At the beginning of the pandemic, it was suggested that lockdown and social distancing could affect the physical, emotional, and cognitive aspects of people, especially the elderly.
ObjectiveTo determine the characteristics of physical activity, mental health, support networks, and lifestyle of the elderly in lockdown by COVID-19 and its relationship with memory functioning.
Method100 healthy elderlies (age ≥60 years) participated and answered a set of online instruments that evaluated 6 variables: demographic data, physical activity, mental health, social support networks, lifestyle, and subjective memory. MoCA and Neuropsi tests were applied through a video call. The study was conducted between September 2021 and May 2022.
ResultsParticipants reported being and having been physically active, the presence of trait and state anxiety was found in 100%, also a higher perception of support from the family network. Insomnia was found in 46% of the sample, increased consumption of stimulant beverages and tobacco, and adequate competence in handling information and communication media. The memory functioning of 97% of the participants was normal or high normal, with fair self-perception of memory functioning. Correlations were moderate between mental health and self-perceived memory.
ConclusionsThe results suggest that having social support networks, good mental health, and staying physically and cognitively active favour memory function.
Al inicio de la pandemia se planteó que el confinamiento y el distanciamiento físico y social pudieran afectar aspectos físicos, emocionales y cognitivos de las personas, en especial de los adultos mayores (AM).
ObjetivoDeterminar las características de la actividad física, la salud mental, las redes de apoyo y el estilo de vida de AM en el confinamiento por COVID-19 y su relación con el funcionamiento de la memoria.
MétodoParticiparon 100 AM saludables (edad ≥60 años) quienes contestaron un conjunto de instrumentos en línea que evaluaron seis variables: datos demográficos, actividad física, salud mental, redes de apoyo social, estilo de vida y memoria subjetiva. Mediante una videollamada se aplicó el MoCA y el Neuropsi. El estudio se realizó entre septiembre 2021-mayo 2022.
ResultadosLos participantes refieren ser y haber sido activos físicamente, se encontró presencia de ansiedad rasgo y estado en el 100%, mayor percepción de porcentaje de apoyo de la red familiar. Se encontró insomnio en el 46% de la muestra, incremento en el consumo de bebidas estimulantes y tabaco, y competencia adecuada en el manejo de medios informativos y comunicativos. El funcionamiento de la memoria del 97% de los participantes fue normal o normal alto, con una autopercepción regular del funcionamiento de la memoria. Las correlaciones fueron moderadas entre salud mental y memoria autopercibida.
ConclusionesLos resultados sugieren que contar con redes de apoyo social, una buena salud mental y mantenerse activos física y cognitivamente, favorece el funcionamiento de la memoria.
The novel coronavirus SARS-CoV-2, which causes COVID-19, was first identified in late 2019.1 Older adults became a high-risk, vulnerable population, with numerous international clinical and epidemiological studies reporting high rates of transmission, morbidity, and mortality in this population.2–7 The rapid spread of the disease led health organisations worldwide to issue recommendations aimed at preventing and reducing transmission of the virus,2,8 such as physical distancing and even lockdown measures.8–10
At the beginning of the COVID-19 pandemic, some communications published in scientific journals warned about the detrimental effects of physical distancing and lockdown in older adults. Aubertin-Leheudre and Rolland9 gathered health and physical activity data using an application paired with a fitness tracker or smartwatch, and found a statistically significant decrease in overall physical activity in older adults, specifically in the mean weekly step count. Like other authors, they concluded that decreased physical activity has a negative impact on physical health,9,11,12 increases frailty, and decreases muscle strength and mass.9,12,13
Other studies suggest that the pandemic may have caused mental health problems,11 particularly anxiety, stress,3 distress, irritability, fear, depression,14 uncertainty, distorted perception of risk, somatisation,15 anger, frustration, boredom,12,16 and loneliness.11,16 With the pandemic, we also expected to observe changes in support networks as both lockdown and physical distancing would significantly reduce contact with relatives and friends. It was also suggested that older adults would become more dependent on their children, needing help for such tasks as shopping for everyday necessities.16 Furthermore, older adults may experience difficulty communicating due to limited access to Internet-based services and smartphones and limited familiarity with new technologies.11,16 They were also at greater risk of presenting increased alcohol and tobacco use,15 insomnia,3,14,15 and neurocognitive problems,12,17 and of receiving less cognitive stimulation.11
Several authors have suggested that episodic memory (the capacity to consciously recall experiences and events) is particularly vulnerable to ageing18–20; therefore, it was of vital importance to evaluate the impact of the pandemic and lockdown on this cognitive domain.
The purpose of this study was to describe the characteristics of physical activity, mental health, support networks, and lifestyle in older adults during lockdown due to the COVID-19 pandemic, and to analyse the impact of these factors on memory.
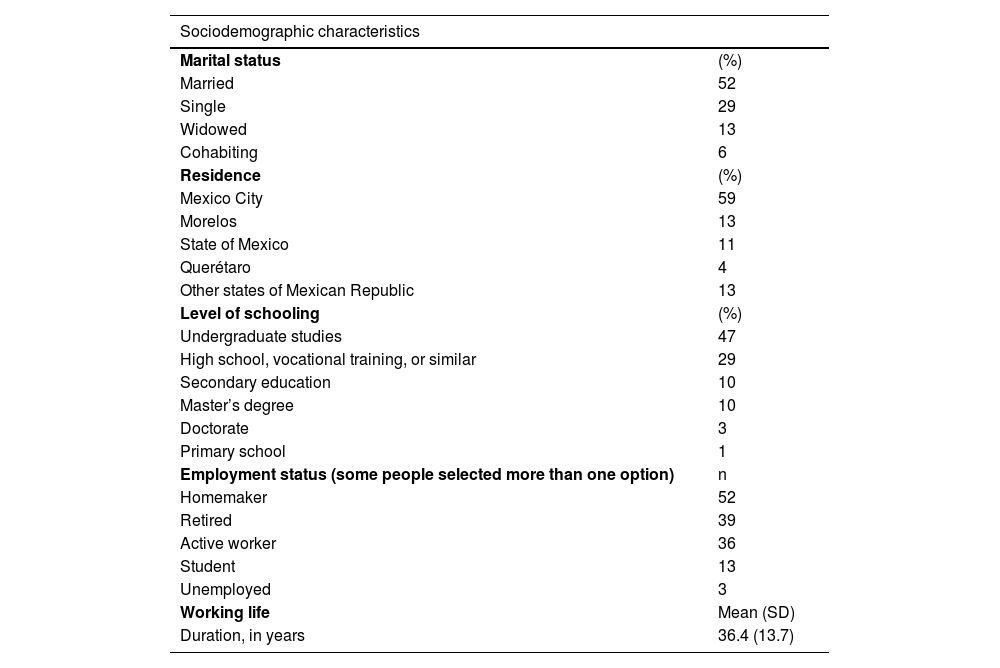
Material and methodsParticipantsThe study sample comprised 100 healthy older adults (aged ≥60 years), who were recruited through social media platforms. Volunteers were included if they met the following criteria: (1) aged ≥60 years, (2) with completed primary education, (3) with access to an electronic device connected to the Internet and with an application for video calling (either by themselves or with help), and (4) presenting a Montreal Cognitive Assessment (MoCA) score ≥24. Table 1 summarises the participants’ sociodemographic characteristics. Mean age (SD) was 67.2 (5.6) years (range, 60–80); 75% were women. Most participants were married (52%), lived in Mexico City (59%), and had a university degree (47%). The most common employment status was homemaker (36.3%), and the average duration of working life was 36.4 years. Mean MoCA score (SD) was 26.4 (1.9) (range, 24–30), which indicates normal cognitive function.
Sociodemographic characteristics of the participants.
| Sociodemographic characteristics | |
|---|---|
| Marital status | (%) |
| Married | 52 |
| Single | 29 |
| Widowed | 13 |
| Cohabiting | 6 |
| Residence | (%) |
| Mexico City | 59 |
| Morelos | 13 |
| State of Mexico | 11 |
| Querétaro | 4 |
| Other states of Mexican Republic | 13 |
| Level of schooling | (%) |
| Undergraduate studies | 47 |
| High school, vocational training, or similar | 29 |
| Secondary education | 10 |
| Master’s degree | 10 |
| Doctorate | 3 |
| Primary school | 1 |
| Employment status (some people selected more than one option) | n |
| Homemaker | 52 |
| Retired | 39 |
| Active worker | 36 |
| Student | 13 |
| Unemployed | 3 |
| Working life | Mean (SD) |
| Duration, in years | 36.4 (13.7) |
We administered the MoCA to rule out cognitive impairment. Data were gathered with an ad hoc questionnaire on demographic and other variables, the Yesavage’s Geriatric Depression Scale (GDS), the State-Trait Anxiety Inventory (STAI), the Social Support Network Scale for Elderly Adults (ERASAM, for its Spanish initials), the Athens Insomnia Scale, and the NEUROPSI Attention and Memory battery.
Montreal cognitive assessment. The MoCA was designed to screen for mild cognitive impairment. It tests 6 domains: attention/concentration/working memory, executive functioning, memory, language, visuospatial skills, and orientation. Administration time is approximately 10 min, and the maximum score is 30 points. In individuals with 12 or fewer years of schooling, the final score is adjusted by adding 1 point. Scores of 0–23 indicate probable cognitive impairment, whereas scores of 24–30 indicate normal cognitive function.21
Questionnaire on demographic and other variables. This ad hoc questionnaire includes open- and closed-ended questions (mixed, polytomous, multiple-choice, numeric-rating), to gather data on 5 variables: (1) Sociodemographic data (age, sex, marital status, place of residence, employment status, and duration of working life). (2) Physical activity during lockdown (total hours spent sitting per day, increase in total hours spent sitting, number and type of incidental activities), physical activity in previous life stages (type of physical exercise, amount of physical exercise activities, frequency of physical activity, session duration in minutes), physical activity before lockdown (amount), physical activity during lockdown (type, number, and frequency of physical activities, session duration in minutes, number of days per week in which participants walked for at least 10 consecutive minutes). (3) To quantitatively evaluate mental health, participants were asked about positive and negative mood states, negative mood during lockdown (fear of contracting COVID-19, fear of attending a hospital or medical consultation, loneliness, sadness, panic attacks, stress, perception that the pandemic changed their life, tolerance, anger, arguments with others), positive mood during lockdown (moments of happiness and feelings of companionship). (4) Lifestyle during lockdown (increased daily consumption of tobacco, black coffee, or black tea; increased weekly consumption of alcohol; type and number of media used to stay informed about the pandemic; type and number of leisure activities performed; number of hours spent on leisure activities per day; type and number of communication tools used during lockdown; frequency of communication with other people). (5) Subjective memory during lockdown (self-perception of memory function, self-perception of memory problems).
Yesavage’s geriatric depression scale. This self-administered scale includes 30 dichotomous questions (yes/no) to screen for specific symptoms of geriatric depression. Scores 0–10 indicate no depression, scores 11–20 indicate mild depression, and scores 21–30 indicate moderate-to-severe depression.22
State-trait anxiety inventory. The Spanish-language version of the STAI measures 2 dimensions of anxiety: state anxiety, or how an individual is feeling at a particular moment, and trait anxiety, or how the individual generally feels. Subjects must rate each item of the inventory on a 4-point intensity scale. Total score indicates the subject’s level of anxiety (low ≤29, moderate 30-44, or high ≥45).23
Social support network scale for elderly adults. The ERASAM is a semi-structured questionnaire that evaluates the level of satisfaction in 3 social support networks: (1) family (partner, children, close relatives), (2) community (friends and the community), and (3) institutional networks. It explores 4 types of support: emotional (affect, company, empathy, appreciation, and attention), instrumental (care, transportation, and housework), material (money, accommodation, food, clothing, and services), and informational support (health promotion, location of support networks, and sharing of experiences). The score ranges from 0 to 100, where a higher score means greater perceived support from the social network.24
Athens insomnia scale. This instrument includes 8 items that quantitatively analyse sleeping, sleep quality, and the impact of sleep on daytime functioning. The cut-off score for insomnia in Mexican population samples is 6 points.25
NEUROPSI attention and memory. This tool evaluates short- and long-term, working, verbal, and visuospatial memory. It is administered by a healthcare professional and provides both quantitative and qualitative data. Raw data were quantified and converted to normalised scores. Total scores and normalisation parameters indicate the grade or level of alteration (high normal, normal, mild to moderate, and severe). We considered the following memory subtests: (1) working memory: digit span; (2) coding: memory curve, paired associates, logical memory stories, Rey-Osterrieth Complex Figure, and faces; (3) recall: spontaneous verbal memory, cued verbal memory, verbal memory recognition, paired associates, logical memory stories, Rey-Osterrieth Complex Figure, face recognition, and global memory functioning.26 The cube regression subtest was not considered, as it requires participants to manipulate materials.
ProcedureThe questionnaire on demographic and other variables, GDS, STAI, ERASAM, and Athens Insomnia Scale were administered virtually using a Google form, between 23 September 2021 and 23 May 2022. Participants received the link via email or text message. At a later stage, a video call was made with each participant; guided by a researcher, participants completed the MoCA, which aimed to rule out cognitive impairment, and the memory section of the NEUROPSI test (objective-episodic memory).
The protocol was approved by an institutional research ethics committee (registration number 32/21). All participants digitally signed and submitted an informed consent form, authorising the use of their anonymised data.
Data analysisWe performed a descriptive analysis (mean, standard deviation, frequency, percentage) to describe the sociodemographic characteristics and data on the physical activity, mental health, social support networks, lifestyle, and objective and subjective memory of our cohort. To analyse associations between variables, we calculated the Pearson or Spearman correlation coefficients, as appropriate. The Spearman correlation coefficient was used in the majority of cases. Statistical analysis was performed with SPSS statistics software, version 26, and the threshold for significance was set at p≤.05.
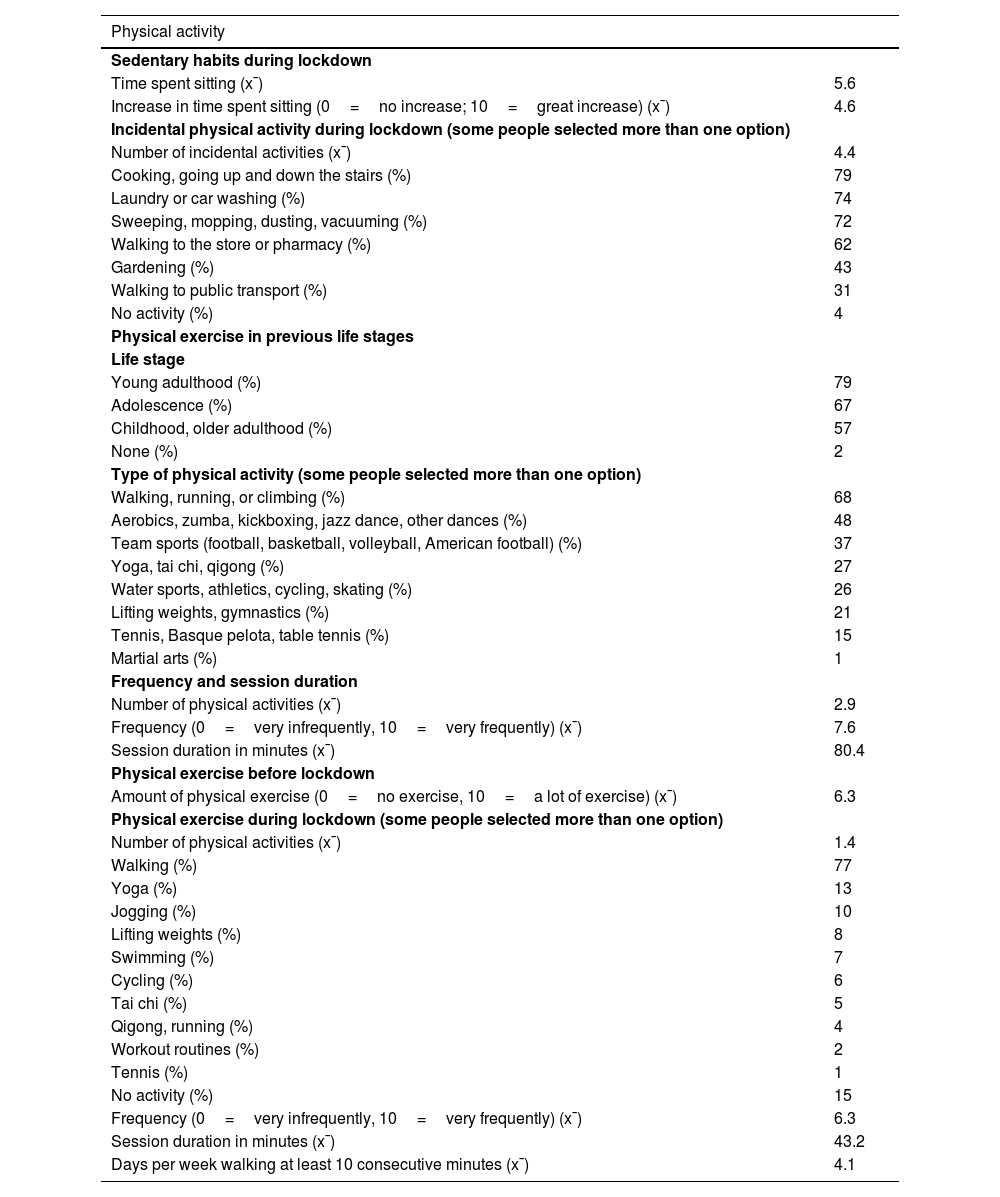
ResultsPhysical activityThe mean time spent sitting during lockdown was 5.6 h per day (SD: 2.6; range, 1–15). Participants routinely performed a mean of 4.4 incidental activities, with the most frequent being cooking, going up and down the stairs, doing the laundry, and washing the car. Furthermore, 79% had performed some type of physical exercise in one or more life stages, particularly in early adulthood; they practised a mean of 2.9 different activities, mainly walking, running, and climbing (68%); they practised sports frequently, with sessions lasting a mean of 81.4 min. Before lockdown, participants performed physical exercise with moderate frequency, whereas during lockdown they reported a mean of 1.4 types of physical exercise, with the most frequent being walking (77%). Frequency of physical activity was moderate, with sessions lasting a mean of 43.2 min. Furthermore, participants reported walking for over 10 consecutive minutes a mean of 4.1 days per week (Table 2).
Characteristics of the physical activity of our sample.
| Physical activity | |
|---|---|
| Sedentary habits during lockdown | |
| Time spent sitting (x¯) | 5.6 |
| Increase in time spent sitting (0=no increase; 10=great increase) (x¯) | 4.6 |
| Incidental physical activity during lockdown (some people selected more than one option) | |
| Number of incidental activities (x¯) | 4.4 |
| Cooking, going up and down the stairs (%) | 79 |
| Laundry or car washing (%) | 74 |
| Sweeping, mopping, dusting, vacuuming (%) | 72 |
| Walking to the store or pharmacy (%) | 62 |
| Gardening (%) | 43 |
| Walking to public transport (%) | 31 |
| No activity (%) | 4 |
| Physical exercise in previous life stages | |
| Life stage | |
| Young adulthood (%) | 79 |
| Adolescence (%) | 67 |
| Childhood, older adulthood (%) | 57 |
| None (%) | 2 |
| Type of physical activity (some people selected more than one option) | |
| Walking, running, or climbing (%) | 68 |
| Aerobics, zumba, kickboxing, jazz dance, other dances (%) | 48 |
| Team sports (football, basketball, volleyball, American football) (%) | 37 |
| Yoga, tai chi, qigong (%) | 27 |
| Water sports, athletics, cycling, skating (%) | 26 |
| Lifting weights, gymnastics (%) | 21 |
| Tennis, Basque pelota, table tennis (%) | 15 |
| Martial arts (%) | 1 |
| Frequency and session duration | |
| Number of physical activities (x¯) | 2.9 |
| Frequency (0=very infrequently, 10=very frequently) (x¯) | 7.6 |
| Session duration in minutes (x¯) | 80.4 |
| Physical exercise before lockdown | |
| Amount of physical exercise (0=no exercise, 10=a lot of exercise) (x¯) | 6.3 |
| Physical exercise during lockdown (some people selected more than one option) | |
| Number of physical activities (x¯) | 1.4 |
| Walking (%) | 77 |
| Yoga (%) | 13 |
| Jogging (%) | 10 |
| Lifting weights (%) | 8 |
| Swimming (%) | 7 |
| Cycling (%) | 6 |
| Tai chi (%) | 5 |
| Qigong, running (%) | 4 |
| Workout routines (%) | 2 |
| Tennis (%) | 1 |
| No activity (%) | 15 |
| Frequency (0=very infrequently, 10=very frequently) (x¯) | 6.3 |
| Session duration in minutes (x¯) | 43.2 |
| Days per week walking at least 10 consecutive minutes (x¯) | 4.1 |
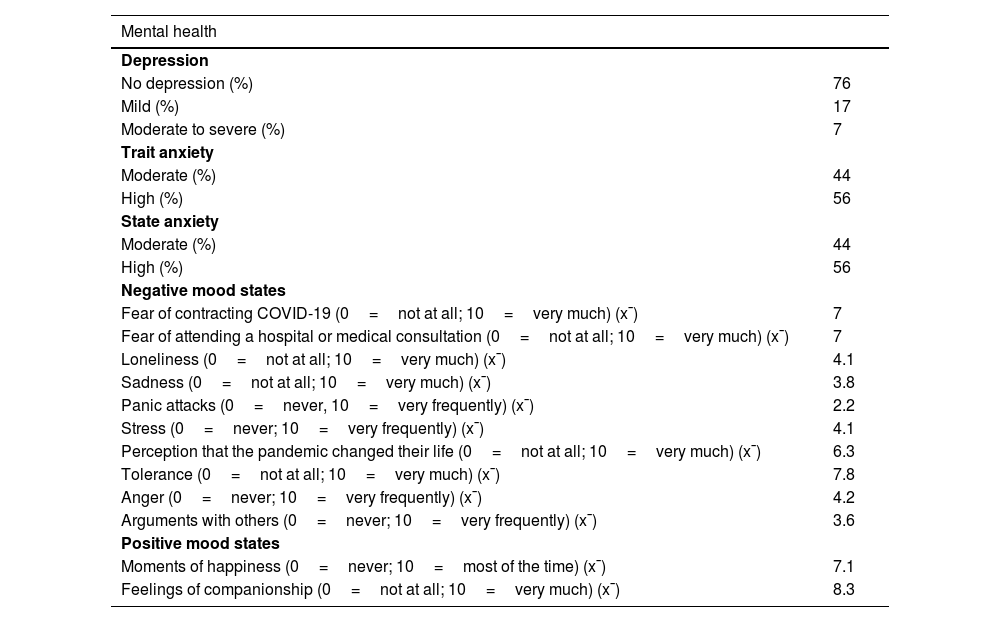
A total of 24% of participants reported symptoms of depression (mild to severe); however, 100% presented scores above the cut-off point for identifying symptoms of trait or state anxiety (moderate to high), with the same percentages in both types of anxiety (44% with moderate anxiety and 56% with high anxiety). Participants reported mood states associated with negative emotions, mainly fear of contracting COVID-19, fear of attending a hospital or medical consultation, and perception that the pandemic had changed their life; they also reported being tolerant of others during lockdown. Regarding positive mood states, participants reported feeling accompanied during lockdown (Table 3).
Mental health and mood states during lockdown.
| Mental health | |
|---|---|
| Depression | |
| No depression (%) | 76 |
| Mild (%) | 17 |
| Moderate to severe (%) | 7 |
| Trait anxiety | |
| Moderate (%) | 44 |
| High (%) | 56 |
| State anxiety | |
| Moderate (%) | 44 |
| High (%) | 56 |
| Negative mood states | |
| Fear of contracting COVID-19 (0=not at all; 10=very much) (x¯) | 7 |
| Fear of attending a hospital or medical consultation (0=not at all; 10=very much) (x¯) | 7 |
| Loneliness (0=not at all; 10=very much) (x¯) | 4.1 |
| Sadness (0=not at all; 10=very much) (x¯) | 3.8 |
| Panic attacks (0=never, 10=very frequently) (x¯) | 2.2 |
| Stress (0=never; 10=very frequently) (x¯) | 4.1 |
| Perception that the pandemic changed their life (0=not at all; 10=very much) (x¯) | 6.3 |
| Tolerance (0=not at all; 10=very much) (x¯) | 7.8 |
| Anger (0=never; 10=very frequently) (x¯) | 4.2 |
| Arguments with others (0=never; 10=very frequently) (x¯) | 3.6 |
| Positive mood states | |
| Moments of happiness (0=never; 10=most of the time) (x¯) | 7.1 |
| Feelings of companionship (0=not at all; 10=very much) (x¯) | 8.3 |
Perception of social support mainly came from the family network (57.3%; SD: 21.5%; range, 5%–100%), followed by the institutional network (29.6%; SD: 22.6%; range, 0%–95%) and the community network (29.1%; SD: 18.2%; range, 0%–100%). Mean overall support was 43.1% (SD: 14.2%; range, 11%–77%).
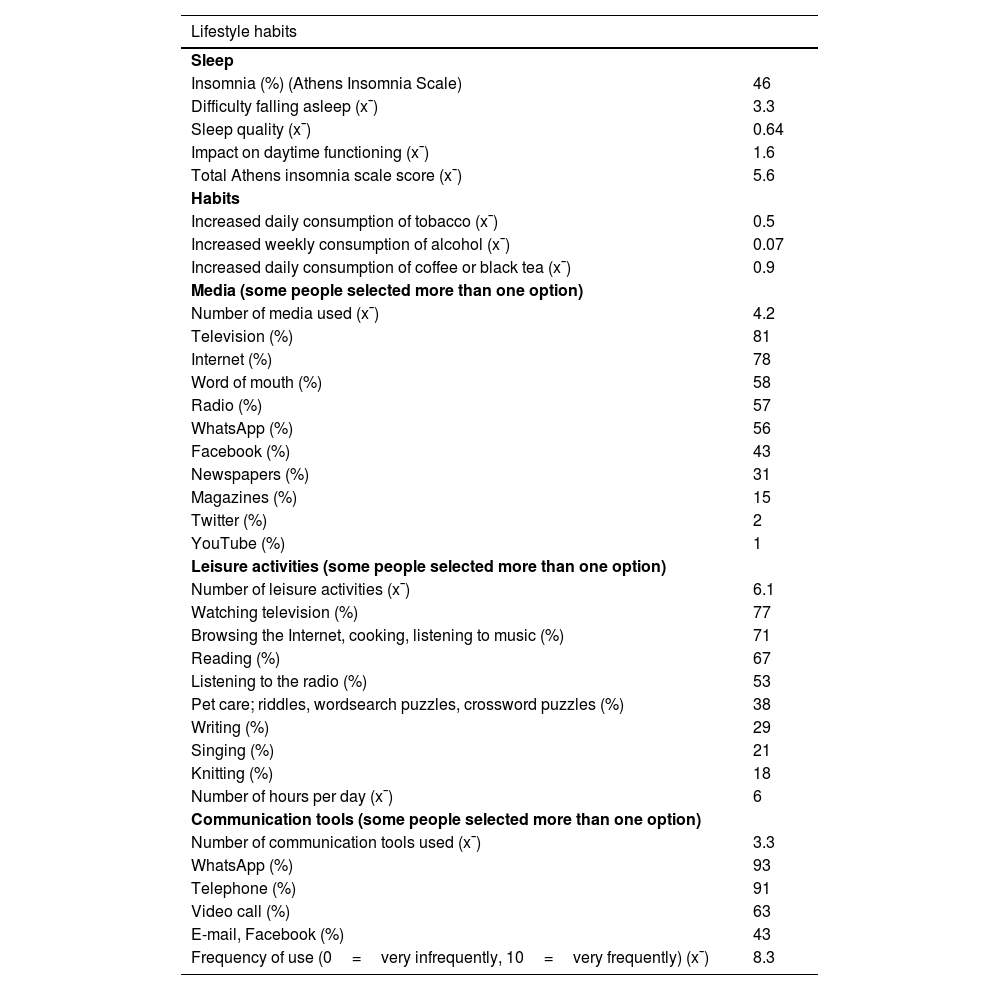
LifestyleThe main sleep-related problem was difficulty in sleeping, with a mean score of 3.3 points (maximum possible score of 12); 46% of participants scored above the cut-off point for insomnia. Participants reported an increase in daily consumption of black coffee or black tea, with a mean of 0.9 cups. The mean number of media used to stay informed about the pandemic was 4.2, with the most frequent being television and the Internet. The mean number of leisure activities performed during lockdown was 6.1, with the most frequent being watching television, browsing the Internet, cooking, and listening to music; mean time spent on leisure activities was 6 h per day. Participants maintained contact with other people using a mean of 3.3 communication tools, with the most frequent being WhatsApp and phone calls. Communication tools were used frequently (mean score of 8.3 on a 10-point scale) (Table 4).
Lifestyle habits during lockdown.
| Lifestyle habits | |
|---|---|
| Sleep | |
| Insomnia (%) (Athens Insomnia Scale) | 46 |
| Difficulty falling asleep (x¯) | 3.3 |
| Sleep quality (x¯) | 0.64 |
| Impact on daytime functioning (x¯) | 1.6 |
| Total Athens insomnia scale score (x¯) | 5.6 |
| Habits | |
| Increased daily consumption of tobacco (x¯) | 0.5 |
| Increased weekly consumption of alcohol (x¯) | 0.07 |
| Increased daily consumption of coffee or black tea (x¯) | 0.9 |
| Media (some people selected more than one option) | |
| Number of media used (x¯) | 4.2 |
| Television (%) | 81 |
| Internet (%) | 78 |
| Word of mouth (%) | 58 |
| Radio (%) | 57 |
| WhatsApp (%) | 56 |
| Facebook (%) | 43 |
| Newspapers (%) | 31 |
| Magazines (%) | 15 |
| Twitter (%) | 2 |
| YouTube (%) | 1 |
| Leisure activities (some people selected more than one option) | |
| Number of leisure activities (x¯) | 6.1 |
| Watching television (%) | 77 |
| Browsing the Internet, cooking, listening to music (%) | 71 |
| Reading (%) | 67 |
| Listening to the radio (%) | 53 |
| Pet care; riddles, wordsearch puzzles, crossword puzzles (%) | 38 |
| Writing (%) | 29 |
| Singing (%) | 21 |
| Knitting (%) | 18 |
| Number of hours per day (x¯) | 6 |
| Communication tools (some people selected more than one option) | |
| Number of communication tools used (x¯) | 3.3 |
| WhatsApp (%) | 93 |
| Telephone (%) | 91 |
| Video call (%) | 63 |
| E-mail, Facebook (%) | 43 |
| Frequency of use (0=very infrequently, 10=very frequently) (x¯) | 8.3 |
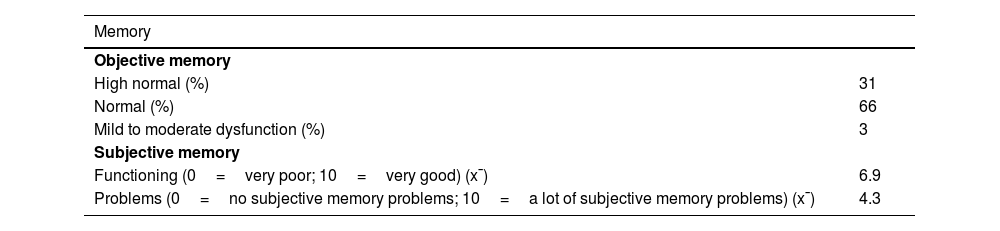
According to NEUROPSI scores, objective memory function was normal (66%) or high normal (31%) in 97% of the sample. Subjective memory was fair both in terms of functioning and subjective memory problems (scores of 6.9 and 4.3 out of 10, respectively) (Table 5).
Characteristics of objective and subjective memory.
| Memory | |
|---|---|
| Objective memory | |
| High normal (%) | 31 |
| Normal (%) | 66 |
| Mild to moderate dysfunction (%) | 3 |
| Subjective memory | |
| Functioning (0=very poor; 10=very good) (x¯) | 6.9 |
| Problems (0=no subjective memory problems; 10=a lot of subjective memory problems) (x¯) | 4.3 |
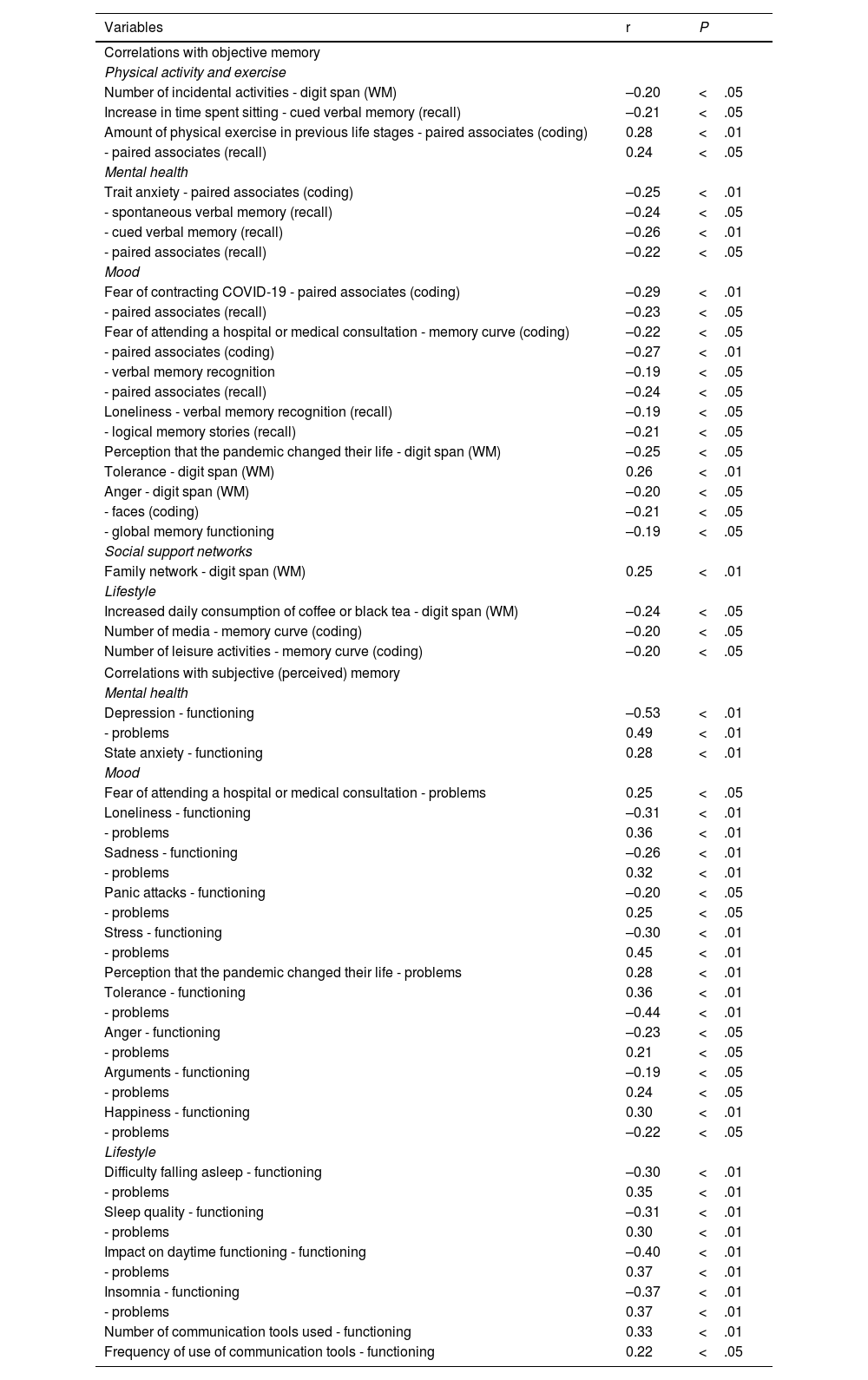
Regarding objective memory, the strongest correlations were between the amount of physical exercise in previous life stages and paired associate coding (r=0.28; p<.01), and between the amount of physical exercise in previous life stages and paired associate recall (r=0.24; p<.05). Other significant associations were found between trait anxiety and verbal memory cued recall (r=–0.26; p<.01), fear of contracting COVID-19 and paired associate coding (r=–0.29; p<.01), family support network and working memory digit span (r=0.25; p<.01), and increased daily consumption of coffee or black tea and working memory digit span (r=–0.24; p<.05).
Regarding subjective memory, the strongest correlations were between perceived functioning and depression (r=–0.53; p<.01) and impact of sleep on daytime functioning (r=–0.40; p<.01), and between subjective memory problems and depression (r=0.49; p<.01), stress (r=0.45; p<.01), and tolerance of others (r=–0.44; p<.01) (Table 6).
Bivariate correlations between objective/subjective memory and physical activity, mental health, social support networks, and lifestyle factors.
| Variables | r | P |
|---|---|---|
| Correlations with objective memory | ||
| Physical activity and exercise | ||
| Number of incidental activities - digit span (WM) | –0.20 | <.05 |
| Increase in time spent sitting - cued verbal memory (recall) | –0.21 | <.05 |
| Amount of physical exercise in previous life stages - paired associates (coding) | 0.28 | <.01 |
| - paired associates (recall) | 0.24 | <.05 |
| Mental health | ||
| Trait anxiety - paired associates (coding) | –0.25 | <.01 |
| - spontaneous verbal memory (recall) | –0.24 | <.05 |
| - cued verbal memory (recall) | –0.26 | <.01 |
| - paired associates (recall) | –0.22 | <.05 |
| Mood | ||
| Fear of contracting COVID-19 - paired associates (coding) | –0.29 | <.01 |
| - paired associates (recall) | –0.23 | <.05 |
| Fear of attending a hospital or medical consultation - memory curve (coding) | –0.22 | <.05 |
| - paired associates (coding) | –0.27 | <.01 |
| - verbal memory recognition | –0.19 | <.05 |
| - paired associates (recall) | –0.24 | <.05 |
| Loneliness - verbal memory recognition (recall) | –0.19 | <.05 |
| - logical memory stories (recall) | –0.21 | <.05 |
| Perception that the pandemic changed their life - digit span (WM) | –0.25 | <.05 |
| Tolerance - digit span (WM) | 0.26 | <.01 |
| Anger - digit span (WM) | –0.20 | <.05 |
| - faces (coding) | –0.21 | <.05 |
| - global memory functioning | –0.19 | <.05 |
| Social support networks | ||
| Family network - digit span (WM) | 0.25 | <.01 |
| Lifestyle | ||
| Increased daily consumption of coffee or black tea - digit span (WM) | –0.24 | <.05 |
| Number of media - memory curve (coding) | –0.20 | <.05 |
| Number of leisure activities - memory curve (coding) | –0.20 | <.05 |
| Correlations with subjective (perceived) memory | ||
| Mental health | ||
| Depression - functioning | –0.53 | <.01 |
| - problems | 0.49 | <.01 |
| State anxiety - functioning | 0.28 | <.01 |
| Mood | ||
| Fear of attending a hospital or medical consultation - problems | 0.25 | <.05 |
| Loneliness - functioning | –0.31 | <.01 |
| - problems | 0.36 | <.01 |
| Sadness - functioning | –0.26 | <.01 |
| - problems | 0.32 | <.01 |
| Panic attacks - functioning | –0.20 | <.05 |
| - problems | 0.25 | <.05 |
| Stress - functioning | –0.30 | <.01 |
| - problems | 0.45 | <.01 |
| Perception that the pandemic changed their life - problems | 0.28 | <.01 |
| Tolerance - functioning | 0.36 | <.01 |
| - problems | –0.44 | <.01 |
| Anger - functioning | –0.23 | <.05 |
| - problems | 0.21 | <.05 |
| Arguments - functioning | –0.19 | <.05 |
| - problems | 0.24 | <.05 |
| Happiness - functioning | 0.30 | <.01 |
| - problems | –0.22 | <.05 |
| Lifestyle | ||
| Difficulty falling asleep - functioning | –0.30 | <.01 |
| - problems | 0.35 | <.01 |
| Sleep quality - functioning | –0.31 | <.01 |
| - problems | 0.30 | <.01 |
| Impact on daytime functioning - functioning | –0.40 | <.01 |
| - problems | 0.37 | <.01 |
| Insomnia - functioning | –0.37 | <.01 |
| - problems | 0.37 | <.01 |
| Number of communication tools used - functioning | 0.33 | <.01 |
| Frequency of use of communication tools - functioning | 0.22 | <.05 |
⁎: Pearson correlation; WM: working memory.
This study provides information about the characteristics of physical exercise, mental health, social support networks, lifestyle, and memory, as well as the association between these variables and objective and subjective memory functioning, in a population of healthy older adults during voluntary lockdown due to the COVID-19 pandemic.
Our results indicate that, during lockdown, our participants perceived an increase in sedentary habits; they also reported being active by performing incidental activities, exercising in sessions of acceptable duration, and walking for at least 10 consecutive minutes an acceptable number of days per week. These data stand in contrast with other results in the literature, as numerous authors had suggested that lockdown may lead to significant decreases in physical exercise in this population.9,11,12 For instance, Okely et al27 reported sedentary habits and a decrease in physical activity, whereas other studies found that total time spent doing physical exercise remained unchanged or even increased significantly,28–30 with walking being the most frequent activity.29 Walking was also the activity preferred by our study participants.
Regarding mental health, we observed symptoms of moderate or severe anxiety (both trait and state) in the whole sample, as well as symptoms of mild to severe depression in approximately a quarter of participants. Furthermore, a study including a sample of older adults reported presence of negative mood states, such as fear of contracting COVID-19 or attending a hospital or medical consultation, perception that the pandemic changed their life, and, to a lesser extent, loneliness, stress, anger, sadness, greater tendency to arguing, and anxiety attacks.
These findings are consistent with the results reported by other authors at the beginning of the pandemic, who identified older adults as a population group at particular risk of developing mental health problems.9,11,16,17 This population group was therefore expected to present anxiety,3,14 depression,14 and negative mood states.12,14,15 Recent studies conducted during the pandemic report anxiety (with rates ranging from 14.4% to 18.8%),31–33 while others have found increased levels of anxiety.30,34,35 Similarly to our results, 2 studies conducted in Cuba found symptoms of anxiety in 100% and 94% of the participants, respectively.36,37 Depressive symptoms have been reported in 17.6%–40% of members of the samples studied during the pandemic29,31–33,38; the percentage of participants reporting depression in our study (24%) lies within that range. Regarding negative mood states, our results are consistent with those of previous studies, which report sadness, distress, fear,39 tension, and significantly higher levels of perceived stress in older adults.30 Our participants also reported negative mood states associated with restrictions due to the pandemic, which led to greater tendency to arguing and fear of attending a hospital.
Regarding social support networks, our results show that participants perceived more support from their family networks than from community and institutional networks. Previous studies have postulated that lockdown and physical distancing must necessarily have a negative impact on such aspects as socialising11,16,17 and perceived family support. This was not the case in our series of Mexican older adults, where lockdown was found to have a positive effect, in line with the results reported by Shaygan and Bahadori.16 These authors report a positive impact of the COVID-19 pandemic, as older adults could rely on their children to solve problems associated with lockdown. In fact, Okely et al27 and Docherty et al30 reported slightly higher levels of social support and interaction among their participants. Regarding social interactions, older adults in our study used different communication tools and media, which enabled them to maintain contact with other people, promoting closeness despite physical distance, and to access a large amount of information to stay informed about the pandemic. The most frequently used media were television and the Internet, and the most frequently used communication tools were text messages and phone calls. The preferred leisure activities were watching television and browsing the Internet. Soon after the onset of the public health emergency, it was suggested that lockdown and isolation would be aggravated by the difficulty faced by many older adults in remotely maintaining contact with family and friends. This difficulty arises from the need to own a device (smartphone, computer, or tablet), to know how to use communication applications (messaging and video calls), and have access to the Internet.11,16,17 Recent studies report that the preferred sources of information are television,29,40 newspapers, the Internet, and radio.29 The main communication tools were phone calls, messaging applications, social media, and email.29 The preferred leisure activities were watching television and using smartphones.40 Our sample presents adequate connectivity and digital literacy, which has an impact on the promotion of support and social interaction. This may be linked to the educational level of the sample, with more than 50% of participants having completed under- or postgraduate studies. In this regard, Dura-Perez et al40 suggest that during lockdown, new technologies have served as a resource for cognitive stimulation, access to information, leisure, and social connection. Maggi et al41 reported that greater perceived social support could result from telephone or online contact with family or friends, and Hamm et al42 noted that their participants felt that during the pandemic, they more frequently communicated and listened to their loved ones thanks to applications and electronic devices.
In terms of lifestyle factors, participants reported an increase in daily consumption of tobacco but not of alcoholic drinks. At the beginning of the pandemic, some researchers suggested that older adults might exhibit risk behaviours such as increased use of alcohol and tobacco.15 However, we did not find recent studies reporting these findings.
Regarding sleep quality in our sample, 46% of participants reported insomnia. Furthermore, the majority reported difficulty in sleeping, especially in terms of the time required to fall asleep, awakenings during the night, waking earlier than desired, and the overall duration of sleep. Several authors had already reported sleep problems and insomnia in older adults during the pandemic.3,14,15 Recent studies found a 46.8% prevalence of insomnia, as well as difficulties in initiating and maintaining sleep,29,32 frequent awakenings29 or waking earlier than desired,29,32 and changes in the sleep pattern.34 Our results confirm previous evidence and support the idea of significant prevalence of insomnia and sleep-related problems in this age group during the COVID-19 pandemic.
The objective memory of our participants was normal to high normal; however, subjective memory was rated as fair. Calderón-Larrañaga et al11 suggested that cognitive function may worsen due to reduced cognitive stimulation during lockdown, while Jiménez-Pavón et al12 recommended engaging in physical exercise during lockdown to prevent cognitive decline. Regarding objective memory, Carbone et al28 conducted a longitudinal study of working memory and long-term memory, finding sustained good functioning. In another study, Qi et al43 observed preserved working memory after 12 weeks of qigong training. It should be noted that our participants reported high levels of social interaction through virtual means and high levels of physical activity during lockdown, which may be associated with the persistence of good objective memory functioning even in conditions of physical isolation. On the other hand, our findings also confirm the trend observed in most recent studies that subjective memory is perceived to function poorly30,41 in 28%39 to 54.3%29 of the participants. Our results highlight the association between depression and perceived memory functioning during lockdown. This may be due to multiple factors present during the health emergency that may have affected emotional and mental health. The negative self-assessment of memory functioning may have been influenced by the possible internalisation of negative attitudes toward ageing,44 as well as negative perceptions about people and their abilities, frequently associated with depression, intensified by the perception of a higher vulnerability to mortality due to COVID-19 in this age group.
Study limitationsThe sociodemographic characteristics of our sample are not representative of older adults as a population group. Furthermore, 75% of participants were women, which further limits the extrapolation of our results to the rest of the Mexican population. Additionally, the sample was recruited virtually, and inclusion criteria required access to and knowledge of digital media and electronic devices, which does not accurately reflect the reality of older adults in Mexico. Furthermore, the majority of participants had a high level of education, suggesting a sociocultural and economic advantage. It is also important to note that during part of the data collection period, COVID-19 vaccination had already begun for older adults in Mexico (February–May 2021), which represents a change with respect to the context of the first year of the COVID-19 pandemic in Mexico. Additionally, we do not know all details of lockdown and company during this period. The use of video calls to assess memory function may have limited raters’ ability to observe important details, as was the case in the Rey-Osterrieth Complex Figure subtest. However, this study also contributes evidence on the use of telepsychology for research purposes.
ConclusionThe results obtained in our study reveal that objective memory functioning was optimal in our participants. However, from a qualitative viewpoint, participants did report memory deficiencies; therefore, it seems important to include the evaluation of depressive symptoms in the assessment of memory function. Regarding exercise, our findings underscore the importance of maintaining the amount of low- or high-intensity physical activity recommended by the World Health Organization for older adults. Engaging in routine incidental activities and reducing sedentary behaviour also demonstrated a protective effect on cognitive processes and psychosocial well-being. The characteristics of our sample, such as participants’ high socioeconomic status, high level of education, and use of computers, applications, and electronic devices, may have acted as protective factors. Technological instruments may serve as sources of cognitive stimulation or even components of an enriched environment. It is also crucial to focus on maintaining mental health, avoiding negative mood states, and cultivating social support networks. Our results highlight the influence of affective states and sleep quality on perceived memory functioning. Therefore, further research should include samples with different sociodemographic characteristics and at later stages of the COVID-19 pandemic. Finally, if physical and cognitive activity shows a favourable association with episodic memory performance and functioning, this study will help guide health interventions aimed at minimising negative consequences for older adults in the context of highly stressful events, such as the COVID-19 pandemic.
Ethical considerationsThe protocol was approved by the institutional research and ethics committee of Instituto Nacional de Rehabilitación “Luis Guillermo Ibarra Ibarra” (project code 32/21). The project was conducted in accordance with the standards of the Declaration of Helsinki on research involving human subjects.
Informed consentAll participants signed an informed consent form.
FundingThis study received no financial support from any institution.