, most likely because it (a) facilitates the gradual exposure to feared/avoided (previously planned) social situations, through group training in a “safe” context “supervised”/controlled by professionals; (b) increases by its practice the dexterity of the execution of social skills (SS), restoring the effect of the disuse generated by the avoidance responses; (c) allows learning new SS (if any); (d) enhances the disinhibition of the execution of SS acquired through the modeling of peer coping and mastery of therapists; (e) it allows positive reinforcement by therapists and companions for achievements (attention and social approval); and (f) favors the increase in ATT.
These potential benefits would allow IAFS participants to significantly increase their odds of facing the relationship/performance with others, with lower personal costs and greater probability of success than those of IAFS-R, both during OSH development and in their homework. These advances in the reduction/elimination of anxiety responses would gradually become generalized to other SS and untrained situations, increasing the statistical and clinical improvements observed in the follow-up measures in line with Beidel et al. (2014) reported in an adult population.
The dramatic effect of the absence of the “protective” role of SST is especially evident in the IAFS-R: six times more dropouts occurred here than in IAFS, despite their initial equivalence (except in RSE). A more detailed analysis of our data shows that, despite starting from positions equivalent to completers in the pretest, except for OE, the dropouts presented a vulnerability profile characterized by lower OE, plus panic attacks, plus avoidant personality disorder (AvPD), more social anxiety (SPAI-SP), higher NSSFA, and less assertiveness (RAS), which are variables usually associated with a higher probability of worse outcomes for childhood anxiety disorders (see Compton et al., 2014). The intersection of this profile with the absence of SST seems to have a large effect on the number of dropouts (especially among women—78.6% vs. 58.6%).
In addition, although there is a general consensus that exposure is the active ingredient supported by the link between more exposure practice and better outcomes for CADs (Ale et al., 2015). In the specific case of SAD, it seems necessary to evaluate previously (a) the dropouts occur mainly in the treatment without SST (IAFS-R), (b) the number exceeds the 15–20% range that the previous studies reported (Taylor, Abramowitz, & McKay, 2012), and (c) all dropouts occur in the first five sessions. Therefore, we understand that these results suggest that the gradual application of exposure (using a format such as SST allows) could facilitate ATT and decrease the risk of premature dropout.
In fact, by adding SST, what we seem to do is make it possible that initially the action/relationship with others, in the most representative dreaded/avoided social situations, occurs (1) gradually accomplished through exposure tasks with age-matched peers, and (2) under the control of therapists who explain, instruct, model, orient, and guide/reinforce, in line with Manassis, Avery, and Mendlowitz (2004), who indicated that the CBT delivered in peer groups that allow for exposure and skills practice might be well suited for youth with a major diagnosis of SAD.
In adolescents with SAD, this approach would facilitate the perception of a less aversive, friendlier, and safer context, which will likely increase participants’ OE during training, with the consequences seemingly derived from preventing abandonment, increased ATT, and improved outcomes. In fact, post-treatment of the clinical significance of the participants’ results with “poor response treatment” shows that they went from 64% (IAFS) and 78% (IAFS-R) in the post-test to 25% and 58.4%, respectively, at the 12-month follow-up (Table 2). In both groups, there was a significant reduction in those who failed to meet the diagnostic criteria after the post-test, but this number in the IAFS (39%) was twice that in the IAFS-R (19.6%) with the difference being that while in the IAFS only 8.3% had an improvement of less than 50% in the NSSFA, whereas in the pretest in the IAFS-R this was five times greater: 41.7%. It appears that the positive and negative effects of the presence/absence of SST on treatment extend beyond treatment sessions.
Also relevant is the role that OEs seem to play in our results since completers showed highly significant differences versus dropouts [t(70)=−3.87, p<.0001], which is in line with previous studies (see Price & Anderson, 2012; Taylor et al., 2012). In addition, high OEs were associated with a higher probability of overcoming SAD even in the worst conditions (IAFS-R). Recall that, although we did not find significant differences between the completers of IAFS and IAFS-R in OE, their average in the latter was higher (3.15 vs. 3.42) and their ES was significant (d=0.28).
Our research has limitations: the generalization of results is limited by the fixed effects design used, the inability to control the occurrence of cognitive responses of escape/avoidance in the participants, or the local character of our sample.
ConclusionsUse of SST is directly related to greater effect sizes and better results in clinical significance, which should support incorporating it into the treatment of adolescents with SAD. The absence of SST in interaction with the vulnerability profile of the dropouts generates an increase in the experimental mortality rate that is six times higher in IAFS-R than in IAFS. Therefore, high OEs are shown to be a strengthening factor that would increase the resistance to abandonment in the face of difficulties, playing a crucial role in ATT completers and their achievements, especially IAFS-R. Finally, although the best statistical and clinical results are related to the use of SST, this component seems necessary only to explain the reduction/elimination of SAD when the participants present vulnerability to abandonment. Furthermore, we posit that although the SST is generally not determinant it plays a necessary and very positive role in the treatment of GSP (severe SAD) in the adolescent community population.