According to the literature, patients with multiple sclerosis (MS) are less active and show higher levels of sedentary behaviour than the general population of the same age range. This study aims to explore the impact of the COVID-19 pandemic on levels of physical activity in these patients.
MethodsAn online survey was launched between May and June 2021, aimed at patients with MS in Spain, regarding their physical activity habits (performance, intensity, and activities carried out) prior to and during the COVID-19 pandemic.
ResultsA total of 230 patients responded to the survey, of whom 69.6% were women, 52.6% were between 45 and 64 years old, and 41.3% had moderate disability (Patient-Determined Disease Steps score 3–5). A total of 82.2% of the respondents reported being physically active before the pandemic, decreasing to 75.9% during the pandemic [P=.057 (McNemar test)]. Activities at sports centres decreased and exercise at home, as well as walking, increased. A total of 61.7% reported not using any technology during physical activity practise before the pandemic. For 63.9% of respondents, the preferred format after the pandemic was the mixed format combining in-person and remote physical activity.
ConclusionsPhysical activity levels decreased during the COVID-19 pandemic among patients with MS. Although SARS-CoV-2 is currently in an endemic phase, this experience should be helpful for the development and implementation of interventions to facilitate physical activity among patients with MS.
Según la literatura, las personas con esclerosis múltiple (PcEM) son menos activas y muestran niveles más altos de sedentarismo que la población de su mismo rango de edad. El objetivo de este estudio es conocer cuál fue el impacto de la pandemia por COVID-19 en el nivel de actividad física (AF) de las PcEM.
MétodosEstudio mediante una encuesta online lanzada entre mayo y junio del 2021, dirigida a PcEM en territorio español, sobre los hábitos de AF (rendimiento, intensidad y actividades realizadas) previos y durante la pandemia por COVID-19.
ResultadosUn total de 230 PcEM contestaron la encuesta, de los cuales un 69.6% eran mujeres, un 52,6% tenían entre 45 y 64 años y un 41,3% una discapacidad moderada (PDSS 3–5). Antes de la pandemia, el 82,2% de los encuestados referían ser físicamente activos, reduciéndose a un 75,9% durante la pandemia (McNemar; p = .057). Disminuyeron las actividades en centros deportivos y se incrementaron las desarrolladas en el domicilio, así como caminar como ejercicio. Un 61,7% refería no utilizar tecnología durante la práctica de AF antes de la pandemia. El formato de preferencia tras la pandemia para el 63,9% fue el formato mixto combinando AF presencial y remota.
ConclusionesLa AF disminuyó durante la pandemia por COVID-19 entre las PcEM. Aunque actualmente se encuentra en una fase endémica, esta experiencia debería ser un impulso para el desarrollo y aplicación de intervenciones que faciliten su práctica entre las PcEM.
Multiple sclerosis (MS) is a chronic, degenerative, autoimmune disease of the central nervous system, affecting over 2 million people worldwide, and is the leading non-traumatic cause of disability in young adults.1 Spain is considered a country with moderate-high MS prevalence, with 80–180 cases/100 000 population.2 MS can cause a broad range of neurological signs and symptoms, resulting in an increase in physical and cognitive disability over time.3
There is a consistent body of evidence that patients with MS are less physically active and present greater levels of sedentary behaviour than the general population in the same age range.4 Sedentary lifestyles are associated with higher levels of disability and the appearance of comorbidities and secondary complications that exacerbate the primary symptoms of the disease.5 It has recently been suggested that lack of physical fitness may contribute to increased motor disability.6
Physical rehabilitation is a key part of the comprehensive management of MS, seeking to maintain or improve physical fitness and levels of activity and participation.7 Tailored exercise interventions have been shown to be beneficial and highly valuable in maintaining good health and preventing complications associated with inactivity; they also reduce mortality rates.8
The COVID-19 outbreak was officially declared a pandemic by the World Health Organisation on 11 March 2020, and had severe repercussions on all areas of the Spanish healthcare system, including neurorehabilitation.9 The lack of specific therapeutic or preventive interventions during the first year of the pandemic, together with the high transmission rate of the virus, led governments to take measures to restrict mobility and enforce physical distancing; this particularly impacted elderly people and people with chronic diseases, including MS.10
These restrictions resulted in the closure of in-person neurorehabilitation departments for the multidisciplinary treatment of MS, including those of Fundació Esclerosi Múltiple (FEM) and the Multiple Sclerosis Association of Biscay (ADEMBI, for its Spanish initials). In response, electronic care protocols were put in place to minimise the impact on patient care.11
The implementation of electronic rehabilitation programmes became a generalised trend. Adherence to these programmes was low, although some studies reported better outcomes in programmes combining in-person physiotherapy sessions with home exercise programmes. This was attributed to the lack of support and supervision during sessions, the lack of immediate relief of symptoms, and doubts about the treatment. Social support appears to be a key factor in adherence to these programmes.12,13
The Special Interest Group in Mobility of the European Network for the Best Practice and Research in Multiple Sclerosis (RIMS) developed a research project at the European level to analyse the initial impact of the COVID-19 pandemic on physical rehabilitation in MS from the patient perspective, comparing the findings against the pre-pandemic situation. This article presents the results from Spain.
The objectives of the study were to understand the impact of the COVID-19 pandemic on participation in physical activity among patients with MS, and to establish patients' opinions on the use of electronic tools in response to the early lockdown measures implemented in Spain.
MethodsAll phases of the project were developed in accordance with the Checklist for Reporting Results of Internet E-Surveys (CHERRIES).14
DesignThe study was based on an online survey aimed at patients with MS. In an initial phase, an interactive survey creation process was followed; from the first draft, researchers from all participating countries (Australia, Belgium, Czech Republic, Ireland, Israel, Italy, Norway, Serbia, Spain, Turkey, United Kingdom) participated in drafting the content of the survey until a final, English-language version was reached.
DevelopmentThe English-language survey was translated into the local languages of each participating country according to the translation/back-translation method proposed by Beaton et al.15 A lead research centre was assigned in each country; in Spain, this was the Multiple Sclerosis Centre of Catalonia (Cemcat). The study was approved by the clinical research ethics committee of Hospital Universitari Vall d'Hebron (project code PR[AG]143/2021). Participating centres and collaborating entities in Spain were the neurorehabilitation centres of FEM, ADEMBI, and Esclerosis Múltiple Euskadi; and the Spanish Federation of Multiple Sclerosis (Esclerosis Múltiple España).
The survey (Supplementary Material 1), distributed with the EUSurvey platform, comprised 74 questions and took approximately 30 min to complete. Questions were presented in a multiple-choice format and could not be skipped; the survey was divided into sections. The first section presented information about the study and required patients to give informed consent before they could access the remaining sections. The next section asked about the characteristics of the respondent: age, sex, time since diagnosis, level of disability (Patient-Determined Disease Steps [PDDS] scale),16 and changes since the beginning of the pandemic.
The main sections of the survey focused on respondents' physical activity before and during the pandemic. For each time period, participants could report up to 3 activities, from a list of 16. For each activity, the following information was collected: type of activity, frequency (days/week), duration (average minutes/session), and intensity (light, moderate, strenuous). The definitions of physical activity and intensity used in the survey were explained.
Lastly, the survey enquired about the reasons for which respondents' physical activity habits may have changed during the pandemic, and a final section asked about their habits and opinions regarding the use of technology to support physical activity.
Data collectionThe survey was distributed over a 6-week period between March and May 2021, using the mailing lists of FEM, ADEMBI, and Esclerosis Múltiple España. A reminder was sent every 2 weeks through the different communication channels of the collaborating organisations.
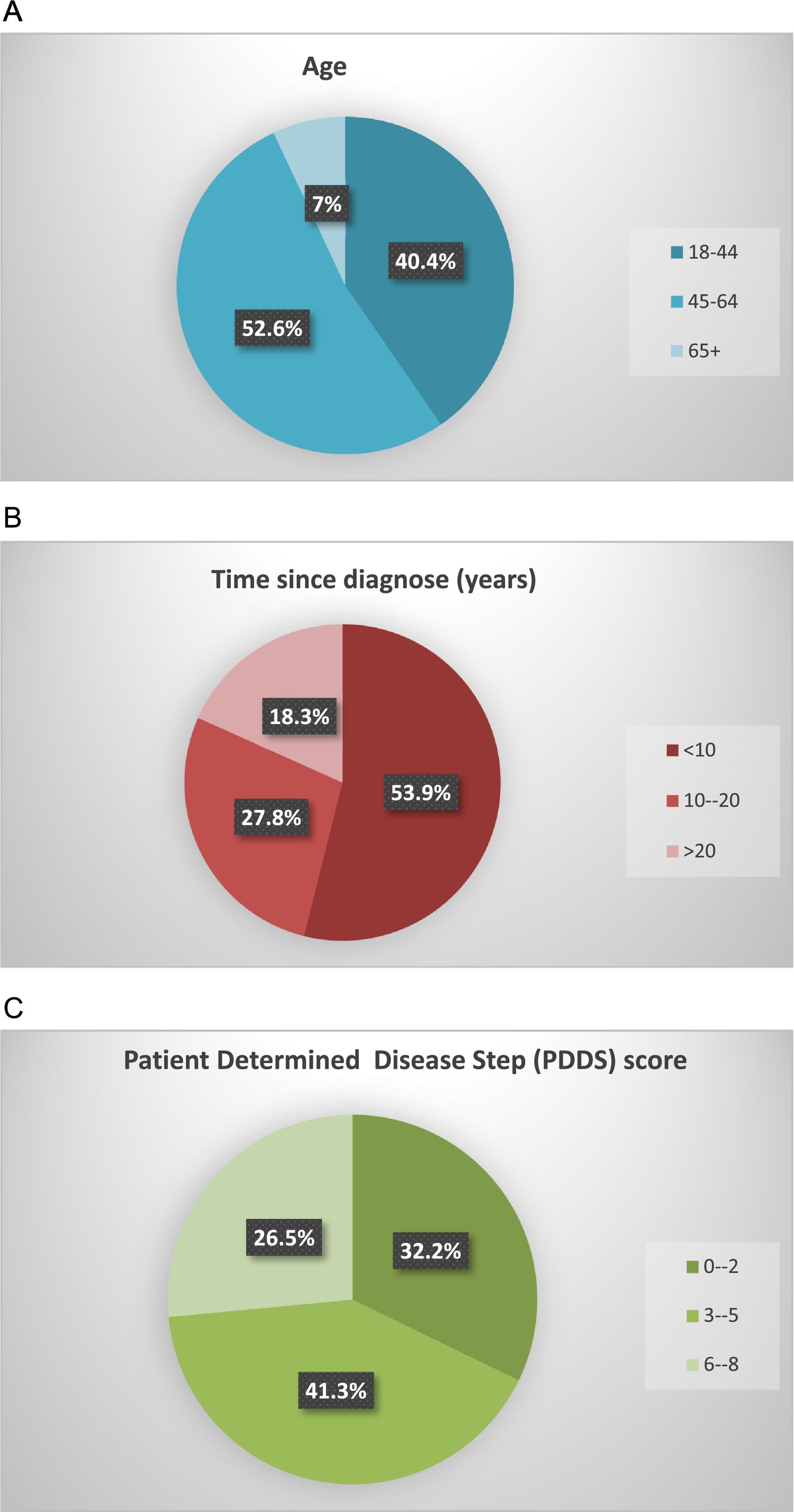
Statistical analysisQuestions involving perceived ratings are reported as percentages of the total number of responses. Age and time since diagnosis were each classified into 3 categories (18–44, 45–64, and >64 years; and <5, 5–15, and >15 years, respectively). PDDS was classified into 3 categories according to the conversion table presented by Kobelt et al17; thus, PDDS scores are divided into 3 levels of disability: 0–3 (mild), 4–6 (moderate), and 7–8 (severe).
The McNemar test was used to determine whether there were differences between the percentage of respondents who performed physical activity before and during the pandemic.
The total number of minutes of activity per week was calculated by multiplying session duration by the number of sessions for each activity; results were added together for up to 3 activities. Subsequently, we calculated the difference in participation in physical activity (minutes per week) before and during the pandemic.
Statistical analysis was performed using the IBM SPSS software (version 23). P-values <.05 were considered statistically significant.
ResultsSociodemographic characteristics of survey respondentsThe results obtained at the European level are reported by Moumdjian et al.18 In Spain, the survey was completed by 230 patients with MS, whose sociodemographic and clinical characteristics are summarised in Fig. 1. The participants constitute a representative sample of the population with MS; 69.6% were women and 52.6% were aged between 45 and 64 years. More than half of respondents (53.9%) had been diagnosed with MS less than 10 years prior, with 41.3% presenting moderate disability (PDDS scores of 3–5).
From the beginning of the pandemic to the moment of data collection (May–July 2021), 75.7% of respondents had not presented symptoms of COVID-19; among the remaining 24.3%, only 7.4% had tested positive for the infection. Of the 24.3% who reported that they had presented symptoms of COVID-19, 8.3% reported worsening of their MS symptoms and a decrease in physical activity levels since the infection, although a much larger percentage (42.1%) believed that their physical condition had worsened during the pandemic, regardless of whether they had contracted the infection.
A total of 43.1% were moderately or extremely worried about SARS-CoV-2 infection; the same percentage reported that their levels of physical activity had changed during the pandemic.
Physical activityA significant decrease was observed in the number of participants performing physical activity after the start of the pandemic [82.2% before the pandemic and 75.9% at the time of survey completion; P=.057 (McNemar test)]. The median number of minutes of physical activity per week also decreased significantly [192 vs 135; P<.001 (Wilcoxon signed-rank test)].
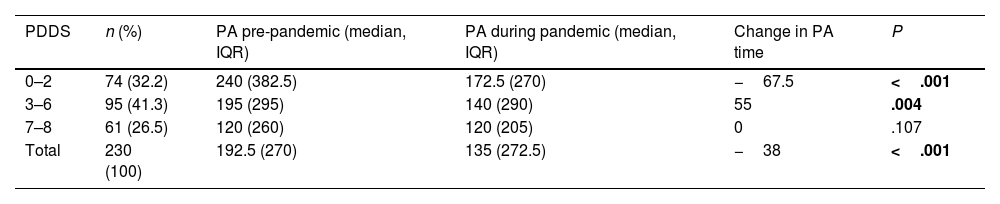
Table 1 presents the relationship between the reduction in physical activity and level of disability (PDDS score).
Level of physical activity before and during the COVID-19 pandemic, in patients with different levels of disability. Physical activity is expressed in minutes per week. IQR: interquartile range; PA: physical activity; PDDS: Patient-Determined Disease Steps score.
| PDDS | n (%) | PA pre-pandemic (median, IQR) | PA during pandemic (median, IQR) | Change in PA time | P |
|---|---|---|---|---|---|
| 0–2 | 74 (32.2) | 240 (382.5) | 172.5 (270) | −67.5 | <.001 |
| 3–6 | 95 (41.3) | 195 (295) | 140 (290) | 55 | .004 |
| 7–8 | 61 (26.5) | 120 (260) | 120 (205) | 0 | .107 |
| Total | 230 (100) | 192.5 (270) | 135 (272.5) | −38 | <.001 |
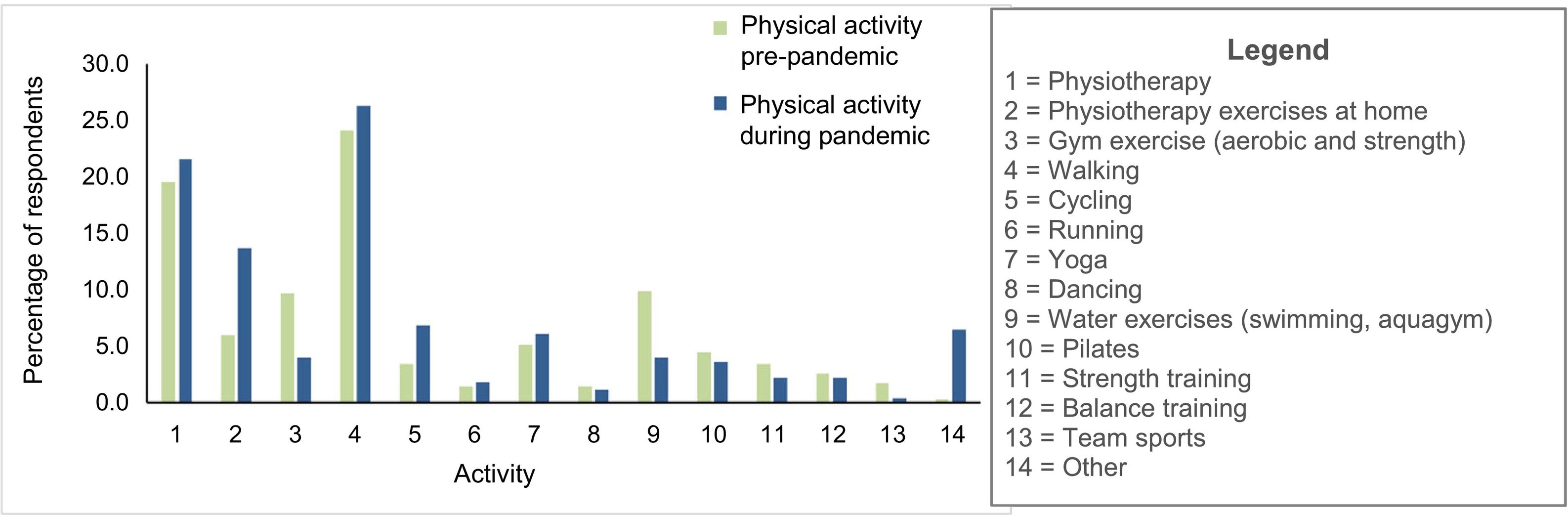
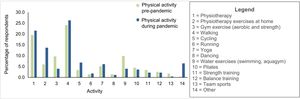
The contingency model revealed changes in the 14 different activities reported (χ2=520.19; P<.001; Fig. 2).
The activities showing the greatest decreases were exercises in the gym (reduction from 13.2% to 5.8%) and exercise in water (from 13.2% to 4.7%). On the other hand, considerable increases were observed in physiotherapy home exercise (increase from 3.7% to 14%), static bike exercise (from 2.6% to 5.8%), and especially walking (from 22.2% to 30.2%).
The places where respondents most frequently reported exercising were at home (30.2%), outdoors (29.7%), and at rehabilitation centres (22.1%); they mostly exercised individually (75.4%) and at light-moderate intensity (90.6%). In addition to this first form of physical activity, 44.1% reported a second and 41.9% a third.
Among respondents whose level of physical activity had remained the same or increased, the most frequently cited reasons were greater awareness of the healthcare authorities' messaging regarding the importance of physical activity (16.1%), greater family support (10.9%), and more structure and routine in the day (10.4%).
Among those reporting decreased levels of physical activity, the main reasons cited were the closure of gyms and rehabilitation centres (26.5%), restrictions imposed on mobility (24.3%), worsening of MS symptoms (20%), loss of motivation (19%), and fear of SARS-CoV-2 infection (17.8%).
Regarding the use of technology to support physical activity, the positive aspects mentioned included not having to travel to the venue (40.9%), the ability to decide when to exercise (23%), and the time saved (20%). The most frequently reported negative aspects were difficulty finding an appropriate space at home (31.7%), lack of social contact (27%), lack of enjoyment of this type of physical activity (15.7%), and difficulty performing exercises without physical support (13%). The preferred format after the pandemic was a mixed approach combining in-person and remote physical activity (63.9%).
DiscussionThis article reports the results obtained in the Spanish population as part of an international study on changes in physical activity habits among patients with MS as a result of the COVID-19 pandemic, with data gathered through an online survey. The main conclusion from the overall data from all participating countries was that the percentage of patients who were physically active significantly decreased, from 83% to 75%.18 Our data show a practically identical decrease, which was also statistically significant.
In terms of the effectiveness of exercise, the time and the type of physical exercise needed to obtain benefits are important. Published guidelines based on the scientific evidence and expert opinion recommend that the general population of patients with MS perform at least 150 min of physical activity per week, including both aerobic exercise and strength training.19,20 With regard to intensity, although patients with MS typically practise low- or moderate-intensity physical activity, Campbell et al21 report that high-intensity interval training is safe, well-tolerated, and effective in improving physical fitness in patients with MS and mild disability. Joisten et al22 found that 3 weeks of high-intensity interval training reduces levels of cellular markers of inflammation in patients with MS; therefore, this type of training may have benefits for disease progression.
In the analysis of the overall data from the full sample, Pedullà et al23 report a general reduction in the time dedicated to physical activity each week, particularly among patients with milder disability.23 The Spanish data also showed a greater decrease (67.5 min) among patients with lower PDDS scores. This may be due to the fact that survey completion coincided with the strictest lockdown measures. However, other authors report lower levels of physical activity in patients with MS and minimal motor involvement than among the healthy population of the same age range. Gervassoni et al24 observed lower levels of high-intensity physical activity and a higher percentage of individuals who performed no physical activity among patients with minimal disability; this finding was associated with higher levels of self-reported fatigue.24 Huynh et al25 also observed a correlation between insufficient physical activity and such symptoms as walking limitations, depression, fatigue, and cognitive involvement.
Patients who were motivated to continue physical activity used their personal resources to try to maintain it. Koopmans et al26 used semi-structured interviews to examine facilitators and barriers to physical activity during the pandemic. Their conclusions note that through creativity and adaptation, participants were able to continue performing physical activity at home, with online classes, or outdoors, where the risk of infection was minimised by limiting social contact. Among individuals in our sample whose physical activity increased, one of the main reasons cited was awareness of the physical and mental benefits of physical activity; family support was another of the most important facilitators.
The type of physical activity showing the greatest growth was walking. There seems to be a window of opportunity to use walking to increase physical activity among patients with MS, although few studies have addressed walking in training programmes seeking to increase physical activity.20,27 Addressing this point, a recent publication by our study group underscored the benefits of Nordic walking training for patients with MS, particularly in those with restricted capacity to walk due to motor or balance problems, as the poles facilitate more upright, stable gait.28 Nordic walking was associated with improvement in gait parameters, mood, and quality of life.28
However, the pandemic saw a decrease in physical activity levels in a community that was already more sedentary than the general population of the same age, or other populations with neurological disorders29; therefore, we must analyse the barriers leading to this decrease. Koopman et al27 point to the fear of infection and the fact that remote physical activity interventions offer less opportunity for social interaction, which was exacerbated by physical distancing policies during lockdown.27 Salmani et al30 identified lack of knowledge about self-care among this patient group, limited access to resources, and greater physical and cognitive disability as barriers to physical activity. The greatest barrier observed in our survey was the closure of sports facilities and rehabilitation centres. At the time the survey was conducted, home exercise was not an option considered for patients with MS as a collective in Spain; this would also explain the decrease in physical activity levels among those with more severe disease.
Regarding technology use, Malliaras et al31 identified facilitators and barriers to telerehabilitation, concluding that the loss of the therapist–patient relationship, environmental barriers, physical distance, and patients' lack of practise all contributed to telerehabilitation being less-effective and less-valued. As facilitators, they noted the savings in travel time and waiting time. Ellis et al32 highlight the initial technical difficulties with the Internet and various virtual meeting platforms.32 Although users expressed surprise at the benefits of telerehabilitation, despite their initial expectations, it is unclear whether the intervention would be as broadly accepted outside the context of the pandemic. Our results show that use of technology was a facilitator for self-management of physical health, although it also constituted a barrier due to some families' limited Internet access, difficulty finding an appropriate space at home, and the fact that physical activity was performed individually and often without professional supervision.
Finally, it should be noted that this healthcare crisis led to the implementation of a broad range of actions in healthcare systems, accelerating the creation of audiovisual and virtual rehabilitation resources in order to reach affected communities. In the case of patients with MS, telerehabilitation may enable the provision of therapy with a broad reach in terms of geographical area, number of users, and duration; this approach to maintenance treatment may improve adherence and ensure long-term neurorehabilitation therapy. Despite this, and as noted by Hale et al,33 it is important for any intervention of this type to be proven to be effective, and to meet the needs and preferences of patients with MS, the end users of this resource.
LimitationsThis study is subject to certain limitations that should be taken into account when interpreting its results. Firstly, the patient sample was relatively small with respect to the total population with MS in Spain, and studied physical exercise habits at a very specific moment of the COVID-19 pandemic; therefore, the results cannot be extrapolated to other populations or contexts.
In addition, the study is based on a self-reported survey, which may have led to bias in the population who completed it and the responses submitted. As data collection was completely anonymous, it was not possible to compare the characteristics of the set of respondents against those who did not complete the survey.
Finally, although the content of the survey was developed by an expert panel, it would have been more appropriate to use standardised, validated scales to enable comparison of levels of physical activity during the pandemic to those reported in previous studies.
ConclusionsDuring the COVID-19 pandemic, physical activity levels decreased among patients with MS, and particularly among those with mild–moderate disability and for moderate–high intensity physical activity. The main reasons for this decrease were difficulty accessing sports and healthcare facilities, and fear of SARS-CoV-2 infection. Among patients who remained physically active, walking was the most frequent form of exercise. Technology use was a facilitator for some respondents and a barrier for others.
Although COVID-19 has now entered an endemic phase, this experience should boost the development and application of interventions to facilitate physical activity among patients with MS. This would encourage self-care and self-management of physical health with a view to future crises; this is of particular relevance to patients with such chronic diseases as MS, who require continuous multidisciplinary care but whose access to healthcare services, and particularly neurorehabilitation, is limited by the finite capacity of the healthcare system.
FundingThis project received no funding of any kind from any public or private organisation.
Informed consentThe authors obtained informed consent from the patients and/or subjects described in the article. The informed consent documents are held by the corresponding author.
Ethical considerationsThe authors declare that the procedures followed comply with the ethical standards of the relevant committee on human experimentation, the World Medical Association, and the Declaration of Helsinki. The authors observed their centre's protocols for the publication of patient data.
The authors wish to thank Sandra Fernández (Spanish Federation of Multiple Sclerosis; EM España), Gisela Carrés (Fundació Esclerosi Múltiple; FEM), and Pedro Carrascal (Multiple Sclerosis Association of Biscay; EM Euskadi) for their support and assistance in distributing the surveys through their communication channels. We are also grateful to the survey respondents for generously taking the time to provide their information.