Dear Editor:
Lung cancer is one of the most frequent types of cancer in both men and women.1 Between 30-70% recur in the first 5 years. Approximately 5-15% of patients present recurrence at 5 years despite previous curative treatment. Pancoast syndrome occurs in only 1%–3% of all lung tumours, and rarely presents as the initial manifestation of late recurrence (15 years of disease freedom).2–5
We present the case of a 57-year-old man with history of squamous cell carcinoma of the lung, treated 15 years previously with right upper lobectomy, chemotherapy (cisplatin), and radiotherapy. He was referred to the neurology department due to 2-month history of an itching and burning sensation in the right arm and axillary hyperhidrosis. The neurological examination revealed mild right ptosis, miotic and non-reactive right pupil, amyotrophy of the trapezius and supraspinatus muscles, and hyperaesthesia in the suprascapular region.
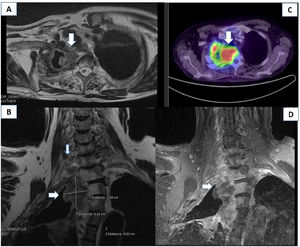
An electromyoneurography study revealed alterations to the superior and middle trunks of the brachial plexus (Fig. 1). A blood analysis detected hypercalcaemia (11 mg/dL) and hyponatraemia (117 mmol/L), which were asymptomatic. A head, neck, chest, and abdomen CT scan revealed irregular thickening of the apical-medial wall of the post-lobectomy cavity; the mass was polypoid and protruded to the lumen, involving soft tissue and eroding the adjacent bone structures. This finding is compatible with tumour infiltration to the T2–T3 intervertebral foramen (Fig. 2). An MRI study of the brachial plexus revealed tumour infiltration in the right brachial plexus at the level of the scalene triangle, with involvement of the nerve roots due to perineural invasion and proximity to the intervertebral foramina, particularly at C7–T1 and C6–C7, with involvement of the C7, T1, T2, and T3 vertebral bodies (Fig. 2). PET-CT revealed increased uptake in the cervical tumoural mass (Fig. 2), with no signs of dissemination to other areas. The cytological study of a bronchial biopsy sample revealed malignant cells (recurrence of lung epidermoid carcinoma, stage IIIB). The patient was started on chemotherapy and radiotherapy, but died 4 months later due to pneumonia.
Electroneuromyography showing no impairment of motor branches of the median and ulnar nerves (A, B), impairment of sensory branches of the right median, ulnar, and superficial radial nerves (C, D, E), and absence of acute activity in the form of spontaneous denervation of the right deltoid muscle (F).
(A) Lung CT scan showing a mass in the apex of the right lung, causing ganglion compression and T2 displacement and invasion. (B and D) An MRI scan of the right brachial plexus (coronal section, STIR and T1FSE sequences) showed a mass measuring 3.58 × 4.42 cm at the level of the lung apex and displacing the T1–T3 vertebral bodies, reaching the roots of the distal brachial plexus. (C) PET-CT scan revealing increased 18F-FDG uptake in the mass.
Pancoast syndrome is defined as a tumour affecting the lung apex and infiltrating to the subpleural lymph nodes, potentially reaching the C7–C8 and T2–T3 nerve roots, causing plexopathy with amyotrophy and pain. The tumour may also affect bone structures and the sympathetic chain, causing Horner syndrome, with the classic triad of ptosis, miosis, and anhidrosis. Although this type of tumour grows slowly, in our patient it developed in barely 2 months from the latest chest CT scan showing normal results. Our patient did not present facial anhidrosis (present in only 4% of patients with the classic triad), but he did present axillary hyperhidrosis and pruritis, secondary to a lesion to the brachial plexus and involvement of T3–T4 sympathetic chain ganglia.
We would like to underscore the importance of correctly assessing such mild symptoms as unilateral hyperhidrosis or pruritis in patients with history of cancer, despite complete resolution many years earlier.
Ethical considerationsThis study complies with our centre's protocols for the publication of patient data and have obtained the relevant permits.
Conflicts of interestThe authors have no conflicts of interest to declare.