Background/Objective: Impaired Inhibitory Control (IC) is a core feature of psychotic disorders and is related with impaired social functioning in people experiencing psychosis. Despite research showing the benefits of mindfulness over IC in the general population, no study has assessed its effects on IC in psychoses. The aim of our study was to assess the effectiveness of a mindfulness-based intervention combined with integrated rehabilitation treatment in a sample of people diagnosed of psychotic disorders. Method: Fifty-six patients diagnosed with psychotic disorder were recruited and randomly allocated either to integrated rehabilitation treatment or integrated rehabilitation treatment enhanced with 26 mindfulness group sessions. Measures comprised PANSS interview, MAAS scale, and Stroop Color Word Test (SCWT). The primary outcome variable was the performance in the non-congruent trials of the SCWT. Results: There were no differences between groups at baseline. At post-treatment patients allocated to mindfulness group increased their scores in non-congruent trials of SCWT and in MAAS. At post-treatment mindfulness group scored higher than integrated rehabilitation treatment in MAAS. Conclusions: Data suggest that mindfulness added to integrated rehabilitation treatment may improve IC in psychosis. Results are convergent with prior works about the effect of mindfulness over cognitive performance in general population.
Antecedentes/Objetivo: Los déficits en el control inhibitorio (CI) son una característica central en trastornos psicóticos y se relaciona con funcionamiento social deteriorado en personas con síntomas psicóticos. A pesar de las investigaciones que muestran los beneficios del mindfulness sobre el CI, ningún estudio ha evaluado sus efectos en las psicosis. El objetivo de este estudio fue evaluar la eficacia de una intervención basada en mindfulness combinada con tratamiento rehabilitador integrado en una muestra de personas diagnosticadas con trastorno psicótico. Método: Cincuenta y seis pacientes diagnosticados con trastorno psicótico fueron reclutados y asignados aleatoriamente a tratamiento rehabilitador integrado o a tratamiento rehabilitador integrado mejorado con 26 sesiones grupales de mindfulness. Las medidas fueron la entrevista PANSS, la escala MAAS, y el Test Stroop de Palabras y Colores (TSPC). La variable resultado principal fue el rendimiento en los ensayos no congruentes del TSPC. Resultados: No hubo diferencias entre grupos antes del tratamiento. En el postratamiento los pacientes del grupo de mindfulness incrementaron sus puntuaciones en TSPC y en MAAS. El grupo de mindfulness puntuó más alto que el de tratamiento rehabilitador integrado en MAAS. Conclusiones: El mindfulness añadido al tratamiento rehabilitador integrado puede mejorar el CI en las psicosis. Los resultados son convergentes con los trabajos previos sobre el efecto del mindfulness en la población general.
Inhibitory Control (IC) is the ability to control one’s attention, behavior, thoughts, and/or emotions to override a strong internal predisposition (Diamond, 2013). IC allows humans to modify their behavior through self-control and behavioral adaptation to the environment (Perri, 2020), for example by reducing a tendency to jump to a conclusion based on limited information, or to avoid a salient threatening stimulus. Lack of IC is implicated in a wide range of disorders, and a proposed deficit in IC has long been central to theories of schizophrenia and psychotic disorders (Ettinger et al., 2018).
Researchers have used the Stroop effect as one way to study the IC deficit in schizophrenia and other psychotic disorders (Laurenson et al., 2015). Prior studies have shown that people experiencing psychosis are slower and less accurate in the interference condition of Stroop test than healthy controls (Cadena et al., 2019; Popov, Kustermann, Popova, Miller, & Rockstroh, 2019) and this difference in performance is not related with premorbid IQ (Martin, Mowry, Reutens, & Robinson, 2015), or affective symptoms (Tyburski et al., 2017), or other cognitive processes (Ettinger et al., 2018). Also, the negative effect of ageing in Stroop performance is more pronounced in psychosis, which suggests that IC decline associated to aging starts earlier in psychosis (Thuaire et al., 2020). Taken together, these findings suggest that the cognitive impairment in schizophrenia is based in a common supramodal process stressed by IC (Spagna et al., 2018). Thus, targeting impairment in IC has been included as a priority in treatments aimed at promoting recovery in people diagnosed with a psychotic disorder (Cella & Wykes, 2019).
Cognitive remediation therapy for psychosis seeks to establish durable and generalizable improvement in cognition (Cella et al., 2019; Kurtz, Gagen, Rocha, Machado, & Penn, 2016; Wykes, Huddy, Cellard, McGurk, & Czobor, 2011). A common strategy in cognitive remediation approaches to psychosis has been to adapt interventions known to improve cognitive function in other disorders or in the general population. In this regard, mindfulness is a promising approach. Mindfulness-based interventions (MBIs) are safe and beneficial approaches for a range of mental and physical health conditions (Baer, Crane, Miller, & Kuyken, 2019), including psychosis (Chadwick, 2014; López-Navarro et al., 2015; Louise, Fitzpatrick, Strauss, Rossell, & Thomas, 2018). Mindfulness has been shown to improve IC performance in other populations (Fabio & Towey, 2018; Jaiswal, Tsai, Juan, Liang, & Muggleton, 2018; Teper & Inzlicht, 2013). Also, MBIs have shown a medium effect on the ability to resist dominant responses (Gallant, 2016).
A central aspect of relating mindfully to psychosis is to allow psychotic experiences such as voices to come fully into awareness by letting go of habitual reactive tendencies to avoid stimuli or react with aversion and struggle (Abba, Chadwick, & Stevenson, 2008; Chadwick, 2019). Therefore, mindfulness for psychosis can be framed as improving IC by teaching people to control prepotent reactions to psychotic sensations. Research has yet to examine the effects of a prolonged mindfulness training on IC in people with diagnoses of psychotic disorders. The present study used a randomized controlled design to compare the effects of 6 months of standard psychiatric rehabilitation versus 6 months of standard rehabilitation enhanced with weekly group mindfulness training on Stroop Color Word Test performance in people diagnosed with psychotic disorders from a community rehabilitation center. Based on the literature reviewed above, the study examined the hypothesis that mindfulness can improve IC to a more extent than integrated rehabilitation treatment alone in people experiencing psychosis. Also, our study explored the secondary hypothesis that the ability to notice feelings, thoughts and sensations without react to them will increase in participants attending mindfulness sessions and that this improvement will be superior to those participants allocated to an integrated rehabilitation program alone.
MethodParticipantsA single center randomized controlled clinical trial with pre and post-treatment measures was designed. Sixty-eight people diagnosed with psychotic disorder from a public community rehabilitation center were assessed for eligibility. Inclusion criteria were (1) age between 18-65; (2) one of the following DSM-IV-TR diagnosis: Schizophrenia (295.30; 295.10; 295.90), Schizoaffective Disorder (295.70), Delusional Disorder (295.70), Bipolar Disorder (296.40; 296.4x; 296.5x; 296.5x); (3) no changes in psychiatric medication or hospitalization in last month; (4) have signed informed consent; and (5) be able to understand and read the Spanish language. Exclusion criteria were (1) significant cognitive impairment assessed through clinical record; (2) inability to attend mindfulness or rehabilitation treatment sessions; (3) posed a risk of violence to the researchers; and (4) refused to participate or to sign informed consent. Due the naturalistic nature of the study, the sample was composed of different DSM-IV-TR diagnoses which had the common feature of presence of psychotic experiences and sensations. Also, participants in the study were unemployed, without any medical condition that could affect treatment outcome, were under anti-psychotic drug treatment, and did not showed comorbidity with other axis I or II DSM-IV-TR disorder. No payment was made for participation in the study. Data collection was carried between August 2013 and July 2015 at the same community rehabilitation center. Intention-to-treat analysis was used.
Multiple stochastic imputation was selected to deal with missing data (Scharfstein & McDermott, 2019). The study complied with the Declaration of Helsinki and was approved by the Research Ethics Committee of the University of Balearic Islands. Informed consent was obtained of each participant. Trial was registered in ISRCTN Registry: ISRCTN52873519.
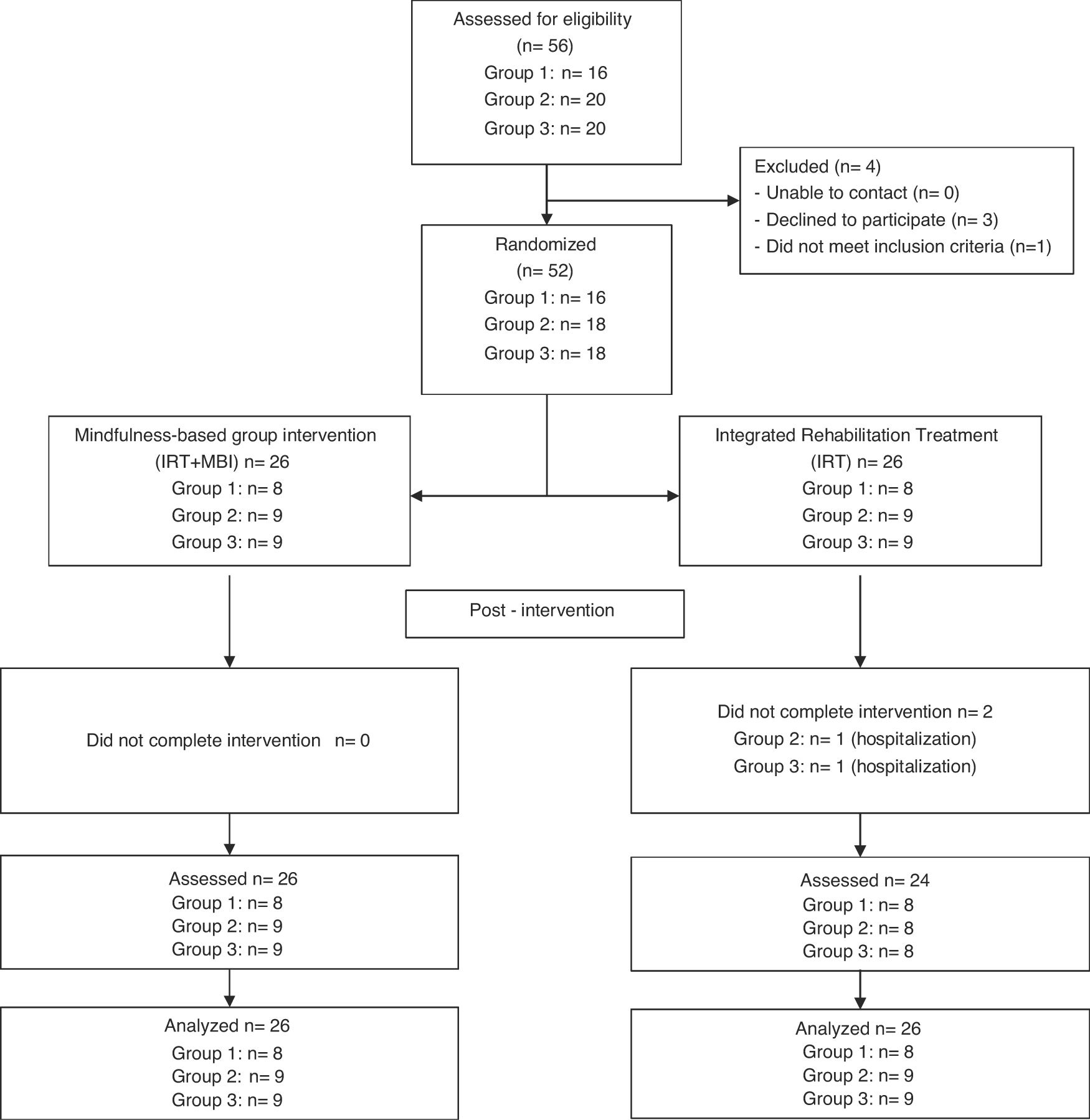
Individuals were contacted initially by their psychiatrist to perform a personal interview to be informed about mindfulness and what participation in the trial would involve and to assess eligibility. At the end of the interview eligible participants, or their legal guardians, were invited to participate and sign informed consent. After informed consent for trial participation was signed, randomization identification was assigned to each patient and recorded in the clinical record form. A master randomization list was created to record randomization identifications and corresponding treatment assignment, access to master randomization list was restricted to psychologist and psychiatrist who led mindfulness sessions. Patients were assessed by a research psychologist specifically trained to manage patients with psychotic features and coordinate clinical trials who was blind to patient allocation. Once assessed, participants were randomly allocated by software to Integrated Rehabilitation Treatment (IRT) or IRT + MBI group, with a maximum group size for MBI ranging from 8 to 12. Each of the three cohorts was randomized once numbers were sufficient to begin a mindfulness group. Recruitment process is detailed in Figure 1.
InstrumentsDemographic data and clinical features of participants were collected through a specifically designed clinical record form. Age, sex, psychotic disorder diagnosed, age at onset and years of education were recorded. Diagnoses were obtained through clinical record. Participants were assessed before and after treatment completion.
Spanish adaptation of the Positive and Negative Syndrome Scale (PANSS; Kay, Fiszbein, Vital-Herne, & Fuentes, 1990) was used to assess the frequency and intensity of psychotic symptoms. Interviews were videotaped to be scored at the end of the intervention by two clinical psychologists who were blinded to patient allocation.
Mindfulness Attention Awareness Scale (MAAS; Brown & Ryan, 2003) was used to detect changes in general mindfulness awareness in daily life. This 15-item scale focuses on attention/awareness component of mindfulness construct, and can be used to assess individuals either with or without meditation experience. The Spanish version of MAAS has good reliability indexes and good temporal stability (Soler et al., 2012).
Assessment of IC was conducted using the non-congruent trial of Stroop Color Word Test (SCWT; Golden, 1978). Paper and pencil version was used as it is validated in the Spanish population. Psychometric properties are equivalent to the original English version, and its considered a better measure of IC than the computerized versions of the Stroop paradigm (Penner et al., 2012). This version of the Stroop paradigm consists of three 45-second trials. In the first trial the participant reads aloud a series of color names printed in black as fast as possible. In the second trial they name the color of a series of ink swatches. In the third, non-congruent, trial, the participant is shown lists of color names printed in ink of a conflicting color and asked to name the ink color rather than reading the color word. Non-congruent trial requires recruitment of processes regarding the operation of deliberately inhibit dominant responses and select less likely behavior in presence of a competing tendency (Diamond, 2013). The non-congruent condition of SCWT is a reliable tool to assess IC in people experiencing psychosis: it is robust to within-subjects variability and detects changes in IC performance even when controlling for education and global cognitive performance (Laurenson et al., 2015; Scarpina & Tagini, 2017). SCWT also combines its reliability with enough sensitive capacity to detect cognitive impairment in psychotic disorders (Shi et al., 2019). Elements processed in 45 seconds were recorded as raw scores and used for statistical analyses.
InterventionThere were two treatment arms: IRT and IRT enhanced with group MBI. Both arms were delivered by routine clinical staff trained in rehabilitation and treatment of people experiencing psychoses, and for IRT + MBI in mindfulness applied to psychosis. IRT was a 26-week rehabilitation treatment oriented to manage intensity and frequency of psychotic symptoms, prevent relapses and hospitalization, as well improve social functioning. IRT comprised 26 one-hour weekly group sessions of cognitive behavior therapy techniques for symptom management as well as strategies for preventing relapse and conflict management. Bearing in mind the mediation effect of daily life stressors in the relationship between psychotic experiences and psychological well-being (López-Navarro, del Canto, Mayol, Fernández-Alonso, & Munar, 2018), group sessions were designed with a strong component of social skills training. Sessions one to six aimed to teach participants about the A-B-C schema and how feelings and thoughts are related with environment. Sessions seven to nine were designed to illustrate the A-B-C schema with daily life situations reported by the participants. During sessions ten to sixteen participants were taught about social skills and assertiveness techniques, which contents were used for the role-playing sessions seventeen to twenty. Finally, sessions twenty-one to twenty-six entailed problem solving applied to daily-life social situations reported by the participants as distressful or harmful for them. Along the group sessions, to prevent relapse and hospitalization each participant was interviewed once a week to adjust pharmacotherapy treatment – if necessary –. IRT contained no mindfulness training or family intervention.
IRT + MBI group ran throughout the 26-week rehabilitation treatment program. Mindfulness component followed the protocol described by López-Navarro et al. (2015). The first author attended 60% sessions to confirm treatment fidelity against the manual. The aim of the mindfulness sessions was to change how participants relate with the psychotic sensations. Mindfulness teach to react with acceptance to the content of the experience instead struggling with. In sum, mindfulness sessions sought to teach participants to perceive voices or thoughts as what they are and not what they say they are. Mindfulness group therapy sessions lasted 60 minutes and were carried out in venue ceded for free by city council. As physical sensations are used in mindfulness applied to psychoses to anchor to the present moment, every session began with a habituation period to the room with relaxing music as background followed by 10-minute body awareness exercises led by a trained psychologist. Then, 15 minutes of guided meditation was led by a psychiatrist and a clinical psychologist trained in mindfulness and experienced in working with psychotic patients. Frequent guidance was imparted encouraging awareness and acceptance of bodily sensations, sensations of breathing, and thoughts, images and voices that might arise. To achieve this, instructions given sought to foster participants to advert and let go of worry and engagement with the content of thoughts, voices or other psychotic symptoms that might arise, and of criticism or judgement. Finally, sessions included 15 minutes of reflective group discussion aimed at facilitating patients’ understanding and insights drawn from the mindfulness practice. Home practice was encouraged between mindfulness sessions and participants were given an audio tape for home practice with the guidance instructions used during group sessions.
Statistical analysesDescriptive statistics were generated for the sample and for each treatment arm. Statistical analyses were performed using raw scores. Assumption of normality and homogeneity of variances was tested in the outcome variable before conduct analyses, using Shapiro-Wilk test and Levene test respectively. Groups were compared at baseline on sociodemographic, clinical variables, self-reported mindfulness, and SCWT scores. The primary outcome variable was IC measured through SCWT non-congruent trial, and self-reported mindfulness assessed with MAAS scale was set as secondary outcome.
To test for group differences, a repeated-measures analysis of variance (ANOVA) was conducted for STCW non-congruent trial and MAAS scores. Treatment condition (IRT, IRT + MBI) was set as between-participants factor and Time (baseline and post-treatment) as within-participants factor. Thus for every measure, there are seven lines of results: the four simple effects, the two main effects -Treatment and Time-, and the interaction effect between these two factors. Interaction was analyzed using Bonferroni correction to control Type I error rate across comparisons. Eta squared was used as effect size. Reliable Change Index (RCI), following the recommendations of Christensen and Mendoza (1986), was used to estimate individual change in primary and secondary outcomes. If parametric assumptions were not met a bootstrapped ANOVA was performed at 2000 iterations. Data were analyzed with IBM SPSS 23 for Windows. Statistical significance was set at .05.
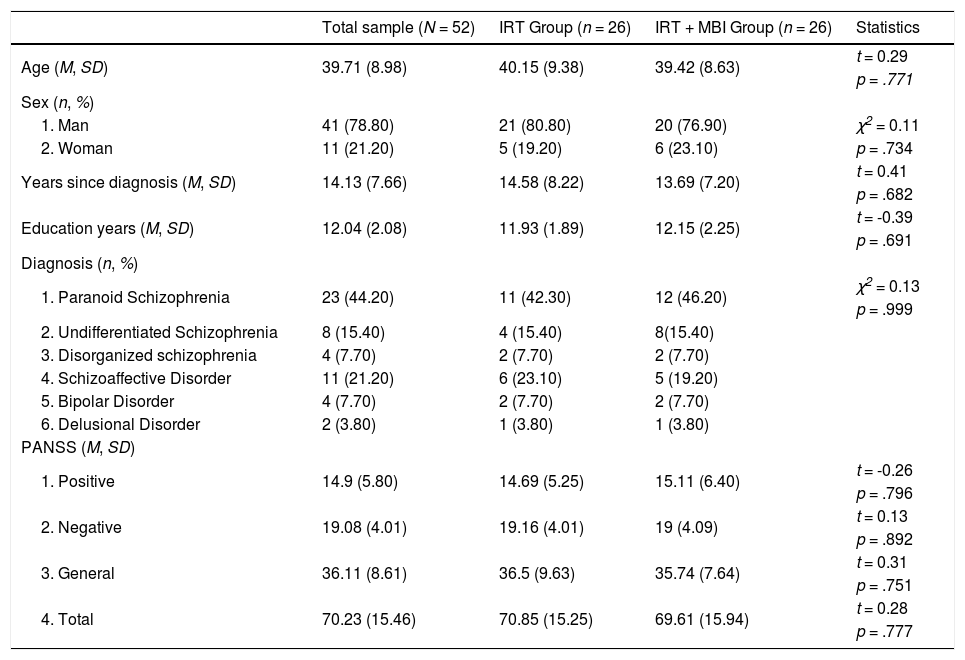
ResultsSixty-eight people were assessed against inclusion criteria, four declined to participate and twelve did not meet inclusion criteria. Fifty-two participants gave signed consent and were randomly allocated either to IRT or MBI + IRT. On average participants attended 91.58% of the 26 mindfulness sessions (range 21 to 26). Table 1 shows the demographics and clinical features of the sample. Both STCW non-congruent and MAAS Scores met normality and homoscedasticity assumptions, W(52) = 0.97, p = .380, F(50) = 0.43, p = .511, W(52) = 0.97, p = .466 – F(50) = 0.43, p = .607, in order.
Clinical and demographic characteristics of the sample.
| Total sample (N = 52) | IRT Group (n = 26) | IRT + MBI Group (n = 26) | Statistics | |
|---|---|---|---|---|
| Age (M, SD) | 39.71 (8.98) | 40.15 (9.38) | 39.42 (8.63) | t = 0.29 |
| p = .771 | ||||
| Sex (n, %) | ||||
| 1. Man | 41 (78.80) | 21 (80.80) | 20 (76.90) | χ2 = 0.11 |
| 2. Woman | 11 (21.20) | 5 (19.20) | 6 (23.10) | p = .734 |
| Years since diagnosis (M, SD) | 14.13 (7.66) | 14.58 (8.22) | 13.69 (7.20) | t = 0.41 |
| p = .682 | ||||
| Education years (M, SD) | 12.04 (2.08) | 11.93 (1.89) | 12.15 (2.25) | t = -0.39 |
| p = .691 | ||||
| Diagnosis (n, %) | ||||
| 1. Paranoid Schizophrenia | 23 (44.20) | 11 (42.30) | 12 (46.20) | χ2 = 0.13 |
| p = .999 | ||||
| 2. Undifferentiated Schizophrenia | 8 (15.40) | 4 (15.40) | 8(15.40) | |
| 3. Disorganized schizophrenia | 4 (7.70) | 2 (7.70) | 2 (7.70) | |
| 4. Schizoaffective Disorder | 11 (21.20) | 6 (23.10) | 5 (19.20) | |
| 5. Bipolar Disorder | 4 (7.70) | 2 (7.70) | 2 (7.70) | |
| 6. Delusional Disorder | 2 (3.80) | 1 (3.80) | 1 (3.80) | |
| PANSS (M, SD) | ||||
| 1. Positive | 14.9 (5.80) | 14.69 (5.25) | 15.11 (6.40) | t = -0.26 |
| p = .796 | ||||
| 2. Negative | 19.08 (4.01) | 19.16 (4.01) | 19 (4.09) | t = 0.13 |
| p = .892 | ||||
| 3. General | 36.11 (8.61) | 36.5 (9.63) | 35.74 (7.64) | t = 0.31 |
| p = .751 | ||||
| 4. Total | 70.23 (15.46) | 70.85 (15.25) | 69.61 (15.94) | t = 0.28 |
| p = .777 |
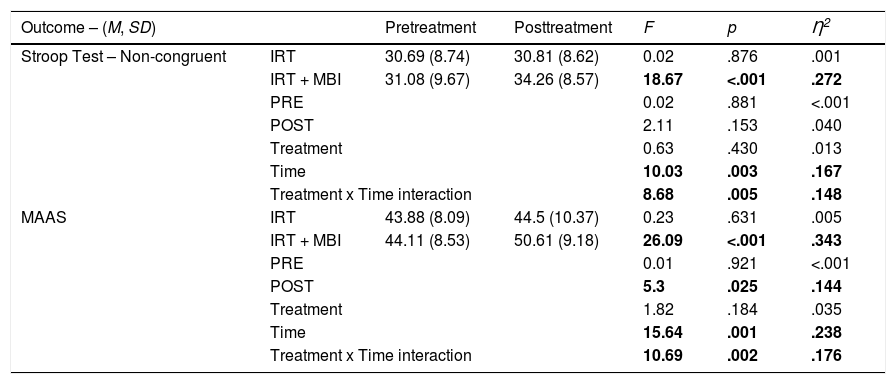
Repeated measures ANOVA on STCW non-congruent scores revealed a significant effect of time, F(1, 50) = 10.03, p = .003, and interaction, F(1, 50) = 8.68, p = .005, both associated to a large effect size, η2 = .167, 95% CI [.038, .314] and η2 = .148, 95% CI [.028, .293], respectively. Analysis of simple effects of the interaction revealed that performance of IRT + MBI group increased after treatment completion, F(1, 50) = 18.67, p < .001, η2 = .27, 95% CI [.108, .272]. RCI estimation showed that 10 out of 26 patients in IRT + MBI presented a reliable change difference in STCW non-congruent scores, and 3 out of 26 in IRT.
The ANOVA on MAAS scores showed a significant main effect of Time – F(1, 50) = 15.64, p = .001, η2 = .238, 95% CI [.083, .385] –. The main effect of Treatment was not significant – F(1, 50) = 1.82, p = .184, η2 = .035, 95% CI [.001, .147]. Interaction between Time and Treatment was significant, F(1, 50) = 10.69, p = .002, η2 = .176, 95% CI [.043, .323]. Analyses of interaction components revealed significant differences between pre and post treatment in the MBI group, F(1, 50) = 26.09, p < .001, η2 = .343, 95% CI [.167, .48], and between groups at post treatment, F(1, 50) = 5.3, p = .025, η2 = .144, 95% CI [.005, .229] (see Table 2). RCI estimation of MAAS scores differences was found significant in 17 out of 26 in IRT + MBI, and 4 out of 26 in IRT group.
Repeated Measures ANOVA over Stroop Non-congruent and MAAS scores.
| Outcome – (M, SD) | Pretreatment | Posttreatment | F | p | Ƞ2 | |
|---|---|---|---|---|---|---|
| Stroop Test – Non-congruent | IRT | 30.69 (8.74) | 30.81 (8.62) | 0.02 | .876 | .001 |
| IRT + MBI | 31.08 (9.67) | 34.26 (8.57) | 18.67 | <.001 | .272 | |
| PRE | 0.02 | .881 | <.001 | |||
| POST | 2.11 | .153 | .040 | |||
| Treatment | 0.63 | .430 | .013 | |||
| Time | 10.03 | .003 | .167 | |||
| Treatment x Time interaction | 8.68 | .005 | .148 | |||
| MAAS | IRT | 43.88 (8.09) | 44.5 (10.37) | 0.23 | .631 | .005 |
| IRT + MBI | 44.11 (8.53) | 50.61 (9.18) | 26.09 | <.001 | .343 | |
| PRE | 0.01 | .921 | <.001 | |||
| POST | 5.3 | .025 | .144 | |||
| Treatment | 1.82 | .184 | .035 | |||
| Time | 15.64 | .001 | .238 | |||
| Treatment x Time interaction | 10.69 | .002 | .176 | |||
Note. IRT and IRT + MBI rows show interaction analysis for Time factor (Within subjects). PRE and POST rows show interaction analysis for Treatment factor (Between subjects).
The present study offers preliminary evidence of benefits in inhibitory control (IC) following long-term mindfulness training added to standard rehabilitation treatment for people experiencing psychosis. The large effect size observed in the mindfulness condition partially supports the main hypothesis of the study, and is consistent with prior research addressing the effect of mindfulness training on Stroop performance in other populations (Chesin et al., 2016; Dunning et al., 2019; Jensen, Vangkilde, Frokjaer, & Hasselbalch, 2012; Teper & Inzlicht, 2013). However, improvement in Stroop scores at post-treatment in the mindfulness group was not significantly superior to rehabilitation treatment alone, which partially does not support the main hypothesis of the study. On the other hand, participants in the mindfulness group showed higher self-reported mindfulness after treatment completion and scoring higher than the rehabilitation condition after treatment completion. These results provide support to our secondary hypothesis about the effect in people experiencing psychosis of a mindfulness-based intervention over the ability of notice feelings, thoughts and sensations without react to them.
The importance of improving IC in people diagnosed with psychosis is well-recognized (Cella & Wykes, 2019; Kurtz et al., 2016). IC as measured using Stroop is correlated with quality of life in people experiencing psychoses (Ojeda et al., 2019), with social functioning in prodromal psychosis and when diagnosis is confirmed (Kim et al., 2019); and IC is identified as a key mechanism for improving social functioning in cognitive rehabilitation for psychosis (Peña et al., 2018). Mindfulness training is known to enhance IC in other clinical and non-clinical groups (Gallant, 2016), and is conceptualized to benefit people with psychosis by training them to recognize and let go of habitual reactions to psychotic sensations, such as aversion and avoidance (Chadwick, Taylor, & Abba, 2005). Learning the skill of over-riding a strong, habitual reactive tendencies and choosing instead to adopt what is initially at least a less likely behavioral response (decentered awareness) can be understood in terms of increased IC.
Strengths of the current study are: the randomized controlled design with blind assessment; the use of a well-defined and standardized active control treatment (participants were drawn from the same community healthcare service); sustained mindfulness training; delivery of both interventions by suitably trained routine clinical staff; low drop-out rate; the naturalistic environment where the trial was performed increases the external validity; and the first data on impact of sustained mindfulness training on IC in psychotic disorders. Limitations include: sample size; an uneven sex distribution although it is convergent with epidemiology of the psychotic diagnosis in Spanish population; home practice of mindfulness was encouraged but not measured; no follow-up period; and active control group did not receive placebo sessions to compensate the extra training received by the mindfulness group. Also, it is important to point out that the features of the sample are mixed, as participants do not share the same psychotic diagnostic. Future research should address this issue. As pointed by Medina-Mora et al. (2019), DSM-IV-TR criteria is less pragmatic and sensible than upcoming ICD-11 guidelines.
FundingThis work was supported by the European Social Fund-European Commission [Operative Project FSE 2014-2020]; the Board of Innovation, Research and Tourism of the Balearic Islands [FPI/1806/2015]; and the Spanish Ministry of Economy and Competitiveness [FFI2013-43270-P].